Editor's Note: This is a transcript of a live seminar. To view the recorded course, register here: /audiology-ceus/course/hearing-hearing-loss-215-hearing-aids-adults-emergence-hearing-loss-in-adult-19816
This is the first in a series of talks on Hearing Loss from the Inside Out: The Patient's View. My goal with this series is to shed light of some of the issues we deal with in the area of hearing loss and hearing aid treatment, especially from the perspective of adult patients who have sensorineural hearing loss. Often in audiology, we focus on our own perception of the world and our beliefs about the way things should be done in our clinical practices. There is always value in taking a step back and seeing it from a different perspective and, of course, the perspective of the patient is a very valuable one to take.
I want to review some data that Oticon has collected, including work conducted through our Eriksholm Research Center in Denmark, that gives us a glimpse into the mindset of an adult who is starting to develop, by our definition, a hearing loss. The way WE define things is exactly the heart of the matter that I want to deal with today. What we define, clinically, as a hearing loss is a change in perception that will gradually occur for adults over the years. It may not necessarily be defined by the patient or potential patient the same way the audiologist would define it. When we talk about the willingness to seek amplification as a solution for the hearing difficulties, the patient's attitude and emerging perception of what they are dealing with matters very much. They are the ones who have to make the active decision to enter the hearing healthcare process. They are the ones that have to make the active decision to obtain amplification and use it. Their viewpoint on exactly what sort of problems they are having is absolutely relevant.
So today, I want to step back and take a look at this issue from the patient's perspective based on data that has accumulated over the recent years. Let's start with this common question an audiologist might ask to a new patient: When did you first notice trouble with your hearing? It is a relatively well-formulated question because it does not label the patient as a person with a hearing loss. It does not ask when they first noticed their hearing loss, but is more operational in nature. It is asking when they first noticed trouble with their hearing. In reality, it is a loaded question. As we have learned more about the emergence of hearing loss over the years, we realize that a big factor in the patient's realization of a hearing problem is the comprehension that this does not happen in one day. It is not something that is immediately apparent to the person, yet it seems everybody around them knows exactly what is going on.
This emergence and gradual realization of a hearing loss is not simple and straightforward. There are many angles and a lot of things to consider. I think many audiologists, especially audiologists in the business of fitting hearing aids to first-time users of amplification, feel a great deal of frustration when they see a very apparent hearing loss on an audiogram, yet the patient is openly not ready to get hearing aids. What is holding them back? One of the things that has to be discussed is patient motivation and how the patient came to the realization that they have a hearing problem to talk about. That process that the person goes through, the feelings that they are feeling, the realizations that they have and the way they define themselves as a person all factor into whether or not they decide to take the next step and do something about their hearing loss. When we talk about "aging" or the typical progression that an adult experiences over the years, it is important to remember that physiological changes happen to the body.
These changes are part of a process; they do not happen the day you turn 65. They can start for different patients during different time periods. It is entirely individual. One of the things that is extremely important to remember and to always pay attention to from our perspective is that hearing is just one of the things that changes in a person as they get older. It is not the first thing that changes. Hearing loss might be one of the later things that becomes apparent as a person ages. Many other things have already changed before hearing: vision, when your hair falls out or turns gray, when you start to have trouble maintaining weight, or when you start to develop some chronic conditions such as diabetes. Part of noticing body change in the adult is whether or not the person him or herself defines those changes as problems. The reason that definition is important to consider is that a person who feels that they are having a health problem is more likely to seek out treatment than a person who casually notices something is different about their body because they are older. People are logical. They are smart. They understand that the human body does not stay in a preserved state throughout the years. If you do not hear as well as you get older, that is not necessarily the same thing as having a hearing loss. It just means something may have changed.
There are, of course, things that do not necessarily change as you get older, such as long term memory. You can sit with your great-grandpa on the porch and he can remember things that happened when he was a young boy. Core intelligence and linguistic skills do not change, but some things do change. A lot of it has to do with functional ability, especially in terms of information processing. One of the other things I want to focus on are things that do change over time, like short term memory and processing and decision speed. When you talk about selective attention, remember that people do not use their hearing just to hear things. They typically use their hearing because they are doing things. They are engaging in conversation. They are enjoying a movie, and they are listening to a lecture. It is not just hearing that matters. It is memory and attention to the material that matters. All these aspects can affect the abilities that are attributed to the person's hearing, and loss of hearing ability might not be terribly apparent. It is apparent to us as audiologists because we test them and know what their sensitivity is like.
