Editor's note: This is an edited transcript of a live webinar. Download supplemental course materials.
Learning Objectives
- Participants will be able to identify the CPT code/ICD9/ICD10 code combinations that require reporting of the audiology PQRS codes.
- Participants will be able to list the ICD10 deadlines.
- Participants will be able to identify the specific items contained in the OIG work plan that pertain to audiology.
Ordering Physicians
In today’s course on billing and coding, we will start first with ordering physicians.
Medicare requires a physician order and medical necessity for coverage of audiologic and vestibular services. The ordering physician must be enrolled in Medicare as either a participating provider, a non-participating provider, or an opt-out provider. Medicare has to know they exist and what their NPI (national provider identifier) number is. When you receive an order from a physician who is unfamiliar to you, you need to make sure this physician is properly enrolled in Medicare. If they are not properly enrolled and your claim is denied, the patient cannot be financially responsible for the cost, meaning that you will absorb the costs of any procedures. Here is a link to the most current list of enrolled physicians. I encourage you to look here for the referring physician prior to providing the test.
Hospital Outpatient Prospective Payment System
For those of you who work in hospitals, there is something called the Hospital Outpatient Prospective Payment System, or HOPPS. I will not going to go into detail about this specifically, but you need to know that certain services are bundled or packaged together with other services, even outside of audiology and vestibular, for that same date of service. It is important for you to know how the audiology services you provide in your hospital are packaged. If you would like more information, visit ASHA and AAA.
Certain services are not reimbursed separately if provided on the same day as other services because you are getting that package price. If you work in a hospital, you bill through OPPS, I encourage you to go to learn more about how your hospital packages services.
ICD-10
The bulk of what I want to talk about today is ICD-10. ICD-10 is slated to go into effect October 1, 2015. However, every week we hear something new, and the changes are ongoing. I think we will know more about ICD-10 implementation as we move through Spring.
The Medicare gap fix expires on March 3, 2015. If Congress does not act and either extend the gap fix or have a new Medicare bill, those large reductions in reimbursement (27% reductions) will go into effect. I think we should all assume that ICD-10 will go forward on October 1, but if you get a notification from your national associations, please read it. We will keep you up-to-date as to what is happening.
ICD-10 on October 1 will be a light switch change. This means that on September 30, you will use ICD-9, and on October 1, you will use ICD-10. Take a breath; it is not a big deal, just a new set of codes. Your super bill will need to update from ICD-9 to ICD-10. If you alphabetize codes instead of using the code number and you are able to search by condition, this means simply inputting or circling a new code.
There has been tremendous growth in our audiology codes. We had around 55 common audiology ICD-9 codes, and now we are up to about 153 with ICD-10. Most of those changes are because ICD-10 is now coded as right, left, and binaural, which has multiplied our existing codes.
Start your focus on ICD-10 in the Spring and Summer before October approaches. Look for available trainings or materials from the national associations of which you are members. Here are the links on this issue from AAA, ASHA and ADA. In addition, I will be presenting a one-hour webinar exclusively on ICD-10 on AudiologyOnline in the spring.
Differences Between ICD-9 and ICD-10
ICD-9 was about 14,000 codes. ICD-10 is closer to 69,000 codes. It has additional information and expansion of injury codes. The diagnostic and symptoms codes that we used to see that were V codes, such as a routine exam of ears and hearing (V72.19), has now moved into the regular code set.
Do these changes in ICD-10 mean that it is going to be reimbursed? No one really knows. We will see that as we start to get codes and process claims through the system. It is a code length now up to seven characters. There is greater specificity to the codes. The V and E codes are now in the regular seven character code sets, which are alphanumeric. Every letter of the alphabet is included, except for the letter U.
What Will You Need to Do?
You need to update your paper super bills, electronic medical record (EMR) and your office management systems to reflect ICD-10. Never assume that software vendors are going to do this for you, especially in the realm of audiology office management system. You may be loading your own codes, and that code set of most common codes is available from your national associations.
You are going to need a manual or software. There are some online options available that you can find through Google. However, be cautious, especially if you are typing in the old ICD-9 code to get the new ICD-10. Remember you are going from a smaller code set to a larger code set, and what you had before may not exist or may exist differently in the new set.
Search by description. For example if I was looking for an ICD-10 code for diabetes, I would search “ICD-10 diabetes.” I would not put the ICD-9 code in. I think everyone should make the purchase, especially this first year, of software access or a manual so that you do have the code sets easily and readily available to you in a reliable format so that you have the less common codes that still apply to your medical necessity. The Internet search option that tends to be most reliable is https://www.icd10data.com.
