 From the Desk of Gus Mueller
From the Desk of Gus Mueller

This month at 20Q, we’re excited to have a guest author who is a researcher at Walter Reed National Military Medical Center. More about her shortly. To get us started, I’d like to talk a little about the audiologic history associated with Walter Reed General Hospital, which in later years was known as Walter Reed Army Medical Center, until its latest relocation to Bethesda, Maryland, and current title.
Many of you have heard the story of the four military audiology rehabilitation centers that were established ~1943, toward the end of World War II, to accommodate veterans with hearing loss. The most talked about, tends to be the one at Deshon Army Hospital in Butler, Pennsylvania, primarily because the head of audiology at that facility was a fellow named Captain Raymond Carhart—who returned to Northwestern University to make quite a name for himself (in case you haven’t heard).
The center, however, that rose to prominence in the audiology world, was Walter Reed. In addition to advanced diagnostics and extensive rehabilitative audiology services, this center has long had a research component. In the early days, there was the notable Robert Galambos and Aram Glorig. Beginning in the 1970s, the research section was under the direction of audiologist Brian Walden, a position he held for ~40 years. Since Brian’s retirement, the Chief Scientist has been Douglas Brungart—Doug visited us here at 20Q back in 2014. For several decades, Walter Reed has been known as a leading source of meaningful audiology research.
Personally, during my seven years at Walter Reed, while I was officially part of the “clinical section,” it was only natural to mingle with the researchers. One memorable project was in 1980, when we conducted some of the first hearing aid verification using probe-microphone measures. I’ll do the math for you—for those of you who think that probe-mic verification is something new—that was 45 years ago! This was before the days of probe “tube” measures—we actually placed the entire microphone (about 4mm by 5mm by 2mm) in the ear canal, within a few mm of the eardrum. If you think cerumen is a problem with probe-mic measurements today, you should have seen the condition of this microphone after a day's work!
Okay, enough history! There are a lot of interesting things happening today. To tell us about many of them is our guest author, Alyssa Davidson, AuD, PhD, research investigator at Walter Reed National Military Medical Center, where she focuses on translating research findings into clinical practice. Her research expertise centers on auditory processing, treatment outcomes, and military exposures.
You’re probably familiar with many of Dr. Davidson's publications. Her research contributions were recently recognized with the 2024 Military Health System Research Symposium Award for Excellence Outstanding Research Accomplishment. She also received the 2021 ASHA Perspectives Journal Editor's Award.
You’ll enjoy reading the research review that Alyssa provides us, as she weaves a common thread through topics such as long-term hearing aid satisfaction, the association with temporal and cognitive processing, the utilization of self-report hearing loss measures, how this relates to normal audiograms, and treatment options.
You’ll see that it’s obvious that the reputation of excellent research at Walter Reed is continuing.
Gus Mueller, PhD
Contributing Editor
Browse the complete collection of 20Q with Gus Mueller CEU articles at www.audiologyonline.com/20Q
20Q: Emerging Research - Normal Audiograms, Real-World Struggles, and Innovative Interventions
Learning Outcomes
After reading this article, professionals will be able to:
- Distinguish between audiometric and patient-reported problems of auditory dysfunction in cases with and without normal hearing thresholds.
- Compare outcomes from low-gain hearing aid fittings in individuals with and without peripheral hearing loss.
- Summarize findings from a systematic review on the relative contributions of auditory and cognitive abilities.

1. I’ve seen your name on several interesting publications in recent years, and I’m hoping we can talk about some of these findings a little more?
Most certainly. I've been fortunate to work with a lot of great people, which has led to exciting research in the areas of evaluating and treating auditory dysfunction, especially where typical hearing tests fall short. Where do you want to start?
2. One that really caught my eye a few years back was the systematic review related to hearing aid satisfaction.
Good place to start . . . that has been one of my favorites, too (Davidson, Marrone, Wong, & Musiek, 2021). Primarily, we were looking at the relationship between different pre-fitting tests that could be used with hearing aid fitting, and how those results are related to long-term satisfaction. The five main categories that are important to consider for a pre-fitting hearing aid assessment were utilized (Ricketts et al., 2019): speech recognition in quiet, speech recognition in noise, reception thresholds for speech in noise, speech-based subjective ratings, and dichotic speech tests, in addition to tests with non-speech material.
After reviewing over 1000 articles, 21 made the cut for evaluating this relationship. We soon found that hearing aid satisfaction was not a simple outcome to evaluate. We had to divide outcomes into hearing aid satisfaction alone and a global score of hearing aid satisfaction that also included other domains. Turns out, pre-fitting measures of speech in noise were the only categories to be a significant indicator of hearing aid satisfaction. When the outcome of satisfaction included other domains, measures of speech in noise still came out on top, but speech-based subjective ratings and tests with non-speech material did show significant relationships. It was also determined that degree of hearing loss did not play a significant role in these outcomes.
