Editor's Note: This is a transcript of the live seminar presented on Novermber 9, 2011 as part of the ReSound online symposium, Advances in Amplification: Meeting the Needs of Aging Adults. To view the course recording, register here. While a few of the images from the presentation have been included in this transcript, please download the pdf of the slide presentation for all images including charts, graphs, etc.
We are going to talk today about auditory aging. We are going to talk a lot about what you can do for older adults with hearing loss above and beyond hearing aids, and this will put hearing aids into a much bigger context.
We are going to try to put ourselves in the shoes of an older adult with hearing loss. The following is a note that was passed to me by someone from the Canadian Hard of Hearing Association after she heard me do a lecture at one of their meetings about aging and hearing loss. This person says, "When you are hard of hearing, you struggle to hear. When you struggle to hear, you get tired. When you get tired you get frustrated. When you get frustrated you get bored. When you get bored you quit." Then she said, "I didn't quit today." I think this note captures why it is important for us to put the issues of older people with hearing loss into a broader context. She was talking about the struggle and effort to keep listening and how it affects her emotionally, and her ability to participate socially.
Over the course of the first hour today we will focus on the connection between hearing and cognition and aging. There is going to be a good guy and a bad guy in this story. On one hand, how does hearing loss, the bad guy, aggravate cognitive problems and make it more difficult for older adults? On the other hand, could improving hearing loss be the good guy and actually help cognitive health? In the second hour we are going to make a progression from cognition to how psychosocial factors could be incorporated into rehabilitation to improve outcomes. Aging is the new frontier, and I think it will resonate with some of your clinical intuitions.
The number one problem that older adults have is understanding in challenging listening conditions. Their problem understanding does not occur in quiet, and really, if everybody lived in a soundproof room we would not have much business to do. If people are in ideal listening situations, wearing good hearing aids, and do not have much hearing loss, they will really not have a lot of difficulty. The difficulty occurs in challenging listening conditions, and unfortunately, these are situations that they encounter frequently in everyday life. It is not just noise. It is not just masking. These challenges include how to interact with multiple talkers in a group conversation, how to deal with people who have foreign accents, changing topics within a conversation, multi tasking while listening and listening when things are happening at a fast pace. I would also say that getting used to a new hearing aid is a challenge (as there are extra demands put on people when they have to go through that experience) that we could possibly frame in a more supportive fashion, especially for older adults.
In these difficult situations, the ultimate risk is that the listener will withdraw from social interaction and become socially isolated. So, although we start with a hearing problem and we travel through some cognitive problems, can someone continue to participate socially? That is a good way to see the end of the road in sight. How are we going to keep people functioning socially?
Difficulty in Noise
People have trouble in difficult situations, including noise. We can measure how much deficit they have, in terms of signal-to-noise ratio (SNR), by using standardized tests. This is a way of quantifying difficulty that may feel comfortable to you as clinicians. One example is the speech perception in noise test (Bilger et al., 1984). This test uses 8 sets of 50 sentences , where half of the sentences in a set provide a context for the final word (high context) and half do not (low context). For example, if the target word that the person is supposed to respond to at the end of the sentence is feast, a high-context wording would be, "The wedding banquet was a _______." A low-context example would be, "John did not talk about the _______.". Generally speaking, younger as well as older listeners with presbycusis perform well when the SNR is high. When the SNR is low, the groups all perform poorly. But in the middle SNR range, we have problems when there is low context, but people still maintain good performance when there is high context. The ability to use non-auditory cues is evident by the performance curves splitting apart (Figure 1; Pichora-Fuller, Schneider & Daneman, 1995); that is when you are thinking differently about the sound you are hearing. I am going to refer to this as the zone of effort for listening. Where the young person is able to score 50% correct at a SNR for these materials of 0 dB SNR, an older adult is going to need about 3 dB SNR. This means that the older adult needs to have a 3 dB advantage in terms of SNR to get the same score as a younger adult without context, even when the older adult has a good audiogram.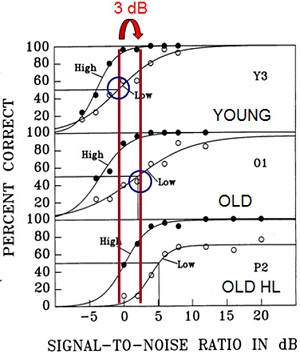
Figure 1. Signal-to-noise ratio comparison between younger, older, and older listeners with presbycusis for a 50% correct score on a word recognition task in noise. The red lines represent the difference between the young listener and the old listener on a low-context task, which equates to 3 dB SNR.
As we are going to see later, the older adults actually have a very interesting way of catching up by using context. We can quantify this problem that older adults have by looking at this chart of performance (Figure 1). If we had technology that could give us the needed 3 dB for older adults, would we overcome all of the problems? Well, it would be a good idea, but maybe it is not going to overcome all of the problems.
Audiograms and Auditory Aging
How else can we understand age related hearing loss? One typical way you might define age-related hearing loss is in terms of the audiogram. The prevalence of age related hearing loss increases with age. The typical age for first-time hearing aid use is about 70 years globally. If we look at the range of 70 to 75 years, about half of the population would have a hearing loss. Figure 2 shows the International Organization for Standardization (ISO, 2000) standards for audiograms as a function of age for men and women.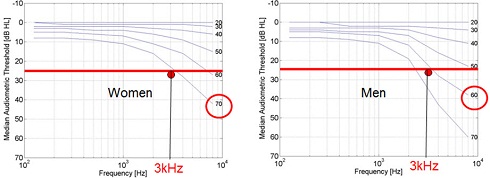
Figure 2. Median hearing thresholds in dB HL as a function of increasing age for men versus women. The red line represents the level of normal hearing (25 dB HL). Comparatively, men suffer more hearing loss than women at 3000 Hz, and at an earlier age.
I am going to discuss research that we did with people who are at the median for their age. These curves are for the median, for different ages spanning from 20 year olds up to 70 year olds. At 3000 Hz, we can see the intersection at 25 dB where we have the boundary between normal and mild hearing loss. We see that men begin to hit this point at around age 60, which is a little younger than the women, where we see the intersection around age 70.
We understand that there is a lot more that happens with aging other than these changes in the audiogram. I would recommend the book edited by Gordon-Salant, Frisina, Popper and Fay (2009) entitled The Aging Auditory System for a comprehensive discussion of this topic. An article published in Seminars in Hearing by Jack Mills' and colleagues (2006) based on their animal research in gerbils described what accounts for these high-frequency hearing losses. In some cases there has been noise-related damage to the outer hair cells, which is not particularly unique to aging. They are very interested in changes in the endocochlear potential, which also result in high-frequency hearing loss. All high-frequency hearing losses are not necessarily due to the same cause, and these changes in endocochlear potentials are unique to older individuals. This could include people who do not have problems with their otoacoustic emissions. People are trying to find clinical ways to sort this out, but we have not quite gotten there yet.
Another interesting area of research is what seems to be neural types of hearing loss. There is very interesting work by Liberman and his colleagues in neuroscience (e.g., Kujawa & Liberman, 2009). showing that animals that have been exposed to relatively low levels of noise, even when their audiogram and otoacoustic emissions look fine, could have permanent neural damage, which may be the secret behind why older adults have trouble understanding speech in noise. One of the apparent consequences of this neural damage is changes in temporal processing.
To summarize, with auditory aging, we do have audiometric changes. There are a few different etiologies. First is loss of audibility which can occur. Even in people that do not have much audiometric loss, there are different levels of temporal cues that we could examine. We could look at the large fluctuations in the speech envelope that correspond to syllables. We could look at the gaps, the onsets and the offsets and the durations that correspond to things like stop consonants. We could look inside the vowels, or at the fine structure of the voice that tells us things about who is talking and what their mood is like. There are definitely characteristics of temporal cues that are not working quite so well for aging adults.
