This text course is an edited transcript of a Siemens Expert Series webinar on AudiologyOnline. Download supplemental course material.
Learning Objectives
- After this course learners will be able to describe the process of using published research to advance clinical practice.
- After this course learners will be able to list three recent research findings that can impact how hearing aid technology is selected for given patients.
- After this course learners will be able to list three recent research findings that impact how hearing aids are selected and fitted.
Introduction
Dr. Mueller: Many hearing aid related articles in the audiology literature contain findings with direct clinical applications. However, keeping up with all of them is no easy task. Last year, there were nearly 200 articles published on hearing aids. Even if you were to find the time to at least glance at these articles, the take-home clinical point may not be obvious. Sometimes, what might be interesting to a clinician may not have been the main focus of the article itself.
Today, I will try to help you out a little by sharing nuggets of what I have gleaned from some of these articles. My review will be brief, but you’ll have the references so you can go back and read the details on your own.
I have divided the articles into four components of fitting hearing aids: pre-fitting considerations, selection of technology, verification of the fitting, and post-fitting follow-up and counseling.
For the past 12 years, Catherine Palmer, Bob Turner, and I have done something similar to what I am presenting today at the American Academy of Audiology (AAA). Some of the articles that I am presenting today were taken the talks that we did within the past two years. They therefore helped contribute to this talk—thanks Catherine and Bob. Also, the students in Dr. Palmer’s lab at University of Pittsburgh have been helpful in tracking down and compiling many of these articles.
Pre-Fitting Considerations
In this category, we’ll talk about tests and procedures that you might consider prior to the actual fitting of instruments. For starters, have you had a patient who was a great candidate for two hearing aids, but said, “Can’t I get by with just one?” When this happens, it leaves you with three options.
First, you can amp up your counseling and become more assertive in trying to convince the patient of the benefits of two hearing aids. Another option would be for you to fit them with one hearing aid initially, and after a period of acclimatization, come back in a few weeks to be fit with the second one. Or, you could say that it is their choice to wear one or two hearing aids, and they can return if they change their mind. Does it matter how you approach this?
Article 1: Better Together: Reduced Compliance after Sequential vs. Simultaneous Bilateral Hearing Aid Fitting (Lavie, Banai, Attais, & Karni, 2013)
In truth, it does matter how you approach this scenario. In this article (Lavie, Banai, Attais, & Karni, 2013), the researchers wanted to know if it made a difference in the long-term if you fit a person on day one with bilateral hearing aids or if you fit them sequentially by letting them get used to one and fitting the second one a month later.
Methods. They had 36 subjects with a mean age of 76. Participants had bilateral, symmetrical hearing losses of similar degree, although hearing loss will not be a factor here. All participants were new hearing aid users. They were randomly selected to go in one group or the other.
Twelve were fitted simultaneously, and 24 were fitted sequentially. I am not sure why the groups had unequal numbers of participants. The sequential group used one hearing aid for a month and then was fitted with the second. They returned to the clinic every 10 days for an interview. At that time, the researchers conducted a “compliance” score. They also collected data logging of the hearing aids. The compliance score was based on four different factors, which were use of the hearing aids, the patient’s report of whether they had good hearing or not, the patient’s report if they were comfortable with the hearing aids, and the patient’s report of satisfaction.
Results. After the first month, compliance for both groups was very similar. About 75% had high compliance by their definition. In the second month, there was no change for the simultaneous group. Their compliance scores stayed the same. The sequential group was different, however. Recall that this was the group that had gone a month with one hearing aid and then the next month were fitted bilaterally. Seventeen of the 24 had reduced compliance in the second month. In other words, they were less happy, and only 25% had high compliance. The compliance score went from 75% to 25%, presumably simply because they were fitted with a second hearing aid.
Regarding hearing aid use, the simultaneous group showed the same results for data logging during both months. They used their hearing aids for an average of five hours a day. The sequential group, however, reduced the use for the ear originally fitted by about an hour a day, from 7.6 hours to 6.4 hours, and the second aid was significantly lower than that at only 4.5 hours a day.
The authors speculated on why this happened. They mentioned that several of the participants were disappointed when they got the second hearing aid. Perhaps they had the notion that if one is good, two will be doubly good. The authors speculated that the sequential group may have had auditory deprivation because they were fitted with only one hearing aid for a month, although I personally feel that is unlikely to happen in only one month of hearing aid use.