For those of you who have local coverage determinations, which is where Medicare guides coverage based upon certain diagnoses, you need to be aware of how the ICD-10 changes will affect those, as well as the Physician Quality Reporting System (PQRS). For PQRS information, go to www.audiologyquality.org. This is a one-stop shop where the 10 audiology quality consortium stakeholders manage the content, and you can get PQRS information and see the ICD-10 transitions there.
Your providers need to be trained, not your front office staff or billing staff. No one should be coding anything other than the provider unless they are a certified coder. I cannot stress that enough. All of the audiologists in your practice need to be trained on ICD-10. You are the ones who will be seeing these patients and selecting what best represents the diagnosis and medical necessity for why you have done what you have done. Here is a link to ICD-10 information and training materials from Centers for Medicare & Medicaid Services (CMS).
Local Coverage Determinations
I want to bring in local coverage determinations. The local coverage determinations that exist today in audiology are shown in Figure 1. Below each covered determination is the Medicare Area Contractor to which it applies. If you have difficulty, you can go to the Medicare Area Contractors, which are the people who process Medicare claims in given areas. It is important for you to know, because when a local coverage determination is in place, you need to have an Advance Beneficiary Notice of Noncoverage (ABN) signed prior to providing the service. You cannot guarantee you are going to have an acceptable diagnosis for coverage until after you have performed the procedure.
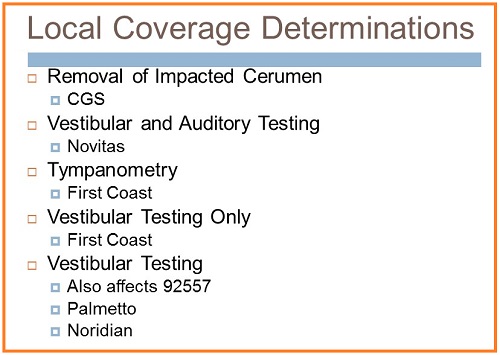
Figure 1. Local coverage determinations.
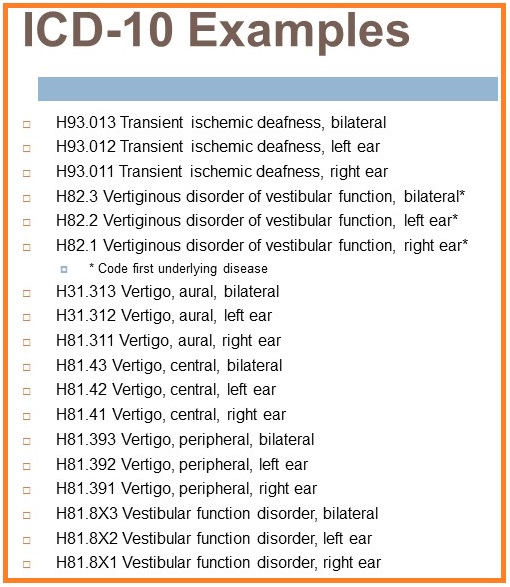
Common ICD-10 Audiology Codes
The following list (Figure 2) highlights several ICD-10 codes you may use. I am not going to discuss each code, but I will highlight some important ones.
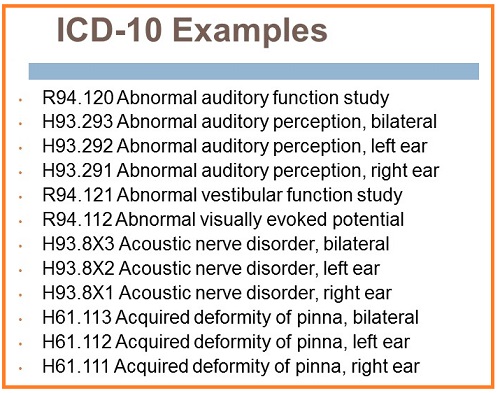
Figure 2. ICD-10 Examples.
Abnormal auditory perception is a diagnosis code I would use when a patient presents to you saying, “I am having trouble understanding,” or “I am hearing things differently than they are being said,” and their hearing test is normal. To me, this code is, in some ways, a precursor to additional testing to rule out auditory neuropathy, an auditory processing disorder or cognitive decline. It is the middle road until you are able to do more testing.
You may also see an acoustic nerve disorder, which is essentially an acoustic tumor or neoplasm. You can use abnormal auditory perception for this condition as well. More examples can be seen in Figure 3.
