This text course is an edited transcript of an Otometrics/Audiology Systems webinar on AudiologyOnline.
Learning Outcomes
After this course, participants will be able to:
- Discuss ways to implement teleaudiology into their practice.
- Describe the types of evaluations that can be performed with teleaudiology.
- Describe the technology needed to initiate a teleaudiology program.
What is Telehealth/Teleaudiology?
The Health Resources and Services Administration, Federal Office of Rural Health Policy defines teleaudiology as follows:
The use of electronic information and telecommunications technology to support and promote long-distance clinical health, patient and professional health-related education, public health, and health administration. Technologies include videoconferencing, the internet, store-and-forward, streaming media, terrestrial and wireless communications.
In this course, we'll take a look at some delivery models of telehealth, discuss a few successful programs delivering teleaudiology and review some of the technology that makes the delivery of teleaudiology services possible.
Goals of Telehealth
One main goal of telehealth is to improve access to specialty care, especially in rural areas, or other areas that are not easily accessible. Someone who needs care may live a great distance away from the nearest hospital or clinic. In addition to distances challenges, there may be access-related challenges. For example, it is 30 miles from the south side of Chicago to the north side, but the trip could take you 90 minutes due to traffic. In addition to improving access, we want to reduce the time spent in travel, for both the patient and for the clinician. Another benefit of telehealth is to reduce the amount of time patients have to take off of work, which will ultimately reduce travel expenses.
Since licensing and billing varies so much by state to state, rather than devote time during this presentation, I am going to refer you to the Center for Connected Health Policy (CCHP) website. The CCHP is the federally designated National Telehealth Policy Resource Center. They are a nonprofit, nonpartisan organization and they have listings of regulations and policies for each state. As a basic rule of thumb, if you are performing teleaudiology services in more than one state (i.e., if you are crossing state lines), you should be hold a license for any of the states in which you practice.
Current Practices in Telehealth
The current methods of delivering care via telehealth are: store and forward, remote monitoring (asynchronous), mobile health and live interaction (synchronous).
- Store and Forward: Images, scans (X-rays) are taken and sent to off-site to a provider for review and interpretation (e.g., radiology, dermatology).
- Remote Monitoring (Asynchronous): Self-monitoring; self-testing of chronic diseases for later review (e.g., diabetes mellitus, cardiovascular disease, data logging in hearing aids).
- Mobile Health: Mobile clinic in a truck; we take the clinic to the patient.
- Live interaction (Synchronous): Real time, face-to-face interaction with patient and caregiver.
For the purposes of this presentation, we're going to spend most of our time looking at mobile health and live interaction (synchronous delivery) of teleaudiology services, because these methods are the most relevant for audiologists.
Mobile Health
Clinic in a Box (Truck)
Figure 1 is a diagram of a large truck that was designed to house a mobile audiology clinic. It contains two audiology suites, one large booth and another smaller booth. It has some bump-outs. This is a good way to bring the clinic to the patient.
