Approximately 30 million people in the United States report having hearing difficulty (NIDCD, 2007), representing 10% of the current population of the United States (Kochkin, 1999). While amplification in the form of hearing instruments represents a viable option to individuals with hearing loss, a significant percentage of the population postpones using hearing instruments. Historically, the hearing instrument market penetration has been low, yielding approximately 22% (Kochkin, 2001). While the market penetration has remained relatively flat, first-time hearing-instrument-user purchase trends have significantly declined over the past several decades. For example, during the 1980s, 60% of the hearing instrument market was comprised of first-time buyers, whereas data in 2001 shows that the percentage of first-time buyers fell to 45% (Strom, 2002). Even with relatively flat market penetration, if first-time hearing instrument buyers comprise a smaller percentage of the current market as compared to the recent past, fewer consumers are actually pursing hearing instruments as an option for assistive technology . One approach to expanding the hearing instrument market involves offering communication solutions in the form of Hearing Assistance Technology (HAT). The purpose of this article is to address some of the barriers to HAT integration, to review current HAT dispensing trends, and to offer practice solutions on how to generate product awareness for a minimal investment of time and money.
Hearing Assistance Technology
Hearing assistance technology (HAT) refers to a broad range of devices beyond traditional hearing instruments designed to facilitate the reception of auditory information (Thibodeau, 2004). The product scope of HAT devices include amplified telephones, cell phone accessories, TV listening devices, personal listening devices, and alerting devices. Regardless of the specific product type, HAT is intended to optimize communication for those with hearing loss in a variety of ways. Some products bridge the distance between the speaker and the listener by routing the conversation from the speaker directly to the ear of the listener without the additional presence of background noise or signal degradation as a result of poor room acoustics. Other products facilitate the reception of auditory stimuli by generating an amplified auditory signal (i.e. loud alarm signal) and/or delivering an alternative signal such as a visual (i.e. lamp flasher, strobe light) and/or vibrotactile indicator (i.e. bed shaker). Furthermore, some HAT products have been designed as stand-alone devices and will not interface with the t-coil of hearing instruments. For example, alerting devices such as alarm clocks or smoke detectors are intended to be used independently. Most HAT products, however, have been designed to interface with hearing instruments equipped with t-coils. In some cases the interfacing design is an optional aspect of the product. In other words, many of the HAT products will function as stand-alone products although they can also interface with the patient's hearing instrument.
Benefit of HAT Technology to Audiologists
The majority of individuals with hearing loss who were users of HAT (75%) consistently report significant benefit (Wayner, 2004). The reported benefits extended well beyond a general communication advantage to other aspects of overall well-being. For instance, an overwhelming majority of the same users (84%) expressed that the integration of this type of technology facilitated independent living (Wayner, 2004). Given the inherent properties of HAT, the reported benefits are to be somewhat expected. What often is overlooked, however, is the benefit of this technology to audiologists who integrate these products into clinical practice. First, giving patients access to HAT offers the opportunity for the clinicians to provide an immediate communication solution. This is particularly beneficial in those situations when the individual is in denial of the existence of a hearing loss and not yet willing or ready to pursue hearing instruments. Putting a hearing-solution product in their possession will most likely increase the chances for that patient to return to your clinic when they are ready to pursue hearing instruments.
Secondly, expanding clinical services to include HAT will assist audiologists in further establishing themselves as communication experts for patients to turn to in matters related to the diagnosis and non-medical treatment of hearing (and balance) disorders. Unfortunately, barriers to HAT integration often times overshadow these benefits.
Barriers to HAT Integration
Despite the inherent benefits of this type of technology, successful integration of HAT into current audiology practices is hindered by a variety of barriers. The most commonly cited barrier is the factor of limited time (Servedio, 2000). Most appointment times for amplification assessments accommodate a review of hearing instruments, with little or not time left to review HAT. Many clinics must sustain a specific patient flow to stay in business; faster-paced clinical environments will inherently have less allotted time to sufficiently review HAT with each patient. A solution to the limited time barrier would be the provision of additional resources, such as an audiologist or trained office personnel who could take the time to review HAT options with patients. Unfortunately, the lack of additional resources serves as another barrier (Prendergast and Kelley, 2002).
Limited space serves as another potential barrier to HAT. Given the number of different HAT categories and associated product lines within each category, the perceived need for stocking space and/or room for product demonstration may be perceived as an overextension of current clinical capacity, particularly for clinics with very small waiting room/reception areas or clinics lacking adequate counseling space. In addition, the plethora of available HAT products may also be overwhelming to the audiologist who has not had the extra time or energy to acquire necessary product knowledge (Ross, 2004).