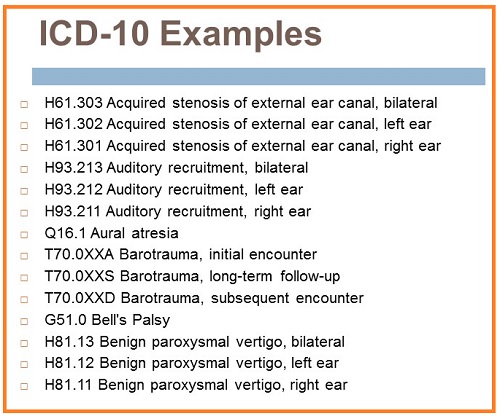
Figure 3. More ICD-10 examples.
Stenosis is a code that we did not have before. Acquired stenosis of the external auditory canal would be for a patient that has collapsing canals. There is now also a code for barotrauma and the different encounters. Initial encounter is the first time you see a patient for the condition. Subsequent encounter is the second time you see the patient for the condition. Long-term follow-up is the third visit and on for that condition. There is also a code for benign paroxysmal vertigo (BPPV) and Bell's palsy.
The next group of codes I would like to point out can be seen in Figure 4.
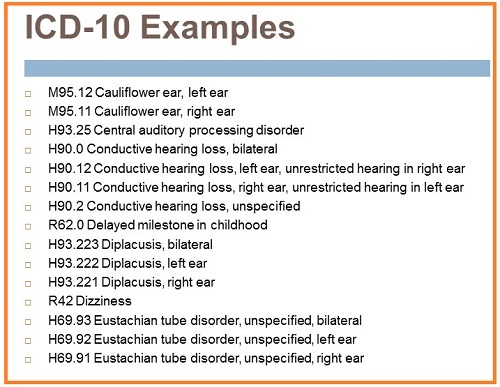
Figure 4. ICD-10 codes - examples.
Let's talk about the conductive hearing loss and the term “unrestricted hearing.” The ICD-10 code set is not perfect. The problem is that leadership in national associations or in coding/reimbursement cannot submit for any changes until 2017. We are going to have to live with this code set as it is for right now. “Unrestricted” means normal hearing in the opposite ear. Conductive hearing loss, left ear, unrestricted hearing in the right ear means conductive hearing loss in the left ear with normal hearing in the right ear.
What happens when the patient has conductive hearing loss in one ear and a mixed hearing loss in the other? In the opposite ear that has a different type of hearing loss, you would conductive hearing loss, unspecified for one ear, and mixed hearing loss, unspecified for the other. There is no other way to code differing hearing losses. You have to diagnose both. That is an important distinction that we need to make.
Delayed milestone in childhood is a great diagnosis code for use by audiologists. A parent presents to you saying, “My child is not talking. They are developmentally delayed.” That means they are not meeting their milestones. That would be great rationale for medical necessity, especially when the outcome is normal hearing. Diplacusis and dizziness are other codes. We also now have a code for Eustachian tube disorder. The unspecified code is used if you do Eustachian tube function testing and it is abnormal.
You will notice exostosis in this group of codes in Figure 5. Currently, family history of hearing loss and feared complaint are ICD-9 V codes. They have changed to Z codes in ICD-10, and I would caution people about using Z codes, as they should only be used when no better option exists. You should not be using rule-out diagnoses once you know a patient does not have that condition. For example, if a patient is referred you for suspected conductive hearing loss and you find normal hearing, you should not be using conductive hearing loss as your diagnosis, because you know they do not have it. If anyone would like documentation of that rationale, I can provide that to you.
There is a great breadth of guidance from payers that they do not want rule-out diagnoses. Once you know that someone does not have a condition, you should not be using that diagnosis. You should be using what they actually present with. Sometimes we code for what exists, not for coverage. We code to represent, because this data is used for etiology and prevalence. You are misrepresenting the prevalence of conditions if you are coding something that does not exist. Use these Z’s or V’s in ICD-9 only when you do not have a better option and you cannot guarantee a patient that there will be coverage.
You will also see a code for a foreign body in the ear with initial or first encounter and subsequent encounter.
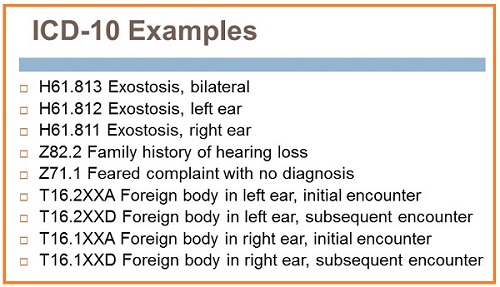
Figure 5. ICD-10 codes - exostosis, Z codes and other examples.
