Learning Outcomes
After this course learners will be able to:
- Describe the impact of severe hearing loss on the perception of speech through hearing aids.
- Identify the criteria that patients with severe hearing loss use when judging the impact of amplification.
- Identify the most appropriate technology choice for each individual.
Introduction
I am Don Schum, the Vice-President of Audiology at Oticon in the U.S. In today's seminar, we are going to discuss managing patients with severe hearing loss. In the fall of 2019, Oticon released a new line of power and Super Power products available to clinicians. We think it's important to understand what it takes to be able to provide good solutions for patients with this amount of hearing loss. At Oticon, we have a long legacy of building excellent power, Super Power and Ultra Power products, dating back for several decades. Because of that, we have spent a lot of time over the years researching this patient demographic, including their perceptions, their needs, and their preferences. We take all this into consideration when we build our products. However, in order to get the most out of the products, it's critical to have a good understanding of severe hearing loss.
The Ability to Fit Severe Hearing Loss: A Lost Art
To begin, let's address the reason why it's important to talk about fitting patients with severe hearing loss. In my opinion, it's starting to become a lost art. In the mid-1980s, patients with a severe hearing loss almost exclusively wore acoustic amplification. Essentially, that was the only option. Cochlear implants (CIs) were just coming into reality in the clinical marketplace. They were mostly research devices. At that time, CIs were not particularly sophisticated, in terms of signal processing, compared to the way they work now. If you were fitting hearing aids in the mid-1980s, you likely had a lot of patients with severe hearing loss in your caseload. As implants have become more and more sophisticated, as implants have been proven effective for patients in this hearing loss group, many of these patients have moved into the range of using CIs. Because of that, the ability to fit patients with severe hearing loss has become a lost art in our field. Granted, not all patients with this amount of hearing loss can be implanted. The reality is that sometimes the patient may choose not to be implanted. They may have a medical condition that won't allow them to tolerate the surgery. Perhaps there is a physiological reason they can't be implanted. The fact remains that these patients do exist and they need to be treated.
Oticon Solutions
Since not every patient can be implanted, we need to explore the non-implantable options for these patients. In the fall of 2019, Oticon released some new products (Figure 1), including Oticon Xceed (Levels 1, 2 and 3), our pediatric line, Oticon Xceed Play (Levels 1 and 2), and our Oticon CROS/BiCROS solution.
![]()
Figure 1. Oticon Xceed, Xceed Play and CROS/BiCROS.
In the Xceed product family, we have both a Super Power (which is based on a 13-size battery) and an Ultra Power (which is based on a 675-size battery). Our pediatric Xceed Play product is physically the same size as the traditional Xceed, but as a pediatric-based product, they do have different capabilities as compared to those that would be worn by an adult. We've released a CROS transmitter that's designed to mate with all of our products that are on the Velox S platform and above, which includes Opn S, 1, 2, and 3 and Opn Play 1 and 2. All of the products that we've released in 2019 can now be compatible with our CROS transmitter. Coming up later in the presentation, we will spend some time talking about that capability and how to make that up for patients.
For more information on the products that we've released in the fall of 2019, there are additional AudiologyOnline courses available that cover all the details about these products. As such, for the purposes of this presentation, I will focus on how to use these products to solve specific problems for specific cases that you may encounter as a clinician.
Physiology of Severe Hearing Loss
With regard to the physiology of severe hearing loss, the variability across patients is very high. As such, if you're going to fit patients with severe hearing loss, you require an adaptive fitting mindset. In other words, simply putting the audiogram in our Genie fitting software and obtaining prescribed settings is not necessarily going to be a solution for each and every patient. That variability exists anytime you fit hearing aids, but it is especially true of patients with severe to profound hearing loss. With this patient population, there is a greater need to make adjustments based on individual preferences and perceptual performance. If you're going to fit someone with that degree of hearing loss, you must accept the fact that you're going to have to spend more time to find the fitting that works well for that patient. Moreover, the severe to profound clinical population needs highly trained clinicians to conduct an adaptive fitting and to understand the nature of hearing loss and how the technology works. It is important to recognize that in the ever-changing hearing aid device market, these patients aren't likely to find an over-the-counter or internet-purchased solution that will work for them. Hearing care professionals will always need to play a role in fitting these patients with severe and profound losses.
As hearing care professionals, when we discuss patients with one another, we have a tendency to describe the patient based on their audiogram. And while the audiogram is a reasonable snapshot of a patient's hearing impairment, it's only part of the story. Hearing impairment is a physiological change in the way the auditory system works. The audiogram is one reflection of that, but it is a limited reflection. Therefore, understanding what could be happening inside the person's peripheral auditory system is essential, especially when dealing with this group of patients. The knowledge that hearing loss is a change in physiology, and that the change in physiology is going to cause a change in perception is important to keep in mind with this patient group.
When we discuss hearing loss, we talk a lot about inner and outer hair cells. Much of our legacy in using multi-channel, non-linear products over the years has been driven by a model of hearing loss that mainly talks about hair cell loss. With mild to moderate loss, it's mostly outer hair cell loss and not inner hair cell loss. Once you get above about a moderate hearing loss, you're dealing with more inner hair cell loss. However, in patients with severe and severe to profound hearing loss, it's important to realize that there are a lot of other things going on in the auditory system that could change, other than just hair cell loss.
There is a lot of physiology that has to be working properly for hearing to occur. It's not just that the inner hair cells bend and fire and send a signal up the eighth nerve, but all the other supporting structures and physiology that has to be in place to make sure that the inner hair cells can fire appropriately. For example, the inner hair cells sit within a certain chemical bath. It's part of this two-chamber system in the inner ear, and there are different fluids in there, the endolymph and the perilymph. They need to have different chemistries; the potassium and sodium content has to be different in those fluids in order to create the electrochemical environment that is necessary for hair cells to fire. Inside the inner ear, you have these membranes that have to be intact for all these mechanisms to work. You have stria vascularis on the wall of the inner ear providing blood flow to all the structures of the inner ear. The inner ear is sensitive to having good, healthy blood flow. If the patient is dealing with any amount of restriction in that area, it could throw off the physiology. You need to have nerve structures, you need this connection between the hair cells and the nerve fibers that lead into the eighth nerve and go up into the central auditory system. All that structure and physiology needs to be working right.
When you deal with some of the etiologies that will cause severe or profound hearing loss, you could be talking about things that go well beyond just hair cell loss. You could have changes in any of the other physiological structures. For example, in cases of meningitis, you can get ossification within the inner ear. With Meniere's disease, patients may have experienced repeated ruptures of those membranes, throwing off the fluid chemistry within the inner ear or resulting in scar tissue such that the membranes don't work as they should. A whole host of things can go wrong, contributing to the complication of the perceptual condition of these patients' ears.
In addition to the fact that many structures are involved in severe to profound hearing loss, it's important to consider how long the individual has had the hearing loss. For example, you might have two patients with the same audiogram. One of those patients has had that audiogram for 40 years and they started wearing hearing aids when they were a child. They change their hearing aids every three or four years. By the time you see them as an adult, they may be on their tenth set of hearing aids. In contrast, an individual who has experienced a sudden or rapidly progressive hearing loss has not had as much time to adapt as someone with a lifetime of hearing loss. The person with newly developed severe hearing loss may experience poor word recognition as a result of their recently disrupted auditory system. They may have a different perceptual experience, as compared to the person with life-long hearing loss. In short, the audiogram does not tell you everything you need to know.
