Editor’s note: This text-based course is a transcript of a live webinar. Download supplemental course materials. This course serves as a foundation for a second course that addresses the components of the written infection control plan, which is available in two formats - recorded webinar and text course.
Learning Outcomes
As a result of this Continuing Education Activity, participants will be able to:
- Identify at least two ways that HIV is transmitted
- Describe how HIV disables immune function
- Differentiate HIV-infection from AIDS based on accepted disease classification systems
Introduction
The terms HIV and AIDS, although sometimes used interchangeably, are certainly not the same thing. HIV refers to the Human Immunodeficiency Virus, whereas AIDS specifically refers to Acquired Immunodeficiency Syndrome. In other words, HIV is an actual microorganism; it's a retrovirus. AIDS refers to a disease state of an individual infected with HIV, who either exhibits specific disease manifestations and/or has reached an objective level of immunocompromise that meets established criteria.
Individuals infected with HIV do not necessarily have AIDS. In contrast, any individual who meets the definition of AIDS, must to be HIV positive. This point is going to be clearer later on when we address disease classification categories. There are two types of HIV: HIV-1 and HIV-2. Both HIV-1 and HIV-2 are transmitted in the same manner. For practical purposes, they really only differ from one another in terms of their respective geographic concentration.
For example, worldwide, the predominant virus is HIV-1. Generally, when people refer to HIV without specifying the type, they are most likely referring to HIV-1. The less common type is HIV-2, which is concentrated mainly in West Africa, and rarely occurs elsewhere.
There are also different subtypes or strains or HIV-1 that fall into three groups: Group M, which is the major group; Group O, which is the outlier group; and Group N, which is referred to as the new group. More than 90% of HIV-1 infections belong to the HIV-1 Group M. Within that group, it's interesting to note that there are at least nine genetically distinct subtypes of HIV-1. For the purpose of this presentation, reference to HIV will mean HIV-1, Group M.
Historical Milestones & Basic Statistics
On June 5, 1981, the first official documentation of what later became known as AIDS was published in the Centers for Disease Control and Prevention's weekly bulletin, the Morbidity and Mortality Weekly Report (MMWR). The original reported cases involved five gay males who are described as suffering from Pneumocystic carinii Pneumonia or PCP. PCP is an extremely rare type of lung infection that only develops in the presence of extremely severe immunosuppression. Now, a subsequent article reported similar PCP outbreaks in gay men in New York and Los Angeles with the additional presence of Kaposi sarcoma, another rare type of skin cancer that was uncommon in the United States. In addition, the same gay men manifested Persistent Generalized Lymphadenopathy or PGL which is a persistent state of swollen lymph nodes.
The development of a variety of opportunistic infections in a group of previously healthy and very young gay men resulted in the increased demand for Pentamidine. Pentamidine is an approved anti-fungal for the treatment and the prevention of PCP. The reason I bring this up is because these two very events started catching the attention of the scientific community, and amongst themselves, scientists started referring to this new disease as 'Gay-related Immuno-deficiency' or GRID. By the summer of 1982, infections that were mimicking GRID were also reported in individuals with hemophilia, which is a hereditary blood disease where the blood doesn't clot. Hemophiliacs often require numerous transfusions of clotting factors that are collected from the blood of many, many donors. This became the huge game-changer because the handful of hemophiliacs manifesting GRID type manifestations were not gay. They also were not intravenous drug users and had no history of such. At that point, these GRID manifestations were no longer considered a gay disease.
Acquired Immunodeficiency Syndrome or AIDS, was coined in July of 1982. Now, although it was suspected early on that AIDS was caused by a virus, it wasn't until 1983 that the virus was isolated by French researchers. These researchers referred to it as 'Lymphadenopathy-Associated Virus' or LAV. Around the same time, the National Institutes of Health (NIH) also isolated the same virus, which they referred to as “Human T Cell Lymphotropic Virus 3” or HTLV-3. This co-discovery of the same virus led to some really interesting political turf wars. The book And The Band Played On by Randy Shilts is very interesting and compelling read about the politics and people of the AIDS epidemic. I highly recommend it. In May 1986, the International Committee of Viral Taxonomy proposed to rename this HTLV-3 or LAV virus as the “Human Immunodeficiency Virus” or HIV.
