This course is an edited transcript of an AudiologyOnline live webinar. Download the course handout.
Learning Outcomes
- Participants will be able to identify the CPT code/ICD10 code combinations that require reporting of the audiology PQRS codes in 2016.
- Participants will be able to list the new CPT codes for 2016.
- Participants will be able to list the ICD 10 codes for 2016.
Dr. Kim Cavitt: Today’s course will cover changes related to CPT as well as to PQRS (Physician Quality Reporting System) for 2016. It is recommended that you download the course handout as a reference as it includes all the codes mentioned in this course as well as other codes, and links to regulations, guidance, and resources.
Coding Changes for 2016
There are no new HCPCS codes that pertain to audiology. HCPCS are the V or L codes that we use to bill for cochlear implants, osseointegrated hearing devices, or hearing aids. There are no new ICD-10 codes that went into effect on January 1, 2016. ICD-10 has an October 1 implementation date. This means you will see new ICD-10 codes on October 1, 2016.
There are two new CPT codes related to caloric testing and three new PQRS measures. The new caloric test codes concerned vestibular testing with recording - the new codes are 92537 and 92538. These codes both replace 92543, which was the old caloric test code. Code 92543 will be completely eliminated from the code set, effective January 1. The new code is 92537, caloric vestibular test with recording, bilateral, bithermal. This is the most common scenario people utilize when billing for caloric testing. You perform one warm and one cool irrigation for each ear for a total of four irrigations. This code will be one unit, as the code in and of itself takes into account the four irrigations. If you only perform three irrigations, then you would add the 52 modifier showing you reduced the service. If you perform more than four irrigations, for example with ice water testing, you would add the 22 modifier to show that you had an increased procedural service.
Code 92538 is the caloric vestibular test with recording, bilateral, monothermal. This means you have done either a cool in the right ear and a cool in the left, or a warm in the right and warm in the left only. It is not four irrigations. It is not bithermal or bilateral. It is two irrigations. If you only perform one irrigation, you would need to add the 52 modifier. These are the only CPT coding changes. These codes are billed as single units. You will not see multiple units as you did in the old caloric testing. You will have a unit of either one of these codes with or without a modifier.
It has been about 90 days since the ICD-10 launch and we have some information as to how claims are being processed and issues that you need to keep in mind. I want to stress that today, everything in healthcare relating to audiology is about looking at the whole patient and coordination of care. It is about practicing audiology back to its fullest extent. We need to think about the whole person when we are coding with ICD-10. You need to code what the patient, the family, and/or the physician report in the case history. Case histories should focus on the whole patient, not only on the auditory system. Some of the co-morbidities, such as diabetes, multiple sclerosis, and cardiovascular issues, can drive the necessity of the test. You need to code those comorbidities that support medical necessity. Cancer, vascular disorders, autoimmune diseases, diabetes, and MS are a few comorbidities.
You need to code what you, as the audiologist, measures, which is the hearing loss or the vestibular disorder. You need to code what you personally visualize such as a collapsing canal, an exostosis, or a cauliflower ear. Coding is not merely about reimbursement. You do not code for reimbursement. You code to represent what you learned from the case history, what you measured in the testing, and what you visualized in otoscopy. You do not need to overcomplicate it. There are more codes, and one reason for this is to denote right, left, and binaural. To be successful in ICD-10 coding, you need to document a comprehensive case history, test results, and a plan of care, especially if you are working in an organization where you are not doing the coding, but a certified coder is coding for you. You need to have strong documentation in order for them to best code the situation.
The Term "Unrestricted" in ICD-10
In ICD-10, "unrestricted" means normal. For example, if the code indicates a sensorineural hearing loss in the right ear and unrestricted hearing in the left, it means there is a hearing loss in the right ear and normal hearing in the left ear.
Medicare has something called a local coverage determination (LCD). A local coverage determination is where a Medicare contractor is trying to restrict coverage. For example, in order for the Medicare contractor to pay for X procedure, you must have one of Y diagnoses. If you have an LCD from your Medicare Area Contractor (MAC), it is important for you to be aware of those. The codes that you see in this course and in the handout that have an asterisk are included in an LCD. It may not be included in your LCD, but it is included in some LCDs. In 2016, you will see the use of some unspecified codes. It is risky to use unspecified codes when you are not billing Medicare. Many private payers have already determined that they are not going to pay for unspecified codes. However, when you are billing certain MACs, because of LCDs, unspecified is something that they might be looking for.
You can look up LCDs by state at this database. The following are the LCDs that exist today: Novitas has a LCD for vestibular and auditory testing; First Coast, which is Florida’s Medicare Contractor, has a LCD for tympanometry and vestibular testing; Palmetto and Meridian have a LCD about vestibular testing, but that LCD also includes 92557. You need to be aware of how these LCDs work and what diagnoses are contained in them.
Code Set
I am going to review the code set in some detail, and point out some specific examples of when and when not to use certain codes. Keep in mind that a 3 as the last digit in a code means bilateral, a 1 means right ear, and 2 means left ear.
Figure 1 includes the first group of codes I will discuss.
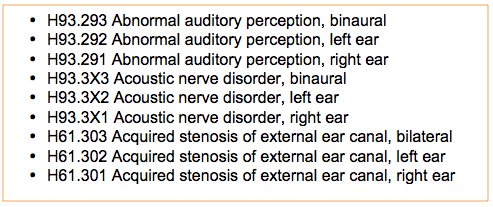
Figure 1. Code set.