Patient Performance
As stated earlier, there is a lot of variability in patients with severe to profound hearing loss. To illustrate this variability, we will look at patient performance by examining two different research studies. The first study (Lamore et al., 1990) focused on speech understanding in quiet. The second study measured speech understanding in noise (Souza, 2009).
Speech Understanding in Quiet
In the 1990s, researchers in Holland looked at speech discrimination/word recognition scores as a function of average hearing loss, measured in quiet at frequencies of 0.5, 1 and 2 kHz (Figure 2). When you measure word recognition performance or speech discrimination performance, you need quiet environments up to or through about a moderate hearing loss (60-65 dB). There's not a lot of variability in patients with this amount of hearing loss in terms of their core speech understanding performance in quiet. You can see some variations, but at least in this data set, all the patients with up through moderate hearing loss scored somewhere at 80 percent or above. Once you get into the 70 to 80 dB range of hearing loss, the variability goes way up. For example, one person with an average hearing loss of around 90 dB has a speech discrimination score better than 90 percent. In contrast, another person with the same average hearing loss scored as low as 10 percent. The performance is all over the board by the time you get into the severe hearing loss category. There are a lot of different things going on with these patients depending on the etiology and the duration of the hearing loss. In addition, depending on the physiological structures involved (some of which are damaged and some of which are still functioning), you won't know how well that system is going to work until you test it. You can test it using headphones in your booth to get an idea of their perceptual performance, but more importantly, you need to determine what sort of absolute performance they can get out of their hearing aids using the remaining functioning physiology.
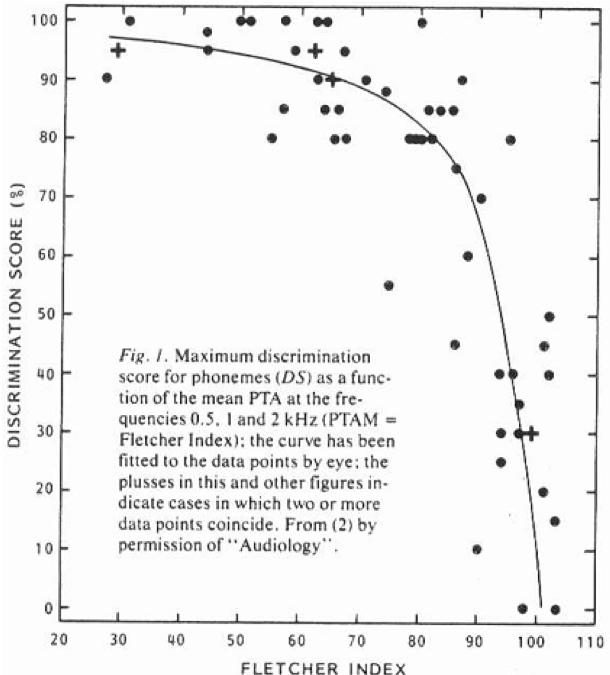
Figure 2. Maximum speech discrimination as a function of average hearing loss.
Speech Understanding in Noise
In 2009, Pam Souza tested two groups of patients on speech understanding performance in noise using the QuickSIN (Figure 3). One group of patients had mild to moderate hearing loss (represented by the blue dots), and another group of patients had severe hearing loss (represented by the red dots). When you move into noise, you see a little bit more variability in the patients with a lower degree of hearing loss, but you see a much greater range of variability when we look at those with more severe hearing loss. Clearly, whether you're looking at speech in quiet or speech in noise, variability is one of the big keys to understanding what to expect out of this population.
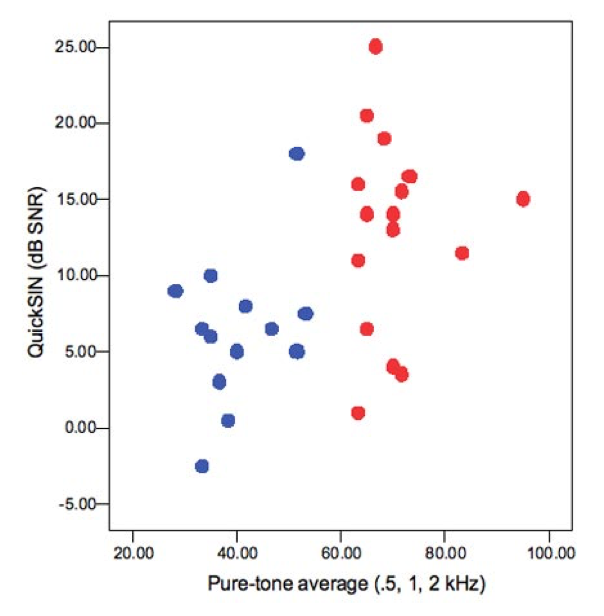
Figure 3. Speech understanding in noise: mild to moderate vs. severe hearing loss.
There are two fundamental cue sets that we use when we're tracking speech. One is spectral cues or frequency cues. The other set of cues are temporal cues. Every phoneme occurs in a different frequency region. Temporal cues are the rhythm of speech. The phoneme to phoneme differences in level. Even within a phoneme, the level may go up and down and change over time. Frequency cues or spectral resolution is one of the first things to go when you have hearing loss. Your ability to tell the difference in the frequency of two different sounds is one of the first things that gets affected by sensorineural hearing loss. That's usually thought to be related to the fact that as you lose outer hair cells, you begin to lose the fine-tuning of the inner hair cells. That seems to be the job of the outer hair cells: to modulate and sharpen the tuning of the inner hair cells.
What ends up happening is, as you lose frequency resolution, you have the tendency to then focus on the cue set that still works well for you, which are temporal cues or temporal resolution. Temporal resolution is a more robust skill set that seems to be a little bit more resistant to loss when you have hearing loss (although eventually, you can lose all your temporal resolution, too). People with classic profound hearing loss might have poor temporal resolution. In this range, especially for patients with severe hearing loss, they probably have shifted their use of cues in speech much more towards using temporal cues and not frequency cues. The reason why that's important is that there are a lot of things that we could do in non-linear hearing aids to disrupt temporal cues. Remember that the job of a non-linear hearing aid is to change the amount of gain you apply to a signal, based on its input level. If you have speech (which changes in level all the time), if you are too aggressive with the way you use compression (especially faster-acting compression), by design, what you're trying to do is get rid of temporal variations in the signal. However, that could be a primary cue set for someone with this amount of hearing loss. I'll talk about the design of our new Super Power product Xceed and Xceed Play, both in Super Power and Ultra Power, where we specifically have done some things in those products to try to preserve the temporal information in the speech signal.
Residual Capabilities
Another topic that is relevant to the nature of severe and profound hearing loss is the notion of residual capabilities thinking. To illustrate residual capabilities, I'd like to use an analogy of fitting a pirate with a peg leg. How would you go about fitting a peg leg to a pirate? You would probably have the pirate lay down and you would measure the length of his good, remaining leg and you would measure the length of the leg that has been lost, and you would find out the differences, right? Then you would cut a piece of wood that is equal to the length of the difference between the fully intact leg and the leg where it's missing a part of it.