According to the Joint United Nations Program on HIV/AIDS, as of 2014, there are approximately 40 million individuals worldwide living with HIV and approximately 2.3 million newly infected cases every year. In the United States, the CDC estimates that there are about one million individuals living with HIV, and approximately 50,000 newly infected cases occurring every year. Most recent studies suggest that about 16% of HIV positive individuals in the United States remain unaware of their HIV status.
HIV Transmission
Only certain fluids including blood, semen, vaginal fluids and breast milk from an infected person can transmit HIV. These very fluids must come in contact with a mucus membrane or damaged tissue, or be directly injected into the bloodstream from a needle or syringe for transmission to possibly occur. Mucus membranes can be found inside the rectum, the vagina, the opening of the penis, and the mouth.
HIV is mainly spread one of two ways: by having unprotected sex with someone infected with HIV; or, by sharing needles, syringes or other items used to prepare injection drugs with someone infected with HIV.
It's important for you to understand that while these are the two main ways that HIV is transmitted, there are other less common ways that someone can become infected with HIV. For example, HIV may be passed from mother to child during pregnancy and birth. It may also be transmitted during breastfeeding. HIV has been transmitted as a result of blood transfusions, blood products or organ tissue transplants contaminated with HIV, although this is extremely rare since the 1985 mandate requiring routine screening of blood products for HIV.
HIV can also be transmitted by being stuck with an HIV contaminated needle or sharp object. It can be transmitted by being severely bitten by a person with HIV where tissue damage is extensive and bleeding is present. There is no risk of HIV transmission if someone with HIV bites you and your skin is not broken; the bite has to be severe and extensive with bleeding. Finally, HIV can also be transmitted by contact between broken skin, wounds, or mucus membranes and HIV infected blood or blood-contaminated bodily fluids.
HIV Prevention
HIV prevention involves eliminating or reducing behaviors associated with HIV transmission. Since one of the main ways that HIV is spread is through unprotected sex, the number of sex partners one has will affect HIV risk. The more partners, the more likely a partner is going to have HIV. The Centers for Disease Control (CDC) recommends reducing the number of sexual partners. In addition, consistent and correct condom use remains one of the most effective ways of preventing HIV, as well as other sexually transmitted diseases, like gonorrhea and chlamydia. Latex condoms have been shown to provide the best protection against HIV. Pre-Exposure Prophylaxis (or PrEP) involves taking an HIV medication daily to prevent HIV infection. This is used in instances where an individual is HIV negative and involved in an ongoing sexual relationship with an HIV positive partner. There's also something called Post-Exposure Prophylaxis (or PEP). This is a preventative option for HIV negative individuals who are currently not involved in PrEP, who have had unprotected sex with somebody who may be or is HIV positive. PEP involves also taking HIV medications on a daily basis for about four weeks, and within three days of the initial exposure.
The second way that HIV is transmitted is by sharing needles or syringes. In terms of prevention, if an individual is unable to stop using injection drugs, other ways to reduce risk in these situations include the Pre-Exposure Prophylaxis meds. It also includes counseling the user to only use new needles or syringes for each injection, and making sure that the needles or syringes are never shared, as well as using sterile water to prep the drugs.
For HIV positive mothers concerned about transmitting HIV to their newborn, the risk of transmission will be greatly lowered when: the mother undergoes a C-section; the mother takes antiretroviral drugs during pregnancy, labor, and delivery; and the mother is counseled to avoid breastfeeding.
While the risk factors of HIV are essentially the same for everyone, there are some racial groups that are more affected by HIV than others. If we view HIV infection as a function of race and ethnicity, African-Americans are most affected by HIV. In 2010, African-Americans made up only 12% of the United States population, but they accounted for 44% of all new HIV infections. Additionally, Hispanics and Latinos are also strongly affected. They make up only 17% of the U.S. population, but accounted for 21% of all new infections.
