Throughout the literature, one finds almost unanimous consensus over the major psychological and psychosocial deterrents for hearing impaired consumers' failure to seek help for their hearing and communication breakdowns. Consensus includes such behaviors as lack of awareness, denial, vanity, social stigma and skewed cost/benefit perceptions (Chartrand & Chartrand, 2004). Indeed, Ramsdell (1978) suggested some years ago that the most significant problems presented by unmitigated hearing loss were psychological, including depression and anxiety, defensiveness, distrust, and social paranoia. Van Hecke (1994) noted the need for development of better counseling methodologies to help hearing impaired individuals overcome negative emotional responses to hearing loss, while Herbst and Humphrey (1980) long ago noted the deleterious impact that hearing loss can have on quality of life for older adults who forego obtaining appropriate help.
Regarding social stigma and vanity, the hearing aid industry has gone to great lengths to overcome reasons why reluctant consumers have not been seeking help with hearing loss. Furthermore, cost/benefit issues have been addressed by numerous researchers (Sweetow, Bratt, Miller, & Henderson-Sabes, 2004; Peterson & Bell, 2004; Crandall, Kricos, & King, 1997). It is beyond the scope of this review to provide an in depth exposition of these and other psychosocial barriers to hearing care. However, these considerations are important for one to have a perspective of the factors for which consensus may not have yet developed, such as the negative impact on prospective consumers with hearing impairment who put off purchasing hearing aids because of someone else's hearing aid experience (Kochkin, 1999).
Indeed, it has been reported that a sizable segment of would-be hearing aid users have been discouraged precisely because of others' negative experiences (Chartrand, 1999). Furthermore, consumer websites are filled with alarm and caution about purchasing hearing aids, as if doing so is fraught with trust issues not as prevalent in other areas of healthcare (Bell, 2006; Berke, 2006; Goddard, 2006). This irrational ambivalence can only contribute to the psychosocial deterrents already keeping many individuals with hearing impairment from seeking help. Ross (2005) sums up the effects of such perceptions this way:
Everybody, it seems, has a friend or a relative who has had an unsuccessful experience with hearing aids, and is quite vocal about it. Many of these people, and there are too many of them, discourage potential hearing aid candidates from trying one, since they "know" that hearing aids are useless. Their attitude plays right into the usual reluctance to accept amplification. (p. 3)While some negative consumer attitudes appear to be changing (Bentler, 2000), others linger on, as the industry comes to grips over physiological and fit factors. Hearing Industries Association (HIA) annual reports indicate credit return rates ranging from 18% to 21%, or about the same rate as 20 or 30 years ago (Peterson & Bell, 2004; Ross, 2001; Kochkin, 1999). That translates into meaning that 18 to 21 of every 100 hearing aids manufactured are returned and scrapped or refurbished for sale. Of course, some of this may begin to change with the recent push with more non-occluding devices. The trends are now rapidly steering away from custom instruments and more toward OTE and BTE instruments, which show promise in removing some of the invasiveness of hearing instrumentation (Nemes, 2007). As recent as 2001, Bray, Johns, and Ghent (2001) reported that return for credits (RFCs) account for nearly 30% of manufacturers' initial cost of producing the next new hearing instruments. These costs go far beyond the cost of wasted parts and labor, but also in expenditures in customer service, billing, shipping, and costs associated with losing future business. Hence, those who keep their custom hearing aids are absorbing the cost of those that do not (Barber, 2005). In the case of over-the-ear (OTE), mini-behind-the-ear (mBTE), or behind-the-ear (BTE) instruments, the cost of returns is estimated at a loss of about 15% of the manufacturing cost, because most of these may be refurbished, restocked, and resold back to the market, provided the actual time period of trials is short, and wear and tear minimized (DigiCare, 2006).
Furthermore, studies published to-date show that some newer technologies and smaller-size instrumentation are burdened with a much higher RFC rate than the older, less costly technology. Admittedly, a sizable portion of this problem is imbedded in consumer expectations of cost-benefit (Peterson & Bell, 2004; Weighland et al., 2002). However, it is also arguable that a large part of the problem is that smaller instrumentation encroaches upon physiological dynamics located deeper into the external auditory canal (EAC) than do larger instruments. Sweetow et al. (2004) conducted a retrospective study in time-cost analysis between three groups of hearing aid users:
- Those that purchased and kept their hearing aids,
- those who exchanged their hearing aids for other models, and
- those who returned their hearing aids for a full refund.
