Exactly how long a hearing aid user must wait to be sure amplification is providing "benefit" in everyday listening situations remains unclear. Audiologists have wrestled with the question of hearing aid acclimatization for many years. Conventional wisdom suggests that the adult hearing aid user requires anywhere between one month and one year to receive maximum benefit from amplification. This statement is not without merit. A recent survey of approximately one hundred hearing care professionals indicated that there is no clear response to the question, "how long does it take adult hearing aid users to experience maximum hearing-aid benefit?" Clearly, there is not a clear consensus among clinicians to this important question (Figure 1).
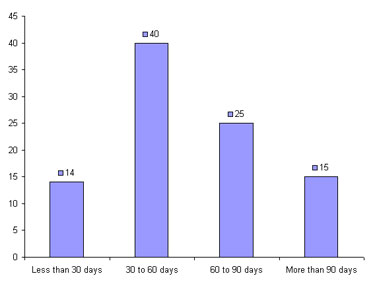
Figure 1. Survey data representing individual respondents' opinion on the amount of time patients require to become acclimated to amplification. Data from internal survey of Amplifon providers in the US and Canada, September, 2006.
Knowing when maximum hearing aid benefit is achieved also has commercial significance. The savvy consumer wants to know when they can expect to be "getting the most" from their new purchase. In a consumer age of instant gratification, informing patients that they may need to wait up to one year to fully acclimate to their new purchase may result in dissatisfaction. It is common for hearing aid users to ask, "How long do I need to wear these until I get used to them?" after they have purchased a set of new devices. Consumers have a vested interest in knowing when peak hearing aid benefit is achieved, and it is the responsibility of professionals to answer this question using the best available evidence.
Historical Background
The acclimatization issue has endured many years of controversy. In 1940, Watson reported increases in word recognition ability of more than 40% after three months of hearing aid use for one subject. Acclimatization, which has also been referred to as the process of adjustment and accommodation in the literature, refers to improvements is speech understanding over time resulting from the use of amplification. Because of the debate surrounding acclimatization, the Eriksholm Workshop on Auditory Deprivation and Acclimatization convened in 1995 and subsequently released a consensus statement. In summary, the Eriksholm Workshop held that acclimatization does occur, and that it is a phenomenon with importance to clinical practice with mean reported improvements in benefit over time any where between 0 and 10%. As a result of this workshop, several investigators sought to determine the magnitude of acclimatization, especially as it relates to the clinical fitting of hearing aids.
Consequently, several investigators began to examine acclimatization more closely. Two separate meta-analyses were published, one in 1996 by Turner, Humes, Bentler and Cox, and the other by Palmer, Nelson, and Lindley in 1998. Both of these meta-analyses concluded that acclimatization does occur to a small extent, but these improvements in benefit-over-time cannot be measured or observed to any noticeable effect in the clinic. Many of these findings, as they relate to clinical practice, were summarized in a special issue of The Hearing Journal published in 1999. In the nearly eight years since that special issue, more studies using modern hearing aid technology have been published on acclimatization. Given the recent advent of evidence-based practice (EBP) and the evolution of hearing aid technology, an update on this clinically relevant subject is warranted. The focused questions to be investigated using an EBP paradigm are related to how long a typical patient must wear hearing aids before maximum benefit it achieved.
Evidence-Based Review
A better understanding of the hearing aid acclimatization process has several important clinical implications. First, most clinicians make one or more adjustments to the hearing aid during the adjustment period, which usually comprises the first 30 to 60 days of use. The number of adjustments the typical clinician makes during this so-called adjustment period is shown in Figure 2. If acclimatization occurs over months rather than days, clinicians might be better off waiting to make these adjustments until after peak benefit has been achieved. Additionally, if benefit peaks at a specific point in time, patients might be best advised to "wear it and get used to it" before returning for any additional office visits in which adjustments to the hearing aid parameters are made.
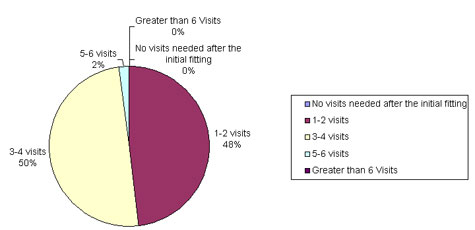
Figure 2. Number of visits needed, on average, between the initial hearing aid fitting and the point at which the hearing aid settings are satisfactory.
Next, if acclimatization takes place over a specific time period, patients should be provided with hearing aids that will lead to the best performance, rather than being fitted with hearing aids tailored to the patient's preference. Third, if there is a point in time when peak benefit is reached, the clinical evaluation of hearing-aid benefit would not be considered valid unless it was performed after this time period. For those interested in documenting self-reports of outcome, this is important because measurements should occur at about the time benefit is at its peak. Fourth, most states require a hearing aid trial period as part of the purchase agreement. The patient is able to return the hearing aids for full or partial credit if dissatisfied for any reason. If maximum benefit is achieved only after a long period of use, states might be inclined to extend trial periods beyond the customary 30 days.