One way we looked at quantifying these temporal difficulties was with the Speech, Spatial & Qualities of Hearing Scale (SSQ; Gatehouse & Noble, 2004). There is an upcoming paper to be published in February of 2012 in the Journal of the American Academy of Audiology on the following results (Banh, Singh, Pichora-Fuller, 2012). We administered the SSQ questionnaire to people in the top half of the distribution who had good audiograms, and we compared them to older people who have hearing loss. There were clear differences between older people with hearing loss and older people with good audiograms. Obviously, people with normal hearing do better on the SSQ. But what was interesting was the comparison of older adults with good audiograms against younger adults. We found that on almost every question there was a significant difference. So, despite the fact that the audiograms are good, the older adults will tell you that they have different types of problems listening in everyday situations. These problems are not related to the audiogram, because all of those older people with good audiograms do not have much pure-tone loss.
If we look at the Words in Noise test (WIN; Wilson et al., 2003) and see that they had trouble in noise, even though they did not have very significant problems with their audiograms, we still do not find a correlation between the WIN and the SSQ. This means that some of the problems that the SSQ is picking up are actually not very correlated with words and noise performance. There were many results on the SSQ for older people that are not being well predicted by either their pure-tone audiogram or their WIN results.
Looking at a person's ability to hear in noise does not tell us the whole story. If we look at the questionnaire items where there are the biggest age differences, we start to see some things that appear to be more cognitive, such as focusing, switching attention, conducting a conversation, or talking to people in a group. On the spatial part of the scale, we saw differences in things like understanding the motion of sources, which includes vehicles approaching. This is obviously quite important to overall safety. And then under the quality scale, we have the common complaint of sounds appearing jumbled. There are auditory problems and temporal processing problems. In addition to that, there seem to be some real cognitive problems. It comes as no surprise that some cognitive problems also increase with age.
Cognitive Aging
In a nutshell, there are two things that are important to know about auditory aging. One is that not everything declines with age. Knowledge, things like vocabulary and information about the world, is very well preserved in old age, and this is why using context is so helpful for older people. This is a strength that we should capitalize on in rehabilitation. The things that go wrong in aging from a cognitive perspective are when we have to manipulate or process information and there are specific kinds of processing that are affected. Cognitive psychologists would think in terms of working memory abilities being reduced, speed of processing slowing and problems with attention, especially divided attention. We will examine these cognitive changes with respect to hearing. And, just as a warning, many of these things look worse in older people because there are cognitive by-products of the testing design, and some factors are actually aggravated if people have sensory problems that are not corrected. There is a real contribution that we have to make to try to keep older people on track by making sure that they have quality input.
Working Memory
Let's start with working memory. Working memory is this idea that memory is not just about the capacity to store information; it is also the ability to use it. If we have people with audiograms or hearing aid fittings that are pretty much the same, some of them go out and do better understanding in everyday life than others. What could be different between those people? Maybe they are different in terms of their working memory. In fact, there are important individual differences in healthy people in terms of working memory. I could give you a list of numbers and ask you to remember them, and that would measure how many items you could store. If I asked you to do mental arithmetic and calculations that would be asking you to also process information. Because you have a limited capacity, the more calculations you have to do, the fewer numbers you could store at the same time. You have to allocate capacity to storage and processing, and the more processing that you have to do the less is left over for storage. This is the principle behind the idea of measuring working memory (Baddeley & Hitch, 1974; Daneman & Carpenter, 1980).
If we go back to listening in noise, we have zones of effort for listening (Figure 1) where people are getting words right, especially in the case of high-context items. However, they are using context to get help to get the items correct. They are doing a different kind of listening -- the kind of listening you do when you are sitting on the edge of your chair really concentrating. If we wanted to take away the disadvantage that older adults have, in terms of needing that 3 dB SNR, we could do cognitive tests where everyone achieves the same performance on words in noise. If we pick the individual SNR where this person gets 50% right without context, and a different SNR for each subsequent person so that every person being tested can get 50% of the words right without context, we can equate them in terms of the effort required for each listening condition and see what happens to them if we do a cognitive test.
One example of such a cognitive test is understanding a simple story. If older adults and younger adults are tested without that correction factor, there are significant age differences; however, when the SNR is corrected, the age differences go away (Schneider, Daneman, Murphy, & Kwong See, 2000). This is the first indication that correcting for those perceptual disadvantages could make some of the apparent cognitive differences in aging go away.
Another way we have tried to do this is by using a temporal distortion of the speech in noise sentences. We used both jittered sentences in speech babble and intact sentences in speech babble. Just a little bit of distortion puts a young listener in a level of difficulty that turns out to be about the same as an older person listening to an intact version of the sentence (Pichora-Fuller, Schneider, MacDonald, Pass & Brown, 2007). We took the original results for young and old listeners on the original, unaltered sentences. We then looked at the young people listening in jitter, and, in terms of understanding words, they performed the same as the older people listening to intact sentences.
We also measured their memory span. If they listened to two sentences in a set, how many of those words could they recall later? Everyone performed well because there were only a few items to recall. However, when we increase the number of items, the young people could remember more than the older people, but when the young people listened to the sentences with jitter, they remembered fewer, similar to older people. Again, this is evidence that some of what looks like cognitive changes in aging are actually the result of difficulties in hearing.
What emerges is this idea that there are inter- and intra-individual differences in cognitive abilities. There are differences in cognitive abilities between people, obviously, but there are also differences within a person. This could be relevant when we are considering who will be able to acclimate easily to a hearing aid.
Say we have someone with a certain listening capacity in quiet. When we put that person in noise, they will use more of their capacity to try to figure out what they are hearing by using context or other information. Their working memory span (how many words they can store and recall later) will be reduced as they are put in more difficult processing situations. This measurement of how much people can remember is inversely related to how much they are processing.
Does putting on a hearing aid reduce a person's consumption of processing capacity? If so, then as processing consupmption goes down, they would remember more of what they heard with their hearing aid. This turns out to be an outcome measure that some of the hearing aid manufacturers have had success in using to evaluate hearing aids (e.g., Sarampalis et al., 2009).
The end of this story is that older adults absolutely have audibility issues. We can overcome those issues by studying people who have good audiograms or by providing amplification. When we equalize the groups, we find out that some of the cognitive consequences are not particularly specific to older adults, regardless of the audiogram or how old you are. When the listening condition gets harder, you are going to have some cognitive stress. Older adults are not actually special except that they live more of their life in a world which is acoustically hostile to them where the SNR is not corrected as it is in our experiments.
Cognitive Neuroscience of Aging and Brain Plasticity
Having done effortful listening studies for decades, we know older adults experience physiological changes in their brain. The brain, in its "default" mode, is habituated to chronic, effortful listening. When people have done brain imaging to compare younger and older people on a variety of perceptual or cognitive tasks, and they compare the groups when they are performing the same task at the same score or level, there is more widespread activation in the older brains than in the younger brains. Older people are doing more work with their brains to achieve the same results. Some people think about this as a way in which older listeners are compensating for their difficulties. The idea of this expansion in the areas of the brain which are used to process information has been described in the Harold model by Cabeza (2002). He recently expanded this to what he calls the PASA model: posterior-anterior shift in aging (Davis, Dennis, Daselaar, Fleck & Cabeza, 2008). This model takes into account the sensory input that comes in to the posterior part of the brain for vision and hearing. As that decreases with age, more of the frontal areas of the brain, where knowledge is stored, are used in order to get the job done.
Different areas of the brain are accessed depending on the type of signal and the context surrounding the message. Results of a study by Obleser and colleagues (2006) indicate that a large area of the brain is activated for listeners presented with either high- or low-context SPIN sentences. Only a very limited portion on the brain is activated, in contrast, when sentences have low context. Much more of the brain is put to work when you are listening to sound and it is helpful if you can access context. Using context is especially useful when the input materials are distorted. The cortical areas that are activated are exactly the areas that psychologists understand to be associated with working memory and semantics or processing of knowledge. That is further evidence that when you are listening in noise you are actually listening in a different way.