Abnormal auditory perception is a great code to use in certain situations. I am a big advocate of hearing handicap inventories. You may have a patient who comes with communication difficulties or a hearing handicap, but they end up having normal hearing. To me, that is an abnormal auditory perception. That is a scenario where you do know what the perception is yet. You do not know if it is a central auditory problem, cognition or dementia. You are still looking into it. Abnormal auditory perception is a good code when you have nothing else, but the patient is illustrating difficulty. This is not about routine issues or someone who has no problems. This is about someone who is having communication difficulties, but they end up having normal hearing. Acoustic nerve disorder is another good coding option. Acquired stenosis of the external ear canal is a collapsing of the canal, as stenosis is a narrowing.
Let’s now look at the next code set in Figure 2.
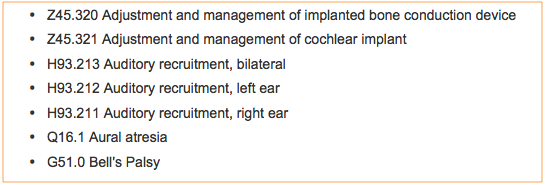
Figure 2. Second code set.
This is the first time we will see the Z codes. In ICD-9, these were V codes. They are now regularly in the code set. Sometimes Z codes can valuable for data collection in your practice. However, if they are the primary diagnosis, it can be problematic with reimbursement. I would avoid using a Z code as your primary diagnosis. Your primary should be the comorbidity, the hearing loss, tinnitus, or a vestibular disorder. Those are a stronger option to be primary.
You can put the code for either adjustment and management of an implanted bone conduction device, or adjustment and management of a cochlear implant on a claim, even a claim you are seeking coverage for, if the insurer pays for those codes. If the insurer deems them to be medically necessary, this should not drive a denial because they paid and recognized these two codes. When we get to the Z codes for a hearing aid, I would avoid putting them on claims that you are seeking coverage for.
Also in Figure 2 are the codes for auditory recruitment, aural atresia, and Bell’s palsy. Atresia does not have a right, left, and binaural attribute to it. The same goes for Bell’s palsy.
Refer to Figure 3.
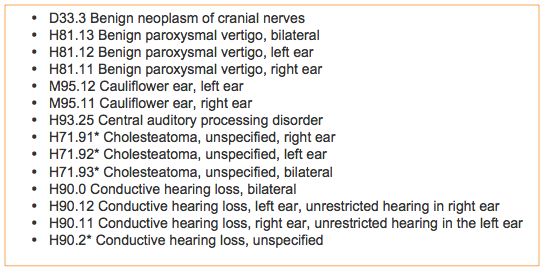
Figure 3. Code set.
The code set in Figure 3 includes is the code for benign neoplasm of the cranial nerves, which you would use for a vestibular schwannoma or acoustic neuroma. For the BPPV codes H81.13, H81.12, and H81.11, please note that they are included in a PRQS measure. After that is cauliflower ear, right and left, which does not have a binaural attribute. Central auditory processing disorder is in this set. Cholesteatoma unspecified is shown in this list with asterisks. Again, the asterisk means that there is a local coverage determination which has this code as an option when you are seeking coverage within that determination. Conductive hearing loss is listed next. Conductive hearing loss, unspecified, might be useful for Medicare. However, I would be careful of using anything unspecified with private insurers or many Medicaid programs.
The next set of codes I will discuss are listed in Figure 4.
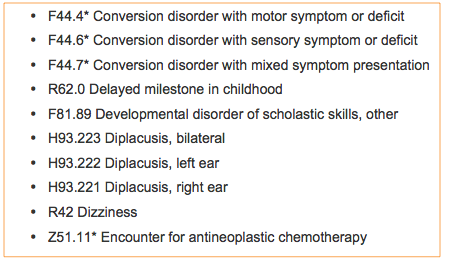
Figure 4. Code set.
Here are the codes for conversion disorder with motor symptom or deficit, conversion disorder with sensory symptom or deficit, conversion disorder with mixed symptom presentation. A conversion disorder is a psychological condition, like hysterical deafness. This code can be valuable when the patient is complaining of something, and you are trying to determine whether or not it exists.
Delayed milestone in childhood is an excellent code to use when you see a child with a normal audiogram, but they are not talking.
The code of developmental disorder of scholastic skills can be used in this scenario: a child is having trouble in the classroom, is diagnosed with a developmental disorder, and you want to see if there are any auditory conditions, but obtain a normal audiogram.
There are codes for diplacusis.
The catch-all dizziness has a code but is also in a PQRS measure for referral for acute or chronic dizziness. Dizziness is a diagnosis that you would use when someone is dizzy, unsteady, or imbalanced, but you have not assessed them yet. Everyone should realize that asking a patient about their balance or dizziness is one of the FDA warning signs of ear disease and should be asked before any hearing aid is fit. It is important to ask this balance or dizziness question, regardless of our clinical setting.
There is a code for encounter for antineoplastic chemotherapy. This is a great code to use when you see someone who does not have ototoxic hearing loss and has not had the chemotherapy yet, and you are trying to get an encounter to determine what their baseline is.
The codes listed in Figure 5 cover Eustachian tube disorders, other specified and unspecified. Other specified means you may know or think you know what it is, but there is not a code to either represent that or it is not a code that you can distinguish between because of your scope of practice. Other specified can be valuable as a term in ICD-10 coding. Unspecified means you do not know what it is. Again, these unspecified codes have asterisks denoting it is in local coverage determination.
