The human auditory system possesses an amazing ability to accept and integrate sensory information from two ears. The ability to understand sound using two ears allows listeners to hear more effectively in noisy environments and to determine the directionality of sound. In this paper, we will discuss the binaural processing cues that our auditory system uses to recognize sounds and to separate them into different sound sources. We will also talk about ways to determine if two cochlear implants are necessary for optimal speech perception and localization performance or if one cochlear implant or one cochlear implant and one hearing aid on the opposite ear is sufficient.
Binaural Cues Associated With Two Ears
Typical cues discussed in the literature that are associated with hearing with two ears include binaural summation, the head shadow effect, the binaural squelch effect, and localization. When listening with two ears, depending upon the direction from which the sound comes from, each ear may receive different acoustic signals. These may include timing, amplitude, and spectral differences. However, each ear could also receive redundant information if the sound is emanating from the front of the listener, producing equal timing and amplitudes at each ear. When these signals from each ear are combined and processed by the brain, the listener may perceive double the loudness of the sound, and the sensitivity to small differences in intensity and frequency might also improve. This process is called binaural summation, and it can improve speech perception in both quiet and in noise.
The attenuation that results after a sound travels around the head to the ear is referred to as the head shadow effect. The head shadow affects high-frequency information more than low-frequency information, because the wavelengths for high frequency sounds are short compared to the size of the head;therefore, high-frequency sounds are attenuated much more than low frequency sounds. The head shadow effect occurs physically rather than as a result of the brain integrating and processing the sounds from the two ears (Shaw, 1974);however, the brain must be able to attend to the ear with the better signal-to-noise (S/N) ratio in order to be able to take advantage of this physical effect. The head shadow can be beneficial, for example, if someone is listening to a talker in a room with background noise;the barrier that is produced by the head and shoulders between the voice and the noise may enable the listener to hear the intended voice more audibly.
Another potential benefit of hearing with two ears is the binaural squelch effect. This effect is the ability to combine noise at the ear with a poorer S/N ratio with the noise from the ear with a more favorable S/N ratio. Through this process, the brainstem compares differences in timing, amplitude, and spectral information between the two ears (Carhart, 1965;Middlebrooks & Green, 1991;Zurek, 1993), and sounds are segregated into auditory objects.
It is also thought that listeners with two ears are able to use localization cues to separate sounds that are coming from different directions (Carhart, 1965;Dirks & Wilson, 1969;Durlach & Colburn, 1978;Yost & Dye, 1997). This ability is an important function performed by the auditory system. In order to perform this function, a listener must be able to detect differences in timing and level between the signals reaching the two ears. For example, when a sound is on one side of a listener, that sound will arrive at the ear closer to the source before it will arrive at the other ear. This difference in arrival time is called interaural time difference (ITD) and is primarily detected with low-frequency sounds. In addition, the level of the sound at the ear closer to the sound source will also be greater than that at the ear farther from the source. This difference is called interaural level difference (ILD) and is primarily localized by high-frequency sounds.
Many researchers have studied the abilities of listeners with cochlear implants to use binaural cues to understand speech in backgrounds of noise and localize sounds. These studies have included individuals with simultaneous and sequential bilateral cochlear implants as well as those with a cochlear implant on one ear and a hearing aid on the opposite ear. In general, research for both populations shows that most users can take advantage of the head shadow effect by disregarding the ear with the poorer signal to noise ratio and concentrating on the ear with the better S/N ratio;however, these individuals are limited in their ability to "squelch" unwanted sounds. In contrast, although most listeners with two cochlear implants are able to localize sounds effectively, this ability is relatively poor in listeners who wear a cochlear implant and hearing aid on opposite ears. Unpublished preliminary data at the University of Iowa have shown that getting a cochlear implant on one ear can be detrimental for localization for some users with two hearing aids. One reason for this might be that the hearing aid and the cochlear implant may be sending different timing and amplitude information to the brain;therefore, localization abilities become poorer when the two signals at both ears are dissimilar.
Cochlear implantation has become such a widely accepted method of giving hearing back to profoundly deafened listeners that some are arguing that bilateral cochlear implantation should become the standard surgical intervention for severely hearing impaired listeners. Because of this, it is important to understand and differentiate the benefits and limitations of bilateral and unilateral cochlear implantation for at least two reasons. First, bilateral implants are more costly and may require a second surgery. Second, because many hearing impaired listeners are requesting bilateral cochlear implants, insurers and government agencies are wrestling with the unknown expected benefits and costs. It is important to understand if listeners who wear a hearing aid and a cochlear implant on opposite ears could benefit from receiving a second cochlear implant. Although several pieces of literature focus on the speech perception performance of bilateral cochlear implant patients, very few compare the performance of patients with one cochlear implant to patients with two cochlear implants.