If we go back and look at the difference between scores on high- and low-context sentences (Pichora-Fuller et al., 1995), the benefit from having context is equivalent to about a 4 dB SNR shift for the young person listening to intact sentences or when the young person is listening to jittered sentences. So yes, young people use context but they seem to saturate on how well they can do it - their 50% score for high-context sentences is about the same as their 50% score for low-context sentences presented at a 4 dB better SNR whether the materials are intact or distorted by jitter. If I put young listeners in a novel distortion, they are not going to be any more expert at using context. The older people, who are experts at using context, actually get about a 2 or 3 dB greater benefit from context. Isn't that interesting? It balances the 2 or 3 dB SNR that they are missing from the signal when we look at their performance on low-context sentences. This is an interesting balancing effect that happens. As listening becomes effortful, older adults have less efficient use of the signal and some compensation from using knowledge. As we travel from easy listening to hard listening, we have a trading of these two.
In other words, as listening becomes more effortful, bottom-up processing (ear to brain) becomes less efficient and top-down processing (brain to ear) becomes more necessary. In terms of bottom-up processing, we can speed up and become more efficient in processing if we have a better acoustic signal. A poorer signal makes processing harder and slows us down. In terms of top-down processing, if we have expectations about what we are going to be hearing, that also can speed us up and make processing easier. If we have to use knowledge to sort out errors, make corrections and to fix our understanding because we have run into problems, that slows us down. From both the bottom up and the top down there are ways that we can make listening easier and ways that we can make listening harder. These variations are important to understand for our work with people with hearing loss, especially older people.
Speed of Processing
Speed is an interesting factor. We can measure how many words people remember. We could also measure how fast people are able to understand. At times we hear the complaint from people that even when they do well on word recognition, listening is effortful. Could this type of complaint about effortful understanding actually be a speed issue? It's no longer about accuracy, it's about speed. Older people slow down in general, so does speed of listening also show some age differences? Is speed something to consider when we try to evaluate what makes it easier or harder for old people to listen?
I am going to tell you about an experiment that has been submitted for publication (Goy, Pichora-Fuller, & van Lieshout, submitted). In this experiment people listen to words and to have push a button, yes or no, if the item that they heard is a real word or not. These (non-)words are always presented clearly in quiet. It is a lexical decision task. What changes in the experiment is that sometimes there is material that comes before the (non-)word that provides context. Ideally, the context is congruent and helpful, and should speed things up or facilitate the decision. In this experiment, we can compare how fast people are at making that lexical decision when the preceding material is semantically congruent or when it really does not help at all. We included a neutral situation; the target word would be preceded by a sentence or carrier phrase such as, "Its name is _______." This is a very neutral context. Sometimes in this experiment the material that comes before the word is incongruent. It can potentially lead you to expect a different word. This could trip you up if you are expecting one word and you hear something that is completely different. If I said, "A zebra has black and white stripes," that would be congruent. If I said to you, "A zebra has black and white spoons," that would be an incongruent context for the word spoons. We are comparing the congruent and incongruent to neutral to find out if there is facilitation or inhibition due to the context.
The contexts may be intact, or they may be distorted in different ways, either by time compression, by multi talker babble or low-pass filtering. So what did we find? Young people benefit from context regardless of the distortion. Congruent context speeds them up by about 250 milliseconds. If the context is distorted, the advantage that is gained from context is reduced to 150 milliseconds. So a poorer signal slows you down by 100 milliseconds; a good context speeds you up by about 250 milliseconds. In this experiment, nothing much was happening with inhibition.
So what happens with older people? The older people speed up even more with context. They love context. They are sped up by 300 milliseconds with context. Furthermore, they are not slowed down significantly by distortion. Overall, they started out being slower than the young group, but the relative effects of signal quality and context trade somewhat differently compared to the effects in younger people.
To summarize, the speed of processing is faster when we have an intact signal as compared to a poor signal. If we have context, we are faster than if we do not. We can play both with the signal and the context to have various effects on speed of processing.
I am going to show you some other experiments that we have been conducting recently. Rather than looking at the accuracy of the word at the end of the sentence, we looked at what is happening in the mind of the listener as the speech is unfolding (Ben-David, Chambers, Daneman, Pichora-Fuller, Reingold & Schneider, 2011). To do this, we use a method called eye tracking. It is a very easy measure, and a way that speech perception is often studied in babies today. There is a very natural deviation in the way the eye moves when you are listening to something. If you look at the circle in Figure 3 and then I say, "Now look at the towel," your eye, without any effort, will go to that towel.
Figure 3. Experiment in eye tracking.
That is the behavior that we are tapping in this experiment. We tested older adults and younger adults with normal hearing and vision. We adjusted the SNR again by 3 dB for the older group to equalize the playing field and get the same level of performance in each group. We performed the experiment in quiet and noise conditions. We used a visual display (following Allopenna, Magnuson, & Tanenhaus, 1998) or matrix, where the subject may have several items to look at, such as tower and towel, which sound similar. Other items are unrelated phonologically. We asked the subjects to look at a target, and we evaluated how their eye moves to the right or wrong items. That tells us in 10 millisecond steps what they are thinking as they are hearing items.
Here is my colleague Bruce Schneider looking at the display (Figure 4). He has two seconds to look around and check out what is happening. Then when he is ready, we tell him to fixate on the center position in white, and then he is told to look at the towel. Briefly, his eyes go to the wrong item and then they settle on the towel. When he has decided that is the place where he is going to look, that is the right answer, he gets some feedback, and then the trial is over.
Figure 4. Experimental setup of eye tracking, with the camera placed below the computer monitor. Note the four lexical choices on the screen with the blank center square.
We look at the proportion of fixations of the eye on the target (towel) versus the competitor (tower) and the unrelated items, and we see how the proportion of time the eye spends on each of those changes over time (Figure 5). We can see over time, how the eyes of the observers focus on the target. In Figure 5, the dotted line is the end of the word. So up until the end of the word and after the end of the word, there is consolidation of the information and the subject settles in on the target. We get the time course of listening using this method.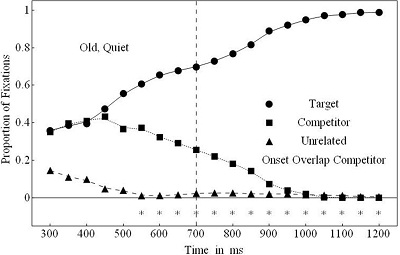
Figure 5. Measure of proportions of fixation over time. The dotted line is the end of the target word.
Data for older listeners show that they are settling in to the word when it is quiet faster than they are settling in when there is noise; they get it right, but take a little extra time to settle on the right word. We have age differences only in very specific situations, and many situations in the study indicated no age differences because we corrected for that signal-to-noise handicap.
The one case where we did find an age difference was on rhymes. This would be words like "candle" and "sandal", where the opening consonant has a big impact on getting the word correct. The young people get it immediately while the older people take more time to get it. So yes, we have slowing in older listeners. In many cases the older people are slower overall, but the differential effects of noise and use of context do not seem to be different.
Attention
Let's look at attention. This is very interesting because when people are in our sound booth, we really do not tax them with some of the attentional demands that are representative of everyday life. This is a study that Gurjit Singh did. In this study people are hearing sentences from three locations. The sentences are being presented simultaneously, each from a different loud speaker and different spatial position. The task is to identify the color and the number that goes with the callsign that people are told ahead of time to listen for. The callsigns that are used might be Charlie, Hopper, and Baron, etc. They are told to listen for Charlie on a specific trial. The sentence says, "Ready [call sign], go to [color] [number] now." They hear "Charlie" embedded in that set of three sentences and they have to say what the color and the number were that went along with the sentence for Charlie. What is the probability that the target is going to come from a particular location? For example, if the target callsign was "Hopper" and you were told that 100% of the time it would come from the front, you could focus your attention on the front. If that dropped down to 80% you would have to also allocate some attention to the side. And in the most extreme case it could be random. You would not know, more than chance, where the sound was going to be coming from. That is something that we have to do in everyday life. So if you know where to listen you do very well. As the certainty about where to listen goes down, your performance drops. That's what happens with young people.