3. Interesting findings—the test that ended up the most significant—speech in noise testing—is the one that most audiologists don’t perform, and the least significant test—degree of hearing loss—is the test that many audiologists pay the most attention to. Why do you think this is?
That’s one of the most interesting and clinically relevant questions related to this research. If you believe that the main goal of a hearing aid is to restore audibility to soft sounds, you might think individuals with more hearing loss would report more benefit from wearing hearing aids. Conversely, if you think that hearing aids provide more benefit to individuals who still have greater residual hearing function, you might think individuals with minimal hearing loss would report more benefit. But the reality is that hearing loss doesn’t reliably predict benefit in either direction. We, of course, were not the first to report this (Hayes et al. 1983; Bentler et al. 1993; Walden & Walden 2004; Ng et al. 2013; Perez et al. 2014; Meister et al. 2015; Mantello et al. 2016; Thorup et al. 2016; Musiek et al., 2017; Kwak et al., 2020).
4. You’re saying that there is more to hearing aid satisfaction than the basic increase in audibility?
Right. The pure-tone audiogram really only tells us how soft a sound can be for someone to detect it — it's a measure of sensitivity at the level of the auditory periphery. But hearing satisfaction isn’t just about detecting a sound; it’s about being able to understand it clearly and comfortably, especially in complex environments. That clarity involves a whole system beyond the ear, including the brainstem and cortical pathways responsible for discrimination, temporal processing, and the interpretation of auditory input into meaningful language.
So, two people could have nearly identical audiograms but completely different experiences with their hearing. One might have intact temporal and cognitive processing, allowing them to make sense of speech even in noise, while another might struggle with those higher-level processes, resulting in distorted or effortful listening. The audiogram wouldn’t tell us anything about that difference. That’s why I think satisfaction is often poorly correlated with the audiogram. It doesn't capture the full complexity of the auditory system, especially not the neural or cognitive contributions that matter most for real-world communication.
5. That makes sense. Your group had a second study related to this same general topic?
Yes, we did a prospective study where we wanted to examine how both auditory and non-auditory factors affected hearing aid outcomes (Davidson, Musiek, Fisher, & Marrone, 2021). We included tests like the Listening in Spatialized Noise Sentence Test (LISN-S), Gaps in Noise (GIN) test, Dichotic Digits Test (DDT), and also personality, self-efficacy, and self-report of hearing disability. Interestingly, Gaps-in-Noise performance—how well someone can resolve quick gaps in noise—was one of the biggest predictors of hearing aid satisfaction. Not necessarily benefit, but satisfaction.
6. I’ve never conducted the GIN test . . . something developed by Frank Musiek years ago I believe?
Yes, Frank and colleagues published the first article on this back in 2005. It’s primarily used in an auditory processing battery to evaluate temporal resolution. Here’s a brief summary:
- Stimulus: The Gaps in Noise (GIN) test presents 6-second segments of white noise.
- Silent Intervals: Within these noise segments, short silent intervals (gaps) are randomly inserted.
- Gap Duration: The gaps vary in duration, ranging from 2 to 20 milliseconds.
- Number of Gaps: Each noise segment may contain 0 to 3 gaps.
- Test Procedure: The listener is instructed to identify when they perceive a gap in the noise, typically by pressing a button.
- Scoring: The GIN test provides measures like the approximate gap detection threshold (APT) and the correct score percentage (CSP). The APT represents the shortest gap duration a listener can detect at least four times, while the CSP is the overall percentage of correctly detected gaps. These are determined for each ear separately.
7. Detecting small breaks in a noise sample doesn’t seem like it would be related to real world problems with hearing, such as understanding speech in background noise?
You’re right, on the surface it doesn’t, but actually, we know from the literature that temporal resolution processing abilities are positively related to understanding speech in noise (Feng et al., 2010; Kumar et al., 2012; Nair et al., 2017). It is likely that individuals with poorer GIN performance have reduced temporal resolution abilities, which may hinder their capacity to rapidly parse complex auditory stimuli. This difficulty in processing speech, particularly in challenging listening environments, could lead to greater communication difficulties and, ultimately, lower satisfaction with their hearing and the performance of hearing aids.
8. You mentioned before that cognition plays a role in “real-world communication.” Have you also looked into how cognitive abilities factor into hearing aid satisfaction outcomes?
As a matter of fact, yes! A few years ago I collaborated with Pam Souza on a systematic review examining the connections between auditory and cognitive functioning (Davidson & Souza, 2023). I was at Northwestern University at the time, and one of the debates we often encountered was whether auditory processing abilities and cognitive abilities are fundamentally related, and if so, whether that relationship is consistent across different domains or more selective—we thought we might find some answers in a systematic review.
