Short Abstract:
This case report describes a post-stapedectomy patient with chronic, treatment-resistant, catastrophic tinnitus that was contributing to suicidal ideation. While Lenire is typically used in moderate to severe cases, this patient experienced significant improvement following a comprehensive treatment plan incorporating Lenire. Within 12 weeks of initiating treatment with Lenire, alongside ongoing therapy sessions, her THI score dropped from 78 to 30. Prior to this treatment, the patient was taking Ambien, Zoloft, Xanax, Ativan, and Lexapro in an attempt to regulate sleep and mood, and she has since been able to discontinue all medications. One year later, her THI had further decreased to 16. As Lenire gains traction in clinical practice, real-world cases like this help clarify its role in managing complex tinnitus presentations, particularly following surgical interventions.
Introduction
Tinnitus, a condition that is often described as a ringing in the ear, affects ~14% of adults worldwide1. This case report presents a complex post-stapedectomy patient with long-standing, treatment-resistant tinnitus who found significant relief with a treatment plan that included Lenire. Lenire is the first and only FDA-approved bimodal neuromodulation tinnitus treatment device.
This success story illustrates how patient-centric, proactive care integrating emerging evidence-based therapies can lead to meaningful reductions in tinnitus, even in patients with a prolonged history of unsuccessful treatments.
This report provides insight for clinicians aiming to broaden their management strategies in similarly complex cases.
Initial Audiology Consultation and Medical History
This female patient in her early 50s presented to the lead audiologist at the Alaska Hearing & Tinnitus Center (AHTC) in May of 2023 with a tinnitus handicap inventory (THI) of 60, which indicates severe tinnitus. However, due to the patient’s marked distress, a recent suicide attempt, and significant emotional impact observed by her audiologist, she was classified as having catastrophic tinnitus.
Tinnitus onset occurred in her early 30s, and at ages 40 and 50, she was diagnosed with conductive hearing loss in her left and right ears, respectively. She was later diagnosed with bilateral otosclerosis.
She noted that she was not getting restful sleep and was receiving ongoing care from a psychiatrist and a therapist. Her psychiatrist prescribed zolpidem (Ambien), a sedative, to improve her sleep, benzodiazepines (Ativan and Xanax) for anxiety, and sertraline (Zoloft) for depression. She had also recently completed a course of ketamine infusions for treatment-resistant depression.
Additionally, she used hearing aids with sound masking features as part of her tinnitus management strategy.
She relied on masking to function throughout the day and was practicing breathing and meditation techniques. In addition to her treatment regimen at this time, the patient had previously pursued other treatments that did not yield sufficient relief. These included tinnitus retraining therapy (TRT), sound generators, vitamins, tapping, and some online remedies.
At her initial appointment, the patient expressed a strong interest in trying Lenire after hearing promising things about it. However, since she had a stapedectomy scheduled in about three weeks, her audiologist recommended delaying the initiation of treatment with Lenire until after her surgery. Although the majority (>70%) of patients fitted with Lenire at the AHTC have moderate or severe tinnitus at baseline, with fewer than 20% being classified as catastrophic (as of April 2025), her audiologist was supportive of moving forward with Lenire once the surgery was complete without complications. The surgeon performing the stapedectomy was consulted and later supported the recommendation for Lenire. After being advised by her audiologist, the patient agreed to try cognitive behavioral therapy (CBT) and some more sound therapy provided via an iPhone app in the meantime.
Other Pre-Surgery Patient–Audiologist Contact
In the two weeks following this appointment, the patient attended two more audiology visits at the AHTC before her surgery. During these sessions, sound therapy and breathing techniques were discussed. Throughout this period, the patient experienced severe anxiety and ongoing suicidal ideation. In response to her expressed thoughts of suicide, her audiologist developed a safety plan. She was also receiving continued support through additional appointments with her therapist, psychiatrist, and primary care physician. Her sleeping medication dose was increased, resulting in partial symptom relief that lasted only a few days. The patient was looking forward to her surgery, with hopes of getting some relief from her tinnitus as well as improved auditory functioning.
Post-Surgery Patient–Audiologist Contact
Twelve days after the surgery, the patient contacted her audiologist. The stapedectomy went well, and apart from sound sensitivity in her left ear in the days immediately following the surgery, the patient was thrilled to be able to hear the wind and watch television on a normal volume with her family with only her right hearing aid in. Although her hearing improved, her tinnitus increased dramatically, causing her significant distress. She remarked the following to her audiologist in the days after her surgery:
“This is the hardest thing I have dealt with in my life, and I'm scared.”
