Question
How Can the Video Head Impulse Test Improve the Diagnosis of Vestibular Disorders in Children?
Answer
Epidemiology
Vestibular dysfunction is increasingly recognized in pediatric populations presenting with balance disorders. Epidemiological studies report a prevalence of up to 36.5%, a figure that rises significantly among children with sensorineural hearing loss (SNHL). In a cohort of 1,022 children not eligible for cochlear implantation (CI), vestibular abnormalities were detected in 54.5% of cases. Notably, mild vestibular deficits often remain undiagnosed due to effective compensation strategies and the absence of overt postural symptoms, thus escaping early neurotological evaluation.
The Vestibular System: From Balance to Cognitive Skills
The vestibular system is fundamental for postural control, spatial orientation, and the coordination of voluntary movements. Its integration with the central nervous system, particularly the cerebellum, and its interaction with auditory, visual, proprioceptive, and cognitive systems support both motor and higher-order functions. Through complex afferent and efferent pathways, the vestibular system ensures fine-tuned modulation between body position and the external environment.
Dysfunctions of the peripheral or central vestibular system cause balance disorders. In adults and in children between 7 and 12 years of age, a vestibular deficit affecting postural control can often be compensated by somatosensory and visual inputs. In contrast, during early development, the nervous system is not yet mature enough to compensate for vestibular deficits because of the immaturity of other sensory systems and the CNS itself. As a result, a child with a vestibular deficit who walks cautiously and attentively may fail to adequately learn spatial relationships within the environment. This can hinder the development of internal spatial representations, leading to delayed motor milestones and impaired postural and motor skills.
A theoretical framework on the emergence of cognitive representations in the brain suggests that sensorimotor circuit activity can be internally simulated and re-represented in the absence of direct sensory input or movement, facilitating anticipatory control and the emergence of cognitive representations. Evidence indicates that the vestibular system contributes to cognitive domains such as spatial navigation, body schema formation, numerical processing, and temporal cognition. Furthermore, vestibular afferents are involved in building a sense of agency (the sense of being the agent of actions), ownership of actions (“this action was mine”), and a more global sense of belonging to one’s body (“this body is mine”), all key components of self-awareness.
At the same time, third-person perspective taking (the visual-spatial ability to temporarily adopt the viewpoint of another individual) is essential for understanding whether an object is to someone’s left or right. This rapid and involuntary ability helps predict other people’s feelings and intentions and forms the basis of empathy.
Given these mechanisms, it is plausible that vestibular dysfunction may contribute to learning disorders, which are classified among neurodevelopmental disorders in the DSM-5. These include dyslexia, dysorthography, dysgraphia, and dyscalculia. They typically emerge during school age and significantly interfere with academic skills despite normal intelligence and motivation. Children with autism spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD), or other communication and intellectual disorders often show overlapping impairments in language, praxis, executive functions, and spatial reasoning. Moreover, increasing levels of childhood obesity and sedentary behavior (e.g., smartphones and tablets) promote the reduction of muscle activity and vestibular synapses. All these conditions can cause long-term personal discomfort and difficulties with social integration.
Vestibular Assessment in Pediatric Age
All children with suspected balance or developmental disorders should undergo a complete ENT and audiological evaluation. Vestibular assessment must be tailored to both age and level of cooperation, using tools validated for pediatric populations.
Thanks to ongoing advances in diagnostic technology, objective and non-invasive methods, such as cervical Myogenic Vestibular Evoked Potentials with air or bone stimulation (air/bone cVEMPs) and, above all, remote camera Video Head Impulse Test (vHIT), allow for accurate evaluation even in very young children.
In infants under one year of age, clinicians can detect the presence of the vestibulo-ocular reflex (VOR), Doll’s eye reflex, and primitive reflexes.
Between one and three years of age, assessment focuses on observing posture, strength, and coordination during spontaneous movements and play, including walking, running, and interactions with the environment and parents. When feasible, and depending on the child’s ability to cooperate, key tests should include: saccadic and smooth pursuit eye movement evaluations; Frenzel glasses or infrared video goggles to search for spontaneous, positional, and positioning nystagmus; Head Shaking Test (HST); vHIT; and air/bone cVEMPs.
For children older than three years, nearly all vestibular diagnostic tests used in adults can be performed.
How to Perform vHIT in Children
The test follows the standard adult protocol, with a few age-appropriate adjustments:
- Build trust by welcoming the child into a friendly environment with toys or dolls.
- Once the child feels at ease, have them sit on the caregiver’s lap facing the remote camera.
- Use a visual target made of colored concentric circles or another eye-catching object that gradually decreases in size.
- Deliver head impulses while the child focuses on a target about 2 cm in diameter; if cooperation is limited, larger targets can be used.
At least five valid impulses per side are needed. Repetitions may be necessary to compensate for blinking, inattention, or spontaneous movements. Lateral and vertical canal hypofunction are defined as gain values below 0.8 and 0.7, respectively.