Perhaps we have some idea of their skills in a noisy environment, but since humans function in a multi modal manner, they are using lots of different capabilities when they go about their day. They do not necessarily isolate out their hearing as a separate component of what is happening. When they start to have trouble with communication, they find themselves struggling a little bit more, and they are not naturally going to recognize what part of that is being caused by a change in hearing every single time. Part of that may be attributable to short term or selective memory issues that occur physiologically at the same time. So when we get back to the way an individual defines a hearing problem: I have a hearing loss versus I do not hear as well as I used to, those two different statements could be two very different perspectives that a person is taking. In one sense, the statement I do not hear as well as I used to may be perceived as active denial, or that the person does somehow not want to admit that they have a hearing loss. However, in some cases it may not necessarily be active denial. They do not necessarily define "not hearing as well" as the same thing as having a hearing loss. You have to remember that when a person says I have a hearing loss or I am a hearing-impaired person, that is a label that they are applying to themselves. If it is perceived as negative condition to have, there is a tendency not to want to use that label. Combine that with the knowledge that the body changes over the years, and it may lead to the point where they will recognize that their hearing is not as good as it used to be.
That is not the same thing as having a hearing loss. The audiologist would say that is the same thing, but it does not matter what we think. The point is that the patient may not choose to use that label. It is a threat to self identity to say, "I am a person with hearing loss." Taking the step to make that statement about oneself can be a road block, and it is one of the things that, as audiologists, we need to understand how emotionally-laden that statement can be for a person.
There are some cases where patients will actively make the statement I do not hear as well as I used to. That does not mean I have a hearing loss. We would oftentimes define that as denial. One of the things to remember about denial is that it is a defense mechanism. Defense mechanisms are reactions that a person will take when they are faced with a reality that they are not emotionally equipped to deal with effectively, and those can include anger or bargaining. People adopt defense mechanisms because they are trying to figure out how they are going to relate to this new reality. When a person says I do not hear as well as I used to, that might be necessary for them to see the situation that way. One of the things that we have learned over the years is that we cannot dismiss denial as a trait that is difficult to deal with. We have to understand that denial is real. It is there for a reason. That does not mean that there are not things we can do to help the person through it, but we have to respect the person enough to realize that if denial is issue, there is a root cause.
What's the Evidence?
I want to turn to several different data sets that have helped shape our opinion at Oticon about what we should know about patients and the way they deal with hearing loss as it is emerging. Back in 2010 we contracted a very large international survey of patients, both those who had hearing loss and had experience using hearing aids and patients who suspected they had a hearing loss but had not done anything about hearing aids yet. We wanted to tap into the way they think about hearing aids, what they are doing about it, their attitudes towards the hearing healthcare process and things like that. There is a tremendous amount of data we have in the survey, and I just want to touch on a few elements of that data.
The data was collected internationally, from the United States, Canada, Germany, France and Italy as a Web-based survey. We had an equal split between those who were experienced hearing aid users and those who suspected that they had a hearing loss but had not formally done anything about it. The group that suspected they had a hearing loss but had not done anything about getting hearing aids was asked, "How concerned are you that this is a problem?" They took the survey because they suspected they had a hearing loss but that is different from knowing how big of an issue it was. Only 17% defined this as either a "concern" or a "major concern" for them. This might mean a lot of different things. It might mean that the person is actively minimizing the effect of the hearing loss, and they do not really want to admit it. But this was an anonymous, Web based survey so they did not have to say this out loud to anybody. I think it is a relatively legitimate look about the way they were feeling about it. The data does point out that just because a person notices they have hearing loss does not necessarily mean they are highly motivated to do something about it.
On the flip side, we also asked them, "How interested are you in a solution for your hearing difficulties?" When we asked the question that way, we had two thirds of patients being either somewhat or very interested in a solution, which could tell us a couple of different things. Maybe it is a mismatch between how concerned they are versus how interested they are in a solution. On the other hand, it could simply be a reflection of a new type of health-care consumer behavior that we have not necessarily seen in decades past, where people are more willing to talk about their hearing and solutions without actually taking action at this point in time. We have this notion that people with hearing loss know they have a hearing loss. They are just not going to talk about it until somebody forces them to do something about it. So they get dragged kicking and screaming by the family into the hearing clinic and then they finally have to confront their issues. It may not be so much that way anymore with the use of the Internet and rapid amount of dissemination of information. The idea that a person may not be terribly concerned about their hearing but is still interested in knowing what the solutions are is perfectly legitimate and consistent with the data. It does point out that just because a person is talking about the hearing loss or seeking information that is not necessarily the same thing as indicating that they are ready to act.