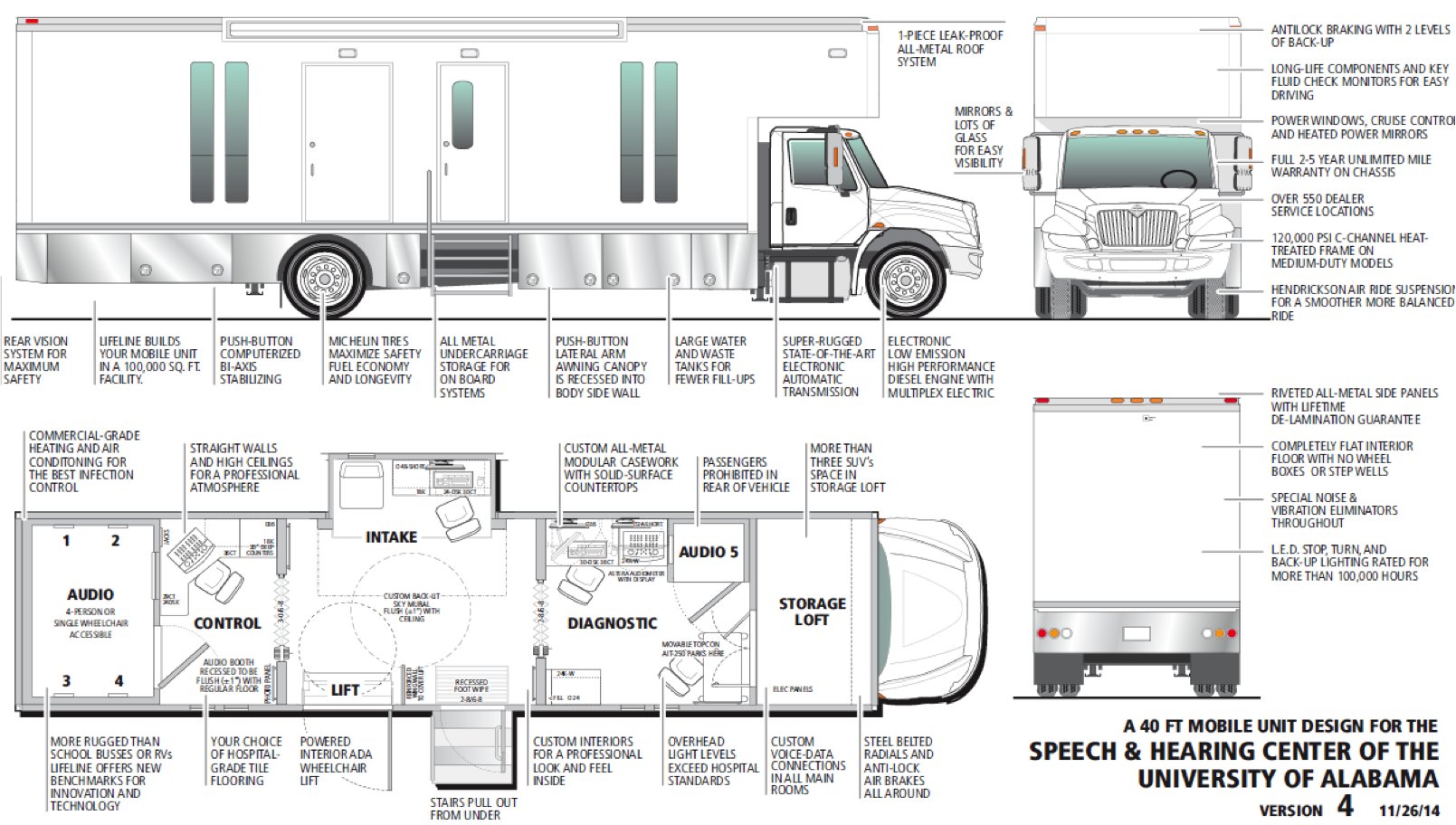
Figure 1. Clinic in a box (truck).
The University of Alabama has a program called Hear Here Alabama! They have a truck that they are currently using for running a rural hearing health study (Figure 2). Their original outreach was to underserved communities. They also take the truck to health fairs. I would encourage you to visit their website. It's quite impressive what they are able to achieve with that truck.

Figure 2. Hear Here Alabama! Truck.
Inside, the truck functions as a regular audiology clinic, only on a much smaller scale. The larger of the two booths (Figure 3) has a typical audiology setup with Video Otoscopy, Astera Audiometer, OTOflex Tympanometer, AURICAL probe microphone measurement (PMM) and AURICAL hearing instrument test (HIT) box. They're able to do hearing aid verification via the AURICAL Real Ear system. In the future, they hope to have internet on the truck, so when they encounter a situation, (e.g., with video otoscopy), they could contact a local ENT to evaluate the patient remotely. In that case, it would be a combining of two delivery types. Right now, it is a completely contained mobile audiology clinic, delivering the same level of service as you would expect in a brick and mortar clinic, except that they are able to bring hearing care services to the local community.