Are Two Cochlear Implants Better Than One Cochlear Implant?
The number of bilaterally implanted patients continues to grow and many studies including multi-center trials have further investigated the benefits of bilateral implants (Buss, Pillsbury, Buchman, Pillsbury, Clark et al., 2008;Litovsky, Parkinson, Arcaroli, & Sammeth, 2006;Laszig, Aschendorf, Stecker, Müller-Deile, Maune, Dillier, et al., 2004). Studies have examined speech perception (Schleich, Nopp, & Haese, 2004;Laszig et al., 2004), lateralization (Tyler, Gantz, Rubinstein et al., 2002;van Hoesel & Tyler 2002), and localization (Nopp & D'Haese, 2004;Grantham, Hornsby, & Erpenbeck, 2005) abilities of bilateral implantation;however, most of the research to date has focused primarily on comparisons that are not entirely realistic. This is because comparisons are typically done by asking a bilateral patient to remove one implant. Although this has the advantage of a within-subject control, the unilateral condition might be at an unfair disadvantage, because these patients routinely experience bilateral listening and lack everyday unilateral experience.
The most ideal way to determine whether having two cochlear implants (CI+CI) is superior to having one cochlear implant (CI-Only) is to directly compare the speech perception and localization abilities of users who have only one cochlear implant to speech perception and localization abilities of those same individuals after they receive a second cochlear implant. That is to compare their performances within themselves. However, because of limitations of insurance aas well as the reluctance of many users with one cochlear implant to receive a second cochlear implant, this comparison may be limited. In our recent research at the University of Iowa, we have focused on this limitation and have taken the initiative to study the importance of having two cochlear implants using another methodology.
In an attempt to make a fair assessment of the benefits of two cochlear implants, we matched a group of CI+CI users to a group of CI-Only users by age at implantation and duration of hearing loss. We chose these two variables as matching criterion because they have been reported in the literature as being important factors in the success of cochlear implantation (Gantz, Tyler, Rubinstein, Wolaver, Lowder, et al., 2002;Rubinstein, Parkinson, Tyler, & Gantz, 1999;van Dijk, van Olphen, Langereis, Mens, Brokx, & Smoorenburg, 1999;Waltzman, Fisher, Niparko, & Cohen, 1995). In a recent study comparing 64 subjects (32 CI+CI and 32 CI-Only) who participated in word recognition testing and 66 subjects (33 CI+CI and 33 CI-Only) who participated in sentence recognition testing, we found that the CI+CI users scored 24% better on word recognition and 19% better on sentences recognition than did the CI-Only users. In addition, the CI+CI users had localization accuracies of 25.4º (RMS-error) better than the CI-Only users (Dunn, Tyler, Oakley, Gantz, & Noble, 2008). In a preliminary investigation of the performance of CI+CI users to CI-Only users matched on age at implantation, duration of deafness, and pre-operative hearing thresholds, testing in noise showed that the CI+CI users were able to withstand more noise than the CI-Only subjects. Both of the tests utilized a target word and background noise that changed locations from an array of eight loudspeakers. In one test called Cueing-the-Listener, an auditory cue ("Hey, I am over here") was utilized to give the listener a 'hint' as to the origin of the loudspeaker that would play one of 12 spondee words. The spondee words were heard against a background of competing speech noise (a male and a female each repeating a different sentence from the same loudspeaker) (Turner et al., 2004) that was played from a spatially separate loudspeaker than the target spondee word. In the second test, Recognition with Multiple Jammers, a spondee word was presented from the front of the listener while at the same time from two separate loudspeakers (jammers) played randomly selected male and female sentences. The target was the same talker, whereas the talkers for the background noise varied from trial-to-trial.
Although there is evidence that two implants can improve performance relative to unilateral devices, it should be noted that the use of bilateral cochlear implants is not without problems. Patients with profound hearing impairment have limited nerve survival that may also be asymmetrical. This may result in an unnatural pattern of neural activity in stimulation with electrical pulses. The asynchronous electrical stimulation across devices might result in individual neural impulses which are unlikely to result in useful cues related to interaural differences. With that being said, it is unlikely that listeners with bilateral cochlear implants would give up one of their implants, even if it is one that does not perform as highly as the other.