Another aspect that came out of the survey was a verification of the well known observation that it takes individuals, on average, seven years between the time when they first notice that they have a hearing loss before they actually do something about it. That average of seven years has been floating in our audiological culture for decades. Normally when you say average, you automatically think that the distribution is a bell curve, centered around the average. The reality when we took a look at the data from the survey was that it was not anywhere near a bell curve (Figure 1).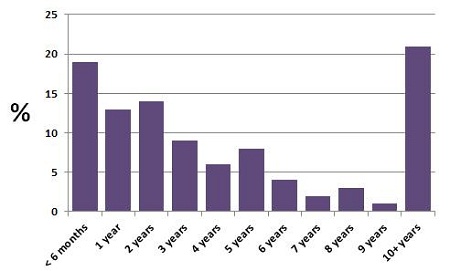
Figure 1. Distribution, based on an Oticon Web survey, of the time frame in which those individuals sought treatment after they first noticed a hearing problem.
What you notice is a tremendously bimodal distribution. In other words, it is not that bell curve that we expected, but rather a large portion of the distribution is within the first couple of years, and then again at ten years and beyond where they actually decide to go to have their hearing evaluated. They might not necessarily get hearing aids at this point, but at least they entered the process.
So although the actual numbers averaged out to equal seven years, the distribution of when people take action is very different than you might expect. That tells us something. It indicates that there is something in the behavior pattern that varies significantly from individual to individual. There will be a distinct difference between the person who seeks advice about their hearing problem within 1 year of noticing a problem versus the person who waits 10 years. We have to recognize that there is variation in the human reaction to hearing loss, and we cannot continue to think that all patients respond to the presence of the hearing loss in a similar way.
Another thing that is important to remind ourselves is that hearing loss for many individuals is considered to be a potential medical issue. Those of us working in the hearing aid aspect of the field know that most adult hearing loss is progressive, and there is nothing that can be done medically or surgically about it; the only real treatment option patients have is amplification. That does not necessarily mean that the patients see it that way.
In the survey, the major concerns of those who said they would do something about their hearing loss are: Will it get worse if I do not do something about it? Do I have a hearing loss or is it something else? Is it permanent or temporary? When should I seek help? These kinds of concerns all tend to be medical issues and we know most of the answers, we need to recognize the validity of these concerns and understand that the patient may not share the same attitude that we do: hearing aids are the best and next step in treatment. The thing that strikes me about this observation is the mindset of a patient who comes to you as a first-entry into the process and their mindset is, "Is this a brain tumor? Is this something I have to worry about? Is my head going to fall off? Is there something to be done to stop it?" They are thinking about this as a physical condition where they are looking for some sort of treatment. Eventually, you come to the place where you can counsel that it is not a medical problem, that it is likely not going to improve and may, in fact, get worse, the only real option is to start thinking about amplification. If the patient walked into that process thinking that this is a medical condition, they may not have had that conversation with themselves yet about the idea of using hearing aids. Depending on your clinic, you might be in a position where you want to start talking to them about hearing aids, but they may not respond very well to that conversation only because they have not realized that within themselves yet.
I want to change topics and talk about a project done by our Eriksholm research center in Denmark a few years ago. It gets to the heart of this emergence issue that I talked about. The question is, "At what point does a person realize what they are dealing with is a hearing loss?" When you test a person's hearing, it just happens to be one day on the calendar where that person actually showed up to have their hearing tested, but that hearing loss did not occur the day before in most cases, of course. That hearing loss occurred over the course of many years. At what point does the person realize that it is a hearing loss? One of the conclusions out of this work is that, early on, the patients did not even conceive of the idea that it could have even been a hearing loss. The concept is that the patients may not have thought about hearing loss as an explanation for the problems they were having until years after the loss probably emerged. Maybe they thought it was an issue of attention, short term memory, concentration, or stress. They may not have realized that it was a hearing loss.
A former colleague, Gitte Engelund (2006) from the research group, described the process that a patient goes through to come to the conclusion that they need to do something about their communication problems. In other words, there must be an unveiling of information and realization on the part of the patient of what the process is like. What happens over the years or months to bring to the person to the point of motivation where they actually do something about their hearing loss? Engelund did a series of extremely intensive, very well documented and well-structured interviews with patients to try to uncover what this process was like. I will be the first to admit that I am not doing anywhere near the sort of service to the good work that she did on this project by just doing a very quick summary. One of the conclusions she made is that there are different dimensions that will affect bringing the person to the point where they realize that they have to do something about their hearing loss. One of the factors that is going to push a person in that direction is the nature of the person's hearing loss. How much hearing loss do they have audiometrically? Oftentimes in audiology, the only definition we think about is the audiometric definition: pure tones, word recognition, et cetera. She also pointed out to bring a person to the point where they are actually going to take action and do something about it, there are other forces that have to come to play.