We separated auditory processing abilities into behavioral measures—like speech-in-noise performance, altered speech perception, temporal processing, and binaural processing—as well as electrophysiological responses, including mismatch negativity (MMN), P50, N200, P200, and P300. On the cognitive side, we categorized abilities into working memory, processing speed, executive/inhibitory control, fluid intelligence, visual perception, and multidomain or global cognitive functioning.
From 126 included studies, we saw a mix of findings, but some clear trends emerged. For instance, tasks involving distorted or noisy speech were consistently related to working memory and processing speed. Temporal order tasks showed significant correlations with working memory, fluid intelligence, and global cognition. On the electrophysiology side, some cortical auditory evoked potentials—particularly later components like the P300—were associated with working memory and executive functions.
All in all, the review underscored the importance of considering both auditory and cognitive factors when evaluating listening difficulties. While they don’t always go hand in hand, there are definitely domains where the two overlap in meaningful ways.
9. Do these findings carry over to the research you’ve been doing recently?
To some extent, yes. One project that stands out is our work on the Tinnitus and Hearing Survey-Hearing Subscale—or THS-H for short (Davidson et al., 2023). This one’s especially close to me because we were able to take something that was just a simple, four-item questionnaire and use it to create a truly impactful tool for evaluating hearing difficulties. Notably, we adapted the THS-H from its original form (Henry et al., 2015) rather than recreating the wheel.
10. I’ve never heard of the THS. Can you give me some background?
Sure. The Tinnitus and Hearing Survey (THS) was originally developed by the Department of Veterans Affairs in 2015 to help evaluate hearing and tinnitus problems. The goal of the original questionnaire was to determine whether hearing or tinnitus issues should be prioritized for treatment. In its initial form, the hearing subscale response options ranged from 0 to 4, resulting in a maximum possible score of 16.
To better align the THS-H with other questionnaires we were using, such as the Speech, Spatial, and Qualities of Hearing Scale (SSQ), we modified the response options to a 0–10 scale. With this change, the maximum total score for the hearing subscale increased to 40, based on the sum of four questions. These questions can either be self-administered by the patient or administered through an interview with a provider. Importantly, our publication (Davidson et al., 2023) also provides a conversion equation, allowing scores from the original 16-point scale and the new 40-point scale to be compared or used interchangeably. Our adaption of the four-item hearing questions from the THS are shown in Figure 1.
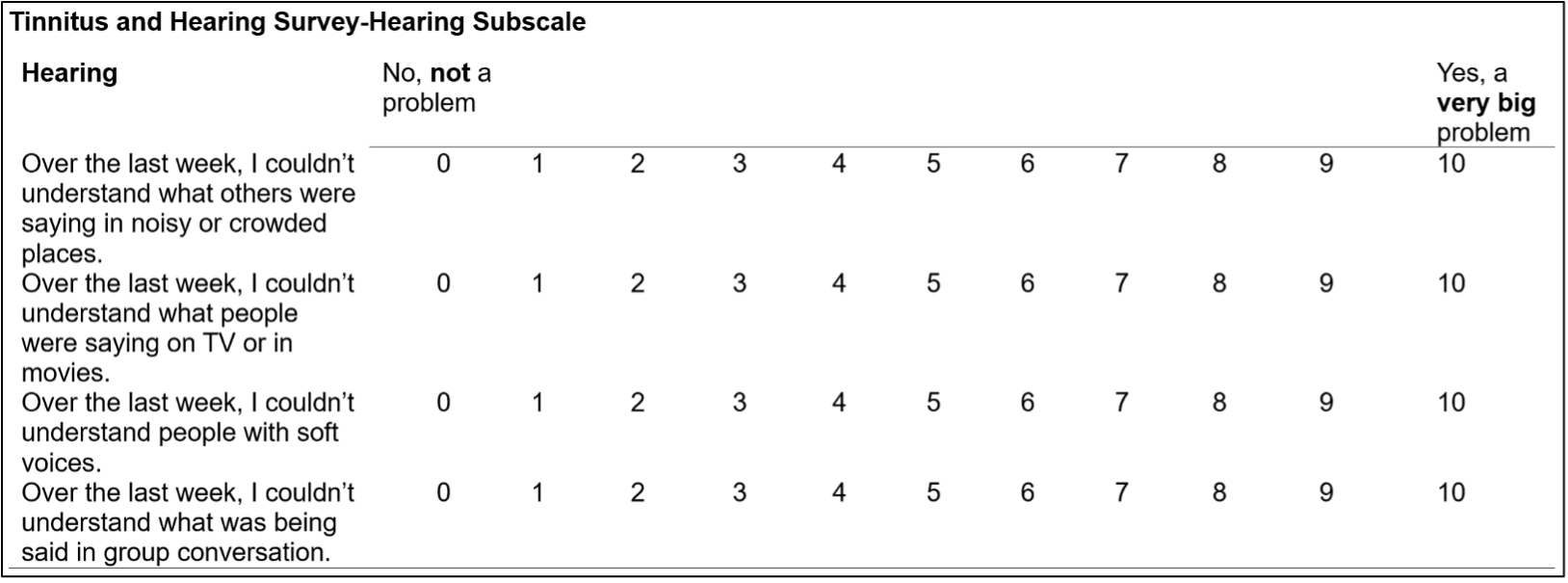
Figure 1. Modified Tinnitus and Hearing Survey-Hearing Subscale (Davidson et al., 2023).