Consequently, the higher the cost, the greater the expectation of benefits and an increased propensity to return instruments for a refund. Weighland et al. (2002) concurs with this finding, noting that in 2001, HIA reported a return rate of 57% for some advanced digital technology models, versus only 16.7% for old/low tech devices. And these studies do not even begin to address other major cost factors, such as factory shell or earmold remakes and innumerable in-office shell and earmold modifications, many of which still fail to satisfy complaints of discomfort, occlusion, or both (Chartrand, 2006).
Recently, the hearing aid industry has responded to the persistent problem of chronic returns for credit, remakes, and modifications—especially higher or more frequent for digital and smaller instrumentation—by investing heavily into the newer Open-Ear OTE, mBTE, and Receiver-In-The-Ear (RITE) instruments. These show promise for those with mild losses, or normal hearing in the low frequencies to moderately severe loss in high frequencies (Schweitzer & Jessee, 2006). However, many of these losses will eventually progress out of range of these configurations, requiring more lows and mids than any of these devices can provide (Rose, 2006; Chartrand & Chartrand, 2006).
Self-Assessment Studies and Reasons for Failure to Fit
In recent years, numerous self-assessment scales have been devised to gauge levels of consumer satisfaction with hearing aids. The most commonly accepted scale has been the Abbreviated Profile of Hearing Aid Benefit (APHAB), which is a shortened version of the much lengthier Profile of Hearing Aid Benefit (PHAB). APHAB is a 24-item self-assessment inventory on the functional before and after aspects of hearing aid adaptation and benefits (Cox & Rivera, 1992). Of its four subscales, ease of communication, reverberation, background noise, and aversiveness, none deal directly with physical discomfort complaints, sensations of occlusion, or own-voice problems.
A more recent scale of consumer perceptions is the Satisfaction with Amplification in Daily Life (SADL) scale. SADL is designed especially to measure quality-of-life perceptions for experienced consumers who have purchased new hearing aids (Cox & Alexander, 1999). Although the SADL invites even more frank consumer responses relative to problems with utilization of hearing aids, it does not include questions such as: "How does your own voice sound?", "Is there any physical discomfort after following the wearing schedule?", or "How long can you wear your hearing aids comfortably?" While consumer feedback on functional issues (vis a vis APHAB and SADL) are immensely important, equally important in terms of user compliance are own voice and comfort issues.
On the other hand, an analysis of the International Outcome Inventory for Hearing Aids (IOI-HA), a seven-item survey comparing outcome data from various research settings, reveals some inclusion of physical acclimatization issues (Cox, Alexander, & Beyer, 2003). Its co-authors note that aided outcomes negatively correlate closely to mean average and standard deviations of patient subjective perceptions in unaided state. In other words, the more difficulty consumers encounter in the unaided state, the less objection they exhibit toward artifacts of acclimatization.
Jenstad, Van Tassell, and Ewert (2003) conducted a hearing aid-user study with a post-fitting questionnaire covering five areas of complaints (gain, output, physical fit, compression characteristics, and unwanted sounds), and found that patients were very lucid in describing complaints relating to physical fit. Their scales of measure were particularly instructive in drawing out these kinds of concerns. Indeed, their findings agree with Resnick (1999), who reported from his study of consumer perspectives, that "the literature tends to emphasize [only] the electroacoustic characteristics contributing to improved performance" (p. 1) instead of testing out the validity and relevance of current consumer satisfaction measures. In an effort to determine the relationship of earmold fit and predicted real ear measures (and outcomes), Hoover and Stelmachowicz (2000) report a positive correlation between a good fit and patient perceptions of benefit (i.e., poor physical fit is often perceived as poor acoustic benefit). Meanwhile, Humes and Wilson (2003) show in a longitudinal study of nine hearing aid users that positive outcomes actually continue to improve even three years post-fitting, albeit gradually and incrementally.