HIV Mechanism / Disease Classification System
We're ready to tackle the HIV mechanism and the disease classification system. I would like to begin with an audience poll to test your existing knowledge. Think about your answers to the following questions - I will address the answers later in the presentation:
- Audience Poll #1: Every HIV positive mother will give birth to an HIV positive newborn – True or False?
- Audience Poll #2: In some cases, having AIDS and being HIV positive mean the same thing. True, false, or not sure?
- Audience Poll #3: The main target of HIV is the B Cell lymphocyte. True, false, or not sure?
- Audience Poll #4: Using established disease classification criteria, I can explain the difference between AIDS versus HIV in adults. True or False?
In order to understand the mechanism of HIV, it's important to briefly review how the normal immune system works. Blood is comprised of two distinct cell populations: red blood cells, and another group of cells referred to as leukocytes (white blood cells). One unique category of white blood cells is referred to as lymphocytes. Lymphocytes are white blood cells that are responsible for executing and managing all the activities of our immune system. There are several different types of lymphocytes, but the two that are important for today's discussion are the B Cell and the T Cell.
The B Cell lymphocyte fully develops in our bone marrow. The job of the B Cell is to recognize the presence of antigen. Antigen simply refers to any substance found within the human body that your immune system recognizes as foreign. When the B Cell identifies the presence of antigen, the B Cell itself is triggered to start mass producing antigen-specific antibodies. In order for the B Cell to start doing anything, it has to receive an activation signal. Once it receives an activation signal, the B Cell will send antibody throughout the body's fluids in order to allow the antibody to attach to the antigen so that it can neutralize and kill the antigen. Because another name for bodily fluid is humor, this entire process where the B Cell generates antibodies so that the antibodies can neutralize and kill the antigen is referred to as humoral immunity. It's a very important function that keeps us healthy.
We also have the T Cell lymphocytes. All T Cells initiate their maturation in the bone marrow. In order for a T Cell to become a T Cell, it has to pass through the thymus. Because thymus starts with a letter “T,” these cells are referred to as T Cells. There are several different categories of T Cells, but the one I want to focus on is the CD4 T Cell. The CD4 T Cell is responsible for detecting the presence of antigen. Unlike the B Cell that lets antibody do all the work, the CD4 T Cell is responsible for neutralizing and destroying the antigen. The CD4 T Cell attaches itself to the antigen in order to neutralize and kill it. Because the CD4 T Cell does all the work, it is referred to as cell-mediated immunity.
Let’s look at these two concepts together. First, we have the antigen, then CD4 T Cell comes in, and attaches itself to the antigen. The B Cell also recognizes the antigen, but doesn't do anything. The B Cell needs to receive an activation signal to start mass producing antibody. That activation signal comes from the CD4 T Cell. Once the signal is received from the CD4 T Cell, the B Cell starts mass producing antibody. Collectively, the antibody and the CD4 T Cell neutralize and kill off the antigen. This is how our immune system keeps us safe from a variety of infections.
What happens when we have HIV?
HIV is an antigen. As I previously indicated, the main target of HIV is the CD4 T Cell. The B Cell will come in and recognize the presence of HIV. At the same time -- whether it's because there aren't enough T Cells, or that the T Cells aren't strong enough to send an activation signal -- nothing happens in terms of cell-mediated immunity, and nothing happens in terms of humoral immunity. The immune system of individuals infected with HIV is weakened. As a result, HIV is able to grow freely. This patient population is extremely susceptible to infections, including those that are caused by ubiquitous microorganisms that we tend to take for granted.