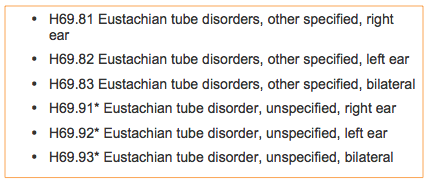
Figure 5. Codes for Eustachian tube disorders.
The next codes (Figure 6) cover exostosis, which is bony growth in the ear canal. You will see a code for family history of hearing loss. This is a Z code. Avoid Z codes as your primary, but having a code for family history of hearing loss can help drive medical necessity. The Z code for fitting and adjustment of hearing aid is a great code to use for hearing aid follow-up visits, when you are not seeking coverage from the claim. My belief is that you make every encounter in your clinic drive data. Anytime you see a patient, everything should be coded, both diagnoses and procedures. Then you will know how many of a particular issue you have seen. This code can then be useful from an internal data collection standpoint. There are codes for foreign body in the ear, initial encounter and subsequent encounter. Initial encounter is the first time you see them. Subsequent encounter is the second time you see them, and long-term follow-up is the third time and beyond. However, foreign body in the ear does not have a long-term follow-up.
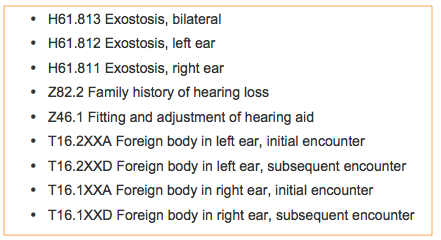
Figure 6. Code set.
Hearing conservation and treatment is the next code in the list. I would be careful about putting this code in any place on a claim that you are seeking coverage from a medical or health care insurer. This is a great code to use for occupational or worker’s comp claims, but not something I would put on a health care claim. It will most certainly drive a denial. Likewise, I would never put presbycusis on a claim. It is not a medical condition. It is age-related changes to the ear and it will often drive a denial.
In Figure 7, you will that there is a code for hearing examination following failed hearing screening. If I have been denied from Medicare from using this code, I would appeal it. The Medicare rules are clear about the fact that Medicare covers hearing tests that are the result of a failed screen. Even if they do not cover the screening, they cover the subsequent hearing test that comes from failed screening. I would feel comfortable using this code, but would avoid using it as my primary diagnosis. Z01.10 is a code is used when you performed hearing or vestibular testing and had normal findings. Using that code as your sole diagnosis or primary will often drive a denial. You should look at comorbidities, case history, and what you visualize, in addition to these things. There are codes for hematoma of the pinna and history of falling. Falls risk is something that those of us who do vestibular testing will be assessing, and history of falling is something you can use when screening for falls risk.
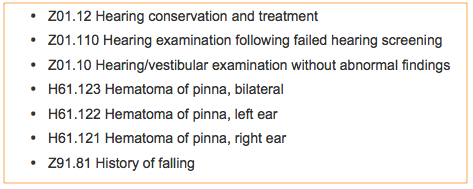
Figure 7. Code set.
The next set of codes (Figure 8) include hyperacusis, impacted cerumen, and inner ear disease unspecified. Impacted cerumen is cerumen covering clinically significant portions of the tympanic membrane, is generally hard, and requires instrumentation to remove. When you find a little black ball of cerumen in the ear canal but you can see the TM, even if the cerumen needs to be removed because the patient uses a hearing aid or so you can conduct the testing, it is not impacted cerumen. You should not code it as such, either on the procedure side or on the diagnosis side. Inner ear disease, unspecified, is in a local coverage determination.
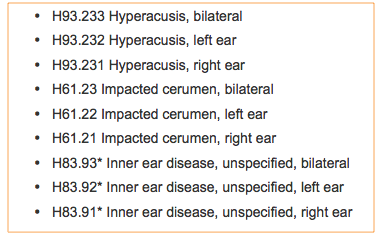
Figure 8. Code set.
Refer to Figure 9. Intellectual disabilities is also in a local coverage determination. Many of you have state mandates for testing of those who are developmentally delayed. These are great codes for you to use to code that disability. Some people have asked me how they are supposed to know; they are to ask the ordering facility or physician. If you do not know what kind of diabetes they have or what their intellectual disability is, ask the ordering physician or facility. These are chronic conditions. You would ask once, and then it would be in the medical record for future claims.
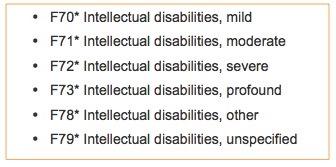
Figure 9. Code set, intellectual disabilities.
In Figure 10, you will see the codes for labyrinthine fistula, long-term use of antibiotics, long-term use of aspirin, malingering, and Meniere’s disease. Long-term use of antibiotics and aspirin are toxicity issues that should be noted in addition to the poisoning. Malingering is in some local coverage determinations, and is faking a hearing loss. There is no distinction in ICD-10 between active and inactive Meniere’s disease.
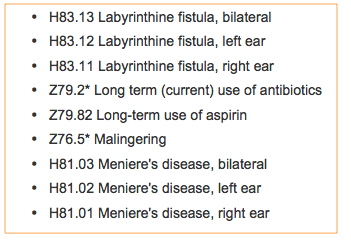
Figure 10. Code set.
Figure 11 lists the codes for mixed hearing loss, myringotomy tube status, noise effects on the inner ear and nystagmus. The myringotomy tube status code is good to use when you are doing tympanometry to see if the tube is open or patent. The code for noise effects on the inner ear is one that will be covered if it was from a blast. However, if it is from an occupational source, you may want to careful using it.