Of course, this is an oversimplification and is not the way modern prosthetic devices are fit. Today, when someone is being fit with a prosthetic device, there is an emphasis on not only replacing what is lost but also a focus on their remaining functioning physiology. A person who has lost part of their leg still has some bone and muscular structure, and possibly even some neural structures that can be tapped into. This way of thinking is known as residual capabilities. The job of someone who fits modern prosthetic devices is to understand the patient's remaining physiology and figure out a way to use technology to get the most out of that remaining physiology, in order that the patient can return to an acceptable level of function.
Now, I want you to think about how we fit hearing aids. What is the only measure we have to make in order to fit a hearing aid? Of course, that is the audiogram. The audiogram is a measure of how much hearing the person has lost, and how much the sensitivity levels in the ear have changed. We need to know how much pure-tone hearing loss a person has because we have to be able to compensate for audibility. But as I said earlier, the audiogram is not a complete description of the remaining physiology that the patient has. When you're working with patients in the severe to profound range, that remaining physiology is very important. That's what we get to work with. It is critical for all hearing care professionals to use this residual capabilities way of thinking. To remember that we are trying to figure out how to make the best use of the remaining physiology that the patient presents. We can't regrow hair cells. We can't make the peripheral auditory system work in a normal way anymore. It's broken. The hearing that the patient has when they walk in your office is the hearing that they have when they walk out of the office. Our challenge is to change sound in such a way that the patient's remaining physiology can get the best use out of that sound. That's a good mindset to have when you're dealing with patients with severe to profound hearing loss.
Success Criteria: What Matters to the Patient?
How will a patient judge the value of a hearing aid? In order for a patient to make a judgment that the fitting works well for them, it has to be on a dimension that's meaningful to that patient. Patients with severe to profound hearing loss have a great deal of variability. Because of that, the patient will need to be the guide, telling you whether or not the hearing aid fitting is doing anything worthwhile for them. Sometimes, we can measure improvement using a standard audiometric measure like speech understanding in quiet or noise, which is something that a lot of clinicians would be very comfortable with. But sometimes you may not see a change or improvement in that level because perhaps the patient's auditory system is so compromised that speech understanding without visual cues is not something that they're ever going to achieve. However, the patient might have judgment based on their ability to identify environmental sounds or the idea that they can combine the auditory signal with visual cues or a lot of other dimensions that might not necessarily fall in the standard clinical practice. Especially patients who've had this hearing loss for a long period of time, they can be very specific about what they feel that they need from their hearing aids.
One of the challenges in dealing with these patients is when you try to change the type of hearing aid that they wear, sometimes they become resistant to change because everything that they hear comes through that hearing aid. They're dependent on the auditory signal that they get through that hearing aid. If you do anything to change the sound of that hearing aid, they can become very reactive. When we moved into the era of multi-channel, non-linear products, it was quite difficult to take patients who had longstanding, powerful linear hearing aids and transition them into a non-linear fitting. Often, a patient will get so locked into a sound quality that they're used to hearing that moving them to a different device can be a challenge.
When working with this type of patient, we need to be mindful of the fact that each patient's criteria of what matters most to them can be different. Furthermore, what the patient deems as important may not necessarily strike you, the clinician, as something that you would think of as being important. Here's a list of some of the criteria that patients, especially in this hearing loss group, might use to judge whether they have a good hearing aid fitting.
- Improved performance in challenging environments
- Improved access to speech in quiet
- Improved awareness
- Speechreading support
- Connectivity
- Better confidence
Design of Power Products
For the purposes of this presentation, I want to point out a couple of things about the design of our products that can help to achieve good fittings for patients in this group. For the last several generations of Super Power products, we have had a dedicated fitting rationale designed specifically for patients with severe or severe to profound hearing loss to help them get what they need out of their hearing aids. We call that fitting rational dynamic speech enhancement or DSE.
There are three main factors to take into consideration when working with this group of patients:
- Adequate loudness perception
- Need for audibility takes priority
- Importance of temporal cues
First, with this severe to profound group of patients, it is important to get the loudness correct, especially if they have had a history of using linear hearing aids. They often get very accustomed to a certain loudness perception out of the hearing aid. In the early days, when people started trying to use multi-channel non-linear hearing aids to fix severe hearing loss, they often failed. This is because they typically were using a lot of fast-acting compression which can result in a muddled signal. For patients with severe hearing loss who needed to hear that "punch" out of the signal, they just weren't getting that.
Second, we need to try to give these patients whatever audibility we can. One of the reasons we try to use non-linear with patients with this amount of hearing loss is to try to get what we can to fit in the remaining dynamic range. We have to do that in a careful way in order for it to work well for these patients.
The third point is that you want to make sure that you protect temporal cues in the signal. Like I stated earlier, these patients typically have poor frequency resolution. You want to make sure that if they've shifted their perception to be dependent on temporal cues that you do the best job possible in protecting these cues. If you take a typical non-linear approach to treating patients with severe hearing loss, because these patients typically have a reduced dynamic range, there is a tendency to try to give them too much compression. You're trying to get a lot of sound to fit in that remaining dynamic range. Because of the resolution of their system, because of what they've grown up listening to, because of the need for loudness, that might sound like too much of a muddled signal for them.
The DSE Strategy
With DSE, we try to make sure that moderate speech inputs are presented within the patient's dynamic range in a more linear fashion. This is a case where linear is good. Linear hearing aids are an older technology, but the idea of being linear in an engineering context means that the output of a system directly reflects the characteristics of the input. There's a lot of information embedded in the speech signal, especially in the temporal cues. You want to process that information in a linear way so that those temporal cues are maintained. Compression can minimize those temporal cues. Instead of trying to get the entire dynamic range of speech to fit within the patient's dynamic range, we do the best job possible of making sure that moderate speech is presented in that remaining dynamic range in a very linear fashion. Moderate level speech is what the patient listens to most of the time. We want to make sure that most of the time they are getting a signal that works well for them. If they happen to be in a softer sound environment where someone's using soft speech, these patients will then just have to turn it up using a volume control wheel. Remember these people are experienced hearing aid users, and they typically don't have a problem with making adjustments on the fly. In some cases, you don't want to sacrifice and use a lot of compression because you don't want the patient to ever have to touch the volume control. However, that's just unreasonable with these patients. If you think about it in terms of protecting moderate level inputs, then you can get a sound quality out of the product and a perceptual effect out of the product that could be much more effective.
With DSE, we take a look at the primary knee point (Figure 4). For most multi-channel, non-linear hearing aids on the market (such as Oticon products OPN-S 1, 2, and 3), we typically have that primary knee point down around 45 dB SPL or so. With severe to profound hearing loss, we move that primary input up to around 65 dB. By moving the primary knee point up to 65 dB, that full range of moderate level inputs still falls within the linear part of the input-output function of the hearing aid. We then set the gain for louder speech. In Figure 4, the area between where the gray shading ends and where the blue shading ends are the upper level, peaks of louder speech. We move those peaks up right below the MPO of the hearing aid. We do the best job we can of getting as much extra room out of the patient's dynamic range and put the louder speech levels up there. Patients are not in situations with loud speech as often as they are in situations with moderate speech. Nowhere near as often. We do have to use compression there, and so we have a non-linear section to the hearing aid, but it's a relatively short compared to what we would do for patients with mild to moderate or moderate hearing loss. DSE is a specific fitting rationale designed to give the perceptual treatment that patients with this amount of hearing loss typically need.