From a financial perspective, many dispensing professionals believe that HAT is not profitable (Servedio, 2000). This is a relevant issue to audiologists employed in all sectors of clinical practice as the livelihood of any business, whether a private practice, clinic, or hospital, depends on profitable cash flow. The gross margin of HAT, even if greater than 30%, will yield a relatively small amount of revenue. The extent of the revenue is further influenced by the amount of time an audiologists spends orienting the patient to an HAT. Spending 30 minutes discussing hearing instrument options will most likely be viewed as a better investment of time than spending 30 minutes orienting the patient to an amplified telephone. As a result, lack of interest and professional apathy also create barriers to HAT integration in the audiology clinic (Bankaitis, in press).
Current Status of HAT within Audiology Practice
The literature assessing the extent to which HAT is integrated within the audiology clinic is quite limited. Most of the available studies do not specifically differentiate the dispensing audiologist from the hearing instrument specialist, combining the two into a more general dispensing professionals group. Of the available studies, most of the literature suggests that that HAT is not being effectively integrated into routine hearing instrument evaluations. Not surprisingly, when dispensing professionals are asked to respond to questions pertaining to the importance of aural rehabilitation in the overall scope of an individual's hearing health care, a unanimous majority (100%) of clinicians rate the provision of information on HAT as beneficial; furthermore, 78% indicate that HAT services are provided "most of the time" (Predergast and Kelley, 2002). In contrast, when patients with hearing impairment were asked about scope of hearing health care services received, approximately 30% indicated that the dispensing professional informed them of HAT beyond traditional hearing aids (Stika, Ross, and Cuevas 2002). In other words, the majority of patients with hearing impairment (70%) were not informed of HAT other than traditional hearing instruments. A plausible explanation for this discrepancy may certainly be attributed to the fact that patients simply did not remember that HAT was reviewed. Recent research, however, has shed some additional insight toward the HAT disconnect that is occurring between patient and clinician.
Keller and Bankaitis (2006) assessed general dispensing trends of HAT by using an on-line questionnaire. While the number of respondents to the survey remained relatively low (5.5% return rate, or N=61), the information gathered from this study suggests that current point-of-purchase strategies implemented by audiologists actively dispensing HATs are ineffective. While the majority (92%) of the respondents reported actively dispensing at least one type of HAT, most audiologists dispensed, on average, zero to two TV listening devices (71%) or amplified telephones (79%) each month. Since both of these products represent the most popular HATs reportedly dispensed, the overall monthly volume of units dispensed remains extremely low. The low sales rate was present despite the fact that the majority of respondents (98%) reported relying on multiple tactics to educate patients about HATs. Interestingly, an overwhelming majority (81%) reported using one-on-one counseling during the hearing instrument orientation to educate patients about HATs; however, less than 10% of patients invested in HATs when these products were introduced during the hearing instrument orientation.
These trends indicate that introducing HAT at the time of the hearing aid orientation is not an effective strategy. While timing the HAT educational process during the initial hearing instrument orientation may seem appropriate to the audiologist, it is possible that using this time as an HAT educational opportunity is too overwhelming to the patient. To the new hearing instrument user, a lot of information about the hearing instrument must be processed. Introducing additional technology during that time is probably not appropriate. Furthermore, hearing instruments are a costly investment to most patients. By presenting patients with additional amplification options, the audiologist may be inadvertently sending a message to the patient that their hearing aids will not be enough. Even if this is true, timing the introduction of HAT to the patient seems to be a more critical component to the patient buy-in process.
HAT Integration: Practical Suggestions
At the time that Keller and Bankaitis (2006) were collecting HAT dispensing trend data, additional observational data was collected in collaboration with the Division of Adult Audiology at Washington University School of Medicine to gain a better understanding of how to effectively market HAT to patients with minimal investment of time and money, and in a manner considered unobtrusive to the daily practice and established routine (Bankaitis, in press). Based on preliminary research with Washington University's School of Medicine's Division of Adult Audiology, the following suggestions are proposed in an effort to further increase HAT sales:
Suggestion #1: Set up working product demos instead of demo models.
A demo is simply a product removed from its packaging and on display for show. Although demo models allow patients to touch and feel the product, demo models do not actually work and therefore do not offer the opportunity for the patient to actually experience using the product. In contrast, working demos refer to products that have been removed from the box, plugged into the necessary electrical outlet, and displayed in a manner that allows the patient to actually use the product to get an idea of its potential benefits. Working product demos are critical for facilitating self-exploration on the part of the patient. More importantly, working demos allow patients to become familiar with HAT at their own pace, minimizing the effort on the part of the clinician or front office staff to educate patients.