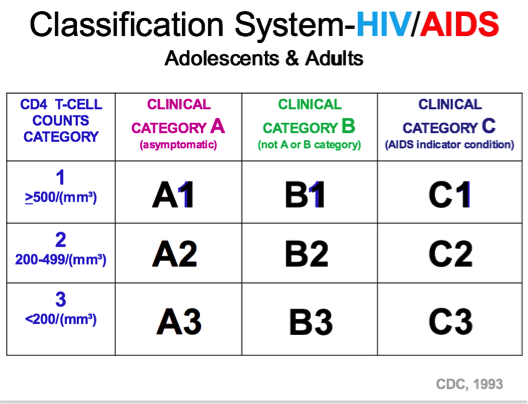
Let's take a look at the proposed classification system established by the CDC for HIV and AIDS (Figure 1). Since the primary target of HIV is the CD4 T Cell, it makes sense to categorize HIV positive patients as a function of their absolute CD4 T Cell counts. We have Category 1, which is designated for those HIV positive individuals with CD4 T Cell counts that are 500 or more. We also have Category 2 which is designated for HIV positive individuals whose CD4 T Cell counts range between 200 and 499 per cubic millimeters of blood. Then we also have Category 3 which is reserved for HIV positive individuals with CD4 T Cell counts of less than 200 per cubic millimeter of blood. As a point of reference, an adult in good health who is not infected with HIV will have approximately 800 - 1200 CD4 T cells per cubic millimeter of blood.
Figure 1. CDC classification system HIV/AIDS.
Because HIV is also associated with the development of a variety of opportunistic diseases, it also makes sense to stratify those individuals according to the presence or absence of common disease manifestations. There are three disease categories that are designated as A, B and C. Category A is reserved for HIV positive individuals who are essentially asymptomatic. They might have a little bit of PGL that I referred to earlier, but for all practical purposes, this group is asymptomatic. In contrast, we also have Category C which is on the opposite end of the spectrum. Category C includes HIV positive individuals who exhibit overt and severe stages of the immunocompromised as defined by a predetermined list of opportunistic infections known as AIDS Indicator Conditions. This is where you have the PCP and the Kaposi sarcoma and the Herpes Simplex categories or diseases. Then finally, we have Category B which is an in-between category where individuals are symptomatic, but they have less severe symptoms. Maybe Herpes Zoster, fever, diarrhea. To summarize, HIV positive individuals are going to be independently categorized according to two factors: their absolute CD4 T Cell counts, as well as the clinical category as it pertains to their manifestation of symptoms.
Regardless of what symptoms you manifest, as long as your CD4 T Cell count is 500 or higher, you will be designated in the number one category. Regardless of your CD4 T Cell counts, if you are asymptomatic, you will also be designated as being in the clinical Category A. This categorization system results in nine distinct categories associated with HIV and AIDS. The definition of AIDS is number one, regardless of your CD4 T Cell count, as soon as you exhibit a clinical Category C condition, you now have AIDS. In addition, regardless of what diseases you are manifesting, as soon as your CD4 T Cell count falls below 200, you now are considered to have AIDS. The groups with AIDS are C1, C2, C3, A3 and B3. The remainder groups (A1, B1, A2, B2) indicates individuals who are HIV positive, but they do not have AIDS.
A similar approach has been applied in classifying HIV positive children, although there are some adjustments that need to be made for the pediatric population for a couple of reasons. Number one, pediatric classification is complicated by the fact that maternal HIV antibodies cross the placenta. Therefore, all infants born to HIV positive mothers will test positive for HIV at birth. Furthermore, the majority of these infants will continue to generate false positives anywhere from nine months to 18 months of age, despite the fact that only about 15 to 25% of babies will truly be infected. Finally, the absolute CD4 T Cell counts for pediatric patients are not as straightforward as you see in adults. The normal ranges for CD4 T Cell counts are going to differ depending on the age of the child. In addition, we also have classification system related to disease manifestations that range anywhere from N which is no signs, A, mild, B, moderate, C, severe. As a result, for pediatric patients, there are more disease categories (a total of 12).
