Editor’s Note: This text course is an edited transcript of a live webinar. Download supplemental course materials.
Learning Objectives
Dr. Lindsay Prusick: Upon completion of this course, attendees will be able to explain neuroplasticity and the positive impacts cognitive exercises and activity engagement can have on the aging brain. Attendees will be able to discuss the relationship between cognition and the auditory system and the implications of hearing loss on this relationship. Finally, attendees will be able to identify the potential positive effects of auditory training for individuals who have both normal or impaired hearing.
Introduction
I would like to start by telling you about some exceptional people. First is Professor Heinz Wenderoth, who at the age of 97 was awarded a doctorate in Science. Next is Gladys “the Gladyator” Burrill, who at 92 years of age ran a marathon. Third is Dr. Leila Denmark who served as a pediatrician until her retirement at the age of 103 years old. Finally, we have Olive Riley, who, up until the age of 108 years old, had an active blog which she kindly referred to as “The Blob.”
What do all of these individuals have in common? Your first thought may be each of these individuals is a bit old, but they are also quite extraordinary. Each of these individuals kept learning something new and took on challenges regardless of their age, and they were successful. How was this possible? Are not later decades of life generally associated with cognitive decline?
Cognitive Skills and Aging
Dr. Jumana Harianawala: The brain begins to experience age-related functional changes and starts to slowly decline as early as 20 to 30 years of age. Basically, as we age, our brain becomes increasingly less efficient. Let’s consider a few of these cognitive skills.
Intelligence, for example, is preserved when crystalized. In other words, knowledge and experiences that accumulated over time remain stable, but abilities that are newly acquired remain fluid and are not well-preserved. Memory of past events that have been stored over many years remains relatively preserved in old age, while recent memory or the formation of new memory is more vulnerable to aging.
Focused attention, such as the ability to attend to a TV program, tends to be preserved in older age. Difficulties may be encountered, however, when divided attention is required such as trying to pay attention to TV and simultaneously talking on the phone. Verbal abilities, including vocabulary, are preserved, and in some cases enhance, as we age. However, word retrieval or the process of getting the words out is difficult. The information is not lost, but it takes longer to retrieve.
Traditional ways of approaching solutions are maintained in older people. Something that they have done and experienced is easier to problem solve again. New problems that have not been encountered may take some extra time to figure out. One of the processes that is most affected by aging is the speed of processing. This does not mean that activities cannot be performed, but they tend to take longer.
A common misconception is that all is downhill with aging, or that the loss of cognitive abilities is inevitable and extensive. Research does not support this claim entirely. Studies have demonstrated that certain skills decline as we age, but some others remain stable. Further, what makes this area of cognitive aging so interesting is that these declines do not affect all individuals equally.
Variability
There is variability in cognitive abilities. Some older adults show pronounced cognitive deficits and other perform as well or better than younger adults. You may be wondering why this happens. Like everything else, a number of factors are involved. Medications, for example, might produce side effects such as drowsiness and mental dullness. Sensory changes could interfere with processing of information. For example, a hearing loss might affect a person’s ability to hear their name being called out when they are introduced. Health-related changes like arthritis and pain could affect cognitive areas such as concentration and processing speed. Finally, changes in mood such as depression and anxiety could alter one’s motivation to learn new information and apply these strategies.
The individuals that Lindsay introduced continued to take on new challenges and learn new information despite aging. How is that possible if cognitive decline is inevitable and extensive?
Neuroplasticity
Dr. Lindsay Prusick: The reason why people can continue to do exceptional things into the later decades of life is because of neuroplasticity. Neuroplasticity is the lifelong capability of the brain to change and rewire itself in response to the stimulation that comes with learning, experience, and training.
Neuroplasticity varies by age. While plasticity does occur over the lifetime, certain types of changes are more predominant during specific ages. A good example of this is cochlear implantation. We know via the research over the last 20 to 25 years that when very young children are implanted, they are far more receptive to the electrical cochlear simulation than older children or adults.