Are Two Cochlear Implants Better Than Using A Cochlear Implant On One Ear And A Hearing Aid On The Opposite Ear?
A second related question is whether listeners with a cochlear implant and hearing aid on opposite ears (CI+HA) would benefit if they had a second cochlear implant. With advances in implant technology and speech processing strategies, the criteria for cochlear implant candidacy has been extended from profound hearing losses to include those with moderate-to-severe bilateral hearing losses. Thus, unilateral cochlear implant users may still have residual hearing amenable to a hearing aid in the non-implanted ear. Despite this, the number of unilateral cochlear implant users who have received a second implant on the opposite ear (sequential implantation) or persons with bilateral severe to profound hearing loss who have received two cochlear implants at the same time (simultaneous implantation) has steadily grown over the last decade. Whether a hearing aid in the opposite ear or a second cochlear implant can provide any additional benefits to cochlear implant users is controversial. Furthermore, very little data has been published on direct comparison of the binaural advantages between listeners with a cochlear implant and hearing aid on opposite ears and listeners with bilateral cochlear implants.
Again, the ideal way to know if CI+HA users would benefit more from a second cochlear implant than from the hearing aid in the opposite ear is to directly compare the speech perception and localization abilities using a cochlear implant and hearing aid on opposite ears to speech perception and localization abilities after receiving a second cochlear implant. In a small study by Ching, van Wanrooy, and Dillon (2007), two former users of a cochlear implant and hearing aid on opposite ears had improved localization abilities and speech perception scores after the second cochlear implant was activated for the first three to six months. However, following this time frame, their performances showed a slight decline. Because of the limited amount of research studying the additional benefit a second cochlear implant could provide a CI+HA user, we describe another way to evaluate the binaural advantages between these two groups. In the following section, we will summarize a methodology to answer whether two cochlear implants is better than using a cochlear implant on one ear and a hearing aid on the opposite ear.
Comparison Between Matched Pre-operative Speech Perception Scores Between CI+HA and CI+CI Users
When comparing two between-subject groups, it is important to try to match for subject variables that could affect the overall general comparison. One such variable that could affect the validity of the comparison between CI+HA users and CI+CI users is pre-operative residual hearing, therefore it is important to try to control for this variable as much as possible. One way to do this is by comparing pure-tone thresholds;however, because subjects who are candidates for cochlear implantation are often profoundly deafened, matching by this criterion could be limited. An alternative way to account for pre-operative residual hearing may be to match based upon pre-operative speech perception scores. Open-set speech discrimination tests, such as the Hearing in Noise Test (HINT) (Nilsson, Soli, & Sullivan, 1994), are widely used to evaluate CI candidacy and can be used as the speech perception measure for matching CI+HA users to bilateral cochlear implant users.
Once subjects have been matched pre-operatively, post-operative speech perception and localization scores can be compared to evaluate differences between these two groups to determine if wearing a hearing aid on the contralateral ear is as effective as using a cochlear implant. In addition, the overall contribution of the second device (the hearing aid for the CI+HA users or the cochlear implant for the CI+CI users) could be evaluated by subtracting the score with both devices worn together from the score with only one cochlear implant. This reveals the binaural advantage of having two devices versus having only one device.
A preliminary study using this methodology was evaluated at the University of Iowa. We matched the pre-operative HINT sentence scores of the hearing aid ear of four CI+HA users to either the right or left ear pre-operative HINT scores of a simultaneous bilateral cochlear implant user. We then compared the post-operative bilateral scores of the CI+HA users and the CI+CI users on Consonant-Nucleus-Consonant monosyllabic (CNC) (Tillman & Carhart, 1966) words in quiet, and City University of New York (CUNY) (Boothroyd, Hanin, & Hnath, 1985) sentences in noise (with noise presented from the front or 90° at the left or right), and Everyday-Sounds localization (Dunn et al, 2005). Each of the CI+HA users were matched to multiple CI+CI users. The average of all of the CI+CI user's post-operative scores that each CI+HA user was matched to was used for the comparisons.