Her surgeon, suspecting that this tinnitus exacerbation could have been due to cochlear irritation, prescribed a corticosteroid, prednisone, for six days. Unfortunately, this was not effective, and her tinnitus remained elevated. During the 10-week period between the patient's surgery and her Lenire fitting appointment, she attended three additional appointments with her audiologist. She also worked closely with her psychiatrist to optimize her medication regimen for improved sleep and anxiety management.
Her psychiatrist transitioned her off Ativan and initiated treatment with Lexapro. The patient’s sleep quality fluctuated, alternating between periods of improvement and episodes of poorer sleep, and she was experiencing anxiety attacks. In addition to her ongoing tinnitus management with her audiologist, she continued seeing her therapist, eliminated her daily nap to support better sleep, and made an effort to walk outdoors more regularly to boost her mental health. She also reached out to a psychologist for CBT and Mindfulness-Based Tinnitus Stress Reduction (MBTSR) and planned on starting this self-guided program in a few weeks.
She had her post-op otolaryngology (ENT) appointment during this period. The surgeon was satisfied with her surgical outcomes and recommended Lenire as an appropriate treatment option moving forward.

Figure 1. Lenire® Tinnitus Treatment Device
Post-Lenire-Fitting Patient–Audiologist Contact
In early August, 10 weeks after her surgery, this patient attended her Lenire fitting appointment with a catastrophic THI score of 78. At this appointment, she trialed the device for 10 minutes and received counseling on device usage and treatment expectations for the initial two-week period. The patient planned to meditate and follow her self-guided MBTSR protocol during Lenire sessions. She performed two 30-minute sessions per day with Lenire, as prescribed.

Figure 2. Clinical Process for Lenire Treatment at the Alaska Hearing & Tinnitus Center. Reproduced with permission from McMahan & Lim, 20252
At her two-week follow-up appointment, she reported that the hissing part of her tinnitus was already decreasing and noted improvements in sleep quality. She discontinued her sleep medication (Ambien) two days before this appointment. The patient then had two consecutive nights of restful sleep, where she either didn’t wake or fell back to sleep quickly after waking. At this point, she also began tapering off Lexapro.
She was visibly happier and full of hope.
At her six-week follow-up appointment, her THI had decreased by 42 points down to 36, indicating a mild tinnitus handicap, bordering on moderate. She indicated that her tinnitus was absent on many days and that when it was present, it was significantly less bothersome than before. She had successfully discontinued both Ativan and Lexapro, was sleeping well, noted improvements in cognitive clarity, and reported that she was starting to feel more confident. Her family also observed this significant increase in well-being. She continued to use Lenire for two 30-minute sessions daily, was doing some MBTSR, and kept up her regular therapy sessions.
Post-Treatment: Discontinuing Medication, Sleeping Well, and Returning to Work
At her 12-week follow-up appointment, her THI score was down to 30. Clinically, she was doing exceptionally well, continuing with two 30-minute Lenire sessions daily and remaining engaged in therapy. She contemplated cancelling her appointment as she felt she didn’t need to see her audiologist; however, she chose to go to report her positive progress.
She reported being completely off all medications, and she no longer needed to wear her hearing aids with sound maskers at night. She was sleeping all night long and was excited to report that she was returning to work. She was enjoying more quality time with her family; notably, her husband even attended the appointment to thank the audiologist for giving him his wife back. She also shared that she was enjoying time with her son and picked him up from the bus stop daily.
One year after her initial Lenire fitting, the patient expressed deep gratitude to her audiologist via a phone call and an email, reporting a THI score of 16 and using Lenire about once a month to maintain symptom relief. She declined an appointment as she was doing so well.