Finally, in testimony before the U.S. Food and Drug Administration (FDA) Hearings Panel, in response to the Etymotic and Gudhear Petitions seeking approval of over-the-counter sales of hearing aids, Magelin (2004) provides an excellent review of the many physical complexities and variations that require keen professional skills to help patients accommodate to amplification. Thus, physical acclimatization success may be intricately intertwined with the skills and attention of a dispensing professional working personally with each new hearing aid user- something that cannot be afforded in a so-called over-the-counter practice setting.
Elasticity & Dynamicism of the Human External Ear Canal
It is entirely probable that some variations between user reports of discomfort, occlusion, and own-voice problems are mostly physiological. In other words, barring idiosyncrasies resulting from chronic illness, pharmacology, personal ear care habits, and levels of professional care, there are likely more similarities than differences between user experiences. These similarities are founded in the predictable, yet variable elasticity and dynamic nature of the ear canal itself. Oliviera et al. (2005) analyzed the ear canal volume changes that occurred in 67 subjects and found that 51% of subjects' ears exhibit dimensional changes of more than 10% by simply opening their mouths, while the remaining 49% showed significant changes up to 10%. In an earlier study by the same investigators, they found a range of ear canal changes of up to 20% in anterior displacement of the cartilaginous region of the external canal accompanying such movements as chewing, smiling, and speaking (Oliviera, Hammer, & Stillman, 1992; Oliviera, et al., 1992).
When one considers that the majority of ear impressions are taken in fixed mandible position, it is no wonder that problems of discomfort arise in so many hearing aid fitting cases. Pirzanski and Berge (2002) present data gathered from a survey conducted by 56 international doctoral audiology students participating in a distance learning course on earmold technology. They estimated from that survey that more than 50% of impressions result in poor earmold fittings from professionals' failure to recognize the dynamic aspects of the human ear canal. It was further noted that only 43% of survey respondents utilized dynamic impression techniques. In other research, failure to take dynamic ear impressions is a major contributor to failure to fit (Boys Town, 2006; Stakeholder Forum, 2001). Indeed, Robert, Funnell, and Laszlo (2005) identify a host of dynamic changes that occur on a perpetual continuum from the aperture of the EAC all the way to the manubrium of the tympanic membrane. These living changes conflict daily against inert earmold and hearing aid shell materials.
Natural, dynamic processes of the human ear canal tend to respond negatively to the fixed, inert materials of hearing aids and earmold, and tend to treat hearing aids and earmolds as invading foreign objects (Chartrand, 2003a). This dynamicism excites the mechanoreceptors imbedded within the tissues of the human epithelium each and every time movement occurs. A case in point is the acclimatization process involved in wearing a wristwatch. Passage of time and relative cessation of movement can cause neural firing to cease, in which case neural adaptation occurs (Nafe & Wagoner, 1941). However, because mandibular and neck and facial muscles, involved in smiling, chewing, talking, yawning, grimacing, etc., never cease movement, mechanoreceptors imbedded within the epithelium of the external ear canal continue neural firing until another control mechanism is activated: the parasympathetic process of a given reflex arc (Carlson, 2003). To subordinate and minimize the effects that movement causes in the dynamic ear canal, therefore, requires dynamic ear impressions that split the difference between dimensional extremes of change (anterior to posterior and superior to inferior) so that the adaptation process can be shortened for the hearing aid user (Chartrand, 2006). Hence, dynamic impression-taking alone can help minimize adaptation barriers to hearing aids. But there are other considerations for adaptation, most importantly the status and health of the layer of keratin that lines the external ear canal.
Role of Keratin in the External Ear Canal
In dispensing and audiological practice, perhaps the least known or appreciated anatomical feature of the EAC is the stratum corneum or keratin layer of tissue. Yet the health of the keratin layer determines the health of the human ear canal, which status can negatively or positively affect the success in hearing aid adaptation (Chartrand, 2004). The keratin layer is the outermost portion of the external ear canal (Johnson & Hawke, 1988). Its physiological role is critical in maintaining homeostasis and adapting comfortably to hearing aids. Yet, though easily viewed through video otoscopy, its status often goes unnoted during the normal course of dispensing activity (Chartrand, 2004).