The results indicated that for CNC words in quiet, the CI+HA users presented larger binaural advantages when compared to the CI+CI users (Figure 1A-C). 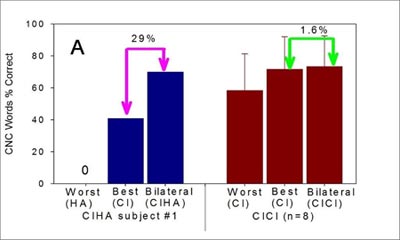
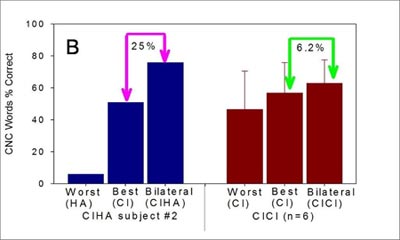
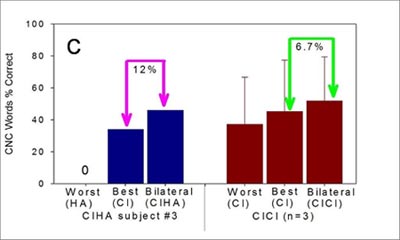
Figures 1A - C: Three CI+HA users (#1, #2, and #3) were matched by their pre-operative speech perception performances with bilateral hearing aids to the pre-operative speech perception performances of CI+CI users. Panels A, B, and C show the individual CI+HA results and the average of the CI+CI users' best unilateral, worst unilateral, and bilateral CNC words performance. The arrows and percentage numbers in each panel indicate the binaural advantages. The error bars show the mean and standard deviation of bilateral scores of CI+CI users. All three CI+HA users indicated larger binaural advantages than the average binaural advantages of CI+CI users.
On the contrary, for the CUNY sentence test in noise, the CI+HA users exhibited smaller binaural advantages compared to the CI+CI users (Figure 2 A-C). 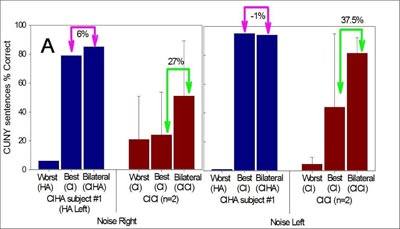
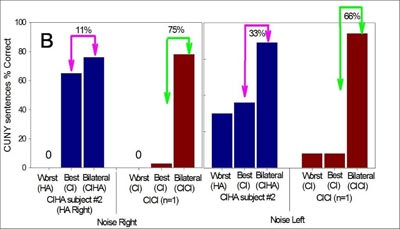

Figures 2A - C: Three CI+HA users (#1, #2 and #4) were matched by their pre-operative speech perception performances with bilateral hearing aids to the pre-operative speech perception performances of CI+CI users. Panels A, B, and C present the CUNY sentences % correct scores for each CI+HA user and their matched CI+CI users' left, right, and bilateral devices. The arrows and percentage numbers in each panel indicate the binaural advantages. The error bars show the mean and standard deviation of the bilateral scores of CI+CI users. All three CI+HA users showed much less binaural advantage than the average binaural advantage of CI+CI users, regardless of the position of the noise.
Finally, when assessing localization abilities, the CI+HA users in this study presented worse abilities than the matched bilateral cochlear implant users (Figure 3). It should be noted, however, that the participants matched in this study was small and a larger number would be needed to confirm these findings.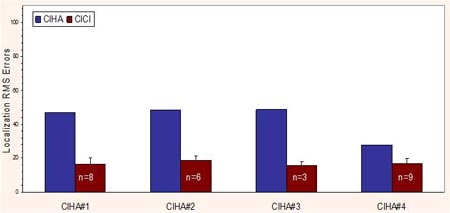
Figure 3: Four CI+HA users (#1, #2, #3, and #4) were matched by their pre-operative speech perception performance with hearing aids to the pre-operative speech performances of CI+CI users. The localization root-mean-squared (RMS) errors of CI+HA users were higher (worse) than the average RMS errors of CI+CI users.