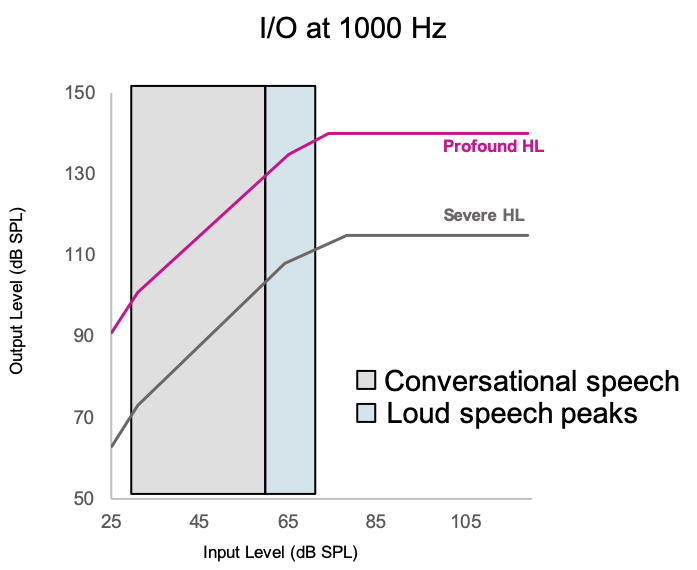
Figure 4. Dynamic Speech Enhancement model.
Speech Rescue LX
Another feature that we have in all of our products (and becomes very relevant in the Power and Super Power products) is our approach to frequency lowering called Speech Rescue. We use a frequency composition approach as opposed to frequency compression. With frequency compression, you're taking the full bandwidth of the speech signal and basically squeezing it down into the mid frequencies. With frequency composition, we identify certain frequency areas up in the very high frequencies that are most likely to be inaudible for the patients and we replicate those areas in the mid frequencies where they can be audible. When we do that, we don't eliminate the very high frequencies, because you never know what the patient might potentially be able to get out of that information. The idea is that we wanted to take that information up there and make it available in the better functioning, and at least more audible, mid frequencies. We call our approach, frequency composition. It's available in almost all of our products, but we don't necessarily see a big use for it until you get it down to this degree of hearing loss. The idea is to try to use a more gentle hand in the way we treat the speech signal. We believe that there's a lot of important information embedded in the speech signal in a natural way, and we don't want to do anything that's too dramatically disruptive to that speech signal.
Triaging Patient Needs
Now that we've talked about the way we put together our Power and Super Power products, let's discuss triaging patient needs and trying to understand which products make the most sense for patients. It's not just about the audiogram. Of course, the audiogram matters because you want to make sure that you're providing enough gain to make things audible, but there are a lot of other things that could affect the way the patient responds to amplification. Here is a partial list of factors to consider when matching the right technology to each patient. As I go through some case examples later, I will touch on each of these factors and how they could impact the type of device that you recommend to a patient.
- Thresholds
- Speech understanding ability
- Asymmetries
- Perceived communication needs
- History with amplification
- Etiology
- Duration of loss
- Willingness to accept invasive devices
Oticon Product Choices
Figure 5 shows the fitting ranges of our miniRITE line of products, the Opn S 1, 2, and 3. These products allow for the use of different speaker units which provide different gain and output and, thus, different fitting ranges. The 100 or 105 speakers can be an option for patients who are approaching the severe hearing loss range. Our miniRITE R offers rechargeability, which may be important to the patient. If they have thresholds down in the 75 to 80 dB range, you might consider using the miniRITE products instead of going right to the Super Power products. Part of the decision-making process is going to depend on how stable you feel their thresholds are. If they've had an audiogram down at 75 or 80 for 10 years, and you think there's nothing about their etiology that would expect them to move, then you do have the capability of getting that amount of power out of a 312 size miniRITE product. Sometimes clinicians forget that these miniRITE products, although they're small and sleek, they also can provide a significant amount of power if you put the right receiver on them.
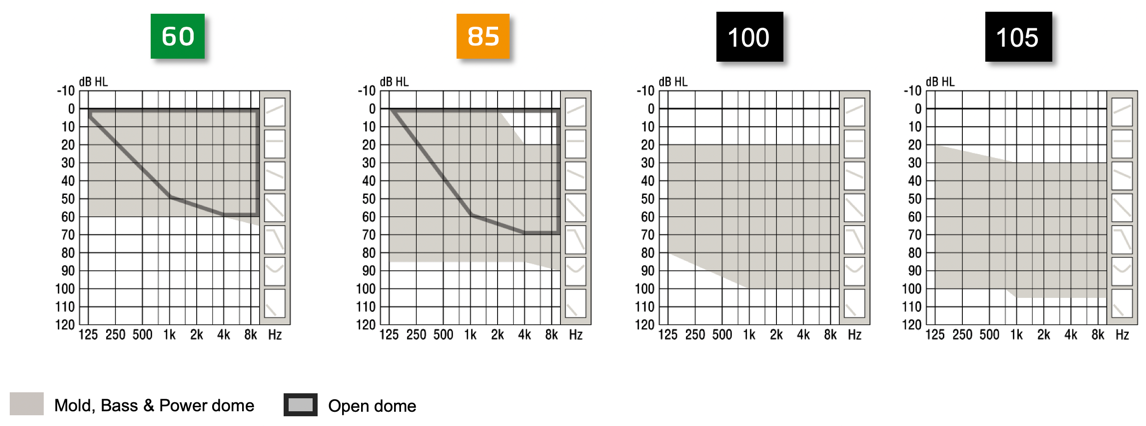
Figure 5. miniRITE, miniRITE T and miniRITE R fitting ranges (now also for severe-to-profound losses with miniFIT receivers)
Figure 6 shows our fitting ranges for our new Xceed products, the BTE Super Power (SP) and BTE Ultra Power (UP) products. They go down to 110 or 120, in terms of fitting range. We also have a BTE Power Plus that goes down to about the 105 level. They do extend the fitting range significantly compared to the miniRITE line. Not all severe hearing losses are the same. Someone with a severe hearing loss of 75-80 dB is going to be very different than someone who has thresholds at 80 and 90, up to about 1 kHz, and then drops down into the 100-105 level. That's a different class of severe hearing loss. Again, it is important to take a close look at the audiogram and determine how stable you think the audiogram will remain.
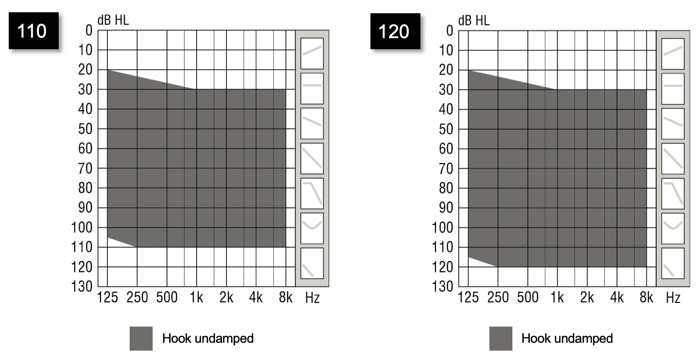
Figure 6. BTE SP and BTE UP fitting ranges (for severe and profound losses).