Keratin is comprised of inorganic protein with no circulatory or neurological system. Chemically, its structure is almost identical to that of human hair and nails (Winter, Schweizer, & Goerttler, 1983; Merck, 2006). In the EAC it completely covers ultra-sensitive epithelial tissue, starting at a point near the umbo of the tympanic membrane and traveling the entire length of the canal lumen to the aperture or opening of the ear canal (Naiberg, Berger, & Hawke, 1984). Not unlike the proverbial elephant in the living room, keratin protein is arguably the most ignored part of the outer ear by hearing health professionals in general, and by hearing aid manufacturers specifically. So important is its role in maintenance of the human ear canal, that, as shown in Figure 1, a good, healthy layer of keratin in the human EAC and also an example of peeled keratin arising from systemic disease. EAC keratin is vital for:
- maintaining pH flora to prevent fungus, yeast, and bacterial infections
- preserving hydration of the EAC to allow homeostasis
- mixing sebaceous and cerumenous secretions
- keeping the ears clean during the desquamation process
- shielding the neuroreflexes of the EAC from oversensitivity
- adapting successfully to hearing aid earmolds
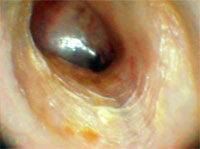

When outwardly migrating keratin approaches the ear canal lumen, it terminates just after contact with tiny hair follicles that grow inward, forming a kind of "ramp" that lifts the desquamated (dead) skin cells, keratin, and its cargo of debris from the epithelium. In turn, minute accumulations of dead skin cells, debris, and earwax are steadily deposited into the concha of the ear for easy removal (Jahne & Cook, 1997). Through otoscopy, keratin protein presents a "shiny" appearance as seen above in Figure 1. As underlying new tissue grows steadily and haltingly outward from the umbo of the tympanic membrane, its migration causes a "bunched up" appearance, forming circular "lines" around the wall of the ear canal. In cases of dehydration or in response to some medications these lines can be so close together as to appear granular (Chartrand, 2004; Johnson & Hawke, 1988).
Undisturbed, keratin is what shields the ear canal from bacteria, fungus, yeast, amoeba, and potentially septic debris. It also helps the epithelium or outer layer of skin tissue—when coated with cerumenous and sebaceous secretions (which together form "earwax")—to maintain a slightly acidic pH environment of about 6.5. Hence, keratin is the protective layer over the skin of the ear canal, without which the ear canal would be more susceptible to invasion, injury, and/or disease (Persaud, Hajioff, Thevasagayam, & Wareing, 2004; Slattery & Saadat, 1997). Consequently, the absence of keratin in the ear canal may contribute to many common complaints among hearing instrument users, such as:
- chronic itching
- hearing aid earmold discomfort
- over-vascularization of the TM (via trigeminal and facial nerve pathways)
- non-acoustic contact occlusion (via the Arnold's branch of the vagus nerve)
- predisposition for chronic externa otitis (fungal, bacterial, etc.)
- oversensitivity of the neuroreflexes of the EAC
So, if one were to place a piece of sand on the tympanic eardrum today, about three months from now that person could remove the same piece of sand from the bowl or concha of the ear by fingertip (Chartrand, 2004). Left undisturbed, healthy ear canals are self-cleaning and wax impaction is rare (Jahne & Cook, 1997). Abnormally low pH (below 6.5) often leaves the ear canal dry with a host of extant skin problems, such as psoriasis, eczema, chronic external otitis, contact dermatitis, allergy and abnormal cell growth such as basal and squamous cell carcinomas. After removal via cotton swab trauma or scratching with any foreign object, it requires about 10 to14 days for a good, strong layer of keratin to re-form. Hence, frequent use of cotton swabs will preclude keratin formation (Chartrand, 2004).
In addition, frequent use of ear preparations containing boric acid or hydrogen peroxide solutions not only destroy keratin and layers of epithelium, they also eliminate the water repellent ability of same and leave the external ear canal at risk for chronic otitis externa. Furthermore, these acids can inhibit cerumen formation, as well as interrupt natural desquamation of tissue and the regrowth of the badly needed keratin. Unfortunately, such harsh solutions are the mainstay of today's over-the-counter otopharmacopia. It must also be noted that an infected ear, or one in which immunology has been comprised, will generally not exhibit keratin (Winter, Schweizer, & Goerttler, 1983), just such an ear cannot normally secret cerumen and sebaceous secretions into earwax (Jahne & Cook, 1997). Thus, an external ear without visible keratin (via video otoscopy) may be considered an abnormal external ear (Chartrand, 2006).