Plasticity is ongoing throughout the lifetime, but there are things that are involved aside from the brain, such as other neurons and cells, that are impacted by this neuroplasticity and can have implications for health. A great example is someone who has a healthier heart and vascular process; they will be more plastic than those who have vascular disease. Environment plays a role also, as do genetics. There are variables that will impact neuroplasticity that we have to keep in mind.
Neuroplasticity can occur for two different reasons: a result of learning, experience and memory formation or as a result of damage to the brain. Functional neuroplasticity is the brain’s ability to move functions from a damaged area of the brain to other undamaged areas. Those are more physiological changes. Structural neuroplasticity is the brain’s ability to change its physical structure as a result of learning and training. This is more of an anatomical change. I will give you some examples of neuroplasticity in action, starting with an example of a functional neuroplasticity study that was done on Macaque monkeys.
Functional Neuroplasticity
Studies done by Merzenich and colleagues (1983a; 1983b) took the median nerve of a monkey’s hand and cut it. The median nerve delivers sensation to the middle of the hand. They wanted to see what would happen to the corresponding area of the brain where activation occurred after severing that nerve. The assumption was that once the nerve was cut, the corresponding area in the brain would be rendered silent and unused due to that lack of sensory input. Two months after they cut this nerve, the researchers found when they provided sensation to the middle of the hand, no activity was recorded in the brain.
They found that when the sides of the monkey’s hand were touched, there was activity in the brain where the median nerve stimulation used to take place. This showed them that cortical remapping had occurred. Basically, the nerves that correlated to the outside of the monkey’s hand had remapped themselves to take over that area of the brain that would have been rendered inactive. This was a huge finding in neuroscience and was a demonstration of functional neuroplasticity.
Structural Neuroplasticity
A study that highlights structural neuroplasticity is from Maguire and colleagues (2006). They found that when comparing London taxi drivers to London bus drivers, the taxi drivers had larger hippocampus regions. The reason why they hypothesized this finding was that London taxi drivers have to navigate around very complex roadways. When you compare London taxi drivers’ needed knowledge to the bus drivers’ knowledge, the bus drivers have very specific routes that they adhere to, thus requiring less city knowledge. The researchers hypothesized that since the taxi drivers constantly have to navigate a great deal of space and maintain information in their short- and long-term memory that this accounted for their larger hippocampus. The hippocampus is the area where the consolidation of information from short-term memory to long-term memory takes place; it is the area responsible for spatial navigation. To put this hypothesis to the test, they did a study that compared taxi drivers about to enter training to control groups of non-taxi drivers.
Prior to the new taxi drivers starting training, the researchers administered some brain scans where they looked at the intensity (gray matter) of the hippocampus region relative to the control group. They did these scans both pre- and post-training. It is important to note that these taxi drivers go through about three to four years of training before they can ever set out on the London streets professionally. Those who successfully completed the training versus those who did not or the control groups had a statistically significant increase in the gray matter in the hippocampus region. This is an example of structural changes that took place in the brain as a result of training and experience. This is very clear evidence demonstrating the brain’s capability to change. So how can we leverage this finding for individuals with hearing loss?
Neuroplasticity and the Auditory System
Dr. Jumana Harianawala: Before I answer this question, let’s revisit cognition. Cognition consists of various processes like learning, memory, perception, and attention. Just like the other three, perception plays a very important role in cognition, and our senses act as a vehicle for perception. There is a relationship between hearing and cognition.
Cognition
Let’s take a look at what exactly that relationship is. This is a remarkable process where, through experience, our brain seamlessly perceives and interprets sounds. When listening conditions are favorable, in the case of normal hearing or with little to no noise in the environment, the input can be readily and easily matched to our phonological representation in our long-term memory. This processing is automatic and implicit. You do not even have to think about it in order for understanding to occur.
For example, if you hear the sound /sh/, you have a very clear representation of the sound in your long-term memory; therefore, you will instantaneously recognize this sound. However, what happens when this remarkable ability is compromised? There is a mismatch between the incoming message and what your long-term memory has stored. A mismatch can occur because the listening conditions are challenging, there is too much noise in the environment, a hearing loss may exist, or there may be a poor phonological representation, which is known to happen in cases of long-term hearing loss.