The Z codes in this next group include hearing conservation and treatment and hearing examination following failed hearing screening (Figure 6). This code was desired by many, but remember that you do not know what insurance will do with these codes for coverage. Z01.10 is normal hearing or normal vestibular function. I would avoid the use of this if the patient reported dizziness or tinnitus or you found a hearing loss. Use abnormal auditory perception if they are having documented trouble understanding but the hearing test is normal. Use any other code that would be applicable and justifiable over coding normal hearing.
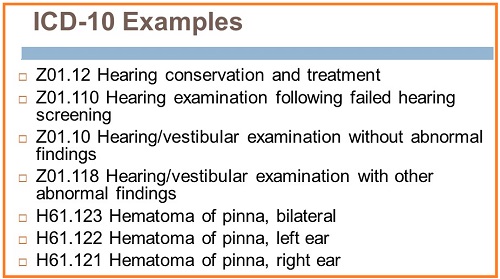
Figure 6. ICD-10 codes related to hearing conservation and treatment and hearing examination following failed hearing screening.
The code Z01.118, hearing/vestibular examination with other abnormal findings, may mean that you found something else abnormal in the patient, but it was not necessarily abnormal hearing or vestibular examination. Maybe you felt a growth on their ear. Maybe you found that they had breathing difficulties or that they were depressed.
Just as in ICD-9 where we use V codes with caution, the same thing applies in ICD-10.
There are codes for hyperacusis and impacted cerumen in this next group (Figure 7). Impacted cerumen has a very clear definition. It is cerumen that is blocking clinically significant portions of the eardrum. It is hard, and requires tools or irrigation to remove it. The little brown ball that is sitting in someone's ear that you need removed so that their hearing aid does not get clogged is not impacted and should not be coded as such. Notice that Meniere’s is not as it is ICD-9. It is straight Meniere’s disease with no distinction between active and inactive.
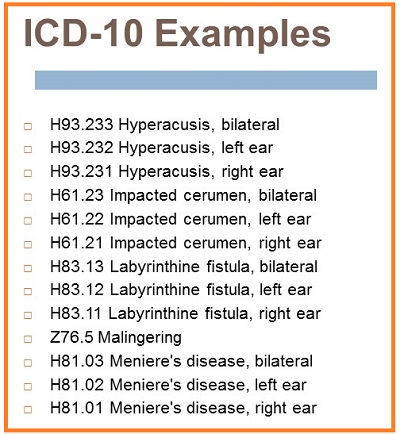
Figure 7. ICD-10 codes for hyperacusis, impacted cerumen, and others.
Included in this next set (Figure 8) are mixed hearing loss, unspecified, for when you have different hearing losses each ear later. Noise effects on the inner ear may be due to a noise trauma. There are also codes for noninfective disorders of the pinna, as well as general nystagmus.
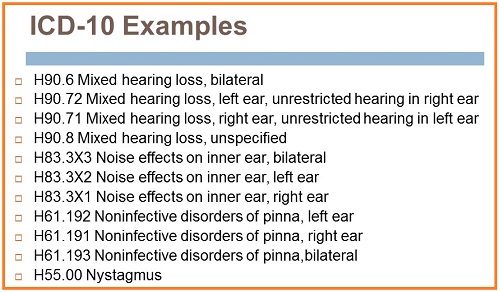
Figure 8. ICD-10 codes for mixed hearing loss, and others.
The codes for otalgia, otorrhagia, otorrhea, and perforation of the eardrum now all have right, left and bilateral markers (Figure 9).
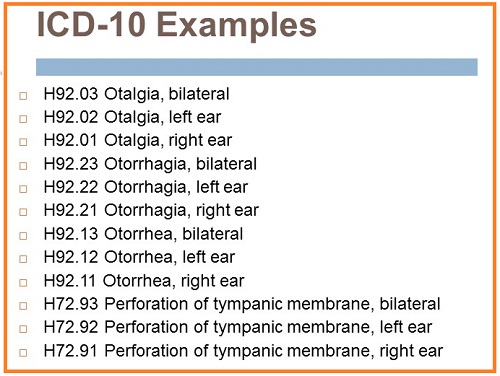
Figure 9. ICD-10 codes for otalgia, otorrhagia, otorrhea, and perforation of the eardrum.