One of the forces that Engelund (2006) categorizes is "activities of consciousness". Basically what she was talking about is this awareness of dealing with a hearing loss, that this is not memory, not selective attention. Perhaps it is not an awareness they come to themselves, but somebody else points it out to them whether that be a family member or a friend. Hearing loss to some people does not really matter unless it is getting in the way. It may not matter to them what it looks like on an audiogram or how far away their thresholds are from normal unless it is getting in the way of their life. When it causes a communication breakdown, that would make a person aware there is something different about their hearing.
The other major influence that is going to move a person in this direction is what Dr. Engelund refers to as "moments of a tribulation". That is when the presence of hearing loss and communication breakdown starts to create problems in the person's life. I did not understand what was said and it is making my family unhappy; It is causing a problem at work; I am embarrassed. I missed something important. Something has caused an emotional or a practical element to the presence of the hearing loss. Just having hearing loss, in and of itself, does not matter unless it is causing issues. I think of my parents, for example. My mother passed away several years ago, but before she died my father had a hearing loss that was untreated. If you want to try to treat my father for his hearing loss, be my guest. But my father had a hearing loss that caused a minimal amount of inconvenience because my mother and father had retired. They had lived in Chicago all their lives. They moved out to San Diego and did not have a strong social circle because they did not know a lot of people there. So the communication my parents did was basically one on one with each other, and my father is not a very social guy by nature. So even though he had a hearing loss it really was not a problem because my mother was fine with making whatever corrections in her behavior that she needed when they watched TV or went out. She learned not to talk to him from room to room, and it was not a big deal to her. Just having a hearing loss was not enough for my father to do anything about it because my mother constructed her life around my father's needs. In short, there were not enough moments of tribulation to move them in the direction to do something about that.
Dr. Engelund (2006) talks about the different drivers that make one recognize it is time to do something about the hearing loss. First, the hearing loss or the communication problem will attract attention. Secondly, the person becomes suspicious that they have a hearing loss. Third, there is something that they need to do. The time order of these occurrences does not necessarily matter. Maybe they have become suspicious and start attracting attention or vice versa. Everyone's life is going to be different. At some point they are going to be sensing tribulation, recognizing that the hearing loss is going to be a problem and is getting in the way of things. It is not going to be one event, but rather a culmination of events over time. Finally, for many individuals the tipping point comes when the hearing loss jeopardizes self-identity. The hearing loss is now causing me, as a person, to be defined differently. The admission of being hearing impaired and using that label is a threat to self identity in the sense that it will keep a person from taking action. But it is the presence of hearing loss, the embarrassment factor, being left out, and withdrawing from situations that will also threaten self identity. For many individuals that is the tipping point where they say, "I have to do something about this because I am not myself any more. People are noticing and do not want to communicate with me as much anymore. I am starting to get embarrassed about this."
The point with all of Dr. Engelund's work is that this is a gradual process. It is a buildup of forces. Patients do not just one day wake up and say, "I have a hearing loss. I am going to do something about it." There has got to be a driver to make them want to do something about it. Those drivers usually are very personal and very emotional to the point that the hearing loss is causing a negative enough emotion for the person to take the next step and do something about it.
There is an interesting project that I refer to often that gives us a little insight into the psyche of those with hearing loss. In the late 1990s, Garstecki and Erler (1998) took a group of older individuals and screened them for hearing loss. They made a recommendation to those who they considered to be candidates for hearing aids that they thought would likely benefit from amplification and that, as audiologists, they considered this situation one where you should do something about it. They then did personality testing for that group of individuals who they identified as being candidates for amplification and tracked those individuals' behavior over time. They wanted to define some personality characteristics that would distinguish those who would follow up with the hearing aid recommendation versus those that would not do anything and just ignore the presence of the hearing loss. What they found was pretty clear evidence that there are specific personality factors associated with those who will do something about their hearing loss and those who will not. The strongest of those personality factors that predicted follow up was higher internal locus of control. A person with an internal locus of control is someone who feels that they are in control of what happens to them and that they are not a victim of the world. They are not a puppet of forces outside of themselves, and that if good or bad things happened to a person it is because they are in control of those sorts of things that happen to them.
