Editor's Note: This is part of a series of six expert seminar presentations and articles on the human side of the fitting process. This series is being presented throughout 2009, and is designed to walk through the hearing aid fitting process from beginning to end with a focus on the human factors that are at play each step along the way. Tools and strategies will be discussed that can assist in ensuring that the patient receives the optimal benefit from modern hearing aid technology. It is designed to be a complement to more typical discussions of hearing aid technology and fitting verification. Please see the accompanying recorded seminar on this topic in the AudiologyOnline eLearning library. Further courses in this series, "Managing Patient Expectations" and "Motivating the Older Patient to Take Action" can also be found as recorded and text-based courses in the AudiologyOnline eLearning library. Look for upcoming live courses in this series - Special Fitting Considerations, the Fine Tuning Process, and the Follow-up Process - that will be presented on 9/11/09, 10/30/09 and 12/4/09. Further details can be found in the AudiologyOnline course listings.
Millions of people are fit with hearing aids every year worldwide. As a field, we have adopted a strategy by which we try to standardize fitting approaches. Further, we base this standardization using a predictive model. We measure relevant audiometric information from patients, use standardized predictive formulas to set the amplification characteristics, verify that the hearing aids provide the intended acoustic response, and then "fix" any problems that arise in follow-up.
Although this theoretically is an efficient approach, it relies on our predictions being highly accurate. The unfortunate reality is that a large number of fittings have to be adjusted after the fact. Even if we are extremely accurate from an acoustic standpoint as indicated by real-ear measures, there are many patients for which a precise target match is simply not acceptable. The problem for many patients has nothing to do with how precise we are. Rather, there is a more fundamental issue: the assumptions that form the basis of modern fitting approaches may simply not be relevant for every individual patient. Maybe not all people want to hear things in the same way.
Does that mean acoustic verification of a match to target using real-ear techniques is irrelevant? Absolutely not. Achieving an accurate acoustic match to prescribed targets is simply good practice as it provides correction for any unusual acoustic variances from the mean. However, verification of a match to target is only the beginning of the fitting process, not the end (Sweetow, 2000). Once the acoustic accuracy of the fit is assured, the process then switches from an objective acoustic exercise to a subjective patient-driven one. After acoustic verification, the issues becomes determining if the prescribed target meets the individual perceptual needs and/or preferences of the patient.
Essentially all fitting rationales, whether independent (like NAL-NL1 or DSL 5.0) or manufacturer specific, use a combination of speech audibility maximization along with loudness perception predictions to determine prescribed gain values across frequency and input level (Kuk, 2000). Loudness perception is, in practice, typically predicted based on hearing threshold levels (HTLs). The underlying assumptions are that the hearing aid user wants to hear a broad range of speech inputs at loudness levels that are acceptable and (in some approaches) similar to normal-hearing individuals. The implementation details vary from approach to approach. What is not specified or accounted for are the following factors, among others:
- Individual differences in spectral balance preferences (more or less bass or treble)
- Individual differences in the loudness/audibility trade-off (some patients will tolerate higher loudness levels in order to maximize audibility, some will sacrifice audibility for the sake of lower on-going loudness levels)
- Individual variation from predicted loudness perception patterns (unless supra-threshold perception is specifically measured for each patient)
- Individual differences in the time course of adaptation to the higher levels or extended bandwidth of amplified sound (especially in the case of first time users)
- Individual preferences for what is the primary signal of interest (speech, music, nature, ambience, etc.)
- Individual differences in the core psychoacoustic integrity of the auditory system (some auditory systems cannot make full use of clean amplified speech due to a high level of peripheral distortion)
- Individual differences in the cognitive processing of speech information (audibility of speech does not guarantee that all listeners can extract information at the speed and complexity that the speech is presented)
- The dynamic behavior of environmentally adaptive systems such as noise reduction, automatic directionality, automatic program changes, etc. (some patients prefer to hear advanced technology in action whereas others prefer a subtle, "behind-the-scenes" approach)
It is clear that we are limited in how much we can specify about a fitting ahead of time. Our clinical processes favor predictive fittings, yet we spend significant clinical time in follow-up sessions with patients in order to find solutions to their sound quality, loudness, speech clarity or performance in noise concerns. There are a broad array of person-based variations in sound perception and preference and a broad array of available flexibility in modern amplification. The map between these two is not well described. Fortunately, over the past decade, we have seen important developments in fitting tools and clinical approaches that enable us to better match technology to the individual needs and preferences of our patients.
The Nature of Fine Tuning
Fine tuning is an extremely important clinical skill for the audiologists. As new hearing aid technology develops, new adjustment skills need to be developed at the same time. However, there are constraints on how much we can expect fine tuning to solve all patient follow-up issues.