I did a study 25 years ago, where we told one group of patients that two hearing aids were best, and we told the other group of patients that they could decide for themselves. The people who were the happiest—benefit and satisfaction—after six months of hearing aid use were the people we told that two hearing aids were the best. I bring this up because perhaps it relates to the findings from this current study. Maybe the people who were fitted with two to begin with assumed that the doctor fit them with two, so therefore, two must be good. The other group might have thought that the doctor was not sure what was good because they fit them with only one for one month.
It does not really matter why it happened. I think the clinical tip from this article would be that if a patient appears to be a reasonable candidate for using two hearing aids, we should fit them with two hearing aids on day one.
Article 2: Placebo effects in hearing-aid trials are reliable (Dawes, Hopkins, & Munro, 2013)
This article (Dawes, Hopkins, & Munro, 2013) has to do with the placebo effect relative to hearing aids.
Methods. The researchers conducted behavioral testing with participants fitted with two different identical pairs of hearing aids. The patients, however, did not know that the hearing aids were the same. They were told that one pair were “new” hearing aids. The testing included speech recognition, subjective ratings and ratings of overall preference. Right away, you might guess that telling them one pair was “new” might influence their preference, but would it have any effect on objective speech recognition measures?
Results. Even though these were identical hearing aids, mean performance for speech recognition was 4% higher for the “new” hearing aids, and 75% of the people showed better performance with these “new” hearing aids. Subjective ratings were made on a 10-point scale for both sets of hearing aids, and the “new” hearing aids were significantly higher than the control. The best part, is that when they asked if they were to be fitted with either of these pairs of hearing aids, 75% of the participants picked the “new” hearing aids and 25% said there was no difference. No one preferred the control hearing aids, even though they were all the same hearing aids.
I took those last data and graphed them on a bar chart, shown in Figure 1. What if you got a White Paper from your favorite manufacturer comparing their new model to last year’s model? You might see data that looked a lot like this. It is certainly possible that the participants in that study may not have been blinded, or maybe even were told that one pair of hearing aids were the new model.
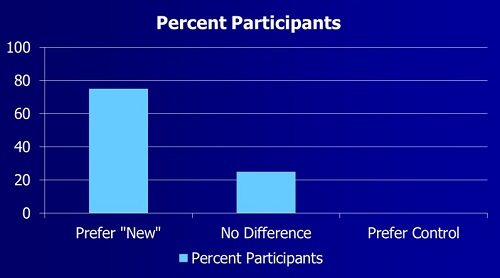
Figure 1. Preference data from placebo study.
Any type of casual comparison you might make in your clinic will be affected by a placebo effect. If you want an honest answer from your patient, be careful of the this effect. Furthermore, when reading about comparative clinical testing of products or features, especially in non-peer-reviewed articles, question if the placebo effect could have been a factor.
Selection of Technology
Directional microphones have been around for over 40 years. Figure 2 is a polar plot of a directional-microphone hearing aid on the right and the left ears of the KEMAR mannequin. You can see the commonly observed type of polar plot where sounds from the back are not amplified to the degree as sounds from the front.
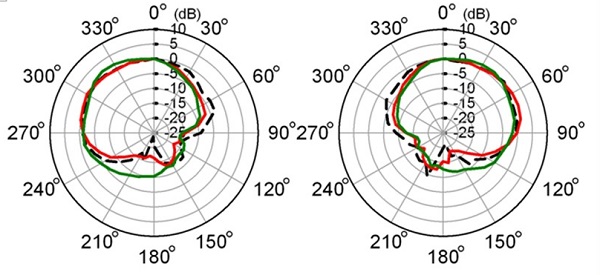
Figure 2. Traditional polar plot of directional microphones from the left and right ear of hearing aids on the KEMAR.
What has been available for the last three or four years, however, is the type of polar pattern seen in Figure 3, which is essentially the opposite. The hearing aid can detect speech from the back. When it detects that, and noise is also present, it flips the polar pattern and attenuates sound from the front and focuses on sounds from the back. In a perfect world, this operates automatically.
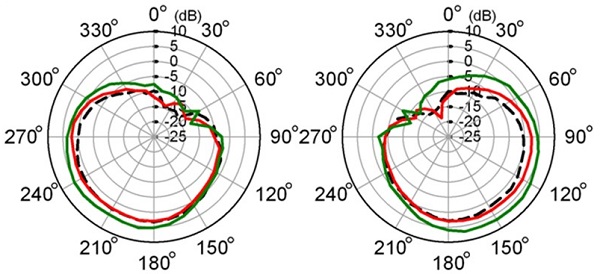
Figure 3. Polar plot of anti-cardioid directional processing. Data obtained with hearing aids fitted on the left and right ears of the KEMAR.