Figure 7 shows the SPL maximum output and the full-on gain for our Ultra Power products. Notice those peaks jumping up at 1 kHz at a very high level. When you build Super Power products, in order to get that loudness "punch" that people with severe to profound and profound hearing loss need, you need to be focused on getting that 1 kHz peak right. Many of these patients have grown up wearing linear based products with that strong 1 kHz peak. In order to get good maximum output levels and maximum gain levels, you need to make sure that it gets down in the mid-frequency 1 kHz range. Before you do anything else, you have to make sure that you get the loudness right for these people. That's why the shape of the frequency response looks as it does. When you're dealing with receivers that can give you that amount of output at 1 kHz, you're naturally going to see a roll-off in the high frequencies. That's why it's important to consider carefully whether or not you want to be using the RITE product line or the Power Plus product line versus going right to the Ultra Power or Super Power products. Because you have a different type of frequency response when you're dealing with that amount of gain and output in a hearing aid. When you're trying to size up your patient, keep in mind the fitting range that's available on the product. It's not necessarily just their thresholds that you have to consider, but it's the whole picture of what you expect out of these patients. If they have some usable hearing out there in the high frequencies (to 2 or 3, or even 4 kHz), you want to make sure that you're choosing the right product to get as much as you can out there in the higher frequencies. Oftentimes when you're dealing with patients with severe and severe to profound hearing loss, the idea of getting any good audibility out past about 1500 or 2 kHz is unreasonable. But if you're talking about someone with 80-85 dB thresholds out at 2, 3 or even 4 kHz, then the idea of getting audibility out there is feasible. You don't want to rule that out too quickly.
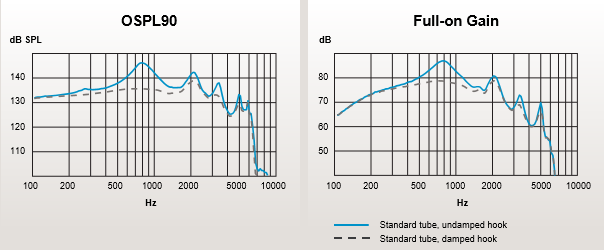
Figure 7. Oticon Xceed with industry leading output and gain.
Another product that we released this fall is our CROS transmitter. The CROS transmitter is designed for patients who have a "dead" ear. It takes sound coming in the dead side and sends it to a hearing aid over on the good side, passing the signal through without any additional gain (other than overcoming the insertion loss of using that product). In a BiCROS situation, the hearing aid functions also as a hearing aid for the hearing loss that the patient has on that side. Many hearing care professionals have strong opinions one way or the other about using CROS. Some use it a lot, while some feel that there isn't a great need for it, or they have had trouble getting patients to accept it. In general, the acceptance of CROS on the part of the patient will come down to their perceived need and if they feel that they're having so much listening difficulty that they're willing to wear devices on both ears in order to defeat the head shadow effect.
Asymmetrical Hearing Loss
Before we go over some case examples, I want to discuss asymmetrical hearing loss. The main goal in fitting someone with asymmetric hearing loss is about trying to achieve that single, unified image, which can be tricky. This relates to the idea of fitting CROS. Patients with asymmetrical hearing loss, based on the nature of their etiology may often have severe hearing loss. Of course, we do see asymmetries in patients with moderate hearing loss, but many of the etiologies that create significant asymmetries often create significant threshold loss. As such, I will often talk about asymmetries at the same time I'm talking about severe hearing loss because there's a lot of crossover between the two.
Types of Asymmetries
There are different types of asymmetries:
- Both ears reasonably aidable, one better
- One dead ear, one aidable
- One normal ear, one aidable
I'd like to share one observation about the decision to recommend CROS or BiCROS. When you make that recommendation to a patient, you have basically told them that their poorer ear is totally unusable and that you are going to bypass that ear. Any sound that occurs on that side of the head, we're going to move over to the other side of the head. That's the basic idea behind CROS. That is the assumption that you're making. I think there are a lot of clinicians who will make that judgment before they can really be sure.
I want to give you an example from the literature. Over 20 years ago, Feldman and Oviatt had a patient with a sloping hearing loss in the left ear who had a history of using amplification on that ear. On the right ear, the patient had a flat, severe hearing loss with no measurable word recognition under headphones. Supposedly, this patient had never been given the opportunity to wear a hearing aid on the right ear. They had only been wearing a hearing aid either on the left ear or a BiCROS setup. These clinicians wanted to see if that ear could participate at all in terms of perception, even though there was no measurable word recognition under headphones in that ear. A lot of clinicians simply would not have tried that, but these clinicians decided to give it a shot.
Figure 8 shows the aided results both in quiet and in noise wearing a hearing aid only on the left ear, and then wearing binaural hearing aids. One of the things that you will notice is a significant improvement, both in quiet but especially in noise, by adding a hearing aid to that ear that otherwise was considered to be unusable for the patient. To me, it only takes one good example to make the point that you don't know for sure if an ear is unusable until you actually put a hearing aid on that ear. All you're losing is a little bit of time by fitting a hearing aid on that ear to find out if the ear is usable.
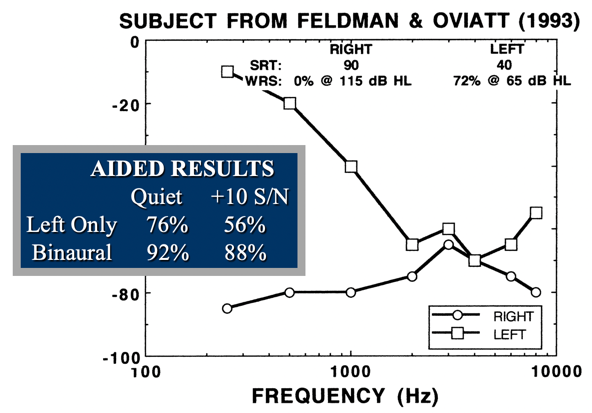
Figure 8. Feldman and Oviatt results (1993).
In many of these cases of asymmetries, you'll end up wanting to fit two ears, but you don't necessarily have to fit two ears at the same time. One of the techniques that I've found to be useful is that when you're dealing with significant asymmetries between two ears, you might consider fitting the hearing aids on different days. If you have a significant amount of asymmetry between the ears, one ear is the better, dominant ear that the patient listens through. That ear is going to do the "heavy lifting" of perceptual tasks for that patient. The other ear might be useful, but you definitely don't want the other ear to compete with that better ear. One technique is to fit that better ear first and give the patient a week or two to get used to that fitting. After that one to two weeks, add the second ear. In delaying the fitting of the second ear, you decrease the amount of confusion that the patient might develop, in terms of what they're hearing. If you take two hearing aids and put them on a significantly asymmetrical auditory system and the patient doesn't like the way it sounds, they might have a hard time discerning exactly what it is about the sound that is throwing them off and what they don't like. However, if you fit the better ear first, followed by the poorer ear, you can improve the decision-making process for the patient. They won't get quite so confused about that. When I walk through these cases next, you'll get some ideas on how that could be applied.