- Fine tuning is a patient-driven process based on subjective preferences for how amplified signals should sound. If the audiologist allows the patient to direct how the devices should be set (as, of course, they should) then the prescribed targets no longer matter. There are plenty of reasons why patients may want a sound quality out of a device that differs from what the chosen target will call for. The audiologist either has to accept that this is a patient-driven process or stick to the targets. Trying to do both will inevitably muddle the fine tuning process. As long as good fine tuning practice is used, the audiologist needs to trust that the patient knows what sounds right.
- First time users of amplification may not be able to give realistic direction to the fine tuning process from the start. They simply have no experience with amplified sound and will tend to direct fine tuning back to make the new devices sound like their norm, unamplified sound. The new user needs to be taken through an adaptation period before being able to effectively provide feedback on preferences for amplified sound.
- Managing the adaptation process for the new user is particularly important. If a first time user drives the gain values down at the initial fitting because amplified sound is overwhelming, later in the process the natural tendency for the professional is to not try to bring those levels back up if the patient is not reporting problems, leading to the potential loss of additional benefit from the devices.
- The audiologist needs to differentiate between patient complaints versus patient reports. Before any fine tuning changes are made, it is essential to investigate whether or not a change is truly needed. There are times when a patient may describe a setting or situation where the sound of the hearing aids was not optimal. Before changes are made, it is important to determine how serious an issue this was for the patient and what other factors may have been involved. Fine tuning is important but should not be a response to everything a patient reports.
- One of the reasons why careful patient questioning is important is that solutions may be specific to one sound or setting. A fine tuning adjustment that solves one problem may create new problems in other settings. Prioritizing the issues that the patient has and explaining the potential implications of fine tuning to the patient will help in making only truly necessary changes.
- The simple reality is that in modern hearing aids there are too many dimensions to fully investigate during fine tuning, especially when you consider the possible combinations of settings. Patients may believe that they can find the perfect combination of settings. The audiologist needs to be able to manage the process so that the goal is to find an acceptable combination of settings as opposed to "the ultimate".
Controlling Flexibility
With the advent of programmable and, more recently, digital technologies, vast new dimensions of device performance have become available. With just a handful of independent technical dimensions, thousands of permutations are possible. In this regard, one could argue technology has clearly outpaced our understanding of the outcomes and interactions of multiple, independent technical manipulations. In fact, little is known regarding the perceptual consequences of dynamic changes along multiple dimensions, and/or the concomitant interaction between dimensions.
Some manufacturers of hearing aids have taken on the responsibility to provide guidance regarding the outcome and interaction of programming changes made on advanced technology dimensions. One approach has been to create intelligent master adjustment handles, referred to as Meta Controls. Meta Controls combine a variety of background technical parameters in the setting of the device into a control that will usually have more of an operational, qualitative name and effect. Patients tend to have global, qualitative descriptors for device performance, for example;too loud, too quiet, too tinny, not sharp enough, etc. When properly engineered and implemented, Meta Controls should have the ability to effectively address such qualitative reports from patients.
Meta Controls have been used to perform a variety of tasks. For example, Meta Controls have been developed to handle patient-based reports such as loudness concerns, tonal balance, etc. Some manufacturers use a Meta Control to manage adaptation to amplification for the first time user. These controls provide gradual, discrete changes on dimensions such as attack time, gain, compression ratio and frequency response. In the Oticon application called Adaptation Manager (Schum, 2001), as the patient progresses from Step 1 to Step 3, gradual changes across these parameters allow the patient to adapt to amplified sound over several weeks, culminating in Step 3, which provides the fully prescribed settings for the product. Although most new users will start with Step 1, experienced users may start with Step 2, while others will go directly to Step 3, depending on their amplification experience and needs.
Schum (1997) reported that prior to implementation of the Adaptation Manager, nearly half (46%) of new users fit with a new advanced technology hearing aid (that implemented a new, proprietary fitting rationale) requested a decrease in amplification. Only 33% of the users accepted the prescribed settings at the initial fitting.
Following implementation of the Adaptation Manager in advanced technology products, new users accepted the final prescribed settings of the same device more readily if they adapted at a slower, prescribed pace over the course of several weeks (Schum, 2001). Figure 1 provides the average deviation from prescribed gain settings across the seven channels of a device 6 weeks after being fit using the Adaptation Manager. Notice the average deviation is within 1 - 3 dB of the prescribed settings. These findings verified the accuracy of the new fitting rationale, yet only after the adjustment period, confirming the importance of fitting new users with an adaptation strategy.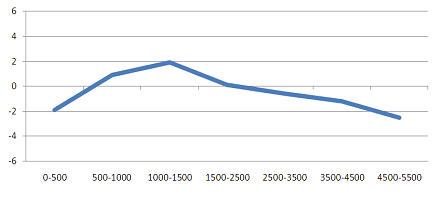
Figure 1. The difference between actual and prescribed settings for a group of new hearing aid users who were fit using the Adaptation Manager (adapted from Schum, 2001). The x-axis is frequency and the y-axis is dB difference from prescribed setting.