Case Reports
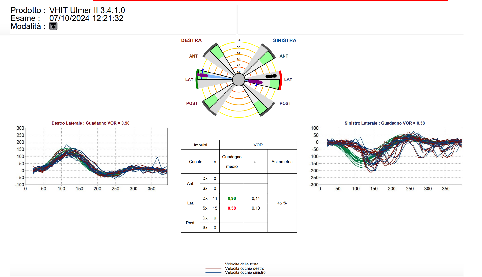
- Case 1: Figure 1 shows normal vHIT results in RB, a 12-month-old female with severe, bilateral, and symmetrical sensorineural hearing loss. Excellent compliance allowed full evaluation of all semicircular canals.
- Case 2: Figure 2 shows vHIT results in AG, a partially compliant 11-month-old male with moderate, bilateral, and asymmetrical sensorineural hearing loss. Only horizontal canal responses were reliably obtained, showing normal gains bilaterally.

- Case 3: Figure 3 shows vHIT results in ER, a partially compliant 14-month-old male with severe, bilateral, and symmetrical sensorineural hearing loss who underwent cochlear implantation in the right ear at 11 months. The child demonstrated clumsiness and unstable walking, with frequent falls, especially in dim lighting. vHIT revealed left lateral canal hypofunction, while the right canal (CI side) was normal.
Discussion and Conclusion
Early identification and management of vestibular dysfunction in children are essential to optimize motor and cognitive development. This requires a multidisciplinary approach involving clinicians, families, and educators, as well as broader public awareness initiatives. The video head impulse test (vHIT) is a valuable, feasible, and reproducible tool for assessing semicircular canal function in children with sensorineural hearing loss (SNHL), balance disorders, or even in those without apparent symptoms. Universal vestibular screening, extending beyond high-risk or symptomatic populations, should be considered to prevent diagnostic delays.
Timely vestibular rehabilitation is crucial in confirmed cases of deficit.
Moreover, vestibular-based interventions may benefit children with learning difficulties even when vestibular function is normal. Vestibular re-education through playful activities such as swinging, rolling, somersaults, trampoline use, and cycling, can stimulate the sensorimotor system and support neurodevelopmental trajectories.
Promoting knowledge exchange and developing age-appropriate, evidence-based vestibular training programs are fundamental to enhancing academic performance and fostering psychosocial integration.
References
- Wiener-Vacher SR, Hamilton DA, Wiener SI. Vestibular activity and cognitive development in children: Perspectives. *Front Integr Neurosci.* 2013;7:92. doi:10.3389/fnint.2013.00092
- Van Hecke R, Cass SP. Evaluation of vestibular function in children. *Curr Opin Otolaryngol Head Neck Surg.* 2021;29(5):378-384. doi:10.1097/ MOO.0000000000000725
- Cushing SL, Papsin BC, Rutka JA, James AL, Gordon KA. Vestibular function after cochlear implantation in children with sensorineural hearing loss. *Otol Neurotol.* 2008;29(3):347-352. doi:10.1097/ MAO.0b013e3181662e13
- Rine RM, Wiener-Vacher SR. Evaluation and treatment of vestibular dysfunction in children. *NeuroRehabilitation.* 2013;32(3):507–518. doi:10.3233/NRE-130877
- Jacob R, Palla A. Head impulse testing and video-oculography in vestibular disorders. *Curr Opin Neurol.* 2016;29(1):1–8. doi:10.1097/ WCO.0000000000000277
- Taylor D, McDonnell M, Lee M, Curthoys IS. The video head impulse test (vHIT) in children: normative data and test-retest reliability. *Int J Pediatr Otorhinolaryngol.* 2015;79(10):1659–1663. doi:10.1016/j. ijporl.2015.07.025
- Lopez C, Blanke O. The thalamocortical vestibular system in animals and humans. *Brain Res Rev.* 2011;67(1-2):119-146. doi:10.1016/j. brainresrev.2010.12.002
- Bigelow RT, Agrawal Y. Vestibular involvement in cognition: visuospatial ability, attention, executive function, and memory. *J Vestib Res.* 2015;25(2):73-89. doi:10.3233/VES-150544
- American Psychiatric Association. *Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM- 5®).* Washington, DC: American Psychiatric Publishing; 2013.
- Lacour M, Bernard-Demanze L. Interaction between vestibular compensation mechanisms and vestibular rehabilitation therapy: 10 recommendations for optimal functional recovery. *Front Neurol.* 2015;5:285. doi:10.3389/fneur.2014.00285
Resources for More Information
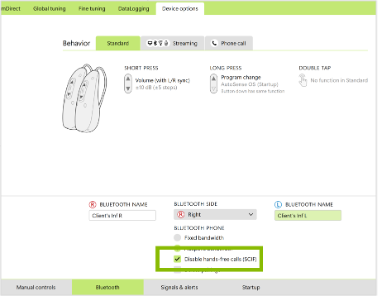
In the two videos presented here, Dr. V. Marcelli, MD demonstrates how SYNAPSYS vHIT enables reliable vestibular assessment in pediatric patients. These real-life demonstrations provide valuable insights into practical strategies for testing children and highlight the essential role of early vestibular evaluation in supporting healthy motor and cognitive development.
For more information about Inventis, visit https://www.inventis.it/en-na