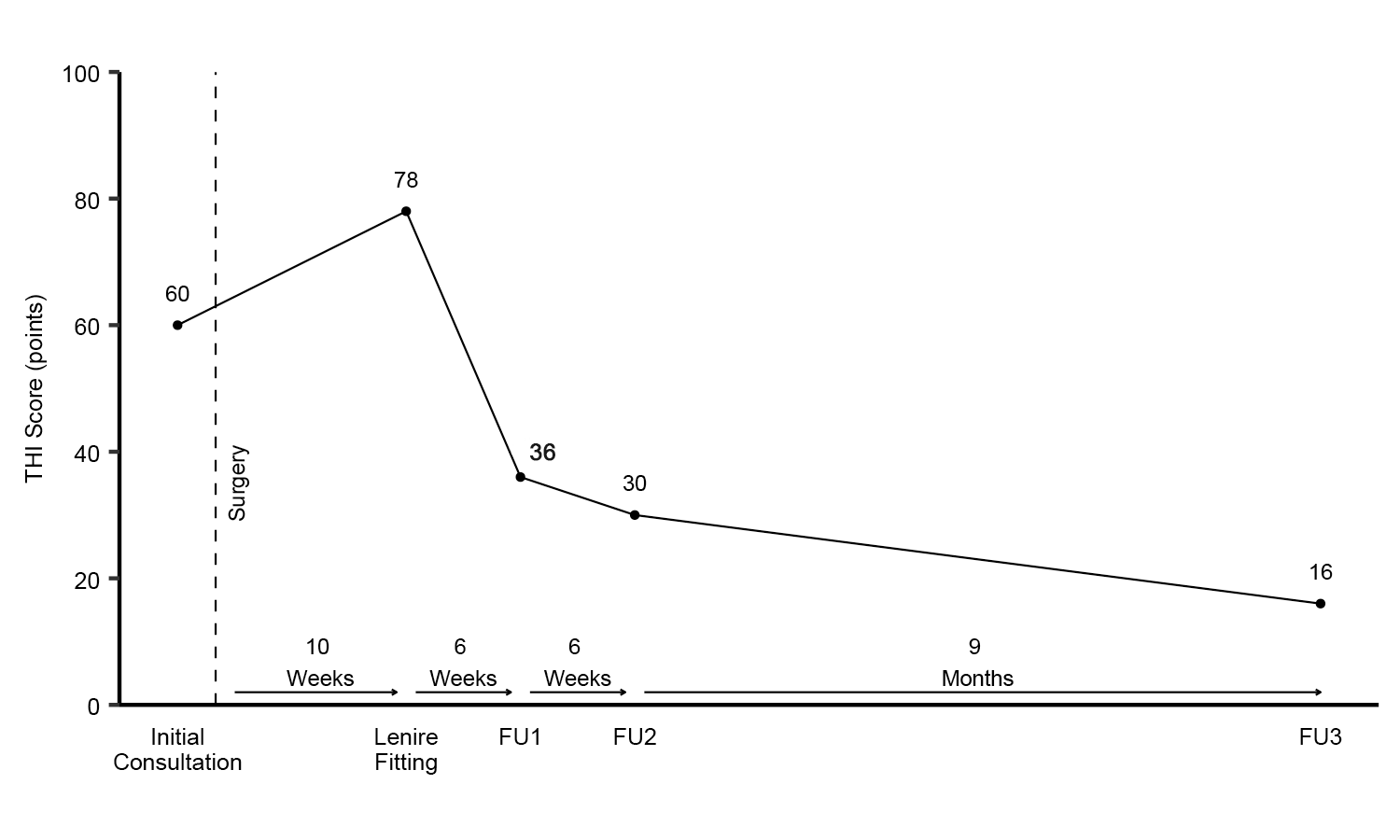
Figure 3. Tinnitus Handicap Inventory Before, During, and After Treatment with Lenire
She also returned to her art studio and sent her audiologist a handmade vase inscribed with the following message:
“Never give up on the hard patients as we still have beautiful work left to complete in this world.”
Closing Remarks
This case marks the end of a 20-year struggle with tinnitus, depression, anxiety, suicidal ideation, and dependency on pharmaceuticals to attempt to maintain a tolerable quality of life. The patient-centric, customized treatment plan described herein culminated in significantly meaningful tinnitus improvements and restored this patient’s lost quality of life.
The purpose of sharing this case is to offer insight to tinnitus care professionals managing complex, chronic cases and to illustrate that Lenire is a safe and effective treatment option following a stapedectomy. Additionally, this case can inform hearing healthcare professionals who are less familiar with tinnitus about the impact that catastrophic tinnitus can have on a patient.
References
- Jarach, C., Bosetti, S., Schietroma, A., et al. (2022). Global prevalence and incidence of tinnitus: A systematic review and meta-analysis. JAMA Neurology, 79(9), 888–900. https://doi.org/10.1001/jamaneurol.2022.2610
McMahan, E. E., & Lim, H. H. (2025). Retrospective chart review demonstrating effectiveness of bimodal neuromodulation for tinnitus treatment in a clinical setting. Communications Medicine, 5, Article 112. 10.1038/s43856-025-00837-3
Acknowledgements
Emily McMahan, AuD, is the audiologist who treated this patient. She is a provider of Lenire and is the owner of the Alaska Hearing & Tinnitus Center. The authors would like to thank the team at the Alaska Hearing & Tinnitus Center for their assistance with the project and clinical administration. The author and clinic received no external funding in relation to the completion of this case report.