In the original experiment (Singh, Pichora-Fuller & Schneider, 2008), we saw no age differences, so older people were performing pretty much the same as younger people. So Singh tried to make it harder, more like it might be in everyday life. In this experiment (Singh, Pichora-Fuller & Schneider, 2010), he looked at how young and old people perform in likely and unlikely contexts in simple and complex conditions. The likely condition was knowing where the target was going to come from. The unlikely condition was a random position of the target sentence. There were no age differences between the younger and older groups for the likely and unlikely sentences in the simple conditions. In the complex condition, the cue is coming from one place but the source of interest is from another. He set up the complex condition such that he told the subject "If the target comes at the left you should answer the color and number from the right" and vice versa. This would mimic a scenario such as sitting in a business meeting where you have to turn and listen to different people or divide your attention. In that complex situation it really does not make much of a difference for the young people. They perform about the same as they did in the original condition. But for the older listeners, if something comes from a place where they were not expecting, they cannot shift focus as easily. They have trouble being able to shift attention from one place to another with the flexibility that is required in the task. Shifting attention seems to be one of the few attentional demands that we have been able to isolate in some of our listening experiments.
In summary, word recognition is achieved in various ways, depending on the environment, person and task factors and we are able to see differences in how people perform. There are not a whole lot of age differences once we correct for the difficulty with the SNR that older people encounter. There is a general advantage that older people have in terms of using knowledge to compensate for a poorer signal.
Cognition and Hearing Aid Benefit
Now I want to make some connections between cognition and hearing aid results by summarizing some of the research. In 2003, several researchers published landmark studies citing a connection between cognition and the ability to benefit from fast-acting hearing aids (Gatehouse, Naylor, & Elberling, 2003; Lunner, 2003; Humes, 2003). This created interest in the connection between hearing and cognition. Since the original topic appeared in 2003, what have we learned? We have learned that when you are listening with a slow-acting hearing aid in a simple condition, the typical pure tone hearing results account for most of the variance. When you are listening with fast-acting hearing aids in a more complicated modulated background, the cognitive measure tells the story (Lunner & Sundewall-Thorén, 2007). Larry Humes (2003) also showed this relationship between pure tone thresholds and how people perform on speech in noise in unaided conditions. With aided conditions, when that auditory problem is overcome with amplification, we have no more correlation with hearing but we have significant variance accounted for by cognitive and central auditory processing factors. Davis (2003) tells us that the people who get greater benefit from hearing aids are the people with poorer cognition. I would speculate that this is because they cannot compensate by using knowledge as well, so they need more signal. The people who really need hearing aids are actually the ones who have poorer cognition even though they may adapt less well to some of the more sophisticated, fast-acting hearing aids, at least without special training. We have evidence from Larry Humes (2003) that people who have less cognitive ability use their hearing aids more, which supports this idea that I am developing. We have work from Thomas Lunner (2003) showing that the more cognitively aware the patient is, the better able they are to participate in describing their experiences of listening. The work from Sarampalis and colleagues (Sarampalis, Kalluri, Edwards, & Hafter, 2009) shows that working memory span measures indeed can be used to differentiate between different kinds of noise-reduction algorithms. Work out of Sweden (Foo, Rudner, RÅ'nnberg, Lunner, 2007) shows that when people are first getting used to new hearing aids they are demonstrating very important individual differences based on cognition. Learning how to use a hearing aid, the initial performance, is very dependent on cognition even though cognition may be less important after people have acclimated to a hearing aid. So we have a plethora of evidence that suggests how people get used to hearing aids and that learning to cope with them draws on frontal cortex knowledge.
In the clinic we see people with a range of vision, hearing and cognitive abilities. That range includes people who have no impairment in one or more areas, to those with total impairment (blindness, deafness, dementia) in one or more areas. What happens when you have a sensory loss and a cognitive loss combined? Now we are moving away from people with good health in old age to people who actually have impairments in other health domains, including dementia.
According to a Canadian Study of Health and Aging (Ebly, Parhad, Hogan & Fung, 1994) 15% of the adults age 75 to 84 years, those who may be coming to you for their first hearing aid, have dementia. And there is some evidence that there is, in fact, a greater prevalence of hearing loss in people with dementia (Gold, Lightfoot, & Hnath-Chisolm, 1996; Uhlmann, Teri, Rees, Mozlowski, & Larson, 1989). We have frequent misclassifications because of the tests that are performed to evaluate cognitive impairments. If people are tested without their glasses or hearing aids, they could be miscategorized. That has happened in one out of three cases according to an early study by Weinstein & Amsel (1986). We have very provocative, longitudinal evidence that people who do poorly on speech in noise tests are 6 to 12 times more likely to develop clinical dementia ten years later (Gates, Cobb, Linn, Rees, Wolf, et al., 1996). We have breaking news this year that even pure tone thresholds can be predictive of incident dementia several years out (Lin, Metter, O'Brien, Resnick, Zonderman, et al., 2011). So hearing loss could be the canary in the mine that warns us that cognition is not going to stand up in the long run because all of the strain on cognition associated with hearing loss could later manifest as a cognitive impairment. That is one idea. Perhaps by using an auditory test we could identify sooner when things are going awry in the brain. If we document that cognitive problems started out with these hearing problems, we can perhaps determine the likelihood that specific patients will be more prone to develop dementia because hearing gave us an early warning sign.
Another idea is that people who have hearing loss or vision loss do not exercise their mind. They do not exercise socially or perhaps physically, and hearing loss is an accelerator for dropping out of an active lifestyle. Moreover, maybe their social isolation aggravates the cognitive impairment (Troyer & Murphy, 2007). We do have evidence that there are cognitive benefits of better hearing. People who have hearing aids have better emotional and social well being and greater longevity (Cacciatore, Napoli, Abete, Marciano, Triassi, et al., 1999), and reduced rate of decline on a cognitive screening test (Allen, Burns, Newton, Hickson, Ramsden, et al., 2003). There is slower decline in mental acuity in Alzheimer's disease in people with better hearing, and people with dementia who wear hearing aids show fewer problem behaviors (Palmer, Adams, Bourgeois, Durrant, & Rossi, 1999). There is considerable reason to believe that we can make a real contribution in helping to slow cognitive impairment or even perhaps preventing it, because keeping an active lifestyle depends on communication, and communication depends on hearing, and that is where we enter into this bigger picture.
Hearing and Social-Emotional Factors in Aging
We are going to progress into a new topic, and that is, social-emotional factors in aging and hearing loss. I'll discuss both the good and bad sides of aging, the emotional positivity effect, and self-regulation of emotion, and how these factors may appear in your clinic, and some of the more problematic areas such as stigma and stereotyping. Finally, we will discuss self-efficacy.
We have been talking about older adults. We can be honest and say that not everyone gets excited to see a 90 year-old patient first thing in the morning, but some of us do. When you know the age of the patient you will see, what kind of reaction do you have? Do you think about the person more positively or negatively based on their age? Do you feel that you are balanced in your opinion? It is time for us to reflect on this. I think there are issues about aging that affect our patients, their family members, and significant others. I sometimes wonder if, in fact, people in our profession may have more difficulty with ageism than some of the patients or their family members.
What exactly is different about older people in terms of what they want? Do they really have different needs than younger adults, or are they the same? To what extent do their communication needs depend on hearing? Are there different kinds of communicators? Maybe the communication one person uses does not depend so much on hearing, and maybe that is why we see some discrepancies between the hearing loss prevalence figures if we look at audiograms versus self report. If someone receives a diagnosis of hearing loss when they are 30 versus 75 do they respond to it differently? Does it matter if you are an older woman or an older man? Think again about this question, "Who is your ideal client?" Is it a young person? Is it an old person? Do you care? These are some things that we are talking about in terms of your everyday practice. It is not all on the audiogram, so what is it really about?