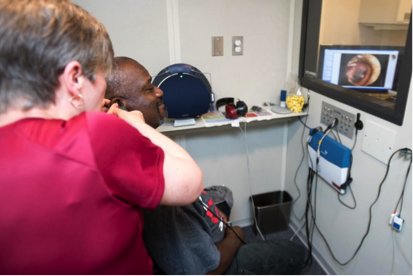
Figure 3. Large booth in the truck.
From the inside, it looks like a standard clinic. In the smaller booth (Figure 4), they have a typical setup with the video otoscopy, tympanometry, and an AURICAL audiometer. They have a hearing aid lab in here as well. The smaller booth is strictly used for testing adults. It may appear to be a small space; however, it is relatively spacious inside for the patient.

Figure 4. Smaller booth.
The truck catches people's attention as it drives down the street. The two providers (JoAnne Payne and Marcia Hay-McCutcheon) were each required to obtain a commercial driver's license (CDL) to drive this rig, which is a small price to pay to be able to deliver services remotely.
Mobile Apps
Using mobile apps for telehealth is becoming much more commonplace. If you download any number of apps, you will be connected with a physician and be able to interact with them real-time (synchronous). Although the apps may be free, there is usually a cost to be seen by the physician. However, it may be worth it to you, especially being able to avoid traveling across town with a sick child and sitting in an Urgent Care waiting room. You can be diagnosed from the comfort of your own home. Clearly, there will be situations where a virtual doctor visit might not be appropriate; it's certainly no substitute for the emergency room. For smaller things, though, it is a nice alternative to have that option.
Recently, an iPad audiometer has been approved. It is available by purchasing a license key through MelMedtronics (a medical device company specializing in developing iOS mobile applications). Both the patient and the audiologist each download an app, and they are able to have a synchronous interaction. This option may not be for everyone, because a patient does have to be somewhat tech savvy to operate the app. If they are not well-versed with technology, there needs to be a care giver present who can facilitate the online exchange. This is a standard audiometer. It uses recorded speech for delivery of speech information, and speech testing. Both the patient and the audiologist can see each other. The audiologist has immediate feedback as to how the patient is responding.
This next image is a snapshot from a program at the University of Texas at Austin (Figure 5). In this picture, they are communicating real-time with the University of Texas Health Science Center at San Antonio. Similar to the University of Alabama’s program, their goal is to improve healthcare of at-risk populations. This is essentially a “clinic on a cart.” Everything is contained: it has an AURICAL audiometer, an Otoflex tympanometer, and Video Otoscopy. It has the ability to do fitting verification; it has a HIT Box. At the top of the monitor, you can see a very high tech camera; that camera can be controlled by the audiologist remotely. They can zoom in; they can pan out. It's a little hard to tell, but on that screen, you can see the audiologist, and in the lower right hand corner, you can see what you are broadcasting to the audiologist.

Figure 5. Clinic on a cart.
The clinic on a cart model is an effective way to deliver services. The reason this equipment works is because the computer on the cart is using the OTOsuite software, and the audiologist at the far site can take control of that audiometer.
The next image may be easier to see (Figure 6). This is the CODEC, which is a piece of high-tech equipment that will allow you to communicate with your patient. In this situation, they are using the CODEC; there is a camera at the top of it (monitor on the left). The software is what gives you the ability to control the testing at a distance.

Figure 6. University of TX audiology telepractice project using the CODEC.
In Figure 7, you can see a better image of the CODEC. In the lower right corner, you can see the person on the other end of the camera. They are fitting the hearing aid, doing some real ear measurements, all through the supervision of an audiologist.
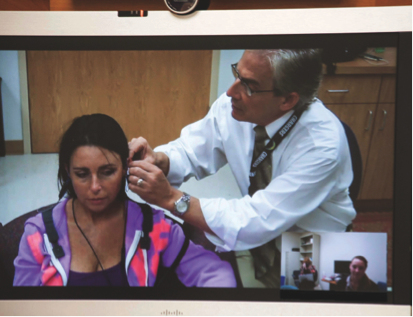
Figure 7. Teleaudiology using the CODEC.