11. Okay, thanks. Sorry for the delay . . .
No problem. Some data for the THS-H were collected on both versions, this is how we were able to create a conversion equation. However, we pulled together data from only the non-converted scores from the 40-point version to evaluate over 22,000 service members performance and establish normative values for the THS-H.
That’s a large-scale dataset in our opinion, and what came out of it was a clinically validated cutoff score of 27—meaning that if someone scores above that, they fall into the bottom 5th percentile in terms of hearing performance. And that one number helps clinicians quickly identify who needs further evaluation, even if their audiogram looks “normal”. To note though, the cutoff was determined in a population that included those with noise and blast exposure. We are currently preparing a document that has a cutoff for those without such histories.
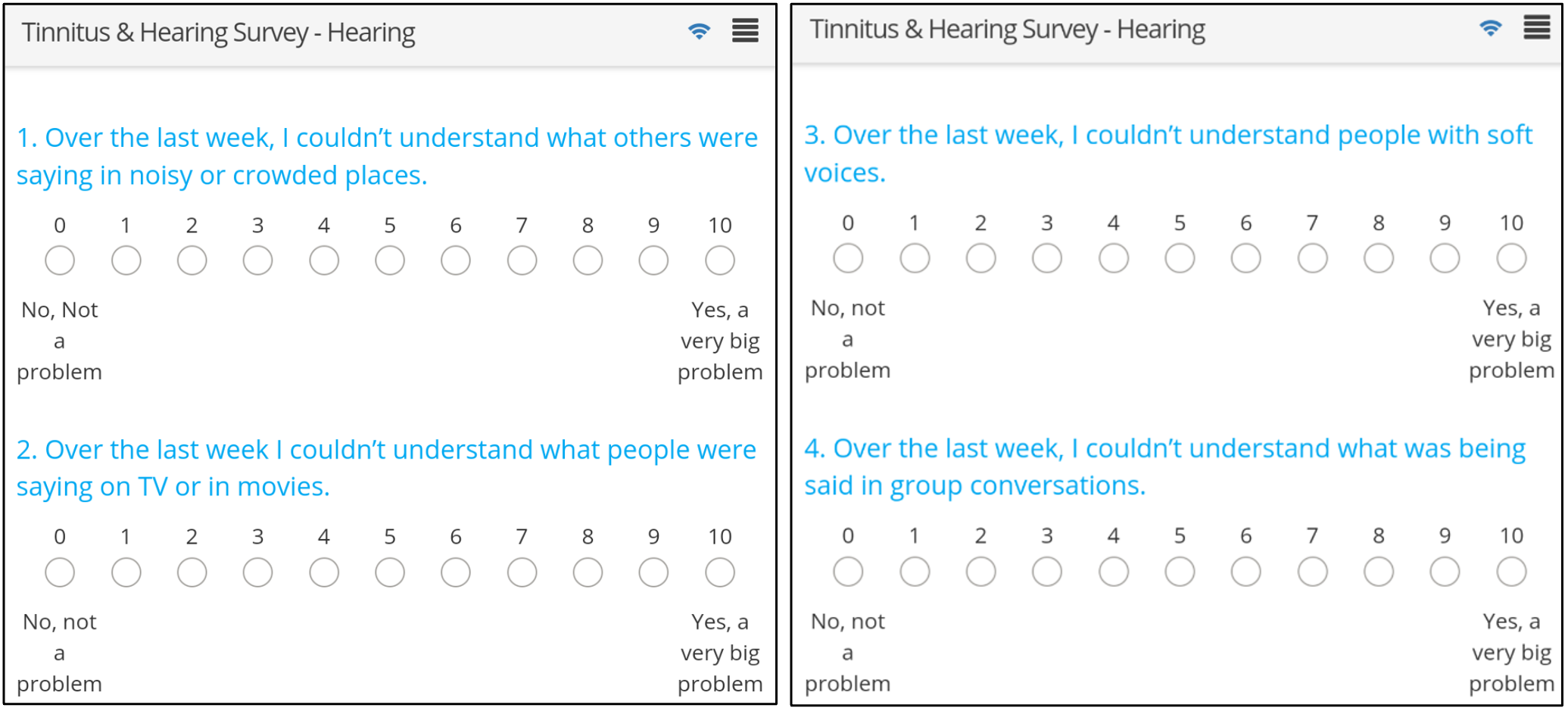
Figure 2. Tablet-based version of the THS-H.