Let's talk about ototoxicity. This is the biggest departure for audiology by far. You not only need to code in which ear the toxicity occurred, but you also need to code the toxin. This is a great complement to documentation of current medications in PQRS. In Figure 10, you will see there is a code for the initial encounter, subsequent encounter, and long-term follow-up, and then you are going to see the ototoxicity. You would need two codes to code ototoxicity: which ear(s) is ototoxic and the toxic agents.
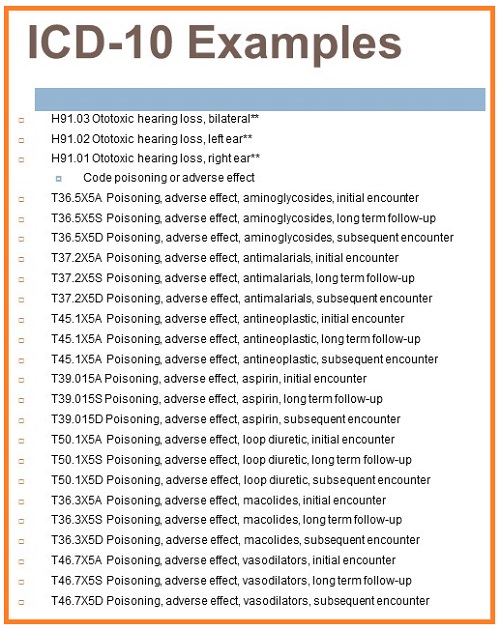
Figure 10. ICD-10 codes - ototoxicity.
There are codes for sensorineural hearing loss and sensorineural hearing loss - unspecified, speech language delay due to hearing loss, sudden hearing loss, temporary threshold shift, and tinnitus (Figure 11). Tinnitus is not classified as subjective or objective in ICD-10.
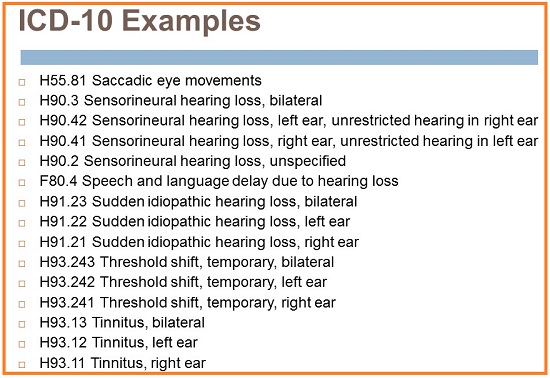
Figure 11. ICD-10 codes for sensorineural hearing loss and sensorineural hearing loss, unspecified, speech language delay due to hearing loss, sudden hearing loss, temporary threshold shift, and tinnitus.
Transient ischemic deafness is another code in vertiginous disorder of vestibular function, and with it you code the underlying disease. Let’s say a patient has Meniere’s. You could code vertiginous disorder of vestibular function with the underlying disease as Meniere’s that results in the vertigo. There are different types of vertigo (aural, central and peripheral), as well as a vestibular function disorder. You can see the relevant codes in Figure 12.
Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) Changes
There are no CPT or HCPCS code additions or modifications for 2015. I do need to state that a CPT Assistant article was released in August 2014 that defined audiology code sets. CPT Assistant is the publication of the American Medical Association (AMA). For those of you do not know, the AMA owns the CPT code set and their use; we lease them for use in healthcare. The AMA, with the assistance of many stakeholders, including audiologists, writes guidance called CPT Assistant. That guidance is the definitive source on code use throughout healthcare.
For example in 2011, CPT Assistant said that VEMPs should be coded using the unlisted 92700 code. They said when doing neurotelemetry for a cochlear implant that you should use the ECOG code of 92584. They have now given coding guidance on the entire audiology code set, but the points that are most different are for visual reinforcement (VRA) and conditioned play audiometry (CPA). “VRA is a test technique that can be formed using either loudspeakers or earphones which uses flashing lights, moving toys or video to reinforce a head turn response to sound stimuli, and it may be used with either tonal or speech.” That means if you are using VRA under headphones or in the sound field for tones or speech, it is a single code. You do not add another code to this. This is a single code because they have defined this as such. This will encompass multiple different modalities now.
Conditioned play was also defined as “a test technique in which the patient is taught a game that requires a response to tonal stimuli. A variety of play responses can be used with conditioned play audiometry, such as dropping a toy in a container or putting pegs in the board. It is typically done using earphones.” You will notice that is tonal only. If speech is also testing with conditioned play, that would be a separate code. Speech awareness or speech reception is 92555. If you are doing word recognition, it would be 92556. If they are pointing at any pictures for either spondees and/or word recognition using an NU-CHIPS or WIPI (Word Intelligibility by Picture Identification), you would also add select picture, which is 92583. The CPT Assistant redefined the code set for us, and we need to be aware of those coding changes.