The clinic on the cart includes the AURICAL audiometer, video otoscopy, the AURICAL PMM (which is the real ear system), the HIT box and the tympanometer. The reason this model works is because the audiologist is able to take control of the computer and test the patient as if they were physically in the same room.
Considerations for Live Interaction
What is required to be able to facilitate a live interaction with a patient?
- Reliable and high-speed internet service on both sides: You don’t want to get bogged down in the middle of a consultation.
- Technology needs.
- Space Needs: You will need a quiet space to deliver these services.
- Support Personnel: Who is going to be the hands of the clinician on the other end with the patient?
- Training for Support Personnel.
- Licensure: If you are crossing state lines, you must be licensed in each of those states.
- Reimbursement: As per the American Academy of Audiology website, current Medicare regulations do not include audiologists or speech pathologists as eligible providers for telemedicine. If you're billing Medicare, you cannot bill them for telemedicine or teleaudiology; however, you can still bill them for a regular visit.
Delivering Service
Let's think about the logistics of how we are going to deliver these services remotely, in terms of our eyes, hands, voice and ears. As an audiologist, you need to consider who is going to help facilitate the interaction at the remote site.
- Eyes: You need to be able to see the patient, so you need a video connection. At a minimum, you need one good camera, but two cameras are ideal: one camera to be able to see the room, and one camera for the audiologist to zoom in on different things. If you are sharing the space or the system with another professional (e.g., a speech pathologist), you might want to consider more closely what video you are going to use.
- Hands: You need to be able to take control of the PC screen and the software. Also, you need to train your personnel on what to do in an actual situation, as if you had the patient in the clinic.
- Voice/Ears: You need to be able to talk to the patient, and both the patient and the audiologist need to clearly hear the back and forth interaction.
Eyes: Video. You can get started with an inexpensive web camera. However, a high-end, wide angle 1080p camera with Far End Control would be ideal. You don't lose as much clarity, you're able to clearly see the patient and, as such, you have a better feel for the patient. Again, consider your needs. Do you need the ability to move the camera? Do you need an ultra-high resolution video to get started? Maybe you don't.
Hands: Controlling the PC/Audiometer. The reason this works is because the audiometer is on the patient side, controlled by software. The audiologist at the far side can take control of the computer to manipulate the audiometer, and test the patient. There are several vendors that offer services to allow a remote party to take control of your computer. These include: LogMeIn, WebEx, Lync Server and Skype. The problem with Lync or WebEx is that they may not have good audio; whereas if you use Outlook (if you already have Outlook through your work setting) you can share your screen with each other. Outlook or Skype are good options to use, because they have audio, and you can use an auxiliary microphone, or set of headphones with a mic attached. Again, it does take the ability for the technician who is with the patient to accept the call and to grant permission to take over that computer. It's not completely a passive system; you're still going to have someone there who grants access for you to control the computer and test the patient.
Mouth/Voice and Ears. The audiometer’s signal routing is a bit trickier, if you need to do live voice. First of all, the Astera and the AURICAL, because they go through OTOsuite, do have the ability to handle embedded speech material. Your usual, and your six list, your usual CIDW22, your spondee lists are already in the computer as if they were on a CD. No additional equipment is needed there. You are able to test using recorded speech, because it is integrated into OTOsuite. You are able to monitor that to the patient. The problem is that to perform talk-over, as if you wanted to perform a Monitored Live Voice (MLV), then you're going to need a higher-end video CODEC system (e.g., a Cisco or a Polycom). With the CODEC system, testing the patient is very similar to what you would do in clinic; but those do add considerably to your costs.
You have to ask yourself if you need the ability to communicate to your patient using MLV. Keeping in mind that you still have the ability to perform SRT's and word recognition with recorded speech, and do so quickly and easily. Do you need monitored live voice? If you don't need MLV, then you don't need the CODEC, and that reduces your startup costs considerably. Although the CODEC does add to your cost, it will give you the ability to use calibrated live voice; whereas if you choose not to use CODEC, and only use recorded speech, you can do that very easily.