An evidence-based review was conducted in order to answer the question, "When is peak benefit achieved for adult hearing aid users?" In order to answer this focused question, this evidence-based review included studies that measured both objective and subjective benefit over a specific period of time. Objective measures of benefit are considered as procedures in which an aided score is compared to an unaided score on any standardized test measured in laboratory conditions. Subjective measures of benefit are considered as any self-report of hearing aid outcome completed by the patient at some point after the fitting. In an EBP paradigm, self-reports of outcome are considered to be the "gold standard" for measuring real-world benefit. Since many clinical protocols and hearing aid research employ both subjective and objective measures of outcome, both were included in this review.
Methods
Using the five steps of EBP outlined by Cox (2005), only papers published over the past 15 years were included in this review in an attempt to answer this question: "How long does it take adult hearing aid users to experience maximum benefit from amplification?" In order for the evaluation of the evidence to be considered effective, studies were included for review if they met the following criteria:
- Published in peer-reviewed journals and other refereed publications and conferences between 1989 and 2007
- Used adult subjects with hearing impairments
- Employed a measurement of either objective or subjective hearing aid outcome using a standardized test or self-report scale
- Utilized hearing aids worn by study participants in everyday listening situations
Click here to download Table 1 addendum (PDF File)
The decision to exclude articles published before 1989 was not arbitrary, as other types of signal processing besides linear did not become widely available until about that time. An important part of this evidence-based review was to investigate the relationship between various types of signal processing found in modern hearing aids and the effects they might have on acclimatization.
It was also determined that adults, rather than children, would be the focus of this review, as results for pediatric populations are considered to be considerably different. Additionally, attempts were made to carefully examine studies comparing changes in benefit for new and experienced users as well as unilateral versus bilateral hearing aid users.
Results and Discussion
A total of 15 studies met the criteria discussed above and were included in this review. A summary of each of these is outlined in Table 1.
Click here to download Table 1 addendum (PDF File)
Most of the studies included in this review were non-randomized intervention studies, which are considered Level 3 evidence (Cox, 2005).
Five of the studies employed unilateral hearing aid users only, and eight of the studies examined bilateral users only. Two of the studies examined a combination of bilateral and unilateral hearing aid users in their study design. There appears to be no relationship between the type of fitting arrangement (unilateral or bilateral) and acclimatization effects.
Seven of the studies examined only new hearing aid users, six included a combination of experienced and new hearing aid users, while two included only experienced hearing aid users. A careful reading of the evidence shows no obvious relationship between amount of experience with amplification and acclimatization.
The effects of age and hearing loss on acclimatization were also considered. None of the studies reviewed compared the effects of acclimatization to age or hearing loss specifically. Therefore, no statements about how age or hearing loss is related to the acclimatization process can be made at this time.
One important motive for conducting this evidence-based review was to investigate the possible role that modern hearing aid technology might play with acclimatization. Because hearing aid circuitry is becoming more complex, it was important to see if the evidence suggests that users of these more complex devices actually need more time to get used to them. Five studies comparing various types of signal processing to acclimatization were reviewed. In three of the five, there appears to be some relationship between the complexity of signal processing in the hearing instrument and acclimatization. Of particular interest are two recently published reports comparing devices with low compression thresholds to a matched linear instrument.
Yund, Roup, Simon, and Bowman (2007) and Kuk, Potts, Valente, Lee, and Picirrillo (2003) found that users of multi-channel wide dynamic range compression (MCWDRC) with short time constants experienced acclimatization on objective measures of speech intelligibility in noise. Acclimatization for users of MCWDRC hearing aids might be related to the fact that more of the speech signal in everyday listening situations is being amplified into the residual dynamic range of the end user compared to those using single-channel WDRC or linear processing. Although these studies suggest acclimatization is related to the complexity of the signal processing scheme used by the hearing aid, more studies are needed to confirm this finding.
Although acclimatization appears to be a real and quantifiable phenomenon, the ability to measure it clinically is difficult., There is no evidence to support acclimatization effects beyond the first 30 days of hearing aid use for both experienced and new hearing aid users when commercially available objective tests and subjective self-reports of hearing aid outcome are used.