Other factors likely to be indicative of follow up were higher ego strength, fewer depressive tendencies, assumed responsibility for communicative success and an overall higher acceptance of hearing loss. There is a personality element to it. What is their personality? How do they respond to negative information? How do they respond to the threat of a changed self identity and what do they do about it? I have always been impressed with the quality of the Garstecki and Erler (1998) study, but also what it tells us about the audiogram and looking beyond that. To dig into that issue even further, a group of researchers, again from our Eriksholm Research Center in Denmark, wanted to examine some of those audiometric and demographic variables that would predict who would enter the hearing care process, who would purchase amplification, and who would benefit from amplification. They did this by reviewing many studies that were already published in the literature that looked at different facets of these questions: Does the audiogram predict who is going to get hearing aids? Does the audiogram predict who is going to benefit from hearing aids? Do age and gender matter? They performed a meta analysis across all these projects to see if there were any specific predictive variables that could help give an indication as to who is going to follow up and do something about their hearing loss. What they found after examining some of the most common demographic and audiometric variables including age, gender, measured hearing loss, duration of loss, socioeconomic status, health expectations, activity level, et cetera, was that none of those factors were found to be consistently related to those who sought out amplification or those that felt they were doing well or not so well with amplification.
This is important because many audiologists have their set predictors. "I know that if a person has more than this amount of hearing loss or if they score this way on a speech test, that is going to tell me whether or not they are going to be a good hearing aid user." It does not look like there are any of those very easy-to-predict variables that are going to give us that information. That is a much more complex sort of set of conditions that have to exist before you can be sure that a person is going to take action. The Eriksholm group did find one factor, however, that did predict which patients would actually go out and seek help for their hearing loss and obtain hearing aids and those who felt that they did well with hearing aids. That factor was self perceived hearing difficulties.
I do not think that this is a Nobel-Prize winning observation. However, it does point out that no matter how we as audiologists or family members define the situation, the personal problems patients feel that they are having is what is going to drive a person to get hearing aids. In other words, are the forces that Engelund (2006) talked about; the tribulation situations, this jeopardization of sensibility, the threat to one's self; strong enough to make a person say, "I am really having problems. This is really causing me difficulties. I need to do something about it." This is an operational lesson for audiologists to remember - if you feel a patient is a good candidate for amplification, but the patient needs some help in moving forward, focusing on self-perceived hearing difficulties is probably the best way to go. This is not news to a good audiologist. It is just a very good project to reconfirm that the patient has to feel like he or she is having problems. It does not matter what your audiogram says. It does not matter what the family says. It does not matter what the doctor says. It matters how the patient feels.
Hearing loss, as you know, is age-related in many cases. Often times one of the issues you run into is that the person thinks hearing loss is just something that happens when you get older. You just have to accept the fact your body does not work as well. People who work in the psychology of aging and healthcare study how a person handles the reality of an aging body. There is a group of responses that a person may give that can be grouped into the terms discounting or misinterpretations or passive acceptance. These terms refer to the attitude that, "Yes, I expect my body to change over time. I know I am not 21 years old anymore. This is just something that happens. I have to get used to it." That distinction between expecting it to happen versus expecting not to do anything about it is exactly that dilemma that we face with a lot of our patients. Individuals will react to a broad range of healthcare or body changes differently.
One of the things pointed out in the psychology of aging literature is that the definition of when something is "clinically relevant" is unclear to patients. In other words, they expect their body to change, but it is unclear to them if they should worry about it or if it is worth mentioning to family, a friend, or a healthcare professional. Hearing loss is not a gaping head wound, so oftentimes a patient will choose to ignore it because they are not ready to take a formal step in the right direction. It might be the classic sort of denial that we talk about, but it could simply be that it is not that big of a deal to the patient yet.
Another question raised in this literature on the psychology of aging is, "What does it take for a person to actually take action on a healthcare issue?" There are a couple of different ways of looking at the problem. One idea is from Leventhal and his colleagues (2001). They describe factors that determine if a person who has a chronic issue will make a behavioral change to improve their health. Another idea is from George (2001), who documents what factors predict that an elderly person will seek out medical attention. One of the things you notice from both sets of authors is that the person with the health issue has to believe that if they take action, their life is going to be better as a result. The confidence of older adults oftentimes becomes eroded and so they just put up with negative things like health issues because they do not believe that they can actually make their life better. It is a sad realization that they have lost enough self-confidence that they do not believe that they can take care of themselves very well. That is an issue that is a little sobering to think about.
Leventhal (2001) says that there has to be proper motivation, a plan, confidence that change is achievable and a good support system. This means that if the patient is going to do something about a problem, they have to want to do it and know that it is going to work out in the end. Usually in the realm of healthcare, these decisions are emotionally-driven and if the emotion is negative or frustrating enough, the person will finally do something about it.