Just like we have seen in the adults, any time a child falls into the C group, or any time their CD4 T Cell count falls below a critical level, they are considered as having AIDS. C1, C2, C3, as well as N3, A3, B3 in children are considered to have AIDS. The remaining six categories of N1, A1, B1, as well as N2, A2, B2 are considered to be HIV positive. HIV and AIDS disease manifestations will occur either as a direct effect or an indirect consequence of HIV. Before I address those, we will discuss what happens in the beginning of the disease.
Course of Disease
HIV is very insidious in nature. The initial phase of the infection is visibly undetectable. Several weeks following exposure, a high majority of individuals experience inconspicuous flu-like symptoms (e.g., night sweats, diarrhea, nausea, vomiting). From the initial infection to the onset of symptoms, which is referred to as an incubation period, the infected person may feel and appear very healthy. Although it varies by individual, the incubation period averages from between eight to ten years. Potentially, it can take ten years for disease manifestations to occur in individuals who are HIV positive.
HIV is also associated with both peripheral and central nervous system manifestations in a very high percentage of patients – particularly in the later stages of the disease. These manifestations include hearing loss, tinnitus, and balance disorders. The occurrence of these disorders secondary to HIV and AIDS is much higher than in the general population. The literature suggests that anywhere from 75 to 90% of adults living with HIV and AIDS manifest these types of diseases. HIV disease manifestations may occur either as a direct or indirect consequence of HIV. While the exact mechanism of HIV remains unclear, direct effects include HIV induced damage to the cell, whereby HIV comes in and destroys all the different cells of the body. The direct effects are also as a result of neural dysfunction as a result of the CD4 T Cell being infected with HIV and it responds by releasing toxic substances, or there is some sort of physiological reaction that affects cell metabolism.
There are multiple things that HIV does to directly affect the peripheral and central nervous systems, although researchers are not 100% sure why. Opportunistic infections and ototoxicity are the two primary means that HIV may indirectly cause hearing or balance disorders. Opportunistic infections originate from very commonplace, ubiquitous organisms that don't produce infection in individuals with intact immune systems; rather they take the opportunity to infect a body that has some degree of immunocompromise which often results in very serious complications. Some examples of opportunistic infections are:
- Candidiasis
- Pneumocystic/Streptococcal Pneumonia
- Cytomegalovirus
- Cryptococcus Infection
- Toxoplasmosis
- Mycobacterium Infections
- Syphilis
- Staphylococcus Aureus
- Kaposi’s Sarcoma
- Herpes Zoster
Many of these opportunistic infections regardless of your HIV status, are associated with causing different forms and degrees of hearing loss. In addition, ototoxicity is very common in patients with HIV.
In the absence of a vaccine, the medical management of HIV relies on numerous pharmacological interventions where patients are ingesting both FDA approved, as well as experimental antiretrovirals. In addition, many HIV infected individuals are prescribed medications as a prophylaxis for the treatment of some of the opportunistic infections. The HIV infected population is prescribed a lot of medications, and many of these medications are known to cause sensorineural hearing loss, tinnitus, vestibular and balance issues.
Although Hispanics and Latinos are influenced more so than many other groups, the African-American ethnicity is most affected by HIV/AIDS in the United States.
Answers to Audience Polls
Poll #1: Every HIV positive mother will give birth to an HIV positive newborn – True or False?
Answer: This is true. What's important to understand is when you test a baby, they're going to test positive because they have the mom's antibodies. They can continue to test positive anywhere from nine to 18 months. Current data suggests that in HIV infants born to HIV infected mothers, only 15 to 25% of those babies will be truly infected with HIV.
Poll #2: In some cases, having AIDS and being HIV positive mean the same thing – True or False?
Answer: The most correct answer to this is false. HIV and AIDS are two totally different things. Just because you're HIV positive doesn't mean you have AIDS, but in order for you to meet the definition of AIDS, you have to be HIV positive.
Poll #3: The main target of HIV is the B Cell lymphocyte – True or False?
Answer: This is false. The B Cell lymphocyte is not the main target. The main target of HIV is the CD4 T Cell. Because the CD4 T Cell helps the B Cell, it's very unfortunate because attacking the CD4 T Cells strips anybody of their Cell-Mediated and Humoral Immunities, and this patient population is very susceptible.