Understanding the right match of technology to each patient is influenced by many factors that can be unique to these populations. Some factors to consider are:
- Thresholds
- Speech understanding ability
- Asymmetries
- Perceived communication needs
- History with amplification
- Etiology
- Duration of loss
- Willingness to accept invasive devices
Clear candidates for Super Power and Ultra Power are patients with audiograms down in the 90 dB range, where you need to deliver a lot of power into the ear. A clear candidate for CROS might be someone who's had an eighth nerve resection on one ear, who has a lot of listening needs who wants to be able to have sensitivity to that truly dead side. A clear candidate for BiCROS might be a patient who has a truly dead ear on the one side and needs a hearing aid on the other ear because that's the only ear they listen with and there is a lot of hearing loss. However, there are a lot of gray areas, which we will see in some of these case examples.
Case Examples
Case #1
A 24-year-old female patient who had worn hearing aids all her life came into the clinic presenting with a flat, severe-ish hearing loss. As you can see in Figure 9, she had a limited dynamic range. Her last set of hearing aids was 10 years old and she stated that everything sounded "loud and rackety".
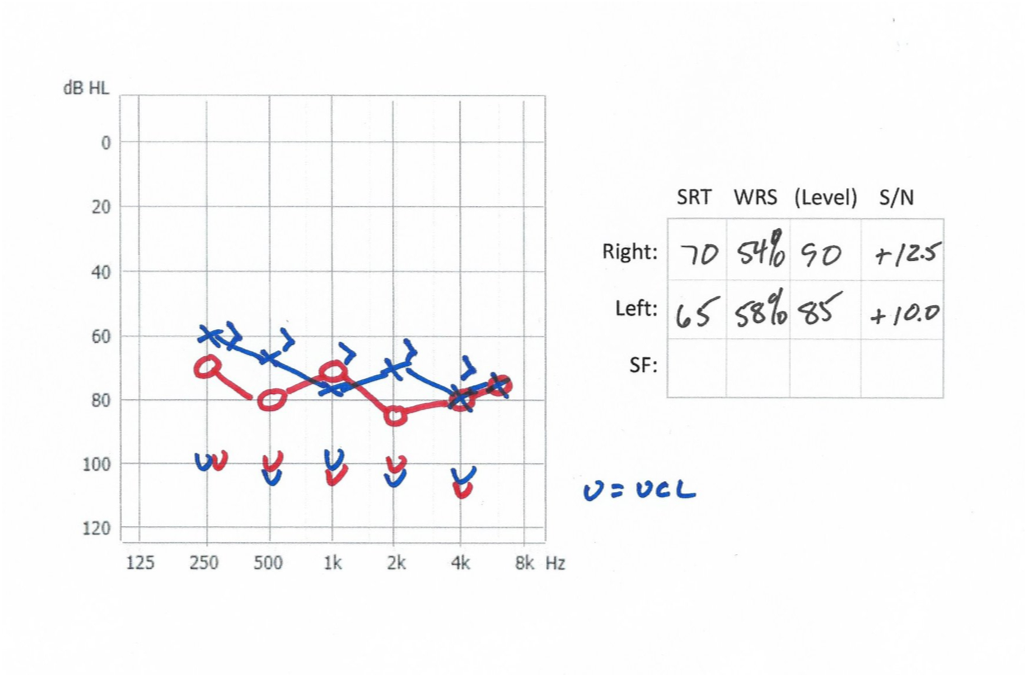
Figure 9. Case #1.
The solution for this patient was to move her from a primary linear hearing aid into a multi-channel, non-linear hearing aid. Given this patient's age, and given the fact that the resolution in her auditory system was still reasonably good, there was still some usable hearing going on in that ear. Moving that patient into a non-linear hearing aid was the right solution for her. Because the patient had a lot of threshold loss, when the older hearing aids were fit, we had to put a lot of power into that ear which she now considered to be loud and rackety. She said when she was younger, she was the type of teenager who didn't want to use her hearing aids because she was getting a lot of linear power out of the hearing aid that was too much for her. In this case, the low UCLs in those ears indicated that she needed a multi-channel, non-linear approach. This would be a case where perhaps some of those RITE products would still make sense for that patient.
Super Power or Ultra Power?
You may wonder whether or not you want to fit Super Power or Ultra Power on patients. Remember Ultra Power gives you about 5 dB more gain in output than you would get with the Super Power. One of the keys to making that decision comes down to what happens above 1 kHz? For example, in Figure 10, looking at the blue audiogram for the left ear, you see this drop off above 1 kHz. It's probably unrealistic to think that there's any reason to provide much amplification up here in this region. The threshold to support it's even unmeasurable at 4 kHz. Whatever is out there, even if you can establish a threshold, there is probably very limited residual capability in that ear. This patient would be a good candidate to shift into this low-frequency, dominant, classic Ultra Power fitting.
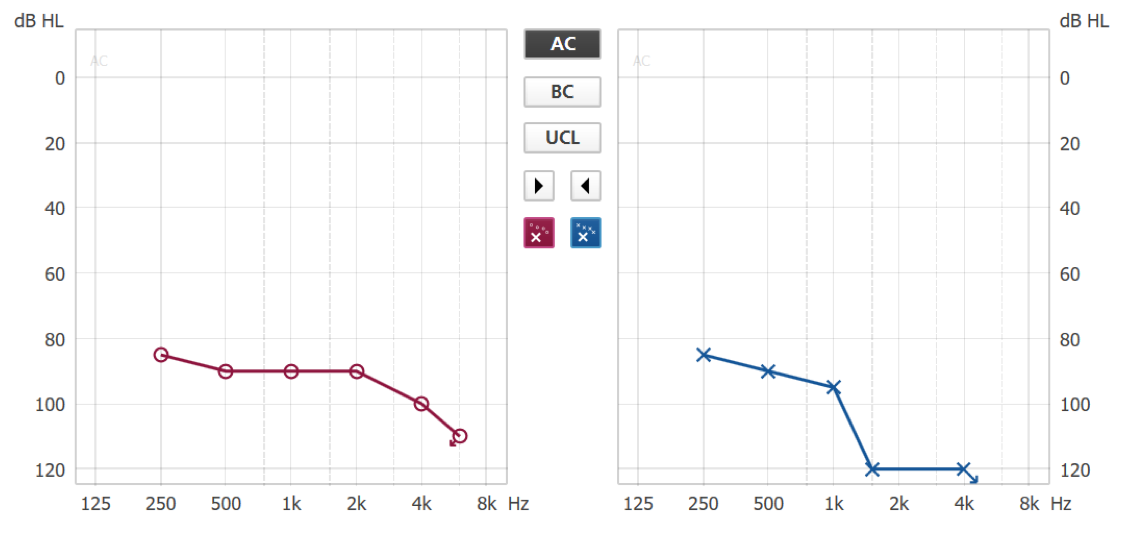
Figure 10. Super Power or Ultra Power?
In contrast, looking at the red audiogram in Figure 10, this patient has measurable, reasonable thresholds all the way out to 4 kHz. To me, this region from 1 kHz to 4 kHz is the key. You can probably reach that using a non-linear approach with patients and probably give them some good speech recognition. This is probably more of a Super Power type fitting where you are still thinking that there could be enough good resolution in that hearing to get some speech perception up in that mid- to high-frequency region. Don't let the thresholds scare you into thinking, "I need to get as much power as I possibly can," because you can easily overpower these losses. You might want to treat it more classically, like a moderately-severe hearing loss, where you can't expect something out of the mid- to high-frequencies from an ear like that. Again, keep in mind the fitting ranges of these products. You're not getting quite as much fitting range out of the Super Power as out of the Ultra Power, but you could still get some reasonable gain out of those products to reach those hearing losses.