Although the evidence would indicate that peak benefit is obtained within the first 30 days of hearing aid use, this conclusion needs to be interpreted cautiously for the following reasons:
- When objective laboratory tests using greater high-frequency information are employed, improvements in benefit over a longer period of time are measurable. Specifically, when the Four Alternative Auditory Feature (FAAF) test (Gatehouse, 1992; 1993) and the Non-sense Syllable Test (NST) are used to measure changes in speech intelligibility, acclimatization ultimately occurs. It is possible that both the FAAF and NST are more sensitive to the subtle effects of the acclimatization process. However, the FAAF, which uses 80 sentences presented at four signal-to-noise ratios, and the NST, which employs a lengthy test time paradigm, are not feasible for clinical use.
- There is some evidence suggesting that users of more complex hearing aids, such as those with MCWDRC experience acclimatization to a greater extent than users of linear or single-channel WDRC devices.
- This review reflects changes in benefit-over-time for the ideal hearing aid user. All of the studies included in this review used participants who wore hearing aids four or more hours per day. The participants, in effect, were all ideal hearing aid users, who faithfully followed the instructions of the clinician and were motivated to wear their devices most of the day. Unfortunately, not all patients encountered in a typical practice would be this compliant. When a lack of motivation or low daily use rate is factored into the equation, it may be possible to measure more significant changes in hearing aid benefit-over-time. For example, the Vestergaard (2006) study would indicate that changes in benefit as measured on self-reports of outcome are conditioned by a certain amount of daily use.
- No studies were reviewed that take into consideration the effects of aging on the process of acclimatization. There is some laboratory evidence suggestive of the fact that acclimatization occurs over a long period of time in the aging auditory system. (Palmer, et al., 1998). This laboratory finding warrants further investigation of the effects of aging on acclimatization to hearing aids in everyday listening conditions.
- An additional factor is related to training effects. One example gaining recent popularity is the Listening and Communication Enhancement (LACE) program. There is evidence suggesting that this type of auditory training programs is effective (Sweetow & Palmer, 2005). Acclimatization, by definition, refers to improvements in benefit over time not related to training effects. In one recent study, Stecker et al. (2006) concluded acclimatization and the effects of systematic auditory training were complimentary. Further investigation on the combined effects of auditory training and acclimatization is needed.
It would appear that most clinicians believe acclimatization exists. This is evident by the fact that nearly all clinicians tell their patients they must wear their hearing aids for a certain period of time in order to "get used to it." Moreover, Mueller and Powers (2001) have even suggested clinicians use a handout displaying the message, "You first have to hear what you don't want to hear to know what you don't want to hear."
The opinion of audiologists that acclimatization exists can be supported by the evidence. Just how long, however, a patient must wear their hearing aids in order to hear what they don't want to hear - and achieve maximum benefit - has no clear consensus, thus warranting this evidence-based review.
Although the effects of acclimatization are difficult to measure clinically, there is evidence suggesting acclimatization does exist during the first month of hearing aid use for both new and experienced users. Given this finding, clinicians should use clinically proven prescriptive fitting strategies at the initial fitting, and advise patients to consistently wear their hearing aids for 30 days before outcome is measured.
The evidence would suggest that measuring benefit at 30-days post-fitting would provide both the patient and the clinician with a reasonably accurate picture of peak benefit. However, patients should be counseled that they may experience additional improvements too subtle to measure clinically. This concept is perhaps best summarized by the late Dennis Byrne who said, "The probability of acclimatization emphasizes the importance of striving to achieve the best possible fitting at the outset so that the hearing aid wearer will acclimatize to the type of sound that is capable of providing the most benefit. The client should be encouraged to get used to the hearing aids that should be the most beneficial rather than the ones that sound the best initially." (Turner et al., 1996, p. 25)
The preponderance of evidence would suggest that clinicians should fine-tune the hearing aid to match a prescriptive fitting target (e.g. NAL-NL1) at the initial fitting using real-ear verification, and allow acclimatization to occur. Even at the first signs of patient complaint, the best course of action would be to give the patient more time to become acclimated, over approximately 30 days. Evidence reviewed elsewhere (Mueller, 2005) proposes that the optimal starting point for achieving benefit for average-level inputs is through the prescriptive target for matching loudness equalization (e.g. NAL).
Another important clinical concern is when to conduct self-reports of subjective outcome in order to document hearing aid benefit in real-world listening situations. Self-reports conducted too early (1-2 weeks) provide misleading information because patients have not been given ample time to better assess real-world benefits. Kuk, et al. (2003) and Vestergaard (2006) suggest that self-reports of outcome did not accurately reflect true outcomes when administered too early in the fitting and subsequent adaptation process. Both these studies attribute the lower-than-expected self-reports of outcome when measured right after the fitting (i.e., one day to two weeks) to inexperience with hearing aids rather than the acclimatization process. The finding that self-reports of hearing aid benefit are artificially low when assessed too early is consistent with the work of Humes and colleagues (2003; 2004), who suggest that outcomes should be assessed approximately one month post-fitting. Additionally, Munro and Lutman (2004) conclude that response bias plays a role in changes in subjective benefit over time. This finding would be in agreement with Cox, Alexander, and Gray (2007) who concluded that the type of self-report used to evaluate benefit contributes to the final measured outcome.