George (2001) points out that an elderly person will seek out medical attention when there is an element of susceptibility. Can it really happen to me? Sometimes the individual may not realize that they are dealing with a hearing loss because they never thought that they could have a hearing loss. I know that seems illogical, but that does not make it untrue. Some patients will say, "I never thought I was the type of person who would get a hearing loss. I have never been around a lot of loud noise. I never went to rock concerts." They do not realize that hearing loss is something that can happen to practically anybody. Do not minimize the idea that they were not even aware that hearing loss could potentially be a problem for them.
The final set of data that I want to talk about was another interesting project done by our group at Eriksholm. It was called the Knarr Project, and they were very interested in the acoustics of real life situations. They found a group of hearing-impaired individuals and they walked around with sound recording equipment to record different situations throughout the course of the day. The researchers sat down with those individuals at one point in the project to debrief them on the acoustical tracings. They very quickly realized that they were missing an important point. They brought in an expert interviewer to do more in depth interviews with these individuals because what they observed was that they were defining a person's auditory world based on acoustics only. In other words, the researchers realized they were categorizing noisy situations in general terms: going to a restaurant, being in your kitchen with other people around, being in the car. We talk about it very much from an acoustic perspective only.
When they started to do these interviews with the individuals, they noticed that the listeners were not talking about the acoustics, but rather they were talking about communication interactions that they were having. In other words, those communication interactions were happening in a specific place and a specific time. But they were not focused on the environmental setting. They were focused on what they were trying to accomplish. They were trying to have a conversation with a certain person, and it happened to be in the kitchen. Their comments centered more on what successes or difficulties they were having. The researchers pointed out that audiologists tend to think of this as passive listening, where the only thing that matters is the acoustic characteristics of the environment including noise and reverberation. From the patient's perspective, the acoustics only became relevant when it got in the way of communication.
This brings us back to self perceived hearing difficulties and the notion of moments of tribulation. Hearing loss based on the acoustics of an environment is talking about hearing loss in a vacuum. If you want to talk about what matters and what is going to drive a person to want to do something about it, you have to think about it in terms of how important it is to the person that they communicate effectively. It does not matter what environment they are in until that environment gets in the way of them doing something important with their hearing, which is having an important conversation or listening to something meaningful.
One of the most important lessons that we can draw out of this material is that it really depends on how the hearing loss is impacting their life. Until the hearing loss impacts their life in a very negative way, and that happens often enough, the patient is not going to be motivated to do something about it. The conversations that we should have with patients about their hearing loss should be very much focused on how is it impacting their particular lifestyle and recurring social situations.
Lessons Learned
To summarize what lessons we can take away from these different studies, the first one is Hearing loss? Really? It is that first step where the person must realize that hearing loss is something to consider, and they may not necessarily notice it right from the start. They may deal with communication difficulties for a number of years before it dawns on them that it is hearing loss. We do not expect them to immediately define communication breakdown as the same thing as having hearing loss. They might not realize it.
The second lesson is that an adult will have a realization at some point that their body changes over time, but it does not come in the same time frame for everyone. Some patients take it to the extreme of saying, "I do not have to do anything about it because it is just something that is going to happen. This is one of those things I'm just not going to fix about myself." That is where you have to be very careful and very specific in the discussion with patients that, "Yes, it might be normal to have hearing loss at your age. Yes, this is something that happens to a lot of people, but a lot of people want to do something about it." That is really where the focus of the conversation has to be.
The next lesson is that some patients are just going to be looking. That might reflect a change in healthcare consumerism these days that more patient are out there searching. They are comparing healthcare providers and doing price shopping on the Internet. There is more information out there to help a person decide when and where and who they are going to deal with. It looks like adults are more likely to use this information before they make a decision. That means many more of these people might show up in the hearing healthcare process at an earlier stage in the process. They are looking around and gathering information. They may come in very early in the process, before the seven to ten year mark, but that does not mean that they are necessarily ready to take action.
I think the final lesson to take away from this is that it has to be about the communication problems that the person is experiencing. It cannot be about what the audiogram says. It cannot be about what environment they are in. It has to be about what they are missing and what sort of frustrations that is causing for the person. If you are trying to get a good indication about whether or not it makes sense to move forward with this patient or how much effort you want to put in to move this person along, the focus of those discussions should be, "How big of an issue is this for you? How much of a problem is it causing to you?" Data would suggest that until the person feels that their hearing is causing them real problems in situations that matter to them, they are not going to be terribly motivated to take action. That just helps frame who we want to deal with.