Given the number of products available, initial observations at Washington University Medical Center have identified four key product categories to showcase to patients in the form of working demos. While it is beyond the scope of this article to orient the reader to review specific products, the following offers a brief description of each category.
Amplified Telephone:
As shown in Figure 1, amplified telephones look and work just like standard telephones with the exception that amplified telephones are designed to increase the volume of the caller's voice when needed. In choosing amplified telephones, it is recommended to include one cord model and one cordless model. This will effectively communicate to patients that choices in amplified telephone models are available. In addition, it is critical to set the telephones up using a relatively inexpensive phone-linking device. These phone-linking devices are also commonly known as telephone-line simulators or telephone demonstrators. A phone-linking device works independently of the telephone network and allows two phones to be linked to one another in such a way that patients can hear the phone ring, manipulate telephone features, and converse over the telephone without requiring access to a phone jack or tying up an existing telephone line. Some of these devices may also have an audio in/out port that allows users to listen to pre-recorded speech material if needed. When the handset of one linked telephone is picked up, the phone-linking device will cause the other linked amplified telephone to ring. The telephone will continue to ring until the handset is picked up, at which time the patient can experience the benefits of the demonstration phone, and make a more informed decision as to whether or not either phone will meet his or her needs. Since phone-linking devices place two linked-telephones in close proximity to one another, the most effective demonstration strategy is to link a cordless phone to a corded telephone. In doing so, patients using the cordless telephone can walk away from the corded telephone being used by the other party. This flexibility allows patients to not only test the cordless telephones reception range, but eliminates the potential of overhearing the conversation from the other party as a result of standing in close proximity to one another.

amplified telephone
Cell Phone Solution:
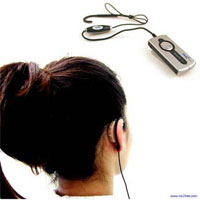
Given the increased demand for eliminating interference associated with cell phone use by hearing instrument wearers, clinicians should be prepared to offer hearing instrument patients a solution for the cell phone. Figure 2 shows an example of an induction earhook that interfaces with the t-coil of the patient's hearing instrument(s) and the user's cell phone. Other cell phone solutions that work with Bluetooth-enabled phones, such as the one shown in Figure 3, are also available. Clinicians should have available at least one cell phone product in their clinical offices for patients to try. Since most cell phone users have their cell phone on hand, a cell phone induction hook, for example, can be plugged into the patient's cell phone and a phone call may be placed by the clinic to the cell phone user to enable the patient to make an assessment as to whether or not a particular product works effectively.

Figure 2. NoiZfree™ Induction Earhook use with cell phones
 >
>Figure 3. NoiZfree™ Beetle Bluetooth Induction Coil
for use with Bluetooth-enabled cell phones
TV Listening Devices:
TV listening devices allow users to listen to the TV (or other sound source, such as a stereo or CD player) without having to increase the volume of the TV or stereo such that it is too loud for others. The devices are comprised of a transmitter and receiver. The transmitter connects to the specific sound source (i.e. TV, stereo) and delivers signals wirelessly to the receiver. The receiver is usually a headset worn by the listener. Figure 4 illustrates a popular TV listening device. At least one TV listening system should be installed in the clinic to allow patients to experience the benefits of this form of technology. Since these types of devices are most commonly for home use with the TV, investing in a dedicated TV would be beneficial to allow for product demonstration. It is not necessary, however, to invest in a TV. Infrared systems may be effectively showcased by coupling the transmitter to other audio sources, including a CD player.

Figure 4.The Direct Ear™ Set 810
infrared system from Sennheiser®
Personal Listening Devices:
Finally, personal listening devices include a range of hard-wired (Figure 5) or wireless products designed to amplify speech and are effective in providing improved signal to noise ratios in challenging environments. Access to these devices is beneficial to help patients in situations where communication may be a challenge during the audiology appointment. For example, allowing the hard-of-hearing patient to use a PockeTalker when test results are reviewed will not only make it easier for both the patient to engage in a productive conversation, but it will also generate awareness about HAT products without requiring the clinician to expend significant energy explaining what the product is or how it works.

Figure 5 The William Sound PockeTalker Ultra™
In general, the specific product to display, while influential in the purchasing process, is not as critical as ensuring that the items displayed actually work and can be used by the patient in the clinical setting. In terms of amplified telephones, a relatively inexpensive phone-linking device is available, enabling two phones to be linked together and actually work without requiring access to an existing phone line. In terms of TV listening devices, the clinic can invest in a TV although a CD player can be used just as effectively to demonstrate the benefits of these devices.
Suggestion #2: Commit to provide independent patient accessibility to working demos.