Article 3: Clinical Evaluation of a New Hearing Aid Anti-Cardioid Directivity Pattern (Mueller, Weber, & Bellanova, 2011)
Methods. In this efficacy study, we presented the Hearing in Noise Test (HINT) sentences from behind the user at 180 degrees. The traditional HINT noise was presented at 0 degrees, and we compared omnidirectional to traditional directional to this new anti-cardioid pattern. The study was then replicated at the University of Iowa.
Results. Notice that at both sites, we found a 10-dB benefit for this anti-cardioid pattern compared to the traditional directional mode. For omnidirectional, there was about a 5-dB benefit. These were very impressive findings. However, this testing was conducted in a test booth and we now that hearing aid processing often is not as impressive in the real world.
To be fair, it seemed to me that we needed to add some reverberation to make this more like the real world. Dr. Wu from the University of Iowa had an even better idea. He decided to test these hearing aids in a real vehicle while driving on Iowa Interstate-80.
Article 4: The Effect of Hearing Aid Technologies on Listening in an Automobile (Wu, Stangl, Bentler, & Stanziola, 2013)
Methods. Dr. Wu traveled a 30-mile stretch along I-80 while making the measures. KEMAR was in the passenger side seat of the van. There were loudspeakers that presented speech from both behind and from the side of the KEMAR. A recording engineer was in the back of the van. This was a real-world study, in a real van, on a real highway. The background noise was the actual road noise. It was designed to replicate the situations of the driver or someone from the back seat was talking. As you might guess, it would be difficult to test real people cruising along in a van, but you can record this and play it back to hearing-impaired subjects to obtain essentially the same result as if that person was sitting in the van.
Results. The authors tested three different hearing aids using the different setting of each. If we look at hearing aid A, we see that in the omnidirectional mode, the scores were around 60%. As you might expect, traditional directional was significantly worse. This is important, as some hearing aids will default to directional in that setting if you have it on “automatic.” In general for the new anti-cardioid algorithm, there was an improvement of around 15%. That is not fantastic, but it tells you two things. First, it was a significant improvement, and it showed that the signal classification system was working. These hearing aids were all set on automatic, which means that the signal classification system of the hearing aid identified the speech from the back, and correctly switched the polar pattern..
The clinical tip is that this signal classification system seems to provide benefit in a real-world situation. To me, this was a nicely designed out-of-laboratory study that had an encouraging outcome.
Article 5: 20Q: Hearing Aid Provision and the Challenge of Change (Cox, 2014)
Have you ever wondered if personal sound amplification products (PSAPs) really work? These are hearing aids that you can buy in various big-box stores such as Best Buy. They typically cost between $300 and $400, or you can order them through the Sunday newspaper. Are hearing aids better than PSAPs? We hope so. Secondly, are premier hearing aids better than entry-level hearing aids? They cost more, so they should be better, right?
Today I want to pull out one area of Robyn’s excellent article (2014), where she reports findings that compared PSAPs to entry-level to premium hearing aids.
Methods. Testing was conducted with two different PSAPs and two different types of hearing aids from two different manufacturers, for a total of six devices. Each of the devices was programmed to NAL-NL2 targets, because of course, if there were gain differences, this easily could influence the overall findings. The products were tested using three different everyday sounds: speech, noise, and music. These signals were recorded through each hearing aid device while fitted on the KEMAR, and then played back to the hearing-impaired subjects.
There were 20 adult listeners who had mild to moderate hearing loss, and they listened to the sound, music, and noise samples. The comparisons were conducted using a double round-robin, paired comparison. It was like a tournament where a PSAP competes against a premier hearing aid and the subject had to pick which one is best. Then the PSAP may compete against the entry-level hearing aid, and so on.
Results. Remember that there were three different categories of hearing aids and two hearing aids for each category. Figure 4 shows these results.
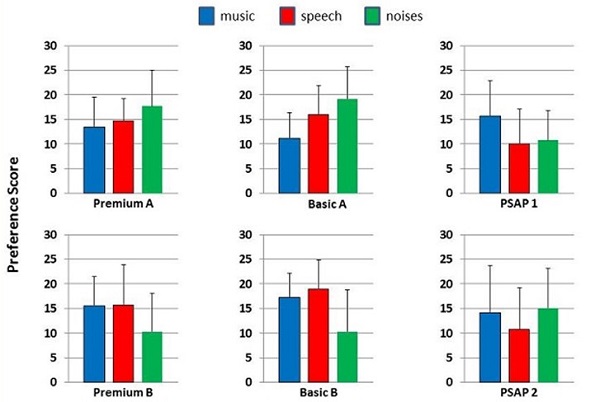
Figure 4. Results of testing PSAPs to premium and entry-level hearing aids in the conditions of music, speech and noise.