-59 Modifier
A -59 modifier is used in situations where you are providing one or two aspects of a bundled code, such as 92557 (Comprehensive audiometry threshold evaluation and speech recognition) or 92540 (basic vestibular evaluation, bundled). It is those two situations where a -59 modifier would be warranted.
Many of you may have heard that new X modifiers that are to replace the -59 modifier. We all agree in audiology that the X modifiers are not appropriate for audiology services. We recommend that those of you using the -59 modifier continue to use it, and do not use the X modifiers.
PQRS
The Physician's Quality Reporting System (PQRS) is a program designed to improve the quality of care to Medicare beneficiaries. We have audiology-specific PQRS information, and our website is www.audiologyquality.org. If you bill traditional Medicare Part B, you need to be reporting PQRS in 2015 or you will have a 2% pay reduction in 2017. It does not apply to Medicare Advantage, hospital or skilled nursing.
I encourage those of you who work in hospital settings or group practices to contact your practice administrators and determine what your PQRS responsibilities are. A lot of people did not ask in 2013 and are being penalized now as a result. Those of you who work in smaller entities and bill Medicare Part B, you need to be reporting PQRS. Eventually, we will not get paid without reporting quality.
PQRS Measures for Audiology
The reporting for 2015 is identical to the 2014 reporting, in order to avoid the penalty, but there are no more incentives now. We have three measures to report in 2015: Measure 261 (referral for otologic evaluation for patients with acute or chronic dizziness), Measure 130 (documentation and verification of current medications in the medical record), and Measure 134 (screening for clinical depression in a follow-up plan of care).
Reporting that you did not do something, that you did not document current medications, that you did not refer for dizziness, or that you did not perform a depression screen, is just as if you did not report it at all. We must report a positive action, such as a referral, documentation or screening, for the reporting to count and to assist in avoiding the penalty. You cannot report that you did not do something.
The depression measure is still optional as long as you are reporting the medication measure. If you report the medication measure, then you do not need to report the depression measure. You have to report dizziness; that is a measure in our wheelhouse. It has to be a positive action that you documented medications or that you referred that patient.
Referral for Acute or Chronic Dizziness
Any time you perform any of these procedure codes below and have a diagnosis of dizziness or BPPV, you must report this measure. CPT Codes include: 92540, 92541, 92542, 92543, 92544, 92545, 92546, 92547, 92548, 92550, 92557, 92567, 92568, 92570, 92575. Patients that have any of these CPT codes, as well as the ICD-9 codes 780.4 or 386.11, fit into the measure’s denominator, or are eligible patients for a measure.
There are three ways you can report referral for dizziness:
- G8856: Referral to a physician for otologic evaluation;
- G8857: Patient is not eligible for the referral for otologic evaluation (e.g., patients who are already under the care of a physician for acute or chronic dizziness);
- G8858: Referral to a physician for an otologic evaluation not performed, reason not specified. This means that you did one of those procedures and you diagnosed dizziness, but you did not refer the patient. It would be a negative reporting, and that is not going to count towards avoiding the penalty.
Documentation of Current Medications
Any time you perform the CPT procedures below, regardless of the diagnosis, you need to be documenting current medications. These codes include: 92541, 92542, 92543, 92544, 92545, 92547, 92548, 92557, 92567, 92568, 92570, 92585, 92588, 92626. Patients that have any of these CPT codes with any ICD-9 code fit into the measure’s denominator (the eligible patients for a measure).
The measures for reporting current medications are:
- G8427: List of current medications (includes prescription, over the counter, herbals, vitamin/dietary supplements) documented by the provider, including drug name, dosage, frequency, and route;
- G8430: Provider documentation that the patient is not eligible for medication assessment;
- G8428: Current medications (includes prescription, over the counter, herbals, vitamin/dietary supplements) with drug name, dosage, frequency, and route partially or not documented by provider, reason not specified.
For G8427, it is important for you to select that code when you have those drugs documented and you have the four conditions documented. G8430 may be for an emergent situation. Perhaps they have dementia and come unaccompanied or they are not native English speakers and they do not understand what you are asking them without a translator. That means you would not be eligible.