The VA and Telehealth
The VA excels at administering telehealth. Figure 8 shows an example of a clinic on a cart. This is a different cart system than was being used by the University of Texas, but all of the pieces are similarly attached. On this particular cart, we have an Astera audiometer, an AURICAL prefit system (for fitting hearing aids), a HIT box, and a tympanometer. This system uses a very high end video otoscope that also doubles for other applications as well. This cart is available through GlobalMed. If you're sharing the cart with dermatology or otolaryngology, then you probably want to look at a higher end system like this. However, if you just need video otoscopy, then the Otocam is a much more affordable way to go.

Figure 8. The telehealth cart.
This system has two monitors: one for the visual back-and-forth between the patient and the audiologist, and one so we can operate and view the software. For testing, the technician can turn that off so that the patient cannot see what you are testing, similar to what we do in a booth.
Before the VA began practicing telemedicine, the only way for a patient to receive audiology treatment was to travel to a hospital or clinic setting. In order to perform hearing care services, audiologists require a booth and a lot of equipment, which could only be found at the hospital or clinic. However, now that teleaudiology is becoming more prevalent, the VA has the ability to reach more veterans remotely, using “the clinic on the cart” model. They've also moved some of those systems out to smaller clinics, and have adopted the mobile clinic idea (“clinic in a truck”).
Figure 9 shows a good example of teleaudiology being performed with the cart. In the top image, you can see the video CODEC system, where the audiologist can monitor what is happening at the test facility. The bottom picture is the patient, the clinician and the technician (i.e., the hands and eyes of the audiologist). The technician has been trained to perform video otoscopy, and the audiologist can see what is being presented. Also, the technician will be the one who sets them up for testing, and putting on the transducers.

Figure 9. Teleaudiology: fitting and diagnostics.
You have to consider how you are going use a technician. Who's going to be that person at the patient site and how are they going to be trained? The VA uses what they call a telehealth certified technicians, or TCTs. Usually, the TCTs are nurses, or other people that have been certified in telehealth, so they're very comfortable with the equipment. They do need to be trained specifically in audiology services. You may consider using another audiologist. Are you going to be able to share services? These are logistics that need to be addressed before implementing any teleaudiology services.
What is on the Cart?
The Otometrics equipment on the telehealth cart, located at the CBOC (Community-based outpatient clinic), includes:
- MADSEN ASTERA two-channel clinical audiometer with high frequency
- MADSEN OTOflex tympanometer
- AURICAL PMM with a built-in HiPro2 (in case wireless connections don’t work well)
- AURICAL HIT chamber
- Noah link (as a backup device)
- CODEC: It has a very nice room camera that the audiologist can control. They can pan out to see the entire room, or them can zoom in and focus directly on the patient.
- Otocam Video Otoscope: for close up work (e.g., to make sure the hearing aids are in correctly and the molds placed correctly, etc.)
- Peltor Headphones
- Ambient Noise Assessor (ANA): a system that we designed for the VA
The audiologist with a video conferencing system can reach many clinics. Since the audiologist isn't traveling, they can save a lot of time. For some remote locations, instead of traveling and hour there and an hour back, we might be able to see a few more patients in that same time frame.
Fitting Training
Assuming you have a technician, they need to be trained, in proper otoscopy and proper hearing aid placement. At the VA, they are trained in how to clean receivers, how to replace receivers, and how to set up hearing aids in a test box, so you can run that remotely. They're also somewhat trained in the manufacturer software, but keep in mind that once the audiologist takes over the computer, they can also take control of the hearing instrument software.
Diagnostic Training
From a diagnostic perspective, the technician should be trained on video otoscopy, proper placement of inserts, and proper placement of Peltor Headphones (with TDH inside). You may know the name Peltor from industrial audiology; they make noise suppression and hearing protection headphones. Finally, the technician should know how to put on the high frequency headphones, as well as the bone conductor.