12. How do you envision the THS-H being used in clinical audiology settings?
I see the THS-H becoming a go-to tool for audiologists who want a fast, standardized way to capture a patient’s functional hearing complaints—especially in situations where the audiogram doesn’t tell the whole story. One of its biggest strengths is how quickly it can be administered while being generalizable to any population. Once the publication is out with the cutoff for a population without noise and blast exposure, a more conservative cutoff can be utilized in any setting.
As I’ve mentioned, we’ve embedded it into a tablet-based tool we developed called the Patient Centered Concierge, or PCC, which automates the process of collecting results from the THS-H and other assessments, and integrates them directly into the audiology medical record. All those data then flow into the DOD-wide hearing database, which is managed by the Hearing Center of Excellence. So, while it’s already making an impact within military audiology, I think the bigger picture is using tools like the THS-H to elevate clinical decision-making everywhere—by making functional hearing status visible, trackable, and actionable.
13. Patients with normal hearing thresholds but high THS-H scores seem to represent a unique challenge—what do you think is driving their hearing complaints?
That’s a question that comes up a lot in our work. For the Service Member and Veteran populations, the answer often lies in the patient’s history. Specifically, whether they’ve ever experienced temporary changes in their hearing after noise exposure, or had a blast exposure in the past. Those kinds of experiences aren’t always documented in traditional hearing conservation programs, but they can reveal a lot. In fact, in our recent paper (Brungart et al., 2025), we looked at over 10,000 Service Members with normal hearing thresholds and found that self-reported hearing difficulties increased systematically even within the so-called ‘normal’ range. Importantly, individuals with a history of noise exposure, and especially those who reported noticeable temporary threshold shifts after noise, had significantly more hearing complaints, regardless of their hearing thresholds.
Another important piece of this puzzle is the 500 Hz N₀Sπ (pi) masked threshold, which assesses binaural integration and is a component of the Masking Level Difference (MLD) test. The MLD enjoyed some clinical popularity back in the 1980s, but is seldom used today, so you might not be familiar with it. The primary version used clinically today is the one created by Wilson and colleagues in 2003. Here’s a brief summary:
- Stimulus: 500 Hz pure-tone signal with broadband masking noise.
- Components:
- N₀S₀: Signal and noise are in-phase and identical at both ears.
- N₀Sπ: Signal is out-of-phase (180° phase shift) between ears, while noise remains identical.
- Presentation: Both signal and noise are delivered bilaterally through headphones.
- Scoring: The listener’s threshold for detecting the tone is measured in both the N₀S₀ and conditions. The MLD score is obtained by calculating the difference between components.
14. This test proved to be sensitive?
Yes, we’ve found that the N₀Sπ specifically (and not the MLD difference score) is highly sensitive to the various kinds of exposures we’re talking about—blast, noise, and temporary threshold shifts (Grant et al., 2021)—and it correlates well with both hearing difficulties and high THS-H scores (Davidson et al., 2022; Davidson et al., in press). For patients with normal audiograms but persistent complaints, N₀Sπ provides a critical additional lens. It helps identify functional auditory deficits that traditional audiometry misses, and we believe it should be part of the test battery for individuals who fit this profile. Additional work on the N₀Sπ is in preparation for dissemination.
15. What do your findings reveal about how we should be thinking about noise exposure and hearing loss—especially in individuals who have normal audiograms but report hearing difficulties?
The findings tell us two really important things: First, that our traditional definitions of noise-induced hearing loss may be too narrow. Historically, we’ve relied almost exclusively on pure-tone thresholds to define hearing loss, but our data suggest that there’s a spectrum of noise-related auditory damage that can occur even when thresholds remain within the clinically normal range. Second, it highlights that small or even subclinical changes in hearing sensitivity—especially when paired with a history of noise or blast exposure—can have real-world functional consequences.
In other words, a person might “pass” their hearing test but still struggle in complex listening environments because of underlying auditory processing issues, synaptopathy, or other neural factors that aren’t detected by standard audiometry. That’s why tools like the THS-H and N₀Sπ are so valuable—they help uncover that hidden burden of hearing difficulty and provide a pathway to earlier identification and intervention. It’s a call to broaden how we define and evaluate hearing health, especially in high-risk populations like Service Members.
16. What about treatment options for these individuals?
There tends to be a historical gap in care—if your thresholds fall within the “normal” range, you’re typically told everything is fine, even if you’re struggling to understand speech or keep up with a conversation in noise. But we’re showing that those complaints are valid and treatable. We’ve found that minimal amplification for this population, often referred to as low-gain hearing aids (LGHAs), has been successful for bridging that gap.
We’ve been using the THS-H to identify individuals who report significant hearing difficulties despite normal hearing thresholds (NHT), and then tracking their outcomes after being fitted with hearing aids with low amplification and a speech in noise program.