Case #2
Figure 11 shows a classic CROS patient. I fit a CROS for this patient because he had a high demand on his hearing. He was a police officer in a small rural town and he was allowed to continue at his job as long as he wore his hearing aids. He felt a better sense of security wearing a CROS transmitter on his unusable ear. I tried that ear and there was nothing I could get out of it. I fit him with a CROS and he was happy with it because at work he felt more secure having the sensitivity off to his left side.
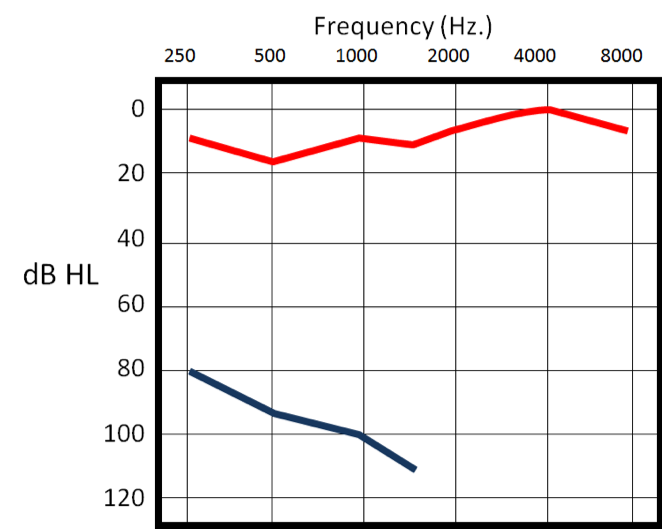
Figure 11. Case #2.
One of the things about classic CROS fittings that I would have you consider is the way CROS hearing aids work these days. You fit the transmitter on the unusable side and it goes to a regular hearing aid over on the usable side. Even though the patient might have quote normal thresholds, that doesn't mean that they wouldn't appreciate a little bit of mild high frequency gain over on that ear. Remember, everything they hear is only going through one ear. Even though they're getting sounds transferred from their dead, unusable side over to the usable side, they're still at an auditory disadvantage. There's no reason why you can't experiment with giving a little bit of mild gain in the mid to high frequencies to see if the patient likes that extra audibility to get some sense of sound coming in that ear and a sense of improved communication effectiveness by giving a little bit of mild high frequency gain. I refer to this as a mild BiCROS fitting, because the patient might want that little bit of extra audibility up there in the high frequencies.
Case #3
Figure 12 shows the audiogram of a patient for whom some clinicians might immediately think BiCROS. They may see those thresholds and think that they could put a hearing aid on there, but with that 8% word recognition, they may consider that to be an unusable ear. In fact, this patient wore a hearing aid on that right ear. I fit this patient with a hearing aid on the right ear and she did fine. It was a bit tricky to obtain the right mixture of the hearing aid on the poor ear with normal hearing on the right ear, but we were able to find that balance and ended up not having to give as much gain on the right ear as the thresholds originally indicated. This patient was a very successful hearing aid user because she had high demands on her hearing.
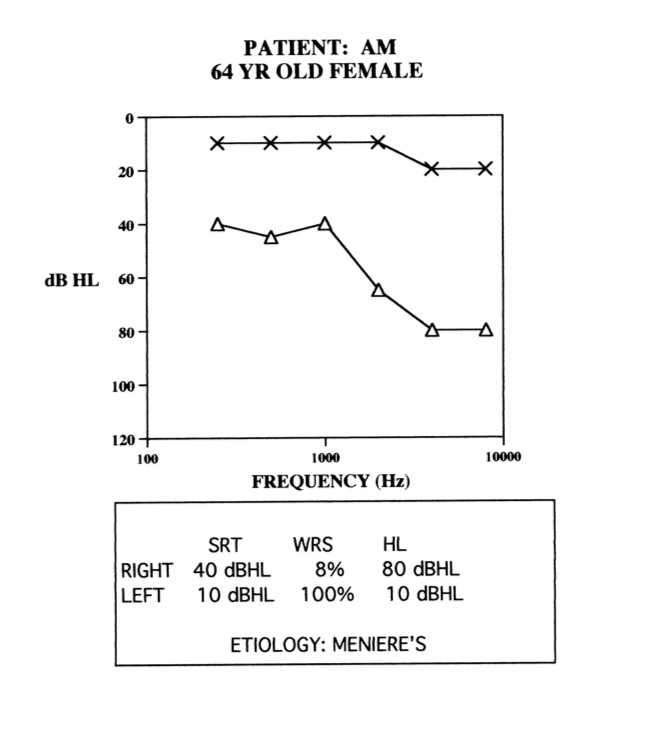
Figure 12. Case #3.
Case #4
Figure 13 shows another case of asymmetry. This 72-year-old female's hearing had been getting worse over the last several years, but she had not tried hearing aids yet. Even though the thresholds in her right ear were within the range of a RITE product, the etiology was unknown and was a little bit unstable. One of the things you might be concerned about is that if you fit a RITE product and those thresholds drop any further, now the hearing aid might be underfit for the patient and underpowered for the patient. You might consider going to the Super Power product simply to protect against any further drops in the thresholds. That is totally dependent on what you think the etiology is and what you think the future for that patient is going to be.
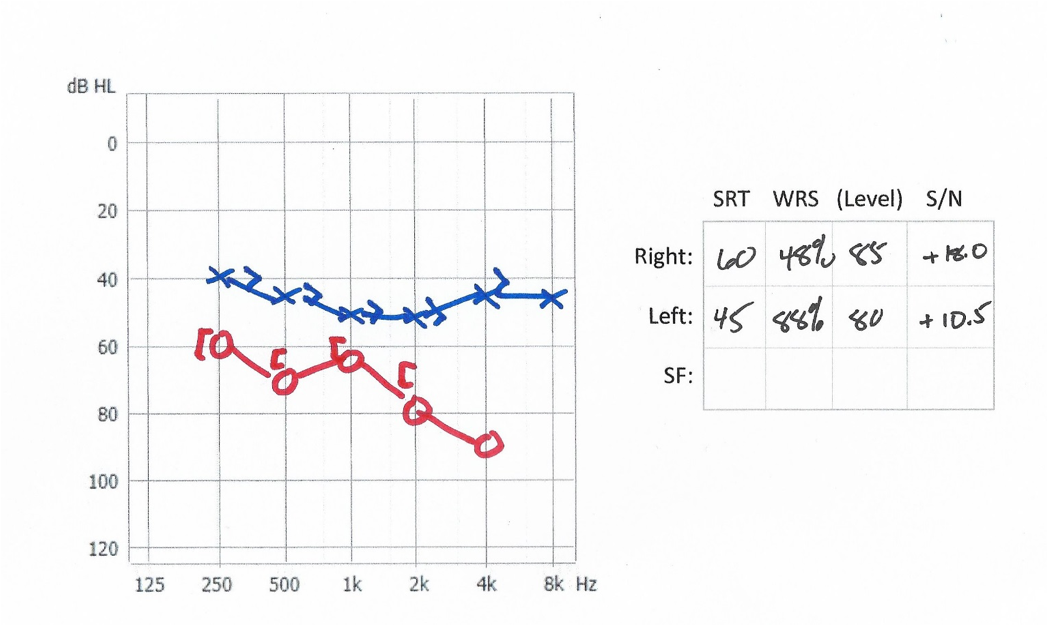
Figure 13. Case #4.