A lot of this information should have sounded quite familiar to most audiologists, especially those who have been in practice for a while, but it never hurts to review this material. Certainly for those of you who are newer to the field of audiology, it is a lesson that you will likely learn fairly quickly; that it is all about the patient's perspective and how they want to define themselves. What motivates a person to take action will vary from person to person. I appreciate you taking time out of your busy day to sit in on this. Thank you very much.
References
Engelund, G. (2006). Time for hearing: Recognising process for the individual- A Grounded Theory. PhD thesis from the Department of Nordic Studies and Linguistics Audiologopedics, University of Copenhagen, and Oticon Research Centre, Eriksholm.
Garstecki, D. C., & Erler, S. F. (1998). Hearing loss, control, and demographic factors influencing hearing aid use among older adults. Journal of Speech-Language-Hearing Research, 41, 527-537.
George, L. (2001). The social psychology of health. In R. Binstock & L. George (Eds.), Handbook of Aging and the Social Sciences (pp. 217-237). New York: Academic Press.
Leventhal, H., Rabin, C., Lventhal, E. & Burns, E. (2001). Health risk behaviors and aging. In J. Birren & K. Schaie (Eds.), Handbook of the Psychology of Aging (pp.186-214). New York: Academic Press.
The Emergence of Hearing Loss in the Adult Patient
April 23, 2012
This article is sponsored by Oticon.
Related Courses
1
https://www.audiologyonline.com/audiology-ceus/course/oticon-government-services-may-2023-38919
Oticon Government Services May 2023 Contract Update
Oticon understands that sudden, disruptive sounds affect a large majority of hearing aid users, making it difficult to stay sharp and focused – especially when engaged in conversation. Oticon Real™ is designed to help with this challenge and keep patients engaged. In this course we introduce new options on the VA hearing aid contact.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
Oticon Government Services May 2023 Contract Update
Oticon understands that sudden, disruptive sounds affect a large majority of hearing aid users, making it difficult to stay sharp and focused – especially when engaged in conversation. Oticon Real™ is designed to help with this challenge and keep patients engaged. In this course we introduce new options on the VA hearing aid contact.
38919
Online
PT60M
Oticon Government Services May 2023 Contract Update
Presented by Kirstie Taylor, AuD
Course: #38919Level: Intermediate1 Hour
AAA/0.1 Intermediate; ACAud inc HAASA/1.0; ASHA/0.1 Intermediate, Professional; BAA/1.0; CAA/1.0; IACET/0.1; IHS/1.0; Kansas, LTS-S0035/1.0; NZAS/1.0; SAC/1.0
Oticon understands that sudden, disruptive sounds affect a large majority of hearing aid users, making it difficult to stay sharp and focused – especially when engaged in conversation. Oticon Real™ is designed to help with this challenge and keep patients engaged. In this course we introduce new options on the VA hearing aid contact.
2
https://www.audiologyonline.com/audiology-ceus/course/why-evidence-matters-38163
Why Evidence Matters
Oticon has a long history of focusing on innovative research into how the brain processes sound and how technology can support the brain’s natural ability to process sound. In this course we will review evidence supporting Oticon’s technology developments and how hearing care professionals can use this information to discuss benefits and explain why they are recommending Oticon solutions.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
Why Evidence Matters
Oticon has a long history of focusing on innovative research into how the brain processes sound and how technology can support the brain’s natural ability to process sound. In this course we will review evidence supporting Oticon’s technology developments and how hearing care professionals can use this information to discuss benefits and explain why they are recommending Oticon solutions.
38163
Online
PT60M
Why Evidence Matters
Presented by Lana Ward, AuD
Course: #38163Level: Intermediate1 Hour
AAA/0.1 Intermediate; ACAud inc HAASA/1.0; AHIP/1.0; ASHA/0.1 Intermediate, Professional; BAA/1.0; CAA/1.0; IACET/0.1; IHS/1.0; Kansas, LTS-S0035/1.0; NZAS/1.0; SAC/1.0
Oticon has a long history of focusing on innovative research into how the brain processes sound and how technology can support the brain’s natural ability to process sound. In this course we will review evidence supporting Oticon’s technology developments and how hearing care professionals can use this information to discuss benefits and explain why they are recommending Oticon solutions.