You see premium A, basic A, and PSAP 1 on the top, and premium B, basic B, and PSAP 2 on the bottom. These are shown for music, speech and noise conditions. The first thing to come to mind is no finding is overwhelmingly high or low. To make this easier to view, I combined the two premium hearing aids, the two basic hearing aids and the two PSAPs, and these average findings are shown in Figure 5.
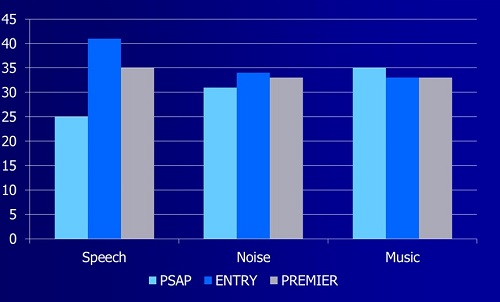
Figure 5. Average preference ratings for each set of instruments for each condition.
Overall, they found no significant differences among any of the three products for music and noise. For speech, both hearing aids were better than the PSAPs, but there was no difference between the entry-level and the premium-level hearing aids for listening to speech. This is measured in percent of wins, meaning when they were in competition, the percent of time the they won. Notice that the PSAPs, even for speech, won 25% of the time (Figure 5). This is just a small piece of a large study that Dr. Cox has been doing the past few years—I suspect there will be several more publications in the near future.
Note: Since the time of this presentation, the following article on this topic has been published: Cox, R.M., Johnson, J.A., & Xu, J. (2014). Impact of advanced hearing aid technology on speech understanding for older listeners with mild to moderate, adult-onset, sensorineural hearing loss. Gerontology, 60(6), 557-68.
The differences among PSAPs, entry-level, and premium hearing aids may not be as large as some people believe. There are two caveats to this. One is that that they were all fitted to NAL-NL2 targets. You could not compare this to someone who walked into a store, bought a PSAP off the shelf and put it into his or her ear. The second is that these were measures in the laboratory. To define modern hearing aids, and particularly premium hearing aids, you might argue that there are a many features that would not show up in that particular test. Obviously, some of the entry-level hearing aids or PSAPs are not going to have the same signal detection, automatic and adaptive processing as the premier models. But, does everyone need this?
Article 6: Siemens Expert Series: Implementing a Gain Learning Feature (Palmer, 2012)
Catherine Palmer did a presentation for AudiologyOnline which had to do with the third generation of trainable hearing aids. These are essentially the generation of trainable hearing aids that you are fitting today; signal classification allowing for compression training for several different listening categories. One of her research questions was, “Does it matter when you start the training?”
Methods. She had two groups of new hearing aid users. In one group, training was off and then turned on at the second visit. In the second group, training was on from the beginning. She fit them all to NAL targets. They all used the hearing aid for two months, but one group used the NAL for a month without training, and the other group started training from day one.
Results. For the control group who started training after a month of hearing aid use, the speech intelligibility index (SII) for soft speech was reduced 2%, and the group who trained for two months had an SII reduction for soft speech at 4%. It is hard to know if this reduction was slightly greater for the second group because they had two months to train rather then one, or if the other group got used to the NAL fitting after being fitted to this algorithm for a month. Real-world loudness judgments did not change during training, and there was no difference between groups.
Speech recognition is a concern for some clinicians who consider using trainable hearing aids. What if the patients train their hearing aids to a point where speech recognition is reduced? Dr. Palmer measured both groups for performance before training and after training. The first question you might ask is, “Were the groups themselves equal?” The data found the groups to be equal. Secondly, “Did training have an impact on speech recognition?” This was measured with the HINT. For the experimental group, pre and post scores were essentially the same, and for the control group, pre and post scores were essentially the same. Speech recognition did not go up, and it did not go down.
And the end of the two month period, the participants were able to compare the two programs (NAL vs. trained), and then determine a preference. They were blinded as to what program they were using and were asked which program they would prefer for continued use. The summary of those results is shown in Figure 6.
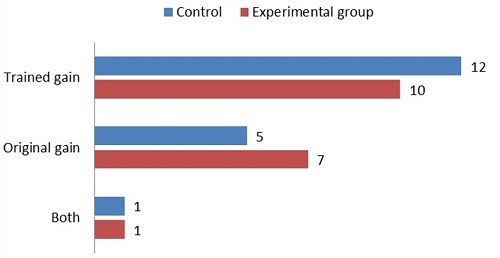
Figure 6. Participant preferences for trained gain versus original programmed gain.