Case #5
Figure 14 is an example of another patient with significant asymmetry, but even in the better ear, the word recognition in quiet was poor, especially given those thresholds. Again, this is another patient who was successfully fit bilaterally with hearing aids. I used the approach of fitting the better ear first and then the poorer ear second. Her thresholds were relatively stable, and so I was okay with fitting a regular-type of product on the right ear. I went to a more powerful product for the left side, because I was a little concerned about the thresholds. Fortunately for that patient, the thresholds didn't move anymore from that point, at least in the time that I was managing her. This is another case where two hearing aids worked out fine. Definitely not a BiCROS sort of situation at all.
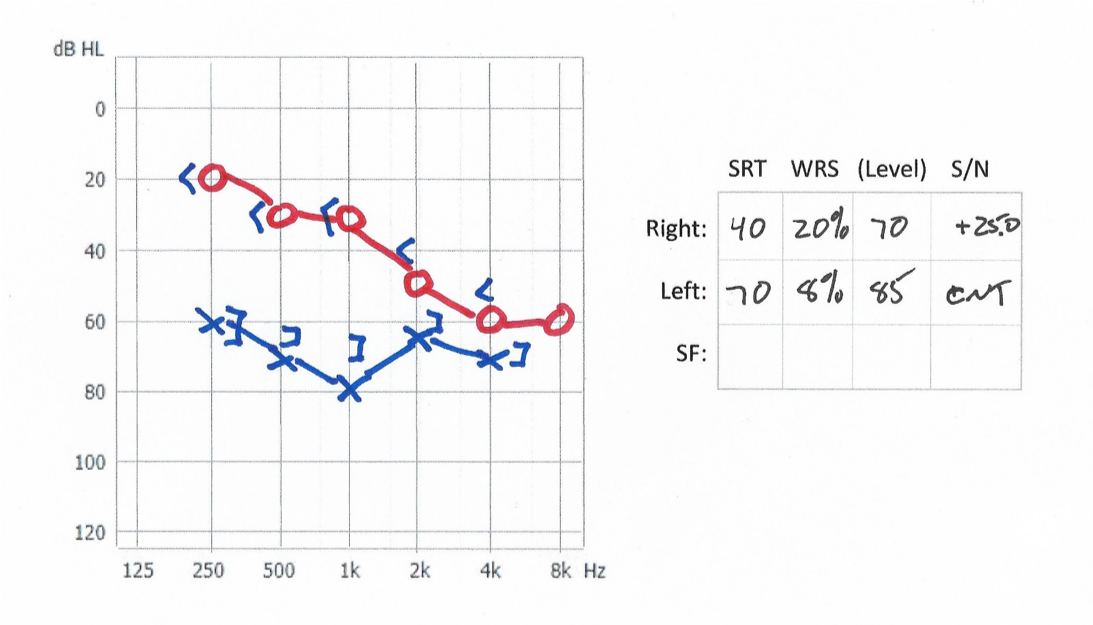
Figure 14. Case #5.
Case #6
Finally, the last patient could be considered a classic Ultra Power product patient (Figure 15). For this patient, there's not a lot you can expect out above 1 kHz. There is a little recovery in thresholds in the very high frequencies for that ear, but I was a bit concerned about that. The word recognition scores are pretty low given that she had hearing up past 1 kHz, but not a lot. This is a patient who ended up wearing an Ultra Power style product, just because that was probably all she had left in her auditory system. There wasn't a whole lot we could get out of this patient's auditory system.
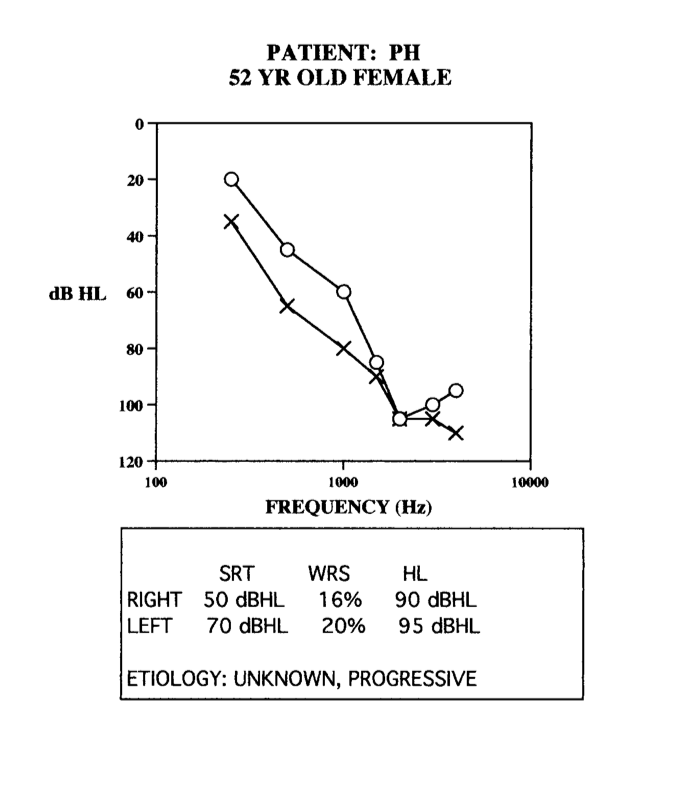
Figure 15. Case #6.
Most of these patients that I've shown you were potential candidates for implants. However, at the time period that I was involved with these patients, implants were not an option.
Summary and Conclusion
My hope is that by walking through these case examples and in talking about these hearing losses and the needs of these patients, you will leave today with a few extra ideas that you haven't had before. If you want to know more about the details of our Power product line, our Super Power and Ultra Power product lines, we offer companion courses on AudiologyOnline that provide more information about these releases. You could also talk to any one of the personnel at Oticon Live to get a better idea of what these products are about. Patients with this amount of hearing loss can be very satisfying to work with if you can get a good fitting. These are exactly the sort of patients who are dependent on well-trained, well-informed, creative-thinking hearing care professionals who can make the most of their remaining capabilities. As always if you have any questions or comments, you can contact me via email: [email protected]. Thank you for your time.
References
Feldman, A. S., & Oviatt, D. L. (1993). BiCros or binaural: A case study. Seminars in Hearing, 14, 3, 229-233.
Lamore, P. J., Verweij, C., & Brocaar, M. P. (1990). Residual hearing capacity of severely hearing-impaired subjects. Acta oto-laryngologica. Supplementum, 469, 7-15.
Souza, P., & Rosen, S. (2009). Effects of envelope bandwidth on the intelligibility of sine-and noise-vocoded speech. The Journal of the Acoustical Society of America, 126(2), 792-805.
Citation
Schum, D. (2019). Managing severe hearing loss. AudiologyOnline, Article 25800. Retrieved from https://www.audiologyonline.com