When we can no longer have seamless processing, we may have to use other resources like working memory to hold the information temporarily while we resolve this mismatch. Now the processing becomes explicit. It is no longer straightforward. There is an increase in demand on our resources to process this new information and to resolve this mismatch. This sometimes can occur at the expense of compromising some other tasks, because those resources may be being used to resolve this mismatch. We have all experienced a mismatch.
In an environment like this, word recognition is bound to suffer, irrespective of hearing loss; whether we have normal hearing or hearing impairment, we will have a difficult time understanding speech. However, in environments where there is no competing noise and the conversational partner and context are familiar, all of us will perform just fine, especially a hearing-impaired person, if we have provided them with appropriate amplification.
It is situations like these when the noise is not loud enough to completely mask the speech, but is enough to make the speech difficult to understand that we see differences in the effort needed to understand speech between individuals who have preserved versus poor cognitive function.
Young vs. Old
A number of studies that have evaluated the performance of older adults versus younger adults for perceptual and cognitive measures. Interestingly, researchers have found that older brains reveal the same level of performance as younger brains. However, the difference shows up in brain scans, which reveal that the brains of older people require more widespread activation in order to carry out the same tasks. Basically, older people get the same answer as younger people, but in different ways. They have to use more of their brain resources to get the right answer, revealing compensatory strategies that are being used to offset the deterioration due to aging.
Another study also determined that the difference was not only between the young and the old, but also between low- and high-performing older individuals. The results of this study showed that low-performing older adults recruited a similar network as young adults, so activation is on the same side of the brain; the low-performing older adults have a more widespread activation of the brain. This processing still tends to be inefficient. The higher performing older adults counteracted these age-related neural declines to plastic reorganization of the neurocognitive network. They split the task across different parts of the brain and achieved success.
We often hear our older hearing-impaired patients say that they cannot keep up. That is because activities that require listening effort become more demanding cognitively. Research has shown that increases in listening effort have deleterious effects on cognitive measures, especially those of comprehension and memory. Cabeza et al. (2000) found that when young and older adults are tested under the same physical stimulus condition, like speech in noise, age differences on cognitive measures are common. However, when the conditions are equated for younger and older adults, many apparent age differences on cognitive measures are minimized. This helps us understand why older individuals can perform similar to younger adults by engaging many more areas of the brain. If you are interested in pursuing this concept or learning more about this, it is worth following Cathy Pichora-Fuller, who has extensive research in this area.
We are certain that there is a relationship between cognitive skills and aging. We just heard how some of these skills begin to decline with age. We also have learned that with listening effort, cognitive skills suffer. Why does the hearing loss have an effect on cognitive skills?
Hearing Loss and Cognition
Dr. Lindsay Prusick: Before we delve into the effect hearing loss has on cognitive skills, I want you to imagine you are driving down the highway. It is a beautiful, sunny day. You have the top down and your favorite song comes on the radio. What do you do? You turn the radio up. You are jamming out and all of a sudden, you come up to an incredible amount of traffic. What is the first thing that you do? You probably reach for that knob and turn the radio down so you can better concentrate on driving. Turning the radio down does not improve your driving skills, but it does allow you the ability to allocate more resources to the task that you are faced with, such as driving into traffic.
When you add hearing loss on top of the cognitive and aging factors, it further stresses the system, especially when we are faced with demanding conditions. We are spread thin. There is certainly a relationship between hearing loss and cognition and aging. We have learned from decades of research that hearing loss further increases cognitive load. It causes fatigue. It can result in poor memory, poor auditory scene analysis, difficulty in focusing your attention and poor mental health. There has been a great deal of research in the last few years, most notably from Frank Lin and his colleagues (2013) that have shown that those with hearing loss have accelerated decline in cognitive abilities relative to those with normal hearing. That certainly has implications.