Most states mandate a trial period in order to allow patients ample time to receive noticeable benefit from their hearing aids. Based on the evidence, the customary 30-day trial is a reasonable time frame for most patients to get fully accustomed to their hearing aids.
Since clinicians do not conduct tests sensitive enough to measure changes in benefit over time, they are advised to pick a specific point in time to measure both objective and subjective benefit. Objective outcome measures should include some type of sentence-length speech-in-noise test because of the high face validity. Self-reports of outcome that encourage the patient to be introspective about his or her everyday listening problems (such as the HHIE or COSI) and measures of daily use are most appropriate (Cox et al., 2007). Conducting these types of measures 30-days post-fitting would be supported by Level 3 evidence.
Conclusion
Based on peer-reviewed evidence, the average length of time a patient may require to become accustomed to their hearing aids, regardless of user history, is approximately 30 days. Subjective and objective measures of benefit over time prove to be useful. However, more sensitive, clinically applicable measures of benefit should be investigated to ensure patient acclimatization and benefits are at a maximum.
References*
Cox, R.M. (2005). Evidence-based practice as a provision of amplification. Journal of the American Academy of Audiology, 16(7), 419-438.
Cox, R.M., Alexander, G.C., & Gray, G.A. (2007). Personality, hearing problems, and amplification characteristics: contributions to self-report hearing aid outcome. Ear and Hearing, 28(2), 141-162.
Gatehouse, S. (1992). The time course and magnitude of perceptual acclimatization to frequency responses: Evidence from monaural fitting of hearing aids. The Journal of the Acoustical Society of America, 92(3), 1258-1268.
Gatehouse, S. (1993). Role of perceptual acclimatization in the selection of frequency responses for hearing aids. Journal of the American Academy of Audiology, 4(5), 296-306.
Humes, L., Wilson, D., & Humes, A. (2003). Examination of differences between successful and unsuccessful elderly hearing aid candidates matched for age, hearing loss, and gender. International Journal of Audiology, 42(7), 432-441.
Humes, L. & Humes, L. (2004). Factors affecting long-term hearing aid success. Seminars in Hearing, 25(1), 63-72.
Kuk, F.K., Potts, L., Valente, M., Lee, L., & Picirrillo, J. (2003). Evidence of acclimatization in persons with severe-to-profound hearing loss. Journal of the American Academy of Audiology, 14(2), 84-99.
Mueller, H.G. (2005). Fitting hearing aids to adults using prescriptive methods: an evidence-based review of effectiveness. Journal of the American Academy of Audiology, 16(7), 448-460.
Mueller, H.G. & Powers, T. (2001). Consideration of auditory acclimatization in the prescriptive fitting of hearing aids. Seminars in Hearing, 22(2), 103-124.
Munro, K.J., & Lutman, M.E. (2004). Self-reported outcome in new hearing aid users over a 24-week post-fitting period. International Journal of Audiology, 43(10), 555-562.
Palmer, C., Nelson, C., & Lindley, G. (1998). The functionally and physiologically plastic adult auditory system. Journal of the Acoustical Society of America, 103(4), 1705-1721.
Stecker, G.C., Bowman, G.A., Yund, E.W., Herron, T.J., Roup, C.M., & Woods, D.L. (2006). Perceptual training improves syllable identification in new and experienced hearing aid users. Journal of Rehabilitation Research & Development, 43(4), 537-552.
Sweetow, R. & Palmer, C. (2005). Efficacy of individual auditory training programs in adults: A systematic review of the evidence. Journal of the American Academy of Audiology, 16(7), 494-540.
Turner, C., Humes, L., Bentler, R., & Cox, R. (1996). A review of past research on changes in hearing aid benefit over time. Ear and Hearing, 17(3), 14S-28S.
Vestergaard, M. D. (2006). Self-report outcome in new hearing-aid users with ski-slope hearing loss: longitudinal trends and relationships between subjective measures of benefit and satisfaction. International Journal of Audiology, 45(7), 382-392.
Watson, N. (1940). Selective amplification in hearing aids. Journal of the Acoustical Society of America, 11(3), 406-419.
Yund, E.W., Roup, C.M., Simon, H.J., & Bowman, G.A. (2007). Acclimatization in wide dynamic range multichannel compression and linear amplification hearing aids. Journal of Rehabilitation Research & Development, 43(4), 517-536.
*Other references cited in Table 1 Click here to download Table 1 addendum (PDF File)