While data from Schum (2001) show that most new users need the full effect, application of adaptation management needs to be determined on an individual patient basis. The time course over which the patient can be moved to fully prescribed settings will vary from as little as one to two weeks to a month. Not all patients will be able to accept the fully prescribed settings no matter how much time is given as they may have a loudness preference that falls below the level of the final setting in the planned sequence.
Cross-system Controls
The last several years have seen the introduction of a multitude of effective environmentally adaptive features in hearing aids. Noise reduction circuitry analyzes the incoming signal and provides comfort-based attenuation without appreciable degradation of important speech sounds, to make devices more acceptable in noisy environments. Automatic adaptive directionality analyzes the acoustic landscape within the patient's environment and shifts to an appropriate directional mode to improve the signal-to-noise ratio provided to the user.
When implementing environmentally adaptive features in advanced technology digital hearing aids, two approaches can be taken:
- The environmentally adaptive hearing aid can slowly and subtly adapt itself to changes in the acoustic environment. For example, as the sound characteristics change, the hearing aid realigns itself to be a more appropriate signal processor for that given acoustic environment, maximizing the signal-to-noise ratio, while assuring optimum sound quality and comfort.
- The environmentally adaptive hearing aid can aggressively adapt itself to changes in the acoustic environment. For example, as the sound characteristics change, directionality, noise reduction and compression are immediately altered to inundate the listener with as many potentially relevant speech cues as possible at each given moment in time.
Unfortunately, potential negative and unpredicted interactions are possible as the professional adjusts the characteristics of one or more individual subsystems. For example, if activation times of the noise management system are adjusted to be rapid, yet the compression or adaptive directional system is set for a more gradual response here can be an unexpected corruption of the signal.
One example of cross-system control is the concept of "Identities" (Oticon, 2004). An Identity is a discrete group of settings, from a broad range of potential device dimensions, designed to operate synergistically and appropriately to create a well defined overall sound processing strategy. Parameters which impact device performance, and are addressed within the Identities are:
- speed of adaptation of polar plots
- speed of changing between directional modes
- speed of application of gain reductions by noise reduction systems
- amount of gain reduction in the in noise reduction modes
- amount of gain for soft sounds
- frequency response shape
- compression attack and release times
- compression ratios
When fitting or adjusting products that feature Identities, the audiologist can select from up to five options: calm, gradual, active, dynamic and energetic. Each Identity represents a unique combination of parameters and settings.
In general, when moving from one end of the Identities continuum to the other, the speed and amount of reaction to variations in the acoustic environment will change. On one end of the continuum (for example, "Calm"), the instrument will have a subtle and slowly adapting reaction to a change in the characteristics of the listening environment. On the other end of the continuum (for example, "Energetic"), the instrument will have a rapid and more aggressive response to changes in the acoustic environment.
The concept of device Identity was developed to responsibly manage ever-increasing device complexity. As hearing instruments continue to include more and more advanced signal processing options, there is an increased responsibility to make changes based on predictable and logical combinations of settings. Some patients may prefer or perform better with a more aggressive approach, whereas others may prefer or perform better with a more subtle approach.
Other manufacturers will achieve cross-system control in other ways. For example, in one approach, hearing aids are designed to switch memories automatically based on an assessment of the sound environment. One memory will set the gain, compression, noise reduction and directionality for quieter environments and another memory will have a combination of settings appropriate for noisier conditions.
The Value of Individualization
Flynn and Lunner (2004) report on 33 patients who were tested in a verification study of the cross-system control. The 33 participants were distributed across the three possible prescribed Identities: 11 were prescribed Dynamic, 14 were prescribed Active, and 8 were prescribed Gradual. The prescribed Identities were based on a combination of patient age, experience with amplification, sound preference.