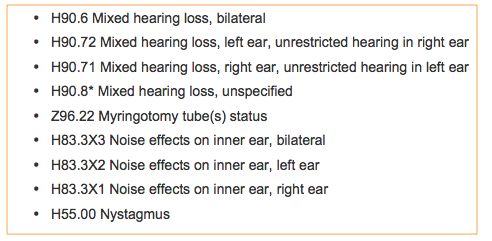
Figure 11. Code set.
Figure 12 lists the codes for otalgia, other specified hearing loss and otitis media. Otalgia is ear pain. I will come back to other specified hearing loss. Otitis media, unspecified, is in local coverage determinations. You would use this when you do not know the specifics, but otitis media has been diagnosed by a medical professional. There are many different kinds of otitis media. We, as audiologists, cannot diagnose otitis media.
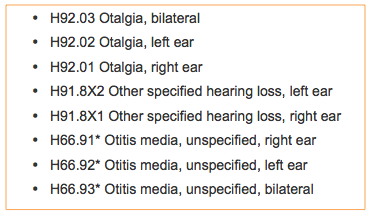
Figure 12. Code set.
Figure 13 lists the codes for otorrhea, which is drainage from the ear, as well as the codes for perforation of the tympanic membrane, unspecified.
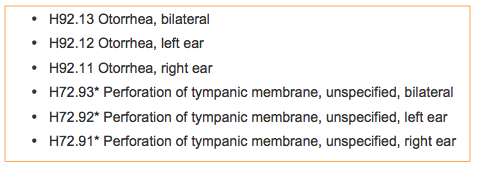
Figure 13. Code set – otorrhea, and perforation of the TM unspecified.
Figure 14 lists the codes for ototoxic hearing losses. You use the code for ototoxic hearing loss when you have deemed that a poisoning agent has created the hearing loss. You do not use the ototoxic hearing loss code until a hearing loss exists, and until you have deemed that the agent was the cause for the hearing loss. You can use the poisoning codes separate from the ototoxic hearing loss codes. If you are doing serial testing on someone who is undergoing chemotherapy, but they never have a hearing loss, you would still code poisoning. Poisoning, initial encounter, is the first time you see the patient. Poisoning, subsequent encounter, is the second time you the patient, and poisoning, long-term follow-up, is the third visit and beyond. There are codes for aminoglycosides, antimalarials, antineoplastics, aspirin, loop diuretics, macolides, and vasodilators. I gave the codes for the most general classes that have ototoxicity.
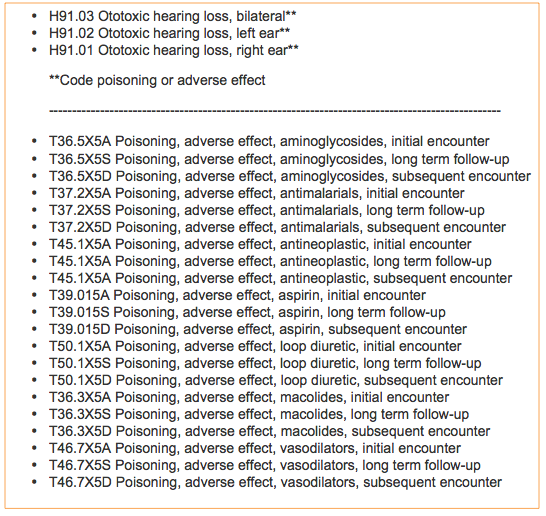
Figure 14. Code set, ototoxicity and poisoning.
In Figure 15, you will see a code for presence of external hearing aid. This is not a code I would put on a claim where I am seeking coverage, but it can be good for data collection. The most common code we will use is H90.3 for sensorineural hearing loss, bilateral. There are codes for sensorineural hearing loss unrestricted and unspecified. We have a code for sequelae following unspecified cardiovascular disease, which is in the local coverage determination, for when a patient has cardiovascular disease and you are doing assessments around that cardiovascular disease. There are codes for speech-language disorders, which can be valuable rationale for testing expressive, expressive/receptive, developmental disorder, or phonological disorders.
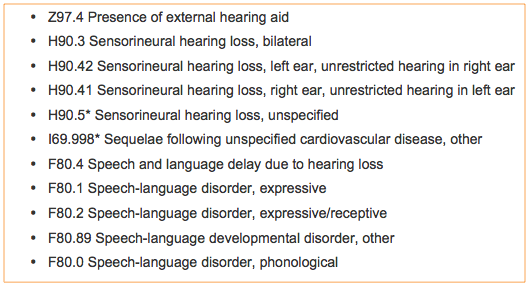
Figure 15. Code set.
Figure 16 lists codes for sudden idiopathic hearing loss, temporary threshold shift, and tinnitus. Remember that tinnitus is neither subjective nor objective. It is merely tinnitus.
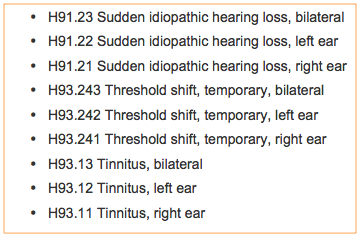
Figure 16. Code set - sudden idiopathic hearing loss, temporary threshold shift, and tinnitus.