Conclusion
The number of bilaterally implanted patients continues to grow and some are arguing that bilateral cochlear implantation should become the standard surgical intervention for severely hearing impaired listeners. However, it is important to be able to determine if bilateral cochlear implants are truly a better option than using only one cochlear implant or using a cochlear implant and a hearing aid on opposite ears. The current methodology to study if bilateral cochlear implants are indeed superior to unilateral cochlear implants is limited as it evaluates one cochlear implant to two cochlear implants by having a bilaterally implanted user remove one implant. In addition, there is very little research to date evaluating whether a listener with one cochlear implant and a hearing aid on the opposite ear would benefit from a second cochlear implant. In this paper we discussed methodologies that are more realistic in evaluating these two limitations. First we discussed research results where there was a comparison in performance of users with one cochlear implant to users with two cochlear implants who were matched by critical predictors of successful performance with a cochlear implant. In addition, a methodology was introduced whereby which we could evaluate the benefit of a second cochlear implant for listeners with a cochlear implant and a hearing aid. These methodologies are important because implanting hearing impaired listeners with two cochlear implants is not only costly but also doubles the risks associated with surgical intervention in both ears. Future studies need to evaluate these introduced methodologies in order to determine the efficacy of two cochlear implants.
References
Boothroyd, A., Hanin, L., & Hnath, T. (1985). A sentence test of speech perception: reliability, set equivalence, and short-term learning. New York: Speech and Hearing Sciences Research Center, City University of New York.
Buss E., Pillsbury HC, Buchman CA, Pillsbury CH, Clark MS, et al. (2008). Mulitcenter U.S. Bilateral MED-EL Cochlear Implantation Study:Speech Perception over the first year of use. Ear & Hearing, 29, 20-32.
Carhart, R. (1965). Monaural and binaural discrimination against competing sentences. International Audiology, 4, 5-10.
Ching, T.Y., van Wanrooy, E., & Dillon, H. (2007). Binaural-bimodal fitting or bilateral implantation for managing severe to profound deafness: a review. Trends Amplif. 11, 161-92.
Dirks, D.D., & Wilson, R.H. (1969). The effect of spatially separated sound sources on speech intelligibility. Journal of Speech and Hearing Research, 12, 5-38.
Dunn, C.C, Tyler, R.S, & Witt, S.A. (2005). Benefit of wearing a hearing aid on the unimplanted ear in adult users of a cochlear implant. Journal of Speech, Language, and Hearing Research, 48, (3), 668-680.
Dunn, C.C., Tyler, R.S., Oakley, S., Gantz, B.J., & Noble, W. (2008). Comparison of speech recognition and localization performance in bilateral and unilateral cochlear implant users matched on duration of deafness and age at implantation. Ear Hear. 29, 352-9.
Durlach, N.I. & Colburn, H.S. (1978). Binaural phenomena. In E.C. Carterette, and M.P. Friedman (Eds.), Handbook of Perception, Volume IV. New York: Academic Press.
Gantz, B., Tyler, R., Rubinstein, J., Wolaver, A., Lowder, M., et al. (2002). Binaural cochlear implants placed during the same operation. Otology and Neurotology, 23 (2), 169-180.
Grantham, D.W, Hornsby, B.W., & Erpenbeck, E.A. (2003). Auditory spatial resolution in horizontal, vertical, and diagonal planes. J Acoust Soc Am., 114, 1009-22.
Laszig, R., Aschendorff, A., Stecker, M., Müller-Deile, J., Maune, S, Dillier, N., et al., (2004). Benefits of bilateral electrical stimulation with the nucleus cochlear inplant in adults: 6- months postoperative results. Otology and Neurotology, 25, 958-968.
Litovsky, R., Parkinson, A., Arcaroli, J., & Sammeth, C. (2006). Simultaneous bilateral cochlear implantation in adults: a multicenter clinical study. Ear & Hearing, 27, 714-731.
Middlebrooks, J.C., & Green, D.M. (1991). Sound localization by human listeners. Annual Review of Psychology, 42, 135-159.
Nilsson, M., Soli, S.D., & Sullivan, J.A. (1994). Development of the Hearing in Noise Test for the measurement of speech reception thresholds in quiet and in noise. Journal of the Acoustical Society of America, 95, 1085-1099.
Nopp P. & D'Haese P., (2004). Sound localization in bilateral users of MED-EL COMBI40/40+ cochlear implants. Ear & Hearing, 25, 205-214.
Rubinstein, J.T., Parkinson, W.S., Tyler, R.S., & Gantz, B.J. (1999). Residual speech recognition and cochlear implant performance: effects of implantation criteria. Am J Otol., 20, 445-52.
Schleich, P., Nopp, P., & Haese, P.D., (2004). Head shadow, squelsch and summation effects in bilateral users of the MED-EL COMBI 40/40+ cochlear implant. Ear&Hearing, 25, 197-204.
Shaw, E.A. (1974). Transformation of sound pressure level from the free field to the eardrum in the horizontal plane. Journal of the Acoustical Society of America, 56, 1848-1861.