Poll #4: Using established disease classification criteria (using the information presented today), I can explain the difference between AIDS versus HIV in adults? Which of the following meet the definition of AIDS in adults?
a. Someone with a CD4 T Cell count of less than 200 but they're asymptomatic
b. Someone with a CD4 T Cell count of 800 and they have Herpes Zoster
c. Someone with a CD4 T Cell count of 505 but they have PCP
d. Someone with a CD4 T Cell count of 1,200 and they just have swollen lymph nodes
You can have more than one answer to this question. Anytime you have a T Cell count less than 200, regardless of the fact that you're asymptomatic, you have AIDS - so answer A is correct. In addition, even though you have a good CD4 T Cell count, anytime you have an AIDS indicator condition such as PCP, you are considered to have AIDS - so answer C is also correct.
HIV Influence on Patient Care
The discovery of HIV had a tremendous impact on how healthcare services were to be delivered, creating a domino effect of new policies and procedures. During the 1980s and early 1990s, a variety of agencies, governing bodies and expert panels (including the CDC and OSHA) offered guidelines and enacted regulations. Included in the new guidelines were universal precautions, body substance isolation, and standard precautions summarizing how to reduce or eliminate the risk of the exposure to infectious agents. To give you a better idea of what occurred, in 1983, when HIV was first isolated but it was yet unnamed, the CDC published a document called the CDC Guidelines for Isolation Precautions in Hospitals. This document outlined precautions for handling blood and body fluids, including the use of personal protective equipment (gloves, masks), as well as sterilizing certain critical instruments in instances when a patient was either known or suspected to have some sort of infectious blood-borne disease.
In 1985, as a direct response to HIV and AIDS, the CDC expanded the original blood and bodily fluid precautions by specifically addressing the prevention of HIV transmission to healthcare workers. Two years later, in 1987, the CDC once again increased the scope of their guidelines recommending that blood and bodily fluid precautions be consistently applied to all patients in healthcare environments, regardless of their HIV or other blood-borne disease infection status. This approach to treating blood, as well as other bodily fluids, as if they were infected with HIV became known as Universal Precautions. Not to confuse the issue, that very same guideline offered another set of rules referred to Body Substance Isolation, or BSI. The BSI guidelines shared many of the same features of Universal Precautions, with the additional emphasis for healthcare workers to also avoid all bodily fluids, including moist bodily substances (such as urine or nasal discharge, etc.) as a means of minimizing the potential spread of disease.
In 1991, to maintain the most up-to-date isolation practices, the CDC, in addition to an expert committee, established updated guidelines for isolation precautions in hospitals. These guidelines include two tiers of precautions to prevent the transmission of infectious agents. These two tiers of precautions include standard precautions, and the added transmission-based precautions in certain situations. Standard precautions refer to a set of precautions that are designed to prevent the transmission of disease in the clinical environment. These standard precautions combine all the elements of universal precautions, along with some key features of the BSI system. Just like the universal precautions, standard precautions are based on the mindset that all human blood and certain bodily substances are potentially infected with HIV, Hepatitis B or other blood-borne pathogens. Standard precautions also incorporate elements of the body substance isolation system, whereby all bodily fluids (including moist substances), as well as ubiquitous microorganisms are deemed potentially infectious. Standard precautions apply to the care of all patients, regardless of presumed or known diagnosis. As such, all patients must be treated with the same basic level of established protocol.
The five main elements of standard precautions include:
- Appropriate personal barriers
- Hand hygiene
- Disinfect touch and splash surfaces
- Sterilize critical instruments
- Dispose infectious waste
You might be asking yourself, "As an audiologist, what does this have to do with me?" With regard to infection control, HIV is not our only concern. As audiologists, we do come in contact with bodily fluids, particularly when we're dealing with cerumen. We are also in a position where we make multiple contacts with multiple objects and multiple patients throughout the day. These situations increase the potential for many types of disease transmission to occur. We need to minimize these cross-contaminations to avoid infection.