One person out of 36 would not make a decision, but the majority wanted to use the trained gain. Although, according the laboratory measures, they were not doing any better with speech understanding, two-thirds of them preferred the trained gain.
Article 7: Real-Life Efficacy and Reliability of Training a Hearing Aid (Keidser & Alamudi, 2013)
A somewhat similar study was conducted at the National Acoustic Laboratories (NAL). Most trainable aids now train compression as well as overall gain. That is, independent training is conducted for soft, average and loud inputs. In the product used for this study, the hearing aid also trains independently in six different sound classifications or environments.
Methods. In this study, the participants were all programmed to NAL-NL2. After the person trained for three weeks, the devices were reset to prescription, and 19 of the participants repeated the training. They looked to see if this training was reliable. Also, the participants made diary ratings for satisfaction during the study.
Results. Many different sets of data were obrtained in this study, of which I pulled one that is interesting for clinicians. They looked at high-frequency gain training and gain variation. There was not much deviation across the six sound classes. The average person was within 1 to 2 dB of NAL-NL2 targets following training. Music was the greatest deviation, but the average departure from target was still only about 2.5 dB. Few people trained above NAL target. From this study, it seems that people prefer to be just a little below the NAL target, but only by 1 to 2 dB.
Of the participants in their study, however, approximately half did not do a lot of training. It is hard to know if this simply was because the person was happy with the settings as-is so they do not train the hearing aid, or if they simply did not want to participate in the training process. For those who did make sufficient changes, training was effective for about 75% to 80%, and it resulted in higher satisfaction.
The clinical tip is that not everyone is a good candidate for trainable hearing aids, but for those who are, training seems to improve overall satisfaction and does not seem to have any downsides. Another peripheral finding was that the NAL-NL2 seems to be a pretty good starting point for adults. On average, people did not deviate very far from this prescriptive fitting.
Article 8: Effects of Noise and Working Memory Capacity on Memory Processing of Speech for Hearing Aid Users (Ng, Rudner, Lunner, Pedersen, & Ronnberg, 2013).
There is much discussion about working memory in the literature as of late. Working memory is similar to what we think about as short-term memory. It operates in just over a few seconds and is like a temporary storage.
This article (Ng, Rudner, Lunner, Pedersen, & Ronnberg, 2013) evaluated the relationship between noise reduction and an individual’s working memory.
Methods. The researchers used a word recognition task and asked the participants to identify and also later recall the last word in a sentence in two different noise backgrounds. It was conducted with noise reduction on, with noise reduction off, and in quiet.
Working memory was measured using a reading span test. The individual was seated in front of a computer screen, where sentences would appear. The person has to say whether the sentence is real or not real. At some point, the person would have to tell the examiner what the first or last word was of each of the last six sentences. While you are trying to determine the sentence is real or not, you also have to save in short-term memory the first and last word of the sentence, as you do not know which you will have to later recall.
Results. As we would expect, noise impaired the recall performance. Interestingly, however, the negative effects from the noise were cancelled by noise reduction for people with high-working-memory capabilities. In other words, their first they got worse with noise, and then performance returned to baseline when noise reduction was activated. In short, the noise reduction feature may be impacted by your patient’s working memory.
I am sure you have had patients where it seems like the noise reduction feature does not seem as beneficial; this could be related to the patient’s working memory, especially if patients do benefit from it. If you are a typical clinician, you do not measure working memory, but you can guess after spending time with these patients that it is often related to their overall cognition.
Keep in mind that experimenters who are doing this research test people for their working memory. If they have poor working memory, they are not included in the protocol. What you then see when you read an article is a study with people who have good working memory. Now, take that technology and fit it in your clinic. The average person may not have a good working memory, and you will not see the same benefit that was demonstrated in the article. To this end, verification is critical.
Verification of the Fitting
Article 9: The Importance of Audibility in Successful Amplification of Hearing Loss (Leavitt & Flexer, 2012)
Methods. In this article (Leavitt & Flexer, 2012), the researchers selected the premier product from the Big Six companies with all the special features activated. They added a seventh pair of hearing aids, which was a 2002 single-channel, analog instrument programmed to NAL-NL1. The subjects were all experienced bilateral hearing aid users. Each participant was given the QuickSIN, which measures signal-to-noise ratio (SNR) loss. As a reminder, the lower the number, the better the score. Participants were tested twice with the premier hearing aids, first with the manufacturers’ proprietary fitting, and then again with the hearing aids programmed to the NAL-NL1 algorithm.