To fully appreciate the relationship between all of these cognitive factors, let’s take a moment and think about how we communicate. The communication process is quite detailed (Figure 1). In order for effective communication to take place, an individual must first be able to hear the sounds; the “listener” or “talker” must be audible to that person. Then with that information, that person has to attend. They have to be paying attention to what someone is saying to effectively receive the signal and then think about what is being said. There are also contextual cues that play into this. What if that individual is also in the presence of background noise? All these different factors play into communication and we must work our way through each of those order for that to take place.
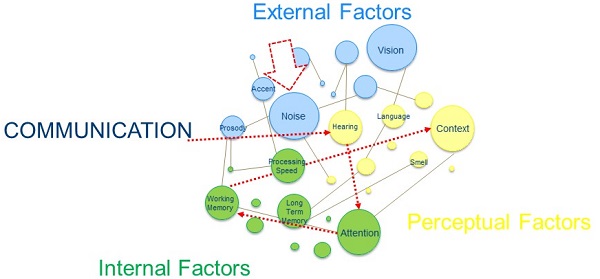
Figure 1. Various facets of effective communication.
When you step back and look at how these factors co-exist with communication, what is it that we as hearing healthcare professionals are focusing on? We are constantly honing in on the hearing piece. Remember that hearing is one small piece of that communication process. We focus a lot of our energy on a evaluating the ability for an individual to hear. We do employ some regular tests like speech-in-noise testing, which certainly increases cognitive load and is taxing to hearing systems. But overall we pay close attention to the peripheral elements of hearing, and do not fully consider the whole communication picture. We use our audiogram to decide if we are going to pursue hearing aid technology, and it is the audiogram that we use when we program hearing aids for our patients. Our rehab decisions are almost entirely based on the peripheral elements.
It is likely that this might start to change in the near future. There are a lot of researchers who are looking at other means of testing how people hear and connecting those cognitive factors so that we may be able to make more accurate rehab and counseling-based decisions for our patients. For now, let’s focus on what we use to make these decisions, which is the peripheral factors.
Hearing Evaluation
You see a patient. They have a hearing loss. What is your next step? When it comes to recommending treatment, our go-to is obviously amplification. We also tend to throw in some other accessories based on what the patient’s needs are in home and public situations. Oftentimes, we will throw in aural rehab tips to help them maximize their listening potential in a given space, such as a restaurant. These are fairly standard practices. I think this approach can be likened to the analogy shown in Figure 2.

Figure 2. Willing participant plus designer running shoes does not equal a marathon runner.
Here you see a pair Adidas Adizero Adios Boost 2 running shoes; they are regarded as the fastest shoes in the world. They are said to help marathon runners shave time off of their personal records. Mary Keitany won the New York City Marathon in a record time of 2 hours 25 minutes and 7 seconds. I could go to my local running store and buy these shoes, but simply putting on these shoes does not mean it will make me the best runner or even allow me to get a 2 hour 25 minute marathon. To be honest, I would have to train a great deal to even run a marathon. While I may be a willing participant with good shoes, those two do not make me a marathon winner. There is tremendous work involved. The same is true of our patients.
When we are providing rehabilitation to our patients, an important element of success with this process is training, specifically auditory training. Simply amplifying the sounds in our patients’ environment does not get them hearing better. Using auditory training will help them ease into their amplification and have them obtaining that benefit much sooner than they would otherwise.
Auditory Training
Dr. Jumana Harianawala: Auditory training refers to the use of formal listening activities that are specifically designed to teach the brain to listen to speech. Training could focus on specific elements of speech, for example, identifying various sounds or syllables of speech with which the person has the most difficulty. It could be presenting speech in a difficult environment or situation where people with hearing loss usually have difficulty listening, such as listening in noise in a restaurant setting. By repeatedly performing these explicit listening activities, we can train the brain to better understand and distinguish sounds and work more efficiently to comprehend speech in the most difficult listening situations.
Why auditory training is challenging, it takes advantage of neuroplasticity. Auditory training uses the brain’s ability to change and reorganize as a vehicle to teach the brain to perceive and process efficiently. Many of you have heard of LACE. LACE stands for Listening and Communication Enhancement. True to its name, it is one of the first commercially available auditory training programs that utilizes gain techniques designed to keep patients engaged while improving speech understanding performance. The program instructs and encourages the listener to recognize speech in difficult listening conditions, like speech in noise or degraded rapid speech. If you perform well, the tasks become increasingly difficult.