We conducted a study including a large sample of 6652 service members undergoing their annual hearing tests and 186 individuals self-identified as hearing aid users (Davidson et al., 2024). These hearing aid users were further categorized based on their THS-H scores (significant hearing difficulties [SHD] vs. non-significant hearing difficulties [NHD]) and audiometric thresholds (normal hearing thresholds [NHT] vs. hearing impairment [HI]). This resulted in four groups: NHT/SHD (n = 13), NHT/NHD (n = 36), HI/SHD (n = 80), and HI/NHD (n = 57).
We found those with high THS-H scores—individuals reporting SHDs despite normal audiograms—showed significantly greater hearing aid usage and perceived benefit from LGHAs compared to their NHD counterparts. Importantly, the NHT/SHD group reported benefit levels comparable to those with peripheral hearing loss, demonstrating that patient-reported hearing difficulties—captured by the THS-H—can be a strong predictor of successful amplification outcomes even in the absence of audiometric hearing loss. This finding reinforces the critical importance of listening to the patient’s experience, not just relying on the audiogram, when considering candidacy for amplification.
Of note, full-time hearing aid use was common across all groups, regardless of peripheral hearing status. When examining reasons for seeking amplification, only 11% of individuals in the NHT/NHD group reported difficulty understanding speech in noise, compared to 39% in the NHT/SHD group—more than three times as often—further supporting the role of perceived auditory difficulties in identifying candidates likely to benefit from hearing intervention (Davidson et al., 2024). That’s a huge shift in how we conceptualize candidacy for amplification and makes a strong case for more personalized approaches to auditory care, even within “normal” limits.
17. Do you find that what’s reported in the research literature and what’s happening in clinics are sometimes out of sync?
I do, yes. There’s often a significant lag between when research findings emerge and when they’re implemented in clinical practice, but we’re actively working to bridge that gap. When it comes to fitting hearing aids in individuals with normal hearing thresholds, there’s still limited published data—beyond some key studies (Bennett, 1989; Roup et al., 2019; Mealings et al., 2024). Because of that, many clinicians, both within and outside the DOD, are understandably hesitant to fit hearing aids without measurable hearing loss, especially with concerns about reimbursement and justification. I’m hopeful though, because audiologists who see these potential LGHA patients are eager to see the results of new studies that can provide evidence-based guidelines on how these hearing aids should be fitted to provide maximum benefit. It’s my understanding that the new NAL-NL3 fitting algorithm for minimal hearing loss may be helpful in addressing this issue (NAL, 2025).
There’s a long-standing belief that hearing aids are for those with measurable loss, so when you introduce something that challenges that framework, there’s naturally going to be some resistance. But I think skepticism is healthy as it pushes us to be more rigorous in our research projects. That’s why we’ve focused so much on collecting large-scale data and publishing normative thresholds with tools like the THS-H. Our goal is to provide clear, actionable benchmarks that help clinicians feel more confident when considering these kinds of interventions.
18. What questions still remain about who benefits most from low-gain hearing aids, and how do you plan to address them in future research?
One question that still remains about who benefits most from LGHAs is how a patient’s history, in addition to their self-reported hearing difficulties, influences the benefit they receive from these devices. We know that factors like temporary threshold shifts and blast exposure can impact scores on the THS-H, but the next step is to determine whether these factors also influence the level of benefit that individuals derive from LGHAs. This is an area of research we’re actively exploring right now. By combining a comprehensive understanding of a patient's hearing history with their subjective reports of difficulty, we hope to better identify the individuals who will benefit most from LGHAs and refine the criteria for their use in clinical practice.
19. It sounds like the integration between clinical care and research is really well-oiled at Walter Reed?
I think one of the biggest factors is how collaborative the environment is here. In my experience, many university labs tend to be somewhat stove-piped, where individuals are assigned to a particular research project or grant. At Walter Reed, everyone is involved in everything and all of our researchers collaborate across projects. Most of our publications have multiple authors from within our section because we’re all bringing different perspectives to the table—whether it’s audiology, engineering, cognition, psychoacoustics, cochlear implants, or speech-language pathology. That cross-pollination of expertise makes the science stronger and helps us tackle problems in a more comprehensive way. It also makes it a really fun and intellectually engaging place to work.
20. Looking ahead, are there areas of audiology you think are ripe for new breakthroughs—or things you’re hoping to dig into next?
As we look ahead, I believe we’re going to see significant advancements in how we approach audiology, particularly with the integration of more nuanced, personalized treatment strategies. The future will likely see an increasing focus on combining traditional audiometric testing with a deeper understanding of a patient's hearing history, including noise exposure and temporary threshold shifts. This personalized approach, particularly with tools like the THS-H, will help us better identify patients who may benefit from treatments like hearing aids, even when their audiograms appear normal.