Provide patients with independent access to working product demos, as patients need hands-on experience to try out HAT products at their own speed and on their own terms, without the perceived influence of the clinician or the investment of clinician time and effort. Independent access to working demos provides the patient with experiences necessary to appreciate product benefits on their own, empowering them to become an active participant in their hearing health care. Furthermore, independent access to working product demos intuitively segregates patients into two general groups: 1) motivated potential buyers, and 2) non-interested patients. Motivated patients will be more likely to seek out information from appropriate clinical personnel compared to non-interested patient counterparts. This type of set up will inherently direct motivated patients to self-initiate the product purchasing process, thereby minimizing the time and effort clinicians typically exert in identifying potentially motivated patients.
Suggestion #3: Rely on the "Less is More" strategy in displaying working models of HATs.
While this suggestion may seem counterintuitive, patients can easily become overwhelmed by too many choices. Selecting a few key HATs to set up will create a less intimidating environment and successfully facilitate the initial HAT purchase process. As previously mentioned, four general HAT product category types have been effective in piquing patient curiosity and generating interest in HAT technology. Displaying four to six working demos throughout the clinical environment is sufficient. In addition, an example of each working demo does not have to be available in each patient care or counseling room. Rather, one counseling room may be equipped with two amplified telephones, whereas another counseling room may be equipped with a working TV listening device.
Suggestion #4: Make room in clinical area for setting up working demos.
Placement of working demos in the reception area may not be as effective. Initially, working demos were placed in the reception area of the Division of Adult Audiology at Washington University Medical Center as it was felt that it would be the most conducive location for patients to self-explore HAT products. Over time, it became evident that patients were not engaged in HAT products when placed in the reception area, perhaps refraining from trying out new technology in the presence of others. Placement of working demos in the clinical patient rooms has been observed to facilitate more patient involvement. For example, most patients placed in a counseling room and left alone for a few minutes at the beginning of an appointment become actively engaged with working demos that were in the room without any prompting.
Conclusion
Certainly, more information is needed to assess the most effective means of integrating HATs into the clinical environment. Based on the initial observations made by the Division of Adult Audiology at Washington University Medical Center, a broader, multi-center study will be conducted in the near future to assess the influence of not only demo mode versus working demos facilitating consumer buy-in of HAT, but also the influence of environment (i.e. reception versus the clinical patient care room) to this process. While additional data needs to be collected, audiologists are encouraged to re-evaluate current HAT implementation strategies. For those not involved in generating awareness about HAT, as well as for those currently engaged in dispensing HATs, implementation of all or even a few of the outlined practice suggestions may assist in boosting patient interest and appreciation of such products.
References
Bankaitis, A.U. (in press). Hearing Assistance Technology. In M. Valente, H. Hosford-Dunn, R. Roeser (Eds.), Audiology: Treatment. New York: Thieme Publishing.
Keller, A.S. & Bankaitis, A.U. (2006). Current Trends in Hearing Assistance Technology. Capstone Project, Washington University School of Medicine, Central Institute for the Deaf, St. Louis, MO.
Kochkin S. (1999) "Baby Boomers" spur growth in potential market, but penetration rate declines. The Hearing Journal, 52, 33-48.
Kochkin, S. (2001). MarkeTrak VI: The VA and direct mail sales spark growth in hearing aid market. The Hearing Review, 8(12), 16-24, 63-65.
National Institutes of Deafness and Communication Disorders (NIDCD). Statistics about hearing disorders, ear infections, and deafness. Accessed July 29, 2007, from www.nidcd.nih.gov/health/statistics/hearing.asp
Prendergast, S., & Kelley L. (2002). Aural rehab services: Survey reports who offers which ones and how often. The Hearing Journal, 55, 30-35.
Ross, M. (2004). Hearing Assistance Technology: Making a world of difference. The Hearing Journal, 57, 12-17.
Servedio, D. (2000). ALDs: It's time to take full advantage of this valuable, but underused, technology. The Hearing Journal, 53, 38-39.
Stika, C., Ross, M., & Cuevas, C. (2002). Hearing aid services and satisfaction: The consumer viewpoint. Hearing Loss, 25-31. Accessed July 29, 2007, from www.hearingresearch.org/Dr.Ross/HAsatisfaction_consumers.htm
Strom, K. (2002). The HR 2002 dispenser survey. The Hearing Review, 9(6),14-32.
Thibodeau, L.M. (2004). Hearing assistance technology (HAT) can optimize communication. The Hearing Journal, 57(11), 11.
Wayner, D. (2004). Integrating assistive technology into a hearing aid practice. The Hearing Journal, 57(11), 43-45.