Sweetow and Sabes (2006) demonstrated the benefits of training with LACE on all the modules of this program. Performance in each of the categories gets increasingly better at lower SNRs as training progresses. In fact, some of the effects of this training were also seen eight weeks post training.
Research
If that is not convincing enough, Song et al. (2012) conducted a study to identify training related improvements when listening in noise. They also wanted to see the biological mechanisms mediating these improvements. They used a training program that incorporates cognitively based listening exercises to improve speech-in-noise perception. They saw improvements in speech in noise onboard the QuickSIN and the HINT test for the trained subjects over a period of time compared to the control subjects.
The trained subjects exhibited significant improvement in speech-in-noise perception over a period of time, and this improvement was also retained six months later. Not only did they see improvements in the speech-in-noise test, but they also wanted to record the auditory brainstem response (ABR) to get the biological information to see if there is a biological change.
When they recorded the ABRs to a [da] stimulus in quiet and in a six-talker babble, they found that the subcortical responses in noise were enhanced for the individuals that were trained to encode the pitch-related cues compared to the responses during pre-training. We could imagine what would have occurred in quiet or in six-talker babble after training. This study was done on a normal-hearing young adult. We know our hearing-impaired adults are nothing similar.
Anderson et al. (2013) wanted to see what happens in adults. In this study, they used older adults, some of whom were normal hearing and some of whom were hearing impaired. They first divided both groups into two and further divided the hearing-impaired group and normal-hearing group into control and experimental groups.
For the training task, they used a directed-attention paradigm where they directed attention to the speech stimulus. After training, they noted that there were positive changes in the speech processing for the group that received the training compared to the group that did not. After training, there were improvements in hearing in noise, working memory, and processing speed.
As with Song et al. (2012), Anderson and colleagues (2013) also wanted to see what happens with the biological mechanism using cortical responses. In the hearing-impaired group that received the training, there was a reduction in the cortical amplitude after the training compared to pre-auditory training. If you compare that to the hearing-impaired individuals that did not receive training or even to the normal-hearing individuals, there was a reduction in amplitude from before training, which matches more closely to the normal-hearing individuals. They noticed that there were changes in the neural representation of the speech envelope, which was presented in noise for these individuals that received training, and there were no changes in the control group.
There is good evidence for auditory and cognitive training. Why, then, are people not using it?
Gamification
Dr. Lindsay Prusick: That is a great question. When you look at the traditional methods or resources available, some people, unfortunately, have found them cumbersome. The games that have been developed do not get people excited to do them. We have seen an interesting emergence of games in the health care field that employ a technique called gamification, which is the concept of using game-thinking and design techniques for non-gaming context, like health and wellness, to engage users to solve problems or change behaviors in a fun, competitive and rewarding way. With the technology boom that we have seen over the last few years, many in the health care industry have begun to uptake this particular technique.
Gamification taps into this primitive concept that when given a reward, people are more enticed to continue with the activity. Rewards can be simple. It can be as simple as knowing you beat a friend or family member at a game or fulfilling the conquering of a new level. Depending on the game, sometimes money is at stake. The idea is that reward, whatever it may be, will keep people connected and engaged to the game, and that over time, changes will be obtained depending on whatever that game aims at. You may be familiar with Luminosity. It has the same principles of cognitive exercising in an attempt to sharpen skills.
Auditory Training
Taking into account gamification and those principles in which it is rooted, why can we not apply this to auditory training? The good news is that we can. Think of gamification as taking the hard stuff like auditory training and making it fun. There is a game that exists called ReadMyQuips. ReadMyQuips is like a crossword puzzle, except instead of a letter, each box contains a word, and the user will listen to a wise or witty saying that is referred to as the quip. Then they have to enter in what they think they heard. As skills improve, the noise level gets louder. The whole point of this game is to mimic real-life, face-to-face communication while providing a fun and enjoyable experience for the user. As they go through each of the examples, it slowly fills in a word-crossword puzzle.