Some data from Canada (Lindsay, 1999) indicate that older Canadians rate their health positively - 12% rate it as excellent, 28% as very good, and 38% as good. Even though there are many age related health conditions, older people generally rate their health quite positively. This may be because many older people are in very good health; today's seniors are much healthier than earlier generations. They may also rate their health positively because if they have chronic conditions, they are coping very well. Their positive outlook may also be partly due to the fact that changes in aging affect people's emotional responses and their social goals. Some of the consequences of health problems may be different for an older person than a younger person, so that these problems do not affect older adults as negatively. Some older people certainly do have better health, and while some may have health problems, they may be dealing positively with the consequences of the health problems for a variety of reasons. It would be great if our patients were dealing with their hearing problems in a positive fashion, as they are with some of their other health issues. How could we take advantage of some of the coping abilities these individuals have used in other domains and apply them to hearing loss?
The place to begin is beyond the audiogram. The audiogram is important, yes, but we have to think about the environment the person is in, as well as their social goals. What are the consequences of hearing loss to people in their everyday activities? What environments are they in and with whom are they communicating?
We want to know what is audible and what is not so that we can amplify those signals for audibility without losing clarity and speech understanding.
If you recall, timing information in the voice tells us if the speaker is a man or a woman or if the mood is happy or sad. As it turns out, older people with good hearing compared to younger people with good hearing do not recognize emotion in the voice as well. There are significant differences for all of these emotions. In a recently submitted paper (Dupuis, Pichora-Fuller, & van Lieshout, submitted), we used NU 6 words spoken by both a young actress and an older actress in angry, sad, neutral, fearful, happy, disgusted or pleasantly-surprised portrayals. The listener then had the option to repeat the word or not, but they had to say what emotion the speaker expressed when they said the word. The young people always scored higher than the older people for all of the emotions. That is interesting. We know that older people have difficulty with speech in noise, but it is a bit of a surprise to know that they are not as good at recognizing emotion in the voice. Therefore, they may not be tuning in to some of that extra linguistic information that comes from speech either. This may also result in them directing attention differently and in not understanding some of the things that people are saying, because although they may have a better semantic context, they may not necessarily have the same emotional context.
It was fascinating when we tried to examine factors that might explain why older adults are not as good at recognizing emotion in the voice. Perhaps cognitive change, or emotional change such as hormones or changes in the parts of the brain that are involved in emotion, are responsible, or perhaps there is a sensory component. What we found was a correlation with the ability to differentiate fundamental frequency of the voice, to tell pitch apart between different voices, in a psychoacoustic type task. Again, we see that temporal auditory processing issues are at least part of the reason why older adults do not recognize emotion in the voice. If you are fitting someone with a hearing aid, and that person would like to know how their grandchild is feeling, they are potentially disadvantaged if they have age related changes in auditory and neural processing that affect picking up the voice pitch cue, which is important for understanding emotion. They are in a sense dampened in terms of some of the emotional cues that they pick up.
So we know that there are some auditory issues that can contribute to the emotional and social landscape of aging. Particularly with older people it is important for us as clinicians to understand what else is happening in their lives. There is a tool that psychologists sometimes use to evaluate changes in life from various events. They attribute Life Change Units (LCU) to different events; the more LCUs an event has, the more impact or stress that event has on your life (Holmes & Rahe, 1967; see also Taylor & Sirois, 2009). Death of a spouse ranks at the top of the list with 119 LCUs, and other events such as personal injury or illness, retirement from work, death of a close friend, also rank high on the list. For some of these events, the number of LCUs that are attributed has changed over the years, so the events are seen as having more of an impact today than 30 years ago. We have to understand that these significant events that our older clients may be experiencing can intersect and affect how they approach their hearing loss, so it is important for us to consider how much we are learning about the general life of our clients. They may want to tell us about these events, and we may not think it is relevant. We may want to focus solely on their hearing; but perhaps these events are relevant.
People who were children during World War II have had different life experiences that are unique to their cohort. Many people are very affected throughout their entire life by early events, so we may want to know not just about the current events in our clients' lives, but also about their past events. Some of those early experiences could have been very stressful; depending on the amount of stress that a person is exposed to at different times in their life, there are interesting consequences to how the brain functions. If you are interested in this, I highly recommend an article by psychologist Sonia Lupien (2009) on stress over the entire lifespan. She refers to this as the Life Cycle Model of Stress. She asserts that the amygdala (which controls emotion), the frontal cortex (which is involved in use of context and semantic information, among other things) and d the hippocampus (which is involved in memory), are extremely sensitive to stress that a person experiences in their life during development and during old age. If someone has a stressful life event when they are aging, it is going to create problems in terms of emotional processing, decision making and executive processing (use of information and memory). Stress plays a large role in the alteration of the hormones and brain chemicals that are generated in response to a life event. Over an extended period of time, this acts like a toxin to the brain. When you are stressed, you need to have that fight-or-flight response to deal with a crisis moment. But if you have extended chronic stress, the on going production of those hormones is bad for your brain and is not helpful if you are trying to deal with a hearing loss as well. I think we now have some better understanding of the connection between stress and health, and it is important for us to try and understand it in a new way in terms of our clients.
Health in general has been defined as the capacity for people to adapt to, respond to and control life's changes and challenges (Frankish et al., 1996). Conversely, stress, by definition is when you do not adapt, respond to or control life's challenges effectively. Control is an important theme in how people cope with stress.
I picture an octopus. I was interested after seeing a science show that said octopus were very intelligent and had evolved to live solo; they are not social animals. They have survived because they have developed exquisite skills to camouflage themselves and adapt to their physical environment. This got me thinking that as human beings, as social animals, the way that we camouflage ourselves, the way that we cope, the way that we adapt to change, instead of changing shape and size and color like an octopus, we change ourselves socially. The ability to fit in and feel like we belong to the group with which we wish to identify is really important for our self preservation. Staying socially integrated is a factor that we have to be aware of when we are working with people with hearing loss. They need to communicate in order to fit in. Depending on how they think they are going to fit in, wearing a hearing aid may trade against being able to communicate well. This is not something that is unique to older people. Teens want to fit in. Older people want to fit in. People want to adapt and gain control and have harmony with their surroundings so they do not experience stress. But we, as audiologists, need to be able to understand and relate to the way in which older people may be trying to accomplish this so that we can help them to do what is appropriate for them.
There are generalizations that we may make about age, some of which are positive, and some of which are negative. Stereotyping is a potential threat to a person when they are out there in society dealing with other people who may hold ageist stereotypes. It may even be a problem in our clinic if we are not responding to each person as an individual and understanding what is going on with them. One of the things in which social psychologists have become very interested is this idea of stereotype threat, which is when you are at risk for being identified as someone who belongs in a social category that is perceived negatively. If society, clinicians, friends and family perceive older people negatively, then the older person is not going to want to be seen as a member of that group. Stereotypes can be assigned externally or internally (Schmader, Johns, & Forbes, 2008). If a person is afraid of being put into a negative category, they will actually be under stereotype threat.
Stereotypes by other people or by self are problematic. The idea, "I am an old person. I probably cannot do that," affects performance in many areas. It affects things like how fast you walk (Bargh, Chen, & Burrows, 1996). It affects cognitive performance and working memory (Hess, Hinson, & Hodges, 2009). There is even a study (Levy, Slade, & Gill, 2006) that shows if we get people into the mindset that they have bad hearing because they are old, they will under-perform on hearing tests. We can set up an undesirable outcome, a self-fulfilling prophecy, but we can also turn it around to counteract some of these problems and set up a more positive situation for our clients.
People have different reactions to hearing aids depending on where the hearing aid is fitting on the map of stereotypes. We can think of this in terms of attribution. If something goes wrong on the part of a person in your "in-group" or in a desirable group, you blame it on the situation, and if it goes right, you attribute it to the person. If someone is in an "out-group", we attribute the problem to the person, while if things go right, we attribute it to the situation.
How do our clients understand things that go right or wrong with the hearing aid? Is it because the hearing aid, or is it because of the person? How much of it is because of hearing loss? How much of it is because of aging? This connection between stigma to hearing loss and stigma to age become intertwined in a way that we need to understand better. That is some of the research that we are doing now.
We have this situation where hearing problems can make communication worse and that can aggravate some of the psychosocial pressures on people. We also have psychosocial issues for aging, such as stigmatization, low self-efficacy, and the stereotype threat that reduces performance on hearing and cognition measures so again a little bit going in both directions. So how do we try to get this right?