To determine accuracy of the Identity prescriptions, patients were allowed to adapt to their original prescribed identity. After that, they were given 2-3 weeks to use both a more aggressive and less aggressive Identity. Following exposure and experience with all three alternative Identities, they were asked to indicate their preference. Results are shown in Figure 2.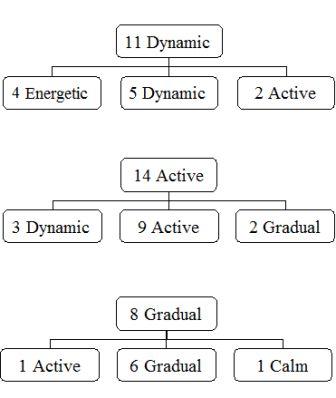
Figure 2. Distribution of patients comparing the prescribed and selected Identity (adapted from Flynn and Lunner, 2004).
Twenty of the 33 participants (61%) chose the prescribed Identity. Across the three prescribed starting Identities, there is an approximately even distribution for those choosing more stable option or more aggressive options.
These data indicate three important aspects of Identity-based prescription:
- Patients can distinguish between Identities. The data from these subjects and from other reports indicate that 75 to 80% of patients can clearly hear one step differences;a change of two identity steps is clearly audible to all patients.
- The criteria that was used to select the prescribed Identity (patient age, experience with amplification, sound preference) appears to be accurate most of the time. When given two other options, patients chose the prescribed option 61% of the time.
- A significant minority of patients chose an alternative Identity which was evenly distributed between more stable or more aggressive alternatives, which justifies the need to be able to customize the setting. The general accuracy of the prescription process is supported, but the need to quickly and efficiently offer alternatives is also indicated.
Fine Tuning and Cross-system Controls in Follow-up
Finding the right combination of settings in follow-up is not a simple task. With the addition of cross-system controls to the toolbox, audiologists need a strategy to incorporate these important new options. The following observation may help in approaching the follow-up process.
First, when deciding to handle a user complaint using fine tuning compared to an adjustment of a cross-system control, consider the specificity of the patient report. If the report refers to a specific sound, event, need or setting, fine tuning should be able to address the problem. In other words, traditional fine tuning approaches work well at addressing problems such as "door slams are too loud" or "speech is not clear enough". If the report is vague or global, or if the report relates to the dynamic behavior of the device, then consider adjustments to cross-system controls. Examples would be reports such as "I just don't do well in noisy rooms" or "my hearing aids seem to be changing all of the time and that bothers me".
Second, when addressing issues via fine tuning, most manufacturers provide a choice of gain adjustment in each specific channel (8, 12, 16 or more) or in frequency regions (typically low, mid and high). Patients rarely report a bothersome sound that can be isolated to a narrow frequency channel. Nearly all sounds encountered in daily live will be reasonably broad band. Therefore, consider using individual channels to adjust for something you see in the real-ear response. Use the broader frequency regions to adjust for something the patient says.
Also, when fine tuning, consider the quadrant or 3x3 (Sweetow, 2000) approaches. That is, try and isolate the problem into one or more frequency and input level areas. For example, a patient report that "speech is too soft" or "speech sounds too distant" tends to relate to soft gain across frequency. The report that "loud environments are too loud" is probably best addressed by loud (and perhaps moderate) gain adjustments. Speech not being clear enough, especially in noise, relates to mid and high frequencies for moderate (and perhaps) loud gain values.
Finally, when adjusting cross-system controls, remember that the patient will not likely be able to judge the effect of those adjustments in the clinic environment. The effectiveness of such changes can only legitimately be evaluated in use in everyday environments.
Final Thoughts
Sensorineural hearing loss affects each patient differently;every patient's auditory system responds to the physiological changes brought about by the loss in a unique way. Cognitive performance varies significantly from patient to patient. Listening preferences vary widely across hearing aid users. It is naïve to believe that one combination of settings on dimensions such as gain, compression, adaptive directional behavior and noise management will be right for all users. Advanced digital devices, with a broad range of effective environmentally adaptive features have the potential to offer the patient information-laden, high quality amplified sound. For maximum benefit to be achieved, it must match the individual needs and preferences of the recipient.
References
Flynn, M. & Lunner, T. (2004). Clinical evidence for the benefits of Oticon Syncro. Oticon White Paper. September.
Kuk, F. (2000). Recent approaches to fitting nonlinear hearing aids. In M. Valente, H. Hosford-Dunn & R. Roeser (Eds.), Audiology treatment (pp. 261 - 289). NewYork: Thieme Medical Publishers.
Oticon (2004). The Syncro Handbook.
Schum, D. (1997). Field evaluation of the Adaptive Speech Alignment fitting rationale. News from Oticon.
Schum, D. (2001). Adaptation management for amplification. Seminars in Hearing, 22(2), 173-182.
Sweetow, R. (2000). Selection and fitting of programmable and digital hearing aids. In M. Valente, H. Hosford-Dunn & R. Roeser (Eds.), Audiology treatment (pp. 433 - 458). NewYork: Thieme Medical Publishers.