Results. The old pair of single-channel hearing aids yielded an SNR loss of about -8 dB when fitted to NAL-NL1 only. All the new premier hearing aids were worse than this for the initial testing. The patients’ performance in background noise for the manufacturers’ proprietary fitting in hearing aids 3, 4, and 5 was more than 8 dB worse with the premier hearing aid than with the old pair of hearing aids. The same hearing aids programmed correctly to NAL showed in most cases, an improvement of SNR loss by about 10 dB. A summary is shown in Figure 7.
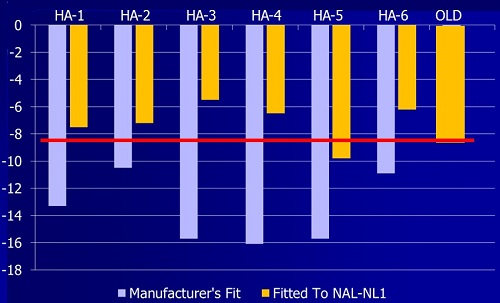
Figure 7. Performance for the aided QuickSIN presented in soundfield at 57 dB SPL. Bars indicate SNR loss. The average SNR disadvantage as compared to individuals with normal hearing. (Adapted from Leavitt & Flexer, 2012).
This clearly shows that it is not the technology, but the person doing the programming, that can make or break a hearing aid fitting. If you are not programming new hearing aids correctly to prescriptive targets, they can perform substantially worse than 10-year-old, single-channel, analog hearing aids.
Article 10: The Accuracy of Matching Target Insertion Gains with Open-Fit Hearing Aids, (Aazh, Moore, & Prasher, 2012)
In a related article, that tells the same story, Aazh, Moore, & Prasher, 2012, conducted probe-mic testing to determine if using the labeled prescriptive target (NAL-NL1) within the manufacturers’ software achieved these targets in real-ear verification.
Methods. Testing was conducted on 51 ears, all with open-fit hearing aids, usinig NAL-NL1 presets in the fitting software. Following the initial measures, adjustment were made to improve the fitting.
Results. Seventy-one percent of the fittings had greater than a 10 dB mismatch from target when the hearing aids were tested in the ear. After making some manual adjustments, 82% met target, with the majority being met through at least 2000 Hz. Eighteen percent still did not meet target, and I suspect that was probably precipitous losses where targets often cannot be met at 4000 Hz or beyond due to feedback issues, or gain limitations of the instrument.
You might argue that this study was published few years ago, is only using data from one manufacturer, and the patients all had been fitted with open earmolds. Would this still be true today?
Article 11: 20Q: Real-Ear Probe-Microphone Measures – 30 Years of Progress (Mueller, 2014)
Methods. In this article, I presented data collected just a few months ago at the University of Iowa by Dr. Elizabeth Stangl. She used premier hearing aids for each of the Big Six manufacturers. The hearing aids were fitted to NAL-NL2 for a downward-sloping hearing loss that was no worse than 65 dB at 4000 Hz. The manufactuers softare fiting was not altered, and all instruments were assess using speechmapping (male speaker of Audioscan Verifit). To give you a snapshot of the findings, I will discuss the three worst hearing aids from these data, although none of the six met targets.
Results. The results are shown in Figure 8. Observe that for manufacturer A, the fitting started to fall below target around 1500 Hz. Manufacturer B fell about 10 dB below target across all frequencies. Manufacturer C missed targets by about 16 dB in the high frequencies. Would that impact a speech understanding? Most definitely.
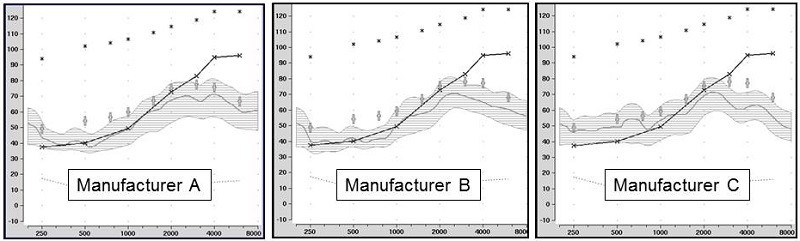
Figure 8. Shown are the speechmapping findings for the premier hearing aid of three major manufacturers, programmed using the manufacturer’s NAL-NL2 option in the fitting software. The test stimulus was the male talker of the Verifit system, presented at 55 dB SPL. Also shown are the sample patient’s audiogram (upward sloping solid line) and the NAL-NL2 targets for this speech input (frequency-specific crosses). Chart courtesy of Elizabeth Stangl, AuD.