Figure 17 lists the codes for transient ischemic disease and vertiginous disorder of vestibular function. Vertiginous disorder of the vestibular function codes are great for someone who is dizzy due to another disorder they have. You could use this code as well as code Meniere’s disease. The underlying disease is Meniere’s which is causing this vertiginous disorder of vestibular function. We also have codes for vertigo with aural, central, and peripheral. You can code vestibular function disorder, other or unspecified. These codes show there is a vestibular function disorder, but it is not something that has a code that has been noted. Vestibular function disorder, unspecified, is under local coverage determination.
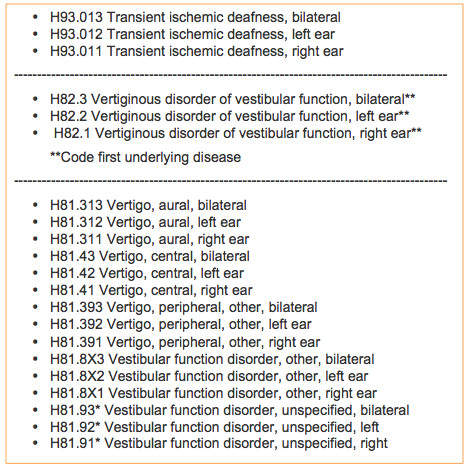
Figure 17. Code set.
Hearing Loss & Coding Scenarios
Different Hearing Losses Right v. Left Ears
Let’s talk about a few different hearing loss and coding scenarios. First, how do you code different hearing losses in the right and left ears? There is no way in ICD-10 to code that you have a conductive hearing loss in one ear and a sensorineural hearing loss in the other.
Instead, use H91.8X2 other specified hearing loss, left ear, and H91.8X1 other hearing loss, right ear. This is one option, and what I would use for billing a private insurer. They do not like unspecified codes. I am not seeing denials from private insurers for other specified hearing loss.
This is the same way I would code a unilateral hearing loss where the better ear has hearing loss, as there is no code for this scenario either. Use these two codes regardless of whether it is a sensorineural hearing loss in one ear, mixed in the other, or sensorineural hearing loss in one ear and conductive in the other. Type of hearing loss does not matter in this case; what matters in this scenario is which ear you are referring to. However, with some of the Medicare programs that have local coverage determinations, you may want to use "unspecified" instead, where you do not care about right or left ear, but you care about the type of hearing loss. When the coverage determination exists that needs this, they do not recognize "other specified". Instead, they recognize the type with "unspecified" after it. To summarize, code:
- H91.8X2 Other specified hearing loss, left ear
- H91.8X1 Other specified hearing loss, right ear
or
- H90.5* Sensorineural hearing loss, unspecified
- H90.8* Mixed hearing loss, unspecified
- H90.2* Conductive hearing loss, unspecified
Coding for Toxicity
Another scenario is toxicity from Viagra where the patient had a sudden hearing loss in the left ear, as an example of coding for toxicity. You code this H91.02. This was the first time you saw the patient with sudden hearing loss, you tested them, and you determined that it was due to the vasodilator.
- H91.02 Ototoxic hearing loss, left ear
- T46.7X5A Poisoning, adverse effect, vasodilators, initial encounter (First date you diagnose an ototoxic loss)
Normal hearing
For normal hearing, use one of the following:
- Z01.10 Hearing/vestibular examination without abnormal findings
- H93.2 Abnormal auditory perception - If they report communication difficulties
Newborn Hearing Screening Follow Up
For newborn hearing screening follow-up, you will want to code the pre- and post-natal conditions or symptoms, any comorbidities, and anything you see or measure. If they have previously failed a hearing screening, you will want to code Z01.110 and would add the -33 modifier to all the procedures. The -33 modifier means that all of these procedures are in the newborn hearing screening step process.
General ICD-10 Considerations
With ICD-10, there is a grace period. In 2015/2016, traditional Medicare will not penalize providers for using unspecified codes. Private insurers, however, are already penalizing providers for using unspecified codes. Medicare is not. This is why you see some local coverage determinations allowing the use of unspecified. The grace period exists in this year. We do not know what will happen beyond this year.
We want to code what we learn from our patients and what we find with our testing using ICD-10, but we do not code for reimbursement. We do not use rule out diagnoses, once you know they do not exist. The following link explains the Medicare position on rule out diagnoses. CGS is one of the Medicare contractors and they do not recognize rule out diagnoses. Once you know the patient does not have a hearing loss, you do not code a hearing loss.
You should only use ICD-10 for dates of service of October 1, 2015 or after. You cannot have ICD-9 and ICD-10 codes on the same claim. If you are still billing something from September 30, 2015 or prior, you must use ICD-9 on that claim. You can have up to 12 diagnoses per claim. All the diagnoses should be linked to procedure. Each procedure can have four diagnoses linked to it. You want to use the most specific code possible. We still do not have a good idea about the impact of Z codes on reimbursement, other than we are seeing denials when they are the primary diagnosis.
In your handout, I have listed coding resources from the national audiology associations and from different manuals. Everyone should have either software or a manual which has all the codes for the extraneous diagnoses that you may see. There may be odd syndromes or odd conditions that you encounter. There are online coding look-up options also available, which are not as good as the manuals. More information on PQRS and the ICD-10 implementation can also be found at the Audiology Quality Consortium website.