Tillman, T.W. & Carhart, R., (1966). An expanded test for speech discrimination utilizing CNC monosyllabic words. Northwestern University Auditory Test No. 6 Technical Report No. SAM-TR-66-55. USAF School of Aerospace Medicine, Brooks Air Force Base, Texas.
Tyler, R. S., Gantz, B.J., Rubinstein, J.T., et al., (2002). Three-months results with bilateral cochlear implants. Ear & Hearing, 23 (Suppl 1): 80S-9S.
van Dijk, J.E., van Olphen, A.F., Langereis, M.C., Mens, L.H., Brokx, J.P. & Smoorenburg, G.F. (1999). Predictors of cochlear implant performance. Audiology, 38(2), 109-116.
Van Hoesel, R. J., and Tyler, R.S., (2003). Speech perception, localization and lateralization with bilateral cochlear implants. J. Acoust. Soc. Am., 113, 1617-1630.
Waltzman, S.B., Fisher, S.G., Niparko, J.K, & Cohen, N.L. (1995). Predictors of postoperative performance with cochlear implants. Ann Otol Rhinol Laryngol Suppl. 165, 15-8.
Yost, W.A., & Dye, R.H. (1997). Fundamentals of directional hearing. Seminars in Hearing, 17, 66S-77S.
Zurek, P.M. (1993). Binaural advantages and directional effects in speech intelligibility. In:Studebaker GA, Hochberg I, eds. Acoustical Factors Affecting Hearing Aid Performance. 2nd ed. Boston: Allyn & Bacon, 255-276.
Acknowledgement: This research was supported in part by research grant 2 P50 DC00242 from the National Institute on Deafness and Other Communication Disorders, National Institutes of Health;grant RR00059 from the General Clinical Research Centers Program, Division of Research Resources, National Institutes of Health;the Lions Clubs International Foundation;and the Iowa Lions Foundation. We would like to thank Beth MacPherson and Ann Perreau for all of their hard work and dedication to collecting data for this project.
New Methodologies for Determining if Two Cochlear Implants are Necessary
September 29, 2008
Share:
Related Courses
1
https://www.audiologyonline.com/audiology-ceus/course/singing-in-rain-using-music-22785
Singing in the Rain: Using Music to Reinforce Listening (Professionals)
Presented by Christine Barton, this course provides participants with additional approaches to using music for spoken language development in young deaf and hard of hearing children. A special emphasis on the use of songs that focus on listening and language development while a young child is playing in the water will be provided.
textual, visual
Singing in the Rain: Using Music to Reinforce Listening (Professionals)
Presented by Chris Barton, MM, MT-BC
Course: #22785Level: Intermediate1 Hour
No CEUs/Hours Offered
Presented by Christine Barton, this course provides participants with additional approaches to using music for spoken language development in young deaf and hard of hearing children. A special emphasis on the use of songs that focus on listening and language development while a young child is playing in the water will be provided.
2
https://www.audiologyonline.com/audiology-ceus/course/best-practices-for-cochlear-implant-33025
Best Practices for Cochlear Implant Candidacy: Pediatrics, in partnership with American Cochlear Implant Alliance
This course examines both the Food and Drug Administration and best-practice candidacy assessment practices for pediatric cochlear implantation. Medical, audiology, speech-language pathology, and other assessments and considerations will be discussed to help identify best practices for candidacy determination.
auditory, textual, visual
Best Practices for Cochlear Implant Candidacy: Pediatrics, in partnership with American Cochlear Implant Alliance
Presented by Denise Thomas, AuD, CCC-A, Lindsay Zombek, MS, CCC-SLP, LSLS Cert. AVEd
Course: #33025Level: Intermediate1 Hour
AAA/0.1 Intermediate; ACAud/1.0; AG Bell - LSLS/1.0 Domain 1; BAA/1.0; CAA/1.0; IACET/0.1; IHS/1.0; Kansas, LTS-S0035/1.0; NZAS/1.0; SAC/1.0
This course examines both the Food and Drug Administration and best-practice candidacy assessment practices for pediatric cochlear implantation. Medical, audiology, speech-language pathology, and other assessments and considerations will be discussed to help identify best practices for candidacy determination.