If you have a senior citizen that does not take any medications, you would still use G8427, because you have documented that they do not take any medications. G8428 is not your positive reporting. It means that you did not document the patient's current medications and their drug name, dosage, or frequency, and the route is partially or not documented. A lot of audiologists in dispensing offices or those that do not perform vestibular or electrophysiologic testing ask why they need this. This is about being able to look at your whole patient diagnose her condition. Do they have ototoxicity that is contributing to their hearing loss or dizziness? Can you look at your patient as a whole? It is about patient care and having a clinical focus.
Many patients now carry their list with them. Do not forget when scheduling this patient to remind them to bring a list of current medications, and do not forget to ask about the list at intake. For those of you who are in a hospital or medical environment, all you need to do is pull up their list of medications that was last listed in the EMR, go over them with the patient, and document that they have been updated. The same goes with the list the patient gives to you. Go over it with the patient, sign and date it to document that it has been confirmed. I like having a space on the patient intake form for people to list their current medications and ask about frequency, route, drug name, and dosage.
Clinical Depression Screening
Remember that this code is optional. It only now applies in 2015 to the tinnitus assessment, regardless of the diagnosis. The CPT code included is 92625. No ICD-9 codes are specified, so all are included. Patients that this CPT code are eligible patients for this measure.
You will report on Measure 134 when it is allowed by your state licensure law and when deemed within your scope of practice in your state by written contact with your state licensure board. Second, if this is within your scope of practice, you should be appropriately trained and competent to perform the depression screening using a standardized tool and you must be comfortable creating a plan of care based upon the result of that screening. Third, that when that plan of care is created and implemented, it is fully documented in the medical record.
The codes for screening for clinical depression are:
- G8431: Positive screen for clinical depression using an age appropriate standardized tool and a follow-up plan documented;
- G8510: Negative screen for clinical depression using an age appropriate standardized tool and a follow-up plan documented;
- G8433: Screening for clinical depression using an age appropriate standardized tool not documented, patient not eligible/appropriate;
- G8432: No documentation of clinical depression screening using an age appropriate standardized tool;
- G8511: Positive screen for clinical depression using an age appropriate standardized tool documented, follow-up plan not documented, reason not specified.
The last two codes, again, are not positive outcomes. Either you did not screen or you have a positive screen but you did not create a follow-up plan of care. I would avoid any negative outcomes, because they will not help you avoid the penalties, and they are not good outcomes for the patient.
Submitting PQRS
You can submit PQRS via the CMS 1500 (837 format) or its electronic equivalent. You can learn more and see sample forms at www.audiologyquality.org. The diagnosis codes are placed in box 21. CPT codes are placed in the CPT HCPCS column of 24D and the G PQRS codes are placed below the procedure codes in box 24D.
Avoiding the Penalty
To avoid the penalty, you need a report at least on 50% of eligible patients. In a nutshell, you report dizziness on at least 50% of your Medicare claims, which you diagnosed as dizziness or BPPV. You need to report on documentation of current medications at least 50% of the time. I would not recommend trying to play the numbers. The documentation of current medications is 50% of each provider’s medical claims if you do a hearing test, calorics, tympanograms, and auditory brainstem response (ABR), comprehensive otoacoustic emissions (OAEs), and/or cochlear implant testing. You need to be documenting current medications.
The incentive programs have ended and all that is left are penalties. The appeal period has ended for those who received a penalty in 2013. We will find out what 2014 penalties are in December 2015, but my goal is to deal in the here and now and help you avoid penalties moving forward.
Penalty Letters
If you received the penalty letter, all of your Medicare claims for 2015 will be reduced by 1.5%. That is a combination of your NPI and your tax identification. It would not follow you to another employer. If in 2013 you did not meet your one measure and you still work for the same employer, you will be penalized. If you work for different employer, you will not be penalized.
If you are nonparticipating provider and you received a penalty letter, you need to reduce the amount you collect in your limiting charge. Your Medicare Area Contractor website has all the fee schedules available; those will tell you what your new limiting charge will be if you received the penalty and are nonparticipating. You can look at your PQRS participation status on QualityNet to see if you are reporting or not. Many people felt like they had been putting things on their super bill or in their EMR, but it did not get transferred to their claims. This will allow you to check on your PQRS reporting status for the current year.
Looking Ahead to 2016
In 2016, we will likely be adding the cost-cutting measures of smoking cessation. What that means is that you need ask your patients if they smoke, and if they say yes, you give them a brochure that tells them to not smoke. It can be that simple.
Falls risk assessment and plan of care is a very complicated measure. In short, we will be asking patients if they have fallen more than twice and if those falls resulted in the need for medical attention. This is another area where we will refer people and create a plan of care when a patient has had two or more falls requiring medical attention.