PQRS
I want to stress that while PQRS has been tied to affordable care, it preceded affordable care. PQRS has been in effect from bipartisan legislation in the Bush administration since 2006. Its use for audiology began in 2010, but implementation for other health care professionals came in 2008. When they passed the Medicare sustainable growth rate bill in the summer, which was out of a republican senate and republican house; bipartisan legislation was passed. It was still about paying for performance. I mention the political aspects of this because the ship left the station 10-15 years ago, and it will not be changed by an administration. We have to get on this bandwagon. Eventually, you will only get paid if you participate in quality reporting. That is the end goal. PQRS is about quality reporting.
For audiology specific PQRS information, go to www.audiologyquality.org. If you need to know whether or not you are eligible to report PQRS because of your work situation, please visit these links: CMS link #1 and CMS link #2. The full URLs are included in your handouts as well. Audiologists who bill Medicare part B beneficiaries must participate in 2016 to avoid a minimum 2% reduction in Medicare reimbursement in 2018. PQRS does not apply to Medicare Advantage, part A hospital, or skilled nursing facilities. PQRS applies to traditional Medicare, and only applies to claims submitted to Medicare for covered services.
Six Required Measures
We have six required measures. All six measures are required; none are optional. If you are eligible to report, you will need to report all six. The six measures are:
- Measure #130: Documentation and verification of current medications in the medical record.
- Measure #134: Screening for clinical depression and follow-up plan
- Measure #154: Falls Risk Assessment
- Measure #155: Falls Risk Plan of Care
- Measure #226: Screening for Tobacco Use/Cessation
- Measure #261: Referral for otologic evaluation for patients with acute or chronic dizziness
Audiologists must positively report on 50% of all eligible Medicare Part B beneficiaries for all six of these measures to avoid a 2018 penalty. You should not report that you did not do it. That would be like not reporting it at all. You have to report a positive action like you referred, documented, or screened for the reporting to count and to assist in avoiding the penalty. That rule also existed in reporting in 2015.
Medicare created this website to walk you through PQRS information. Here is a link to the actual measures themselves. Again, these links are subject to change but they were accurate and active at the time of this presentation. I encourage you to read the measures yourself directly from the source. This will help answer or alleviate some of the questions you may have.
Measure #261: Referral for Otologic Evaluation for Patients with Acute or Chronic Dizziness
This measure is dependent on diagnosis code. This has to be reported a minimum of once per calendar year for 50% of eligible patients. Anytime you perform vestibular testing, tymps and audio, or if you have the diagnosis code of dizziness or BBPV, you need to report on this measure as it is diagnosis code driven.
The first code, G8856, is a positive reporting, meaning that you referred a patient because they were dizzy or they had BPPV. G8857 means you did not refer them because they are already under the care of a physician for acute or chronic dizziness. G8858 is a negative reporting and when used, it is like you did not report it at all. This measure is the only time ICD-10 comes into PQRS.
Measure #130: Documentation and Verification of Current Medications in the Medical Record
Documentation of current medications has to be reported on every patient visit. You need to code to the best of your ability and document it fully. Here are some distinctions. Writing, “high blood pressure medication, insulin”, is not to the best of your ability. The best of your ability is that you have the drug name, the frequency and the route, but you may not have the dosage. This is an important measure to patient care, regardless of your work setting, and should be done to the best of your ability. When I worked clinically, I could not have interpreted an audiogram if I did not know about the patient’s medications.
This is done for vestibular testing. Code 92543 is listed, but would be replaced with 92537. I did not replace it in my list purposefully as the measure still talks about 92543, and until that change, I want to keep this consistent with what the measure says. However, if you are doing vestibular testing, audio, ABR, comprehensive OAEs, cochlear implant or osseointegrated evaluation, you want to document medication.
Code G8427 is that you have listed medications, including prescription, over the counter, herbals, and vitamin/dietary supplements, which are documented by the provider including the drug name, dosage, frequency, and route, to the best of your ability. This would be a positive reporting. Code G8430 is for provider documentation that the patient is not eligible for medication assessment. Situations for this could be an emergency situation, non-English speaking and unaccompanied, or cognitively impaired and unaccompanied. Code G8428 is negative reporting as if you did not report at all and does not count towards avoiding the penalty. If the patient does not take medications, you would use G8427. You have documented that they do not take any medications.
Documenting medications is not just about PQRS; it is about good patient care. Documenting medications is important in practicing audiology. It is something that the patient should be instructed to provide at the time they schedule the appointment. Almost every health care provider in the country asks about medication. Sometimes, the provider may need to call the primary care physician or pharmacist to obtain the list. Most people carry a list of their current medications. It can also be in a shared medical EMR or comes over on the order. Then, all you are doing is making a copy asking the patient about each medication, verify whether it is current, sign it, date it, and place or scan it to the medical record.
Measure #134: Screening for Clinical Depression and Follow-up Plan
The screening of clinical depression measure is no longer optional, but is only tied to assessment for tinnitus. You have to report this a minimum of once per calendar year for any patient for which you use the assessment for tinnitus codes. An important factor to keep in mind is whether you are allowed by your state licensure law to screen for depression. It is the responsibility of the providers themselves to find out, in writing, from their state. If you are not reporting on this measure and you are penalized for it, you will need to supply documentation of why you did not do it. I would not do this if you are not appropriately trained and competent to perform the screening and provide the plan of care. You need to create a plan of care and at a minimum refer to a practitioner who is qualified to diagnose and treat depression.
The depression measures are:
- G8431: Positive screen for clinical depression using an age appropriate standardized tool and a follow-up plan documented.
- G8510: Negative screen for clinical depression using an age appropriate standardized tool and a follow-up plan documented.