3
https://www.audiologyonline.com/audiology-ceus/course/implementation-cochlear-implants-enhanced-candidacy-37377
Implementation of Cochlear Implants: Enhanced Candidacy Criteria and Technology Advances
The participant in this course will understand the extended candidacy criteria with cochlear implantation and expectations. The course will cover implanting under age one, hybrid hearing with cochlear implantation, CI under local anesthesia, single-sided deafness, cochlear implantation, and auditory brainstem implantation.
auditory, textual, visual
Implementation of Cochlear Implants: Enhanced Candidacy Criteria and Technology Advances
Presented by J. Thomas Roland, MD Jr.
Course: #37377Level: Intermediate1 Hour
AAA/0.1 Intermediate; ACAud/1.0; AHIP/1.0; ASHA/0.1 Intermediate, Professional; BAA/1.0; CAA/1.0; Calif SLPAB/1.0; IACET/0.1; IHS/1.0; Kansas, LTS-S0035/1.0; NZAS/1.0; SAC/1.0
The participant in this course will understand the extended candidacy criteria with cochlear implantation and expectations. The course will cover implanting under age one, hybrid hearing with cochlear implantation, CI under local anesthesia, single-sided deafness, cochlear implantation, and auditory brainstem implantation.
4
https://www.audiologyonline.com/audiology-ceus/course/adult-assessments-in-hearing-healthcare-38660
Adult Assessments in Hearing Healthcare: Working Across the Continuum
This five-course series on adult assessments in hearing health is intended to stimulate collaborative approaches for hearing health professionals, regardless of what hearing technologies they typically provide. Ideally, professionals will support patients in their long-term hearing loss journey, facilitating transitions when appropriate and a comfortable sense of the range of ways hearing loss can be addressed throughout one’s hearing journey.
auditory, textual, visual
Adult Assessments in Hearing Healthcare: Working Across the Continuum
Presented by Camille Dunn, PhD, Susan Good, AuD, MBA, Alejandra Ullauri, AuD, MPH, Ted McRackan, MD, MSCR, Donna L. Sorkin, MA, Rene Gifford, PhD
Course: #38660Level: Intermediate5 Hours
AAA/0.5 Intermediate; ACAud/5.0; ASHA/0.5 Intermediate, Professional; BAA/5.0; CAA/5.0; Calif SLPAB/5.0; IACET/0.5; IHS/5.0; Kansas, LTS-S0035/5.0; NZAS/3.0; SAC/5.0; Tier 1 (ABA Certificants)/0.5
This five-course series on adult assessments in hearing health is intended to stimulate collaborative approaches for hearing health professionals, regardless of what hearing technologies they typically provide. Ideally, professionals will support patients in their long-term hearing loss journey, facilitating transitions when appropriate and a comfortable sense of the range of ways hearing loss can be addressed throughout one’s hearing journey.
5
https://www.audiologyonline.com/audiology-ceus/course/adult-perceptions-hearing-status-and-38407
Adult Perceptions of Hearing Status and Options: Professionals Facilitating a Life-long Hearing Journey, in partnership with American Cochlear Implant Alliance
Adults with severe-to-profound hearing loss utilizing hearing aids are typically not benefitting sufficiently from traditional amplification and often would benefit from hearing implants. This course will review ways hearing care professionals can support adult patients who may benefit from implants (either now or in the future) by presenting information on the cochlear implant (CI) option early in an individual’s hearing journey. A CI is not a last resort, but rather a means for those who fall within the guidelines to experience hearing improvement, rather than continued decline.
auditory, textual, visual
Adult Perceptions of Hearing Status and Options: Professionals Facilitating a Life-long Hearing Journey, in partnership with American Cochlear Implant Alliance
Presented by Donna L. Sorkin, MA
Course: #38407Level: Intermediate1 Hour
AAA/0.1 Intermediate; ACAud/1.0; AHIP/1.0; ASHA/0.1 Intermediate, Professional; BAA/1.0; CAA/1.0; Calif SLPAB/1.0; IACET/0.1; IHS/1.0; Kansas, LTS-S0035/1.0; NZAS/1.0; SAC/1.0
Adults with severe-to-profound hearing loss utilizing hearing aids are typically not benefitting sufficiently from traditional amplification and often would benefit from hearing implants. This course will review ways hearing care professionals can support adult patients who may benefit from implants (either now or in the future) by presenting information on the cochlear implant (CI) option early in an individual’s hearing journey. A CI is not a last resort, but rather a means for those who fall within the guidelines to experience hearing improvement, rather than continued decline.