The first two things that microorganism needs to potentially cause infection is a mode and a route of disease transmission. A mode refers to how the microorganism gets from the environment to the vicinity of the human body. This can occur in many different ways, including direct contact (e.g., touching a draining ear with your bare hands), or indirect contact (e.g., handling contaminated objects). Once a microorganism has a mode, it needs a route, or portal of entry, into the body. Normal portals of entry include dry chapped hands, as well as natural orifices of the body including the nose, the eyes, the mouth, and the ears. While many other things need to happen after a microorganism enters the body, our responsibility as audiologists is to control the mode and the route of microbial transmission in the clinical environment. The cornerstone of an effective infection control plan is the actual written infection control plan that OSHA requires. In part two of this series, we will address the written infection control plan.
HIV Take-Home Points
HIV is mainly spread through unprotected sex and/or intravenous drug use with someone who is HIV positive, although there are other less common ways that HIV can be transmitted. The virus attacks the CD4 T Cell which compromises humoral and cell-mediated immunities. These patients are extremely susceptible to a variety of opportunistic infections, many of which are associated with audiological consequences in the form of hearing loss, balance disorders, and tinnitus. HIV has been the catalyst of infection control. It changes the way that healthcare professionals are required to provide professional services.
If you have questions, I can be reached via email: [email protected]. In addition, on my blog, AUBankaitis.com, there is an infection control section that lists some of the more up-to-date pieces of information.
Questions and Answers
As new research comes out about HIV, how do you keep up?
Dr. Bankaitis: That's a really good question. Regarding infectious diseases in general, CDC does a very good job in updating their guidelines. For example, since HIV was first found in the mid-1980s, there have been several renditions of the CDC guidelines.
One of the most significant recent updates had to do with the fact that, when it comes to infection control, we need to be concerned with more than just blood and other obvious bodily fluids. We also need to be careful about generally ubiquitous, every day, run-of-the-mill microorganisms like Staphylococcus. Research has shown that the surfaces of hearing aids are contaminated with bacteria and fungi that are not necessarily part of the normal ear canal flora. Therefore, if we don't practice infection control procedures, we run the risk of passing on a disease.
In the future, I expect a little bit more of a tightening of the guidelines. I should also mention that in 2006, the CDC released another revised recommendation regarding to HIV testing. They have asked every healthcare facility adapt a policy of routine HIV testing for everyone between the ages of 13 and 64, as well as all pregnant women. HIV screening continues to be voluntary, but the CDC recommends what is called 'opt-out screening'. This means that the physician will recommend an HIV test as part of routine care. Unless a patient explicitly refuses to have an HIV test, he or she will get tested for HIV. In the past, you were only tested for HIV if you exhibited some specific manifestations or risk factors. Now, with the opt-out screening, the screening will occur unless the patient explicitly refuses.
Do patients have any obligation to disclose an active disease they may have?
Dr. Bankaitis: It’s important to know that confidentiality of HIV testing is paramount, not only to ensure patient sensitive information remains private, but that you as an healthcare practitioner are abiding by established laws. There are different laws for different states, so I'm going to use Florida as an example. Patient test results in Florida cannot be revealed to anyone other than the patient, the patient's legally authorized representative, the healthcare provider - and that usually means the physician involved in the patient's care as it pertains to HIV status - and to those who have written authorizations.
In Florida, therefore, it is not necessary for a patient or for a physician to necessarily disclose HIV status to you. The bottom line is that it is very important to check with your state laws. I think most people assume that if you are HIV positive, you have to legally disclose it, but you do not have to disclose it. The reason they don't have to, is because healthcare professionals should be practicing in a manner that minimizes the spread of disease, and assume as if every patient you see has a potentially infectious disease.
Citation
Bankaitis, A.U. (2016, April). HIV/AIDS overview: Catalyst for change in infection control. AudiologyOnline, Article 16913. Retrieved from www.audiologyonline.com