Some common consumer and professional practices that inadvertently remove or disturb the vital keratin layer of the external ear canal and which can set up one's external canal for the above-described problems are:
- daily use of cotton swabs
- insertion of foreign objects
- frequent use of boric acid and/or hydrogen peroxide solutions
- aggressive cerumen removal
- dry and/or overly tight oto-block during impression taking
- forcing one-size-fits-all earmolds into the ear
Potential Medication Side-Effects Impacting the EAC
More than 180 prescription medications have been found to adversely affect the human cochlea (Edmunds, 2006; Briggs & Gadre, 2001). Indeed, these suspect medications garner the lion's share of research attention, while medications affecting the human EAC are only peripherally explored (Kavanaugh, 2007) compared to research with veterinary external ear issues (Haar, 2003). It is not our purpose to include a review of vestibular or cochlear ototoxicity, but instead to focus upon the less-explored external ear effects.
Table 1 lists medication classifications that have been found to adversely affect human epithelium and keratin, both directly and indirectly (Facts & Comparisons, 2006). Although most of these medications are generally not prescribed for ear-related conditions, they exhibit varying levels of effects upon hydration, immunological, and dermatitis issues. The effects of these otherwise helpful medications on the human EAC need to be considered when they appear to be causing cases of failure to fit. Moreover, perhaps the most universal effect is that the medications cause or contribute to dehydration. Some stimulate production and secretion of antidiuretic hormone (ADH) production, which can significantly affect electrolyte and cellular osmotic activity (Chartrand, 2007; Pagana & Pagana, 2002). Others interrupt homeostasis, delay healing, and interact adversely with other substances, including food and other drugs. Any medication that exacerbates chronic semi-dehydration causes a loss of keratin formation and sets the stage for chronic otitis externa problems (Chartrand, 2003b). These facts point to a need to keep in mind that pharmaceutical solutions were meant to be temporary, rarely permanent, solutions to healthcare issues until underlying causes can be addressed. To not follow that paradigm of healthcare risks setting up far too many individuals with hearing impairment with limited auditory rehabilitative options, namely hearing aids and cochlear implants.
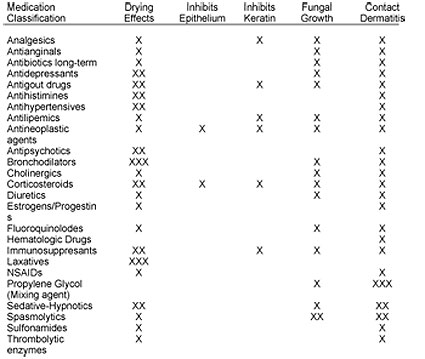
Table 1.
Medications Known or Suspected to Contribute to EAC Problems (Facts & Comparisons, 2006; Pagana & Pagana, 2002)
Conclusion
It is likely that the vast majority of consumer complaints relative to acceptance or rejection of hearing aids pertain to discomfort and own voice problems. At the same time, hearing aid self-assessment questionnaires tend to side-step these troublesome issues in favor of auditory and psychosocial perceptions. This is likely due to the paucity in the literature of definitive, explanatory information showing a strong link between hearing aid comfort and consumer perceptions. However, on an empirical level, working professionals see evidence of such a link in everyday practice.
In the meantime, the hearing aid industry continues to be plagued with consumer, medicolegal and regulatory agency misperceptions about the benefits and crucial need for hearing instrumentation. These chronic misunderstandings create an overly cautious and distrusting market, and contribute mightily to chronically suppressed sales of hearing aids. In addition, there is the historically chronic problem of excessive RFCs, factory remakes, and in-office modifications. These add cost pressures on the industry, while discouraging the next hearing impaired prospect from seeking hearing help.