For clinicians, one key takeaway would be to start or continue looking beyond the audiogram. Hearing difficulties don’t always correlate with hearing loss in the standard frequency range, and we need to be more attuned to the broader picture—such as the patient's history, their self-reported symptoms, and how they perform in different listening environments. Testing auditory abilities such as speech-in-noise performance, temporal processing, and utilizing tools like N₀Sπ will be vital in understanding the complexities of auditory function.
I also anticipate that we’ll continue to see more technological advancements, including further refinements in hearing aid fitting algorithms and perhaps even the integration of machine learning to help us predict who will benefit most from specific interventions. The challenge will be ensuring that we’re continually collecting robust, real-world data and using that to inform clinical practice.
References
Bennett, C. D. (1989). Hearing aid use with minimal high‐frequency hearing loss. Otolaryngology–Head and Neck Surgery, 100(2), 154–157. https://doi.org/10.1177/019459988910000207
Bentler, R. A., Niebuhr, D. P., Getta, J. P., & Anderson, C. V. (1993). Longitudinal study of hearing aid effectiveness. II: Subjective measures. Journal of Speech, Language, and Hearing Research, 36(4), 820–831. https://doi.org/10.1044/jshr.3604.820
Brungart, D. S., Sheffield, B. M., Galloza, H., Schurman, J. R., Russell, S., Barrett, M. E., ... & Heil, T. (2023). Developing an evidence-based military auditory fitness-for-duty standard based on the 80-word Modified Rhyme Test. Ear and Hearing, 44(1), 209–222. https://doi.org/10.1097/AUD.0000000000001257
Davidson, A., Eitel, M., Lange, R. T., French, L. M., Lippa, S., Brickell, T. A., & Brungart, D. (2023). Efficient estimation of the binaural masking level difference using a technique based on manual audiometry. Journal of Speech, Language, and Hearing Research, 66(4), 1378–1393. https://doi.org/10.1044/2022_JSLHR-22-00313
Davidson, A. J., Ellis, G. M., Jenkins, K., Kokx-Ryan, M., & Brungart, D. S. (2024, March). Examining the use and benefits of low-/mild-gain hearing aids in service members with normal hearing thresholds and self-reported hearing difficulties. Healthcare, 12(5), 578. https://doi.org/10.3390/healthcare12050578
Davidson, A., Ellis, G., Rallapalli, V., & Brungart, D. (in press). Exploring auditory processing abilities and the impact on response time and hearing aid benefit. Perspectives of the ASHA Special Interest Groups.
Davidson, A., Ellis, G., Sherlock, L. P., Schurman, J., & Brungart, D. (2023). Rapid assessment of subjective hearing complaints with a modified version of the Tinnitus and Hearing Survey. Trends in Hearing, 27, 23312165231198374. https://doi.org/10.1177/23312165231198374
Davidson, A., Marrone, N., Wong, B., & Musiek, F. (2021). Predicting hearing aid satisfaction in adults: A systematic review of speech-in-noise tests and other behavioral measures. Ear and Hearing, 42(6), 1485–1498. https://doi.org/10.1097/AUD.0000000000001032
Davidson, A., Musiek, F., Fisher, J. M., & Marrone, N. (2021). Investigating the role of auditory processing abilities in long-term self-reported hearing aid outcomes among adults age 60+ years. Journal of the American Academy of Audiology, 32(7), 405–419. https://doi.org/10.1055/s-0041-1731007
Davidson, A., & Souza, P. (2024). Relationships between auditory processing and cognitive abilities in adults: A systematic review. Journal of Speech, Language, and Hearing Research, 67(1), 296–345. https://doi.org/10.1044/2023_JSLHR-23-00224
DVIDS. (2024). MHSRS 2024: Dr. Alyssa Davidson. Defense Health Agency. Retrieved from https://www.7atc.army.mil/Media-News/Video/videoid/934415/dvpTag/MHSRS/
Feng, Y., Yin, S., Kiefte, M., & Wang, J. (2010). Temporal resolution in regions of normal hearing and speech perception in noise for adults with sloping high-frequency hearing loss. Ear and Hearing, 31(1), 115–125. https://doi.org/10.1097/AUD.0b013e3181b0dbb1
Grant, K. W., Kubli, L. R., Phatak, S. A., Galloza, H., & Brungart, D. S. (2021). Estimated prevalence of functional hearing difficulties in blast-exposed service members with normal to near–normal-hearing thresholds. Ear and Hearing, 42(6), 1615–1626. https://doi.org/10.1097/AUD.0000000000001062