- G8433: Screening for clinical depression using an age appropriate standardized tool not documented, patient not eligible/appropriate - Patient refuses to participate.
- G8432: No documentation of clinical depression screening using an age appropriate standardized tool.
- G8511: Positive screen for clinical depression using an age appropriate standardized tool documented, follow-up plan not documented, reason not specified.
G8431, G8510, and G8433 are all positive reporting. The patient was not eligible if they refused to participate or there was an emergency situation, and you would use G8432. G8511 is again a negative report stating you did not report and I would not use this for liability purposes. Using these will not help you avoid the penalty.
Here is a list of appropriate depression screening tools. There are links to these tools in your handout.
- Patient Health Questionnaire (PHQ-9)
- Beck Depression Inventory (BDI or BDI-II)
- Center for Epidemiologic Studies Depression Scale (CES-D)
- Duke Anxiety-Depression Scale (DADS)
- Geriatric Depression Scale (GDS)
- Cornell Scale Screening
- PRIME MD-PHQ2
Measure #154: Falls Risk Assessment
Falls risk assessment is one of the new measures for 2016 that apply to audiologists. You have to report at least once per calendar year. I have added links for each of the measures themselves in your handout. The falls risk assessment needs to be completed by the audiologist prior to performing a balance assessment. It is only for patients that you perform a balance assessment on. The risk assessment must include balance/gait, and/or one of the following: postural blood pressure, vision, home fall hazards and documentation on whether or not medications are a contributing factor to falls within the last 12 months. You must document in the medical record that you have performed a falls risk assessment or that you have referred - either by observing a transfer from a chair and walking or using a standardized scale; or, you must document referral for assessment of balance and gait. This has to be done. You have to document one of the three: 1. that they are functioning well or not functioning well with vision, or that you have documented a referral for an assessment of vision; 2. that you have either counseled them on home falls hazards or documentation that you have asked about home falls hazards; or, 3. that you have referred for home falls hazards assessment; or that you have talked about medications and whether or not they are contributing to falls.
Please refer to the Falls Risk Assessment Tools and links in your handout, including Get Up and Go, Tinetti, and Berg.
It is important that you ask the following case history questions. I recommend they be asked at intake.
- Have you ever experienced dizziness, unsteadiness, imbalance or vertigo? Yes or No
- If yes, are you feeling dizzy today? Yes or No
- If yes, please describe: _________________________
- Frequency of occurrence: __________________________
- If yes, is it accompanied by any of the following: nausea, ringing or noises in your ear, hearing loss, visual disturbances, or other
- Have you fallen within the past 12 months? Yes or No
- If yes, how many falls have you experienced in the 12 months? ________
- If you have fallen, have you been injured? Yes or No
- Please describe your injury: _____________________
- Do you experience visual difficulties or disturbances? Yes or No
- If yes, please describe: _______________________________________
- Do you currently take a Vitamin D supplement? Yes or No
Figure 18 is a table for falls risk assessment. If a patient has fallen two or more times in the past 12 months, or they have had one fall with an injury, you need to go through the risk assessment process. You either observe the transfer and walking, do a standardized test like the Get-Up-And-Go, Tinetti or Berg, or you refer them for falls risk assessment. You also talk about the blood pressure, vision, home fall risks hazards or the medication review.
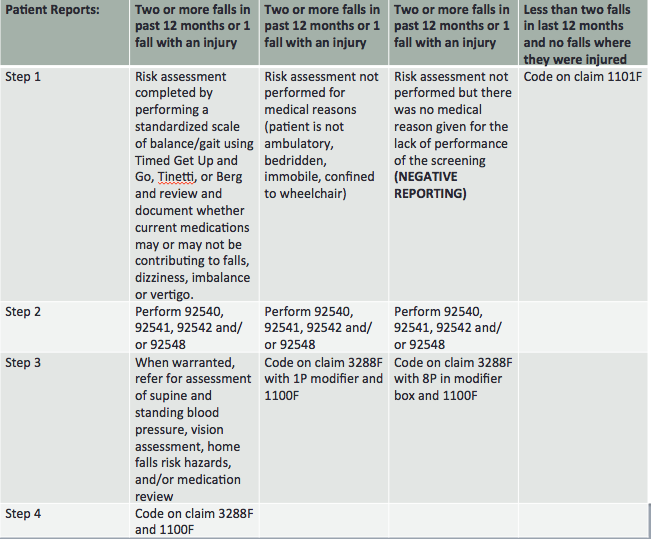
Figure 18. Table for Measure #154, Falls Risk Assessment.
Once you have done this, you would code a positive reporting that you have done it. This is code 3288F and 1100F. Those should be put on the claim just like the G codes were put below the procedures.
If a patient has had two or more falls or one or more injuries, but you cannot assess them because they are bed-ridden, not ambulatory, immobile, or confined to a wheelchair, then they are ineligible for a falls risk assessment. You would code 3288FF with 1P in the modifier box, and 1100F. If they have fallen two or more times and one or more with injury, but you did not do a risk assessment or did not make a referral, you did not meet the criteria of the code and this is negative reporting. It is just like you did not report at all. Instead of the 1P modifier, you would put 8P. If you see a patient for vestibular testing and they have not fallen twice in the last 12 months and have not been injured in any fall, this is a positive reporting and you would code 1101F, as not a falls risk.