Medicare Fee Schedule
The Medicare fee schedules for 2015 are valid until the end of March. Audiologists have already seen a reduction in reimbursement from their 2014 rates for the vestibular code family, because those codes were surveyed and revalued when billed individually; the bundle was unaffected. Pay attention to your national associations to see what will happen to the Medicare fees schedule as the year starts to go on.
Medicare Advantage
Except for Medicare Advantage HMO's, most Medicare Advantage plans do not require a physician order this year. I strongly advise you to consult each plan to determine their specific requirements. What does exist in Medicare Advantage is that ABNs are not applicable and are inappropriate for Medicare Advantage. They have their own process called pre-service organization determination. You may need pre-service organization determination from a payer prior to performing a service or dispensing an item. What they require to be predetermined can vary. For some payers, anything that is not covered, such as a hearing aid, could require pre-service organization determination if you are an in-network provider for that Medicare Advantage plan. You need to consult each payer for their guidance on pre-service organization determination for 92700, L9900, V5298 and V5299, as this varies by state insurance laws and individual payers.
Medicare Data
When my colleagues and I were trying to find audiologists to participate in our PQRS testing, we had to start Googling people, because we needed to know if there was more than one audiologist in a facility. Now that Medicare has had their data dump, there is a lot of information available about you on the Internet and how many claims you submitted and for how much and how you compared to the national average. That data is going to become more prolific.
I strongly encourage you Google yourselves. Many of you will find that your Medicare claims data is available online to consumers, and the degree of disclosure depends on how much they want to data mine. You can find some of this data through the SMC. There is also the Medicare website, Physician Compare, which will ultimately house detailed PQRS information about how much you report and the quality of your practice. As time goes on, more and more data is going to be housed there for public viewing and dissemination.
Conclusion
While there is much changing this year for audiology and the way we file claims and bill for reimbursement, it is not an insurmountable task. We need to pay attention and proactively inform ourselves of the changes that will directly affect our clinics. The professional organizations will be a good source of information as these rules evolve.
Questions and Answers
Can you use the code for unrestricted hearing if there is a high frequency hearing loss which does not affect the patient's speech perception?
How would you describe that in your documentation? If you would describe it as a hearing loss in the other ear, even though it is not aidable, I would not use the unrestricted code. If you are not going to describe it or document it as a hearing loss, then you could use unrestricted hearing.
A training I took by an audiology professional association on ICD-10 said to use the rule-out codes, which you said not to use. Which is correct?
I would be happy to send you guidance for Medicare that tells you not use rule-out diagnosis codes. All I can say is what I know. I will tell you that my colleagues at the professional associations do not talk about rule-out codes, and they stopped talking about rule-out codes about nine years ago. Was it a recent presentation that you saw? Remember that things change the world of coding reimbursement every year. That is why we provide resources and regular updates for audiologists.
Is a physician referral required for an audiologist to remove ear wax?
No. Removal of earwax is statutorily excluded from coverage if provided by an audiologist. Because there is not coverage involved, the physician order is not required. As long as it is within your scope of practice as an audiologist in your state to remove cerumen, you do not need a physician order, and you can bill the patient privately for cerumen removal.
What would our situation be if we have not filed for Medicare up to now? Most of our patients are private pay or their insurance pays a portion of our services.
Audiologists cannot opt out of Medicare. We are mandatory claims submitters. When you are seeing people who are Medicare eligible, you have three choices. You can be enrolled in Medicare as a participating provider, you can be enrolled in Medicare as a nonparticipating provider, or you can give all your testing free to every patient you see, regardless of age. There is not a fourth option where we can opt out and enter into private contracts and have patients pay privately for testing. Medicare beneficiaries have the right to access their benefits.
When a patient sees the physician and audiologist on the same day and the physician records current meds or updates the meds, does the audiologist also need to document this also in the note?
Yes. Remember on the Medicare claim, the audiologist is the rendering provider. We should not be billing incident to. Because of that, you need to write in the audiologist documentation that you have reviewed and confirmed current medications.
Do hospital-based audiologists who bill audiological services to Medicare Part B have to participate in PQRS?
Maybe, and that is why I indicated that those working in a hospital or large medical group need to reach out to the administrators and compliance officers to see what the reporting requirements are. Is your facility in a group reporting option? If so, what kind of group reporting option? Some require an audiologist to report; some do not.
Cite this Content as:
Cavitt, K. (2015, May). Billing and coding: 2015 update. AudiologyOnline, Article 14038. Retrieved from https://www.audiologyonline.com.