Hayes, D., Jerger, J., Taff, J., & Barber, B. (1983). Relation between aided synthetic sentence identification scores and hearing aid user satisfaction. Ear and Hearing, 4(3), 158–161. https://doi.org/10.1097/00003446-198305000-00006
Henry, J. A., Griest, S., Zaugg, T. L., Thielman, E., Kaelin, C., Galvez, G., & Carlson, K. F. (2015). Tinnitus and hearing survey: A screening tool to differentiate bothersome tinnitus from hearing difficulties. American Journal of Audiology, 24(1), 66–77. https://doi.org/10.1044/2015_AJA-14-0042
Kumar, U. A., Ameenudin, S., & Sangamanatha, A. V. (2012). Temporal and speech processing skills in normal hearing individuals exposed to occupational noise. Noise and Health, 14(58), 100–105. https://doi.org/10.4103/1463-1741.99893
Kwak, M. Y., Choi, W. R., Park, J. W., Hwang, E. J., Ha, Y. R., Chung, J. W., & Kang, W. S. (2020). Assessment of objective audiometry to predict subjective satisfaction in patients with hearing aids. Clinical and Experimental Otorhinolaryngology, 13(2), 141–147. https://doi.org/10.21053/ceo.2019.00942
Mantello, E. B., da Silva, C. D., Massuda, E. T., Hyppolito, M. A., & Dos Reis, A. C. M. B. (2016). Relationship between speech perception and level of satisfaction of hearing aid users. International Archives of Otorhinolaryngology, 20(4), 315–320. https://doi.org/10.1055/s-0036-1584292
Mealings, K., Valderrama, J. T., Mejia, J., Yeend, I., Beach, E. F., & Edwards, B. (2024). Hearing aids reduce self-perceived difficulties in noise for listeners with normal audiograms. Ear and Hearing, 45(1), 151–163. https://doi.org/10.1097/AUD.0000000000001344
Meister, H., Rählmann, S., Walger, M., Margolf-Hackl, S., & Kießling, J. (2015). Hearing aid fitting in older persons with hearing impairment: The influence of cognitive function, age, and hearing loss on hearing aid benefit. Clinical Interventions in Aging, 10, 435–443. https://doi.org/10.2147/CIA.S77029
Musiek, F. E., Shinn, J., Chermak, G. D., & Bamiou, D. E. (2017). Perspectives on the pure-tone audiogram. Journal of the American Academy of Audiology, 28(7), 655–671. https://doi.org/10.3766/jaaa.16057
Musiek, F. E., Shinn, J. B., Jirsa, R., Bamiou, D. E., Baran, J. A., & Zaida, E. (2005). GIN (Gaps-In-Noise) test performance in subjects with confirmed central auditory nervous system involvement. Ear and Hearing, 26(6), 608–618. https://doi.org/10.1097/01.aud.0000188069.80699.41
Nair, P. G., & Basheer, B. M. (2017). Influence of temporal resolution skills in speech discrimination abilities of older subjects. Acta Otorhinolaryngologica Italica, 37(1), 58. https://doi.org/10.14639/0392-100X-493
National Acoustics Laboratories (NAL). (2025). NAL-NL3: The next generation fitting system. Retrieved from https://www.nal.gov.au/nal_products/nal-nl3-the-next-generation-fitting-system/
Ng, E. H. N., Rudner, M., Lunner, T., & Rönnberg, J. (2013). Relationships between self-report and cognitive measures of hearing aid outcome. Speech, Language and Hearing, 16(4), 197–207. https://doi.org/10.1179/2050572813Y.0000000015
Perez, E., McCormack, A., & Edmonds, B. A. (2014). Sensitivity to temporal fine structure and hearing-aid outcomes in older adults. Frontiers in Neuroscience, 8, 7. https://doi.org/10.3389/fnins.2014.00007
Ricketts, T. A., Bentler, R., & Mueller, H. G. (2019). Essentials of modern hearing aids (1st ed.). Plural Publishing.
Roup, C. M., Post, E., & Lewis, J. (2018). Mild-gain hearing aids as a treatment for adults with self-reported hearing difficulties. Journal of the American Academy of Audiology, 29(6), 477–494. https://doi.org/10.3766/jaaa.16134
Thorup, N., Santurette, S., Jørgensen, S., Kjærbøl, E., Dau, T., & Friis, M. (2016). Auditory profiling and hearing-aid satisfaction in hearing-aid candidates. Danish Medical Journal, 63(10), A5275.
Walden, T. C., & Walden, B. E. (2004). Predicting success with hearing aids in everyday living. Journal of the American Academy of Audiology, 15(5), 342–352.
Wilson, R. H., Moncrieff, D. W., Townsend, E. A., & Pillion, A. L. (2003). Development of a 500-Hz masking-level difference protocol for clinic use. Journal of the American Academy of Audiology, 14(1), 1–8. https://doi.org/10.3766/jaaa.14.1.1
Citation
Davidson, A. (2025). 20Q: Emerging Research - normal audiograms, real-world struggles, and innovative interventions. AudiologyOnline, Article 29319. Available at www.audiologyonline.com