3
https://www.audiologyonline.com/audiology-ceus/course/oticon-government-services-introducing-more-36630
Oticon Government Services: Introducing Oticon More
Sound scenes are dynamic, complex and unpredictable. It is the role of the brain to handle this complexity to hear and make sense of it all. Oticon is committed to developing life changing technologies that support the way the brain naturally processes sound. Get ready to discover the new perspective in hearing care with a fundamentally new approach to signal processing. *This is a recording of the VA Oticon More Introduction Event from May 3, 2021*
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
Oticon Government Services: Introducing Oticon More
Sound scenes are dynamic, complex and unpredictable. It is the role of the brain to handle this complexity to hear and make sense of it all. Oticon is committed to developing life changing technologies that support the way the brain naturally processes sound. Get ready to discover the new perspective in hearing care with a fundamentally new approach to signal processing. *This is a recording of the VA Oticon More Introduction Event from May 3, 2021*
36630
Online
PT60M
Oticon Government Services: Introducing Oticon More
Presented by Candace Depp, AuD, Thomas Behrens, MS, Danielle Tryanski, AuD, Sarah Draplin, AuD
Course: #36630Level: Intermediate1 Hour
AAA/0.1 Intermediate; ACAud inc HAASA/1.0; AHIP/1.0; ASHA/0.1 Intermediate, Professional; BAA/1.0; CAA/1.0; IACET/0.1; IHS/1.0; Kansas, LTS-S0035/1.0; NZAS/1.0; SAC/1.0
Sound scenes are dynamic, complex and unpredictable. It is the role of the brain to handle this complexity to hear and make sense of it all. Oticon is committed to developing life changing technologies that support the way the brain naturally processes sound. Get ready to discover the new perspective in hearing care with a fundamentally new approach to signal processing. *This is a recording of the VA Oticon More Introduction Event from May 3, 2021*
4
https://www.audiologyonline.com/audiology-ceus/course/genie-2-fitting-focus-series-36119
Genie 2 Fitting Focus Series: Oticon More First Fit
In this course we will cover the initial fitting steps for a successful Oticon More initial fitting using Oticon’s Genie 2 fitting software.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
Genie 2 Fitting Focus Series: Oticon More First Fit
In this course we will cover the initial fitting steps for a successful Oticon More initial fitting using Oticon’s Genie 2 fitting software.
36119
Online
PT30M
Genie 2 Fitting Focus Series: Oticon More First Fit
Presented by Amanda Szarythe, AuD, CCC-A
Course: #36119Level: Intermediate0.5 Hours
AAA/0.05 Intermediate; ACAud inc HAASA/0.5; AHIP/0.5; BAA/0.5; CAA/0.5; IACET/0.1; IHS/0.5; NZAS/1.0; SAC/0.5
In this course we will cover the initial fitting steps for a successful Oticon More initial fitting using Oticon’s Genie 2 fitting software.
5
https://www.audiologyonline.com/audiology-ceus/course/art-reflection-in-audiology-using-36635
The Art of Reflection in Audiology: Using the Ida Institute Reflective Journal in your daily practice
How can reflective practices help hearing care providers become mindful of the gap between the intention clinicians have to make appointments person-centered, and the reality of implementing person-centered care in daily clinical practice? What are the benefits of setting aside time to reflect? In this session, we will introduce self-development tools for analysis and reflective practice, including ethnographic videos and the Reflective Journal, which will help clinicians to understand their patients’ needs and preferences, as well as their own professional development needs, to improve the outcomes of appointments.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
The Art of Reflection in Audiology: Using the Ida Institute Reflective Journal in your daily practice
How can reflective practices help hearing care providers become mindful of the gap between the intention clinicians have to make appointments person-centered, and the reality of implementing person-centered care in daily clinical practice? What are the benefits of setting aside time to reflect? In this session, we will introduce self-development tools for analysis and reflective practice, including ethnographic videos and the Reflective Journal, which will help clinicians to understand their patients’ needs and preferences, as well as their own professional development needs, to improve the outcomes of appointments.
36635
Online
PT60M
The Art of Reflection in Audiology: Using the Ida Institute Reflective Journal in your daily practice
Presented by Natalie Comas, BSpPath, LSLS Cert. AVT
Course: #36635Level: Introductory1 Hour
AAA/0.1 Introductory; ACAud inc HAASA/1.0; AHIP/1.0; BAA/1.0; CAA/1.0; Calif. SLPAB/1.0; IACET/0.1; IHS/1.0; Kansas, LTS-S0035/1.0; NZAS/1.0; SAC/1.0
How can reflective practices help hearing care providers become mindful of the gap between the intention clinicians have to make appointments person-centered, and the reality of implementing person-centered care in daily clinical practice? What are the benefits of setting aside time to reflect? In this session, we will introduce self-development tools for analysis and reflective practice, including ethnographic videos and the Reflective Journal, which will help clinicians to understand their patients’ needs and preferences, as well as their own professional development needs, to improve the outcomes of appointments.