As shown in these examples, it is very risky to use the manufacturers’ fitting algorithm without doing any real-ear verification. Unfortunately, that happens every day. Check out this paper by Sanders, Stoody, Weber & Mueller (2015), which shows that things haven’t gotten any better. These authors show the poor match to target for the five leading manufacturers.
I have suggested in these last two articles that fitting to prescriptive target is a good thing; but is there research evidence to support this?
Article 12: Initial-Fit Approach Versus Verified Prescription: Comparing Self-Perceived Hearing Aid Benefit (Abrams, Chisolm, McManus, & McArdle, 2012)
Methods. Harvey Abrams and colleagues (2012) looked at experienced hearing aid users using a crossover design where half were fitted by the manufacturer’s first fit and half were fitted with NAL-NL1. Participants used the hearing aids for four to six weeks, and then they crossed over to the other prescriptive condition.
Results. They used the Abbreviated Profile of Hearing Aid Benefit (APHAB) self assessment scale to compare the two conditions. For the subscales ease of communication, reverberation, and background noise, the APHAB scores between the two prescriptions were statistically significant. Overall, they found that APHAB scores were significantly better for people fitted to the NAL. At the end of the study, people were asked what they preferred, and 15 of the 22 participants preferred the verified NAL fitting. The clinic tip here is that fitting to target does matter. The only way to know if targets have been met is by real-ear microphone measures, which was illustrated previously.
Post-Fitting Follow-Up and Counseling
Article 13: The effects of hearing aid use on listening effort and mental fatigue associated with sustained speech processing demands (Hornsby, 2013)
In this research, Dr. Hornsby (2013) was examining hearing aid use, to determine if it had an impact on listening effort and auditory mental fatigue.
Methods. He included 16 adults with mild to severe sloping hearing loss with a dual-task paradigm comparing word recognition, word recall, and visual reaction time to the material that was being tested. These individuals were fitted with hearing aids, which they used in the real world for two weeks prior to each test condition. They gave subjective ratings of listening effort during the day. Part of this was to see if real-world listening effort correlated to what was being measured in the laboratory. They also gave ratings of fatigue and attentiveness before and after the task to see if results would differ for the individuals.
Results. Hearing loss and age were not predictive of the results. Interestingly, the objective measures of listening effort and fatigue and the patient’s ratings were not correlated. Word recognition and recall were resistant to mental fatigue. Word recall was better and reaction times were faster when the subjects were aided compared to unaided.
Sometimes we forget about the subtle benefits of hearing aid use, such as improved dual-tasking. If we could make life a little more relaxed, indirectly, we will likely see better word recognition.
Article 14: The Just Noticeable Difference in Speech-To-Noise Ratio (McShefferty, Whitmer, & Akeroyd, 2015)
How much SNR increase can a patient detect? The authors looked at “meaningful” in two different ways. One related to what could be noticed as a difference clinically.
In the clinic, what was the just noticeable difference (JND) for an SNR change? Casually, people have suggested 2 dB over the years. McShefferty, Whitmer, & Akeroyd (2015) found that 3 dB was the JND for the average person.
A second questions was: what SNR becomes meaningful where participants would be willing to make a change? They asked the participants if they would be willing to see an audiologist for a given increase in SNR. They also asked if the participants would be willing to swap devices for this increase in SNR. This was not asking if they could detect the difference, but if they would be willing to do anything different. Would this improvement be meaningful enough to change something, such as buy a new pair of hearing aids? While this was not their specific question, it is a real-world question you might ask.
Results. It took a 6 dB difference before people would make a change. If your patient is a previous user, it is unlikely that the new hearing aids would provide even a 3 dB advantage to what they were wearing previously. If there is a new product that is 1 dB or 2 dB better, that might be statistically significant in some laboratory studies, however, it seems that we may need 3 dB before our patients will be motivated.
We will see a 6 dB advantage only with a remote microphone. Take that into your counseling. This helps explain why when a directional hearing aid is only 2 dB better than the previous model, patients do not hear any difference.
Conclusion
While there is a multitude of research, I hope these articles will provide clinical applicability for your hearing aid fittings. I encourage you to go back and read the articles, as they will enrich your clinical practice and knowledge.
Questions and Answers
As we present around the country, we are often asked about research regarding frequency-lowering techniques and algorithms. I am guessing that you might be able to lead us to some good frequency-lowering articles.