One of the models proposed by Ellen Ryan and her colleagues (1986) called the Predicament Model is a simple idea really. When we encounter an older person, we recognize old-age cues. If we are meeting them for the first time, such as somebody who is coming to get their first hearing aid, you have some stereotyped expectations. You may actually communicate with them in a way that takes that into consideration. For example, you could modify your speech in a way that may or may not be appropriate. If people react on the basis of stereotypes in a way that underestimates the abilities of the person, then over an extended period of time that becomes a self-fulfilling prophecy, and the communication competence of the person can decline. There is literature that says that nurses and nursing homes ignore competent behaviors and reinforce incompetent behaviors (Baltes & Wahl, 1996). That is a cycle that accelerates a drop in competence in terms of communication. Are we allowing our clients to achieve their best, or are we putting them down? How ageist are we? How ageist is the industry? I think the tide is turning and we'll be less ageist in the future.
Ellen Ryan and her colleagues (1995) propose a simple solution to combat and break the cycle of inducing communicative incompetence. When we encounter older people, yes, we recognize that they are older, but we also must take into consideration their personal needs. We have to understand their individual abilities and empower them so that they can achieve a sense of well being, maximize communication and reinforce their competence as opposed to undermining it. Easier said than done, perhaps.
How might this look applied to therapy or intervention to go along with hearing aids? For example, the client comes in with a family member, specifically a son or daughter. Do you talk to the person or do you talk to the family member? It is often easier to talk to the adult child, but it is not necessarily going to reinforce competent behaviors on the part of the older communicator. Talking to the person who has the problem is something of which you have to be mindful. On the other hand, you might be in a position where it is necessary to talk to a family member. Where is the line between involving the family member as a support and the patient's privacy and confidentiality? How do you make it acceptable to involve the family member so you have a better insight into the patient while gaining support of the patient without contravening their rights? There are consequences to the caregivers if the patient is in a situation where they have other health issues or dementia and the family is looking after them. Understanding the whole family context is important. In some cases you may find that the decision making is a bit of a balancing act between what the family needs and what the person needs. Finding the happy medium where everyone agrees to and supports the solution is important for success.
You are probably familiar with the World Health Organization International Classification of Functioning model (2001). The basic idea is that when you have a health condition, there is an impact on body function and structure that we can measure through our diagnostic testing in the clinic. There are tasks or activities that the person needs to perform, such as listening to speech in noise, that we can measure and address with rehabilitation. There is a participation component; the person is going out into the world and participating in activities and we need to provide accessibility. We need to find out in which activities they need to use hearing to be able to participate fully.
At this time, I am going to go into the environmental and personal factors, which are the context part of the ICF model, and where there may be supports and barriers. As audiologists, it is important to identify the supports and barriers that our patients have as they navigate different listening encounters in the real world. Your patient may have trouble with something like speech in noise. They want to be able to continue to attend their social club. What is going to help them there? The proper support can provide motivation and acceptance and allow a continuation of that activity. If they encounter barriers that they cannot overcome they are going to become stressed and they are not going to adapt. Ultimately, they are going to withdraw from social activities.
We need to draw on the personal and environmental factors, including social support, in our context of care. You can think about the lifespan as it relates to the population you see. If you are working with children then are you are clearly working with the parent because the child is a dependent individual. As people get to be older, asteenagers and young adults they become more independent. In the later ages there may be interdependencies or complete dependence between spouses or other family members.
Seeing the Patient as an Individual
Understanding the dynamics of the patient's day-to-day life is not something that we spend enough time doing, but would be very helpful, especially if you have returning clients who you get to know over time. There are barriers and supports associated with each variable. When dependent, some people may have services brought into the home, whether that is to prepare meals, do some housekeeping or provide assistance with other activities of daily living. How are those service providers communicating with them? What do they know about hearing aids? How can we extend some of the work that we are doing to help ensure effective communication with these outside people who are involved in caregiving? Some of our patients may be going to special centers for people who have similar health conditions or they could be living with family members and attending a day program at a center. We see patients who are living in residential care. Depending on the level of care, some of these can be very challenging and very hostile environments where communication is certainly challenged. How do we keep people communicating in those different contexts? We have to know these things about people in order to understand how the hearing aid and rehabilitation are working in terms of the rest of their life.
We do not want to be setting up a stereotype threat. We do not want to reinforce the idea that it is difficult to get used to a hearing aid such that people are going to have difficulty because they think it is going to be difficult. We have to find the way of making them confident enough to try it. We have to reduce stress when they are getting a hearing aid, especially for the first time. According to Lupien (2009) novelty, or when things are new, causes stress, as does unpredictability, threat to self, and sense of loss of control. Therefore, getting a hearing aid might be stressful because it is a new experience. Since unpredictability causes stress, making sure that people know as much as they possibly can about their hearing loss, hearing aid and the process so that they do not have to deal with the unknown could reduce stress. We do not want people to think that this is going to be unrealistically simple, but we do not want them to fail because they have worked themselves into a situation where they believe that they are going to fail. Achieving a sense of control and coping is also going to be very important.
In order to have control we are going to need self efficacy. We would like to have a person who comes in with conviction. "Yes, I want a hearing aid. Yes, I am ready for it. Yes, I can do this, and I have all the support I need. It is all going to be fine." That is not actually how it happens, of course. We discussed this idea of stress as being an adaptation to your environment, so when we are in balance with our environment we are not stressed. For people with hearing loss who have problems there are two ways to achieve this balance with the environment and reduce stress.
First, they can gain control by being assertive and seeking help from people if they need it once they get a hearing aid. They can also create balance by avoiding a situation that is too difficult for them. Perhaps by avoiding using the hearing aid and not using the hearing aid at all is a way of coping, but in the long run, the coping mechanism should probably not be avoidance. There has to be some balance between controlling and avoiding. I am going to give you an example of how we could have a judicious combination of controlling and avoiding. First, we need to know what the person's priorities are. Let's take the situation of a noisy restaurant. We want the person to define their goals, and we want them to have the conviction about what is important and what is not. Clearing that up at the beginning is going to set the stage for success.
It is difficult to go to a noisy restaurant and have an intimate evening between a husband and a wife. They are clear that their priority is to have a nice evening with each other. Interacting with the staff or the quality of the food is not their priority. In terms of communication, that then opens the door for some solutions which are going to focus on achieving this goal of intimacy. In this particular case, the husband and wife have decided before going out that the wife would use an audio input microphone to connect to the hearing aid and the husband with the hearing loss would focus on listening to his wife and surrender his role as being the one who does the ordering and the communication with the wait staff, which was not part of his important goal. In turn, he would let his wife take those roles that so he could focus on understanding her. He is controlling the aspect of the communication with his wife and is avoiding the aspect of communication with the wait staff. This is a mix of avoid and control that happened to work out in that situation. We have control over various factors such as the technology, the behavior of the person with hearing loss, the behavior of the spouse, and how do we put it all together to find the solutions to achieve the goals that we are most important?
In finding solutions, there are some questions to ask. What do you really want to do? What are you prepared to do? Who else has a stake in this – family members, co-workers, service providers, pets? Where are you going to do it – a private home, a residential facility, a school, an office, a factory, a public facility? All of these things are ingredients that we can put together to design an intervention that is more ecologically relevant so the person can go out and achieve his or her goals.
Conviction is a good start. We then want to motivate clients to implement solutions so they can find a long term treatment that will solve their problem. We have collected some unpublished data that we are just now looking at. We found that the fear of aging was significantly related to answers on questionnaires about attitudes towards loss of hearing, expected benefits from hearing aids, the unaided Abbreviated Profile of Hearing Aid Benefit (APHAB; Cox & Alexander, 1995), the Hearing Handicap Inventory for the Elderly (HHIE; Weinstein, Spitzer, & Ventry, 1986), the SSQ and a few self efficacy questionnaires about hearing aids and listening in noise that Sherri Smith has worked on. Interestingly, the fear of aging was not correlated with these measures for people who were already hearing aid users. This leads me to believe that this overcoming of fear is really an important thing that we should focus on more at the beginning so people are not afraid. Fear of aging, by the way, is not correlated with chronological age.