Ambient Noise Assessor (ANA)
For many telehealth situations, you don't have the benefit of a booth. Typically, telehealth is conducted in very small offices. How do we control for background noise? We are very comfortable with and trust the testing that occurs in our booths; but what do we do for these situations where we do not have a booth? Now, we have what we call the Ambient Noise Assessor (ANA). It's going to monitor the background noise where the patient sits, using the FreeFit collar and the room mics on the FreeFit collar (Figure 10). This gives the audiologist the ability to see the noise level in the patient’s environment. It is not an accurate for the clinician or the technician to estimate what they believe to be “quiet enough”; they need to measure the noise level. The Ambient Noise Assessor continually monitors the noise level in the room where the testing is being performed, and it compares it to an ANSI standard. It also gives the audiologist a visual display that is very frequency-specific and transducer specific, to determine at that moment in time, if the room was quiet enough to meet ANSI standards. It gives a visual feedback (green is good; red is bad), and it stores the status of that background noise for every stored threshold.

Figure 10. FreeFit collar.
Background and Rationale
The ANA was originally developed for the VA. However, it is available for anyone who's looking to implement a teleaudiology program. With the ANA, you have to think about noise a little differently. When we have our booths checked to make sure that they are quiet enough, the calibration is done at one moment in time for each frequency, at one time during a day. For example, on Monday morning at eight o'clock, that booth passed inspection, and that booth is quiet at each frequency. That may not be the case when you have a full clinic. If you have children in the waiting room, and many people walking around in the clinic, the noise level goes up considerably. There is no way of saying for sure that that booth is quiet enough throughout the day. However, with an Ambient Noise Assessor, it's going to give you much more interaction and that's going to be based at that moment in time. It's going to allow the clinician to know that when they presented a tone, at that moment in time at that frequency with that transducer, did it meet ANSI standards. The standards assume a static environment. The ANA applies an approach which is appropriate for more dynamic environments, and allows users to carry out valid diagnostics in otherwise uncertain environments.
Diagnostic testing requires acceptable ambient noise levels, which can be achieved in a sound enclosure or booth; but we need a way for the audiologist to see if the conditions change. Certainly, if you are interested in teleaudiology, you want to get a good idea about whether your intended testing environment is quiet enough. However, noise levels change throughout the day. When traffic increases, does that area continue to remain quiet enough to allow testing? Using the Ambient Noise Assessor, you can be sure that when you present a tone, you had an environment that was quiet enough for testing. ANA assumes a dynamic environment. It takes into account the presence of the patient and a changing noise landscape during test procedures, and allows for valid diagnostic testing in a potentially changing environment.
Peltor headphones are shown in Figure 11. Inside the sound enclosure is a TDH 39 headphone. We also use the FreeFit collar for monitoring those noises; the microphones are now on their shoulders, and not on their ears.

Figure 11. Peltor headphones and Aurical FreeFit collar.
Instead of hanging the reference microphones on their ears, we place them on each shoulder, with the microphones facing upward (Figure 12). In this way, the mics are now monitoring, or listening to, the room noise, and continually giving real-time feedback as to the noise level in that room.

Figure 12. Reference mics monitor the ambient noise.
Figure 13 shows how it is displayed in OTOsuite. The audiogram on the left has a green check mark in the lower left hand corner. That indicates that for every presentation of sound, we were able to meet ANSI standards for that frequency, for that transducer, at that moment in time. We can be very confident that our environmental noise was quiet enough that our audiogram is valid.
Conversely, the audiogram on the right shows what you would see when the noise level does not meet ANSI standards. When you present a tone, the reference mics listen and determine whether at this intensity at this frequency at this moment in time with this transducer, if it is quiet enough in this room. If it is too noisy, the audiologist will see the real-time results on the screen (indicated by the orange background). That gives the audiologist the ability to figure out what's going on. They may need to wait a minute; or they might need to find a quieter location. There may have been noise in the room that you could not detect at the far site, but that was picked up by the reference microphones and recognized as too loud. That gives the audiologist a lot more information on how to proceed.