This taps into a multi-tasking element. Keep in mind the user is having to selectively attend to the relevant sound or what the gentleman is saying in the presence of the background noise. They have to suppress the background noise, but also remember what the man said. This listening, remembering, and then quickly typing in those boxes is a cognitive task, not just a listening task.
You may be wondering is there any data to support this game. A pilot study done by Levitt et al. (2011) evaluated the performance of ten individuals who engaged in ReadMyQuips. They found that there were significant improvements in speech recognition. The average improvement for nine of the experienced hearing aid users was 2.8 dB. A subjective report from the users indicated that it was an enjoyable game and they did feel that their ability to hear in the presence of background noise had improved. That was a very small group of individuals that were evaluated.
Another study was done by Bock and Abrams in 2013. They included 29 new hearing aid users and looked at their engagement with ReadMyQuips versus a control group. They did a variety of pre- and post-test measures with all 29 subjects, but for the purposes of demonstrating benefit, I am going to talk about data from the HINT and the Word in Noise test.
Before I go through the data, there is one little point I want to make. The individuals who were assigned to the ReadMyQuips group were encouraged to engage in 600 minutes of ReadMyQuips during the study period. Of the 15 people who were in that group, only three or four of them met the requested amount of time to be engaging with this system. Even though all the individuals did not engage for the recommended amount of time, we still saw some great benefit.
We found a significant improvement for the ReadMyQuips group in comparison to the control group when the individuals were engaged in a static directional condition. We did see marked improvements in their HINT score when they were engaged in a directional mode. We also saw a significant improvement on the Words in Noise test for the ReadMyQuips group versus the individuals who were in the control group. It was interesting that we found this in both the unaided and aided conditions. This data demonstrates that engaging with this tool translated to improvements in hearing-in-noise tests.
I was perusing the Internet and came across an interesting study (Whitton, Hancock, & Polley, 2014) from Massachusetts Eye and Ear Institute. In this experiment, they used adult humans and mice that had normal hearing. They were trained on a rudimentary audio game that was inspired by a sensory foraging behavior, which required the individuals and the mice engaged in this task to discriminate discrete changes in loudness of a tone that was presented in moderate background noise. This game was similar to the children’s game of hot and cold. The idea was to have them seek out a very specific tone in the presence of that background noise. They were provided continuous auditory feedback. Over the course of training, both the mice and humans learned adaptive search strategies that allowed them to more efficiently convert noisy dynamic audio cues in order to find that specific target.
The reason I am presenting this to you is because we are talking about auditory training and this games piece. Interestingly, at the conclusion of the study, they evaluated the human subjects’ ability to hear in the presence of background noise. They found that the humans who engaged had a generalized improvement in the ability to understand speech in noisy conditions relative to the control group.
This does not necessarily mean that every auditory game is going to improve individuals’ ability to hear in the presence of background noise. I bring this up because I think that we are going to continue to see some interesting data that evaluates these gamification techniques and the transference that they have to other domains for improvement. In this example, it is the ability to hear in the presence of background noise. I encourage you to keep checking into this topic because there will be new games and improvements to technology over time.
Instead of telling patients that they have to do auditory rehabilitation training, we can tell them that we have a suite of games that will cognitively challenge them and may result in better hearing in noise.
Other Games
In addition to ReadMyQuips, there are some other games that may lend great benefits from a cognitive perspective and maybe the auditory training piece. There is a suite of games called Brain HQ. It is developed by PositScience. For those of you who are not familiar with Brain HQ, it is an exercise workout for attention, memory, brain speed, people skills, navigation, and intelligence. There are a variety of games that fall into those categories that are designed to help people become more efficient in their skills. Figure 3 shows a list of the games that are available in the Brain HQ suite of games. Each box in that image represents a game that engages the auditory system in this suite. These are all games that engage the cognitive system by using the auditory system or auditory signals.