Measure #155: Falls Risk Plan of Care
Measure 155 for falls risk plan of care needs to be done if you are doing measure 154 - they go together. It needs to be reported once per calendar year. It always must be reported when a patient is screened for falls risk. The plan of care must include consideration of vitamin D supplementation, as well as balance, strength, and gait training. The medical record must include documentation that the patient was referred to their physician for vitamin D supplement advice. The documentation must include information that balance, strength, and gait training (vestibular rehabilitation) were provided or that they were referred for that type of care if they are a falls risk. This measure applies if they were a falls risk in measure 154. If they were not a falls risk in 154, then you do not do this measure. Figure 19 is a table for falls risk plan of care. If you do vestibular testing and the patient has been deemed to be a falls risk (fallen two or more times or fallen with an injury), you need to go through the process of positive reporting with 0518F code. You can also do positive reporting with code 0518F and modifier 1P, for a non-eligible patient due to being bed-ridden, etc. It is a negative reporting if you do not do the plan of care aspect.
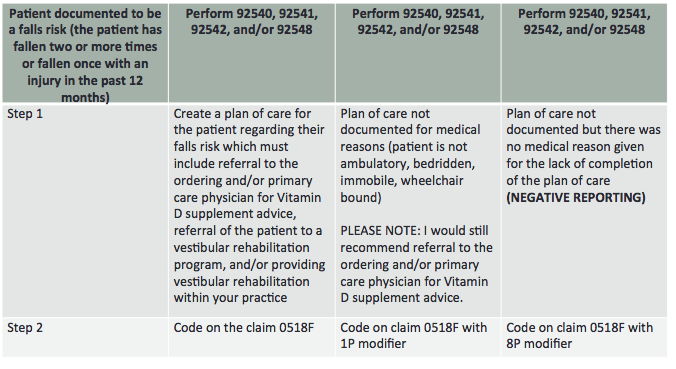
Figure 19. Table for Measure #155, Falls Risk Plan of Care.
Measure #226: Screening for Tobacco Use/Cessation
The final new PQRS measure for audiologists is screening of tobacco use. Tobacco use can have an effect on hearing, balance, and tinnitus. It must be reported at least once per calendar year for 50% of eligible patients. You need to advise patients to quit tobacco use and refer the patient to a physician for counseling and pharmacological options. You can make this less complicated by asking the following question at intake:
- Have you used a tobacco product (cigarette, cigar, smokeless tobacco) one or more times in the past 24 months? Yes or No
- If yes, how often have you used a tobacco product in the past 24 months?
- If yes, what type(s) of products have you used? ____________________
If you are doing vestibular testing, an audiogram or assessment of tinnitus, you need to ask your patients if they have used tobacco in the last 24 months. Then, you should recommend that they quit using tobacco. You will write in the report to the ordering physician and/or primary care physician that you recommended they quit, and that you give them a sheet, created by the Audiology Quality Consortium, printed out to tell them that they need to quit. You can also get materials from the American Lung Association, American Heart Association, and American Cancer Society to pass out to your patients. You would code on that claim 4004F. If you did an audiogram, vestibular testing, or assessment for tinnitus but you did not screen them for tobacco use due to limited life expectancy or they could not answer questions, they are not eligible and you would code 4004F with modifier 1P. If you did not screen, did not provide intervention, did not ask the questions, did not recommend them to quit, or did not give them any material or counseling on quitting, this is a negative reporting and would not help you avoid the penalty. Finally, if they do not use tobacco, this is a positive reporting as they are not a positive tobacco user. You code 1036F on the claim. You can find a table for this measure in your handout.
Summary
We know that PQRS is complicated. It is showing that audiologists’ role in the coordination of care for the whole patient is valuable, and elevates our stature in the health care system. The government is requiring every health care provider to get to a threshold of nine measures. As a member of the Audiology Quality Consortium, we are trying to make measures that mean something to the hearing and balance systems, and to audiology care, and that are not egregious. There is a sample claim form with PQRS at www.audiologyquality.org, to help you in filling one out. If you want to know about your PQRS reporting data and how well you have done reporting, you can go to www.qualitynet.org. Many of you went there to file a PQRS appeal. Visit the website, go to the physician’s section and use the verification tool to look at your past and current reportings.
If you have any further questions about PQRS or the codes that have been presented, I strongly advise you to reach out to the national audiology associations that you are a member of, and visit the Audiology Quality Consortium website. If you do vestibular testing, it is important that you have a new CPT manual for 2016. Everyone should have a 2016 ICD-10 manual, and become well informed about PQRS.
Questions and Answers
Can you perform falls risk assessment and refer if you do not perform vestibular testing?
You do not have to do falls risk if you do not perform vestibular testing. For the Falls Risk Assessment measure, you are only eligible to report it if you do vestibular testing. It is important for you to ask your patients if they have fallen and refer them out. However, you do not have to report that measure unless you are doing vestibular testing.
Since one of the manufacturers just came out with FDA VEMP equipment, how do you document VEMP testing?
In March 2011, as the American Medical Association owns CPT codes and their use, the CPT Assistant journal says that VEMP testing should be reported using 92700, unlisted, otorhinological item or service. If you are billing Medicare for that, you would have a patient pay at the time of visit, have them complete an ABN, and then you would refund them probably 30% of the time that a payer will reimburse you for that. ABNs are only for Medicare.
How do PQRS guidelines relate to pediatric evaluations?
PQRS does not relate to anything but traditional Medicare, so it is not applicable to pediatric evaluations.
Cite this Content as:
Cavitt, K. (2016, February). 2016 Coding and reimbursement update. AudiologyOnline, Article 16245. Retrieved from https://www.audiologyonline.com.