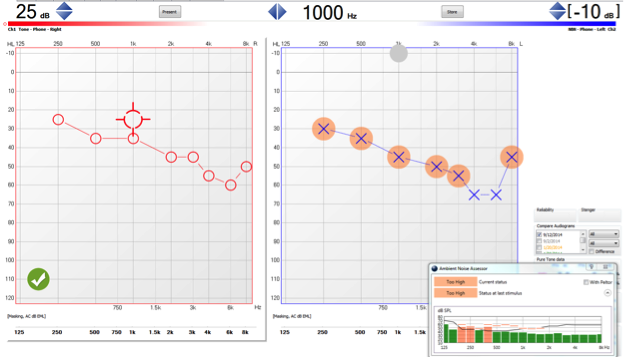
Figure 13. ANA display in OTOsuite.
Figure 14 is a close-up of what the ANA is doing. The line that goes from left to right is the transducer line, which indicates the ANSI standard for this transducer at these frequencies. In the top graph, we can see that in the 250 Hz and 500 Hz range, it is not quiet enough to present those tones. On the bottom graph, we are within ANSI standards and we can be confident that we have good test results. The bottom graph would give us the green checkmark in the bottom left hand corner, and the top graph would give us those orange backgrounds that indicate it's too loud.

Figure 14. Ambient Noise Assessor display tone (enlarged view).
Figure 15 shows how ANA is displayed when performing speech testing. The microphones will pick up not only the ambient room noise but also the patient’s verbal response. When it is quiet enough, the green background behind the dB level appears; when it is not quiet enough, the orange background appears. We can be confident that when we are performing the test, that the noise level was sufficiently quiet to meet ANSI standards and that we have good valid results. With the Ambient Noise Assessor box, we have that constant feedback, so the audiologist can monitor the room noise during presentation, select the appropriate status and then save the results.
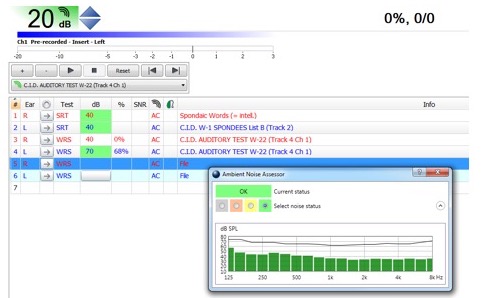
Figure 15. ANA display OTOsuite-Speech.
Comparison Between FreeFit and Bruel & Kjaer SLM
How good is ANA? We compared it to the Type 1 sound level meter (i.e., Bruel & Kjaer sound level meter) and found that the precision of the FreeFit was very close - it was within +/- 1 dB for frequencies below 2 kHz, and +/- 1.5 dB for frequencies above 2 kHz. At no time was the Ambient Noise Assessor off more than 1.5 dB. It’s close enough to affirm that this room is quiet enough for testing. We do have a microphone on each shoulder, so at any given moment, when it listens for the room noise, it's going to give the feedback for the mic that received the largest amount of noise. If the noise was on the right side, and the mic on the right side detected a louder level than the mic on the left side, it's going to show you the loudest level on the right.
In some situations, we are able to use the clinic on a cart in conjunction with a booth (Figure 16). The cart would remain on the outside of the booth. Next to the monitor, there is a camera, so the audiologist working remotely is able to still see the patient while taking control of the audiometer. Of course, you wouldn't leave the view of OTOsuite on while you are testing in there. Again, a very well trained technician is necessary to be able to assist you with testing at the clinic site.

Figure 16. “Clinic on a cart” with testing performed in a booth.
Support Personnel
To reiterate, in order to successfully implement teleaudiology, you will need someone on the other end to facilitate interaction with the patient. Are you going to use an audiology technician? Do you have someone who could be trained well enough to be your eyes and hands? They're going to do a lot more than putting the transducers on. They will greet the patient when they arrive. They must be able to counsel them a little bit. Some locations do have technicians who are trained in basic troubleshooting and hearing aid repairs, since the patient would likely have to travel a long distance to get to an audiology clinic for testing.
Questions and Answers
Are there any ethical concerns that have arisen?
I'm not aware of any. Some people are opposed to telepractice due to the lack of in-person interaction. They may feel that in treating a patient virtually, they will be unable to interpret body language or facial cues. I can certainly see that point of view; however, I think if there is a good connection between the technician and audiologist, and you have a good camera, you can pick up on a lot more of that body language. There are a lot of studies that show that hasn’t been so much of a concern, because patients do not see this as a deterrent for participating in teleaudiology. I think they're a lot happier to not have to travel so far.