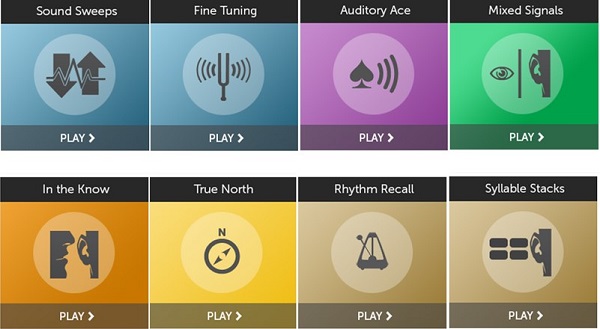
Figure 3. Suite of games included in Brain HQ.
Conclusion
I hope that after today’s presentation you can appreciate that cognition, aging, and hearing share an intricate relationship, and you will start thinking about what we can provide to our patients to help ensure the best outcomes with their amplification and on their hearing loss journey.
References
Anderson, S., White-Schwoch, T., Choi, H. J., & Kraus, N. (2013). Training changes processing of speech cues in older adults with hearing loss. Frontiers in Systems Neuroscience, 7, 97. doi: 10.3389/fnsys.2013.00097
Bock, K., & Abrams, H. (2013). An evaluation of the efficacy of a remotely delivered auditory training program. Starkey Hearing Technologies. Retrieved from https://starkeypro.com/pdfs/technical-papers/An Evaluation of the Efficacy_Remotely_Delivered_Auditory_Training_Program.pdf
Cabeza, R., Dolcos, F., Graham, R., & Nyberg, L. (2002). Similarities and differences in the neural correlates of episodic memory retrieval and working memory. NeuroImage, 16, 317-330. doi:10.1006/nimg.2002.106
Whitton, J. P., Hancock, K. E., & Polley, D. P. (2014). Immersive audiomotor game play enhances neural and perceptual salience of weak signals in noise. Proceedings of the National Academy of Sciences of the United States of America, 111(25), E2606-E2615. doi: 10.1073/pnas.1322184111
Leavitt, H., Oden, C., Simon, H., Noack, C., & Lotze, A. (2011). Entertainment overcomes barriers of auditory training. Hearing Journal, 64(8), 40, 42. doi: 10.1097/01.HJ.0000403510.80465.7b
Lin, F. R., Yaffe, K., Xia, J., Xue, Q., Harris, T. B., Purchase-Helzner, E., et al. (2013). Hearing loss and cognitive decline in older adults. Journal of the American Medical Association, 173(4), 293-299. doi:10.1001/jamainternmed.2013.1868
Maguire, E. A., Woollett, K., & Spiers, H. J. (2006). London taxi drivers and bus drivers: a structural MRI and neurophysiological analysis. Hippocampus, 16(12), 1091-1101. doi: 10.1002/hipo.20233
Merzenich, M.M., Kaas, J.H., Wall, J., Nelson, R.J., Sur, M., & Felleman, D. (1983a) Topographic reorganization of somatosensory cortical areas 3b and 1 in adult monkeys following restricted deafferentation. Neuroscience, 8, 33-55.
Merzenich, M.M., Kaas, J.H., Wall, J., Sur, M., Nelson, R. J., & Felleman, D. (1983b) Progression of changes following median nerve section in the cortical representation of the hand in areas 3b and 1 in adult owl and squirrel monkeys. Neuroscience, 10, 639-665.
Song, J. H., Skoe, E., Banai, K., & Kraus, N. (2012). Training to improve hearing speech in noise: biological mechanisms. Cerebral Cortex, 22(5), 1180-1190. doi: 10.1093/cercor/bhr196
Sweetow, R. W., & Sabes, J. H. (2006). The need for and development of an adaptive Listening and Communication Enhancement (LACE) program. Journal of the American Academy of Audiology, 17(8), 538-558. doi: 10.3766/jaaa.17.8.2
Cite this Content as:
Prusick, L., & Harianawala, J. (2015, July). Anti-aging for the auditory system: no botox needed!. AudiologyOnline, Article 14499. Retrieved from https://www.audiologyonline.com.