You may have heard of The Health Belief Model (Rosenstock, 1966; see also Taylor & Sirois, 2009). The Health Belief Model asserts that in order to solve a health problem you have to know that it is a problem, know that it affects you, and believe there is a solution. It means being willing to approach the solution, and believing it could work for you. The model can be applied to a variety of health behaviors, like stopping smoking; it is not unique to hearing. There are very logical steps to making changes in any health behavior. This belief, this overcoming of fear, takes us to Self Efficacy theory.
**The Self-Efficacy Theory has to do with a specific behavior, like wearing a hearing aid. The theory starts with a belief, or domain-specific confidence that one can master skills needed to change a certain behavior (Bandura, 1997, 2001). “What is my confidence that I would be able to succeed wearing a hearing aid?” The confidence is unique to that behavior. Someone who is great at one behavior could have very poor self-efficacy at using a hearing aid. “I am great at using the Internet but I do not think that I would be very good at using a hearing aid.” An example of the thought process an older individual may go through would be, “Yes, I know I have a hearing loss. Yes, I know this is a problem. Yes, I know that a hearing aid is a good solution. Do I have the confidence to do it? If I do not have good confidence, what can be done about it?”
This idea of self efficacy has been applied in many areas of health care including diabetes care and dieting. People who have high self-efficacy are the ones who succeed and have very good compliance. They do not get discouraged and they keep trying. In audiology, we have dabbled in self-efficacy, applied to things like wearing ear protection (Lusk, Ronis, & Hogan, 1997; Lusk, Kerr, Ronis, & Eakin, 1999; Melamed, Rabinowitz, Feiner, Weisberg, & Ribak, 1996) and to some other areas of audiology (Tinetti, Richman, & Powell, 1990; Jennings, 2007; Smith & Fagelson, 2008). More recently we have started to examine how it might apply to rehabilitation. I recommend the articles by Smith and West in the reference list for more information (2006a, 2006b). One of the articles is a great tutorial on self-efficacy in aural rehabilitation, and the other is a hearing aid self-efficacy measure that you may find useful. Sherri Smith has been a leader in this area and I’ve had the privilege to work with her on some research.
In the last couple of minutes today I want to take you through some of the work that is described in a recent paper on listening self-efficacy (Smith, Pichora-Fuller, Watts, & La More, 2011). I am going to skip through the material on listening self efficacy and how we developed the scale, and discuss intervention techniques.
These intervention techniques would be used for clients who know they have a problem and they may know there is a solution, but they are afraid. An older person could possibly be afraid, not because they are old but they could be afraid of being perceived to be old. That extra fear of aging is going to aggravate the confidence that they may need to get a hearing aid. You have to build self-confidence so that you do not encourage people to take on a new behavior that they are just going to fail at. The techniques include: explicitly teaching about the stereotype threat; blurring inter-group boundaries; providing positive role models; reshaping views; modifying performance expectations; and making achievements salient.
You set them up for success, perhaps by even mentioning about stereotype threat and talking about being afraid. We should attempt to blur some of the inter-group boundaries and get them in the mindset of identifying things that older people are very good at. Give them positive role models, and let them see a different way of how they might succeed. Make sure that they are not trying things under conditions where they are already stressed. This is where relaxation and anxiety-reduction techniques will possibly make a positive difference after introducing a new behavior, like wearing a hearing aid. Some of the things you could do in your practice to help build self-efficacy are to practice or role play, set realistic goals, grade tasks with easier tasks before harder ones, break complex tasks into smaller pieces and review tasks from simpler ones to complex. In this way, you can provide feedback and encouragement. Most importantly, make sure that you are not putting them into a stereotype-threat situation and that you are giving them ample time and ability to succeed.
So we have many different levels to work on. Along with the provision of hearing aids, we can change what a person does, what a person thinks and what a person feels and we have to individualize it in order to have success. There is a connection between emotion and social factors, between cognition and hearing. All of these things meet up in the brain and play out in real life. Age is not just about loss; it is about understanding how all of these things play out together while trying to make them all work in a positive fashion as we help people to achieve their goals.
References
Allen, N.H., Burns, A., Newton, V., Hickson, F., Ramsden, R., Rogers, J., Butler, S., Thistlewaite, G., Morris, J. (2003). The effects of improving hearing in dementia. Age and Ageing, 32(2), 189-193.
Allopenna, P. D., Magnuson, J. S., & Tanenhaus, M. K. (1998). Tracking the time course of spoken word recognition using eye movements: Evidence for continuous mapping models. Journal of Memory and Language 38, 419-439.
Baddeley, A.D., Hitch, G.J.L (1974). Working memory. In G.A. Bower (Ed.), The psychology of learning and motivation: Advances in research and theory (Vol. 8, pp. 47–89). New York: Academic Press.
Baltes, M. M., & Wahl, H.-W. (1996). Patterns of communication in old age: The dependence-support and independence-ignore script. Health Communication, 8(3), 217-231.
Bandura, A. (1997). Self efficacy: the exercise of control. New York: Freeman.
Bandura, A. (2001). Guide for constructing self-efficacy scales. In: Pajares, F. & Urdan, T. (eds.), Self-efficacy beliefs of adolescents (pp. 307-337). United States of America: Information Age Publishing.
Banh, J., Singh, G., Pichora-Fuller, M.K. (in press for Feb 2012). Age affects responses on the Speech, Spatial, and Qualities of Hearing Scale (SSQ) for adults with minimal audiometric loss. Journal of the American Academy of Audiology.
Bargh, J.A., Chen, M., & Burrows, L. (1996). The automaticity of social behaviour: Direct effects of trait concept and stereotype activation on action. Journal of Personality and Social Psychology, 71, 230-244.
Ben-David, B.M., Chambers, C.G., Daneman, M., Pichora-Fuller, M.K., Reingold, E.M., & Schneider, B.A. (2011). Effects of aging and noise on real-time spoken word recognition: evidence from eye movements. Journal of Speech, Language, and Hearing Research, 54(1), 243-262.
Bilger, R.C., Nuetzel, M.J., Rabinowitz, W.M., Rzeczkowski, C. (1984). Standardization of a test of speech perception in noise. Journal of Speech, Language & Hearing Research, 27, 32-48.
Cacciatore, F., Napoli, C., Abete, P., Marciano, E., Triassi, M., & Rengo, F. (1999). Quality of life determinants and hearing function in an elderly population: Osservatorio Geriatrico Campano Study Group, Gerentology,45(6), 323-328.
Cabeza, R. (2002). Hemispheric asymmetry reduction in old adults: The HAROLD model. Psychology and Aging, 17, 85-100.
Cox, R., & Alexander, G. (1995). The abbreviated profile of hearing aid benefit. Ear and Hearing, 16(2), 176-186.
Daneman M, & Carpenter PA. (1980). Individual differences in working memory and reading. Journal of Verbal Learning and Verbal Behavior, 19, 450–466.
Davis, A. (2003). Population study of the ability to benefit from amplification and the provision of a hearing aid in 55-74-year-old first-time hearing aid users. International Journal of Audiology, 42(2), S39-2 S52.
Davis, S. W., Dennis N. A., Fleck, M. S., Daselaar, S. M., & Cabeza, R. (2008). Que PASA?: The posterior-anterior shift in aging. Cerebral Cortex, 18, 1201-1209.
Ebly, E.M., Parhad, I.M., Hogan, D.B. & Fung, T.S. (1994). Prevalence and types of dementia in the very old: results from the Canadian Study of Health and Aging, Neurology, 44(9), 1593-600.
Foo, C., Rudner, M., RÅ'nnberg, J., & Lunner, T. (2007). Recognition of speech in noise with new hearing instrument compression release settings requires explicit cognitive storage and processing capacity. Journal of the American Academy of Audiology, 18(7), 618-31.
Frankish, J., Green, L., Ratner, P., Olsen, L., & Larsen, C. (1996). Health impact assessment as a tool for effective health policies and program (Report to Health Canada). Ottawa, ON: Health Canada.