How would this work with speech testing?
For speech testing with OTOsuite, you do have the ability to use embedded word lists. Think of it as old-school when we had a CD player, and we would run that through the audiometer, and you would have a calibrated speech signal. You would have your NU6 word lists on a CD, or your CD from Auditech; then you would play those through the audiometer, so the audiologist can choose them, play spondees, still get their SRT. They can perform word recognition with whatever speech material you usually use, and still attain that. It's a lot faster than a traditional CD, because you have control to present the word when you're ready for the word. I think traditionally, people don't like doing recorded speech because it is slow, but it is accurate. With OTOsuite, you have the ability to present the word when you're ready for the word, and that allows you to perform the SRT or the word recognition at the patient's pace. If they're a super-fast processor, they can go through that word list quickly, you can give them the words at their pace. Or, if they're a very slow processor you can slow that down, and present to them at the pace that they need.
Do you do remote programming of hearing aids?
Yes. The VA program and the University of Texas both do remote programming/fitting of hearing aids, because they're able to take control of the computer. The audiologist needs to train the technician, or whoever will be their hands at the patient site, to properly place the probe tube, put the hearing aid on correctly; but then the audiologist can see the response from the probe mic, to see if we're meeting target or not. They can take control of the hearing aid software all on the same screen, all on the same computer, all with the same mouse in hand, and make those adjustments as needed. What makes that possible is the software that controls the real ear system and the audiometer, and being able to take control of that computer.
What was Medicare's objection to teleaudiology and what are we doing about it?
I haven't looked into that a great deal other than to know that we audiologists were not initially included in Medicare's ruling. As a profession, we need to try to raise awareness and get reimbursement for treatment via telehealth. Especially as our numbers dwindle, and the population increases, there is going to be a broader need for that.
Do you see a future where the audiologist will be based in another country, kind of like call centers today?
The thought of a call center scares me. However, I think there are some hearing aid manufacturers that are already doing something similar. They have sites where a patient can phone in, and an audiologist or technician working remotely can take care of them. With our changing field, we need to own this; we need to take control of this. As far as another country, I do see the positive aspects of the telehealth “clinic on a cart” model. These systems are already being used in the Department of Defense to meet that need of our service members. For example, an audiologist in Italy can program someone’s hearing aids in the Middle East, or at least evaluate them. Audiologists typically are not located in combat zones, but there are times when service members do need to be evaluated. In that respect, yes they are in different countries.
What are the considerations for interaction within teleaudiology?
You need to determine who is going to be your hands with the patient. You also need to figure out if you can live without monitored live voice. Keep in mind that you can still communicate verbally with the patient, the technician and the audiologist -- that's not an issue. The issue is whether you need a calibrated speech signal as we would use in monitored live voice. If you don't need that, then you don't have to have a CODEC (which allows the audiometer to work through a video conferencing system and give you a calibrated system). It's a little bit outside of our expertise; I'm much more comfortable routing the audiometer on the computer. When setting up a CODEC, you may need IT support.
The goal for telehealth in general is to not have to move the patient as much, so we're going to reduce the travel time. Certainly, in-clinic, we've all seen the physical decline of some of our patients and the inability to get them back into the clinic. I think that teleaudiology could fill that gap. We can meet more patients’ needs if we can travel to the patients more, whether that's a mobile clinic, clinic on wheels, or a clinic on a cart. Like I mentioned earlier, some of the time it's not a physical barrier, but it could just be congestion in traffic. They're using a cart system and telehealth at the Pentagon. They have a health clinic in the Pentagon, but for service people who are across town, they would lose a whole day, essentially, just for a small check. They're doing more industrial type testing, but they can do it very quickly, remotely, and they don't have to lose time away from work.
Citation
Moore, K. (2017, April). Teleaudiology 101. AudiologyOnline, Article 19711. Retrieved from www.audiologyonline.com