I would keep my eye on a lot of the work that is being done with children. There was a large multi-center project conducted by the University of North Carolina, the Boystown group, and University of Iowa, and those publications are starting to come out. I encourage you to search Ryan McCreery, and you will find some good work in the last few years. That is all using frequency lowering with children.
As far as adults are concerned, I do not recall anything of real significance in the last year or so. We did some review articles here at AudiologyOnline on frequency lowering recently. In the clinic, one of the problems with frequency lowering is that it is often fitted poorly, and the lowered signal is not made audible. Basically, what people have done is take a signal that was inaudible at 6000 Hz and they lowered it, and made it inaudible at 3000 Hz. To the patient, inaudible is inaudible, and frequency lowering has no impact.
One of the publications from last year by Ryan McCreery’s group pointed that out that, in many of these cases, we did not know if it worked because of how it was fitted. You would assume in a research study that would be taken care of. However, in practical use, that has been a big limitation as to whether or not frequency lowering works.
References
Aazh, H., Moore, B., Prasher, D. (2012). The accuracy of matching target insertion gains with open-fit hearing aids. American Journal of Audiology, 21(2), 175-180. doi: 10.1044/1059-0889(2012/11-0008).
Abrams, H. B., Chisolm, T. H., McManus, M., & McArdle, R. (2012). Initial-fit approach versus verified prescription: comparing self-perceived hearing aid benefit. Journal of the American Academy of Audiology, 23(10), 768-778. doi: 10.3766/jaaa.23.10.3.
Cox, R. (2014, April). 20Q: Hearing aid provision and the challenge of change. AudiologyOnline, Article 12596. Retrieved from: https://www.audiologyonline.com
Dawes, P., Hopkins, R., & Munro, K. J. (2013). Placebo effects in hearing-aid trials are reliable. International Journal of Audiology, 52(7), 472-477. doi: 10.3109/14992027.2013.783718.
Hornsby, B. (2013). The effects of hearing aid use on listening effort and mental fatigue associated with sustained speech processing demands. Ear and Hearing, 34(5), 523-534. doi: 10.1097/AUD.0b013e31828003d8.
Keidser, G., & Alamudi, K. (2013). Real-life efficacy and reliability of training a hearing aid. Ear and Hearing, 34(5), 619-629. doi: 10.1097/AUD.0b013e31828d269a.
Lavie, L., Banai, K., Attais, J., Karni, A. (2013). Better together: Reduced compliance after sequential vs. simultaneous bilateral hearing aid fitting. American Journal of Audiology, 23(1), 93-98.
Leavitt, R. J., & Flexer, C. (2012). The importance of audibility in successful amplification of hearing loss. The Hearing Review. Retrieved from: https://www.hearingreview.com/2012/12/the-importance-of-audibility-in-successful-amplification-of-hearing-loss/
McShefferty, Whitmer, & Akeroyd. (2015). The just noticeable difference in speech-to-noise ratio. Trends in Hearing, in press.
Mueller, H.G. (2014, January). 20Q: Real-ear probe-microphone measures - 30 years of progress? AudiologyOnline, Article 12410. Retrieved from: https://www.audiologyonline.com
Mueller, H.G., Weber, J. & Bellanova, M. (2011). Clinical evaluation of a new hearing aid anti-cardioid directivity pattern. International Journal of Audiology, 50(4), 249-254.
Ng, E. H., Rudner, M., Lunner, T., Pedersen, M. S., & Ronnberg, J. (2013). Effects of noise and working memory capacity on memory processing of speech for hearing-aid users. International Journal of Audiology, 52(7), 433-441. doi: 10.3109/14992027.2013.776181.
Palmer, C. (2012, August). Siemens expert series: Implementing a gain learning feature. AudiologyOnline, Article 20951. Retrieved from: https://www.audiologyonline.com
Sanders, J., Stoody, T., Weber, J., & Mueller H.G. (2015). Manufacturers’ NAL-NL2 fittings fail real-ear verification. Hearing Review, 21(3),24.
Wu, Y. H., Stangl, E., Bentler, R. A., & Stanziola, R. W. (2013). The effect of hearing aid technologies on listening in an automobile. Journal of the American Academy of Audiology, 24(6), 474-485. doi: 10.3766/jaaa.24.6.4.
Cite this Content as:
Mueller, H.G. (2015, April). Siemens Expert Series: day-to-day hearing aid fittings - clinical nuggets from recent research. AudiologyOnline, Article 13768. Retrieved from https://www.audiologyonline.com.