Gatehouse, S., Naylor, G., & Elberling, C. (2003). Benefits from hearing aids in relation to the interaction between the user and the environment. International Journal of Audiology, 42(S1), S77-85.
Gatehouse, S., & Noble, W. (2004). The speech, spatial and qualities of hearing scale (SSQ). International Journal of Audiology, 43(2), 85-99.
Gates, G.A., Cobb, J.L., Linn, R.T., Rees, T., Wolf, P.A., & D’Agostino, R.B. (1996). Central auditory dysfunction, cognitive dysfunction, and dementia in older people. Archives of Otolaryngology Head & Neck Surgery, 122(2), 161-167.
Gold, M., Lightfoot, L.A., & Hnath-Chisolm, T. (1996). Hearing loss in a memory disorders clinic: a specially vulnerable population. Archives of Neurology, 53(9), 922-928.
Gordon-Salant, S., Frisina, R.D., Popper, A. & Fay, D. (Eds), The aging auditory system: Perceptual characterization and neural bases of presbycusis. Springer Handbook of Auditory Research. Springer: Berlin
Hess, T.M., Hinson, J.T., & Hodges, E.A. (2009). Moderators of and mechanisms underlying stereotype threat effects on older adults' memory performance. Experimental Aging Research, 35, 153-177.
Holmes, T.H., & Rahe, R. H. (1967). The social readjustment rating scale. Journal of Pscyhosomatic Research, 11, 213-218.
Humes, L.E. (2003). Modeling and predicting hearing aid outcome. Trends in Amplification, 7(2), 41-75.
International Organization for Standardization (ISO). (2000). ISO-7029: Acoustics statistical distribution of hearing thresholds as a function of age. Switzerland.
Kujawa, S.G., & Liberman, M.C. (2009). Adding insult to injury: Cochlear nerve degeneration after “temporary” noise-induced hearing loss. Journal of Neuroscience, 29, 14077-14085.
Levy, B. R., Slade, M. D., & Gill, T. (2006). Hearing decline predicted by elders’ age stereotypes. Journal of Gerontology B-Psychological Sciences, 61, 82-87.
Lin, F. R., Metter, E. J., O’Brien, R. J., Resnick, S. M., Zonderman, A. B., & Ferrucci, L. (2011). Hearing loss and incident dementia. Archives Neurology, 68(2), 214-220.
Lindsay, Colin. (1999). A portrait of seniors in Canada. 3rd ed. Cat. no. 89-519- XPE. Ottawa: Statistics Canada.
Lunner, T. Cognitive function in relation to hearing aid use. International Journal of Audiology, 42(S1), S49-58.
Lunner, T. & Sundewall-Thorén, E. (2007). Interactions between cognition, compression, and listening conditions: Effects on speech-in-noise performance in a two-channel hearing aid. Journal of the American Academy of Audiology, 18, 604–617.
Lupien, S. (2009). Effects of stress throughout the lifespan on the brain, behavior and cognition. Nature Reviews Neuroscience, 10, 434-445.
Lusk, S. L., Ronis, D. L., & Hogan, M. M. (1997). Test of the health promotion model as a causal model of construction workers’ use of hearing protection. Research in Nursing and Health, 20, 183–194.
Lusk, S. L., Kerr, M. J., Ronis, D. L., & Eakin, B. L. (1999). Applying the health promotion model to development of a worksite intervention. American Journal of Health Promotion,13, 219–227.
Melamed, S. M., Rabinowitz, S., Feiner, M., Weisburg, E., & Ribak, J. (1996). Usefulness of the protection motivation theory in explaining hearing protection device use among male industrial workers. Health Psychology, 15, 209–215.
Mills, J.H., Schmiedt, R.A., Schulte, B.A., & Dubno, J.R. (2006). Age-related hearing loss: A loss of voltage, not hair cells. Seminars in Hearing, 27, 228-236.
Obleser, J., Wise, R.J., Dresner, A.M., & Scott, S.K. (2007). Functional integration across brain regions improves speech perception under adverse listening conditions. Journal of Neuroscience, 27(9), 2283-2289.
Palmer, C.V., Adams, S.W., Bourgeois, M., Durrant, J., & Rossi, M. (1999). Reduction in caregiver-identified problem behaviors in patients with Alzheimer’s disease post hearing aid fitting. Journal of Speech, Language and Hearing Research, 42(2), 312-328.
Pichora-Fuller, M.K., Schneider, B.A., & Daneman, M. (1995). How young and old adults listen to and remember speech in noise. Journal of the Acoustical Society of America, 97, 593-608.
Pichora-Fuller, M.K., Schneider, B.A., MacDonald, E., Pass, H.E., & Brown, S. (2007). Temporal jitter disrupts speech intelligibility: a simulation of auditory aging. Hearing Research, 223, 114-121.
Rosenstock, I. M. (1974). Historical origins of the health belief model. Health Education Monographs, 2, 328-335.
Ryan, E.B., Giles, H., Bartolucci, G., & Henwood, K. (1986). Psycholinguistic and social psychological components of communication by and with the elderly. Language and Communication, 6, 1-24.
Ryan, E.B., Meredith, S.D., Maclean, M.J., & Orange, J.B. (1995). Changing the way we talk with elders: Promoting health using the Communication Enhancement Model. International Journal of Aging and Human Development, 41, 89-107.
Sarampalis, A., Kalluri, S., Edwards, B., Hafter, E. (2009) Objective measures of listening effort: Effects of background noise and noise reduction. Journal of Speech, Language, and Hearing Research, 52, 1230-1240.
Schmader, T., Johns, M., & Forbes, C. (2008). An integrated process model of stereotype threat effects on performance. Psychological Review, 115, 336-356.
Singh, G., Pichora-Fuller, M.K., & Schneider, B.A. (2008). Auditory spatial attention in conditions of real and simulated spatial separation by younger and older adults. Journal of the Acoustical Society of America, 124, 1294-1305.
Singh, G., Pichora-Fuller, M.K., & Schneider, B.A. (2010). Age-related differences in auditory spatial attention depend on task switching complexity. Journal of the Acoustical Society of America, 127, 1810.
Smith, S.L. & West, R.L. (2006a). The application of self-efficacy principles to audiologic rehabilitation: a tutorial. American Journal of Audiology, 15, 46-56.
Smith, S.L. & West, R.L. (2006b). Hearing aid self-efficacy of new and experienced hearing aid users. Seminars in Hearing, 27, 325-329.
Smith, S.L., Pichora-Fuller, K.M., Watts, K.L., & La More, C. (2011). Development of the listening self-efficacy questionnaire (LSEQ). International Journal of Audiology, 50(6), 417-25.
Taylor, S. E., & Sirois, F. M. (2009). Health psychology: Canadian edition. McGraw-Hill Ryerson: Toronto.
Tinetti, M. E., Richman, D., & Powell, L. (1990). Falls efficacy as a measure of fear of falling. Journal of Gerontology, 45, 239–P243.
Troyer, A.K., & Murphy, K.J. (2007). Memory for intentions in amnestic mild cognitive impairment: time- and event-based prospective memory. Journal of the International Neuropsychological Society, 13(2), 365-369.
Schneider, B. A., Daneman, M., Murphy, D. R., & Kwong See, S. (2000). Listening to discourse in distracting settings: The effects of aging. Psychology and Aging, 15, 110-125.
Weinstein, B., & Amsel, L. (1986). Hearing loss and senile dementia in the institutionalized elderly.Clinical Gerontologist, 4, 3-15.
Weinstein, B.E., Spitzer, J.B., & Ventry, I.M. (1986). Test-retest reliability of the Hearing Handicap Inventory for the Elderly. Ear and Hearing, 5, 295-299.
Wilson, R.H., Abrams, H.B., & Pillion, A.L. (2003) A word-recognition task in multitalker babble using a descending presentation mode from 24-dB S/B to 0-dB S/B. Journal of Rehabilitation Research and Development, 40,321–328.
World Health Organization (2001). International classification of functioning, disability and health (ICF). Geneva, Switzerland.