More importantly, however, it is time for more research to engage in a frank discussion regarding the emerging data showing a link between hearing aid discomfort and own-voice issues and entrenched cases of failure to fit. Such considerations as the dynamicism the external ear, the need to recognize and counsel regarding the importance of keratin, and the neuroreflexes of the external ear, and the effects of underlying disease and medication side-effects must be explored and acted upon as an industry.
In doing so, we stand to reduce RFCs, remakes, and innumerable shell/earmold modifications. We might even remove cost pressures on the manufacture and sales of hearing instrumentation. Moreover, we may enjoy far fewer failure-to-fit cases and many more successes stories of lives changed positively because of advances in the field of hearing health.
About the Author

References
APHAB. (2006). Abbreviated Profile of Hearing Aid Benefit. University of Memphis, School of Audiology and Speech-Language Pathology. Retrieved May 2, 2006, from www.ausp.memphis.edu/harl/aphab.html
Barber, S. (2005, May 16). Hearing Aid "Sticker Shock" and Things to Consider When Purchasing. Healthy Hearing. Retrieved January 24, 2006, from www.healthyhearing.com/library/article_content.asp?article_id=710.
Bell, J. (2006). Why Purchasing a Hearing Aid is a Consumer Nightmare. Retrieved May 10, 2006, from www.bio.net/bionet/mm/audiolog/1997-September/003548.html
Bentler, R. (2000). Accepting New Truths in Hearing Aids. Healthy Hearing. Retrieved on May 9, 2006, from www.healthyhearing.com/library/article_content.asp?article_id=60
Berke, J. (2006). Your Guide to Deafness/Hard of Hearing. Retrieved on May 9, 2006, from deafness.about.com/mbody.htm
Boys Town. (2006). Areas of Research: Clinical and Behavioral Studies of Human Communication. Retrieved on May 4, 2006, from www.boystownhospital.org/Research/areas/ClinicalBehavioral/hearing_aids.asp
Bray, V., Johns, M.A., Ghent, R.M. (2001). Description and rationale of a digital, instant-fit hearing aid. The Hearing Journal, 54(4), 38-47.
Briggs, R.D., & Gadre, A.K. (2001, November 7). Ototoxicity. Grand Rounds Presentation, UTMB, Department of Otolaryngology.
Carlson, N.R. (2003). Physiology of Behavior (8th edition). Boston, MA: Allyn & Bacon.
Chartrand, M.S. (2007). How Much Water is Needed for Good Health? Colorado City, CO: DigiCare Hearing Research & Rehabilitation, www.digicare.org
Chartrand, M.S. (2006). Utilization of Neurophysiology of the External Auditory Canal in Resolving Problem Hearing Aid Fittings. International Institute for Hearing Instruments Studies, Livonia, MI.
Chartrand, M.S. (2004). The importance of the keratin layer in successful fitting and treatment. The Hearing Professional, July-August, 14-18.
Chartrand, M.S. (2003a, February 10). But What's Wrong with Q-Tips? Audiology Online, Article 407. Retrieved April 25, 2007, from the Articles Archive on www.audiologyonline.com Direct URL access at www.audiologyonline.com/articles/article_detail.asp?article_id=407
Chartrand, M.S. (2003b). Video Otoscopy Observation and Referral: The FDA Red Flags. The Hearing Professional, January-February, 9-14.
Chartrand, M.S. (1999). Hearing Instrument Counseling: Practical Applications in Counseling the Hearing Impaired, 2nd edition. Livonia, MI: International Institute for Hearing Instruments Studies.
Chartrand, M.S., & Chartrand, G.A. (2006). Resolving a Root Cause of Failure to Fit: Re-examining the Ear Canal. The Hearing Review. Retrieved April 25, 2007, from www.hearingreview.com/issues/articles/2006-03_14.asp
Chartrand, M.S., & Chartrand, G.A. (2004). If A Tree Fell in the Forest: What's Really Holding Back the Market? The Hearing Review, 10(10), 21-23.
Cox, R.M., Alexander, G.C., & Beyer, C.M. (2003). Norms for the international outcome inventory for hearing aids. Journal of the American Academy of Audiology, 14(8), 403-413.
Cox, R. M., & Alexander, G.C. (1999). Measuring satisfaction with amplification in daily life: The SADL Scale. Ear and Hearing, 20, 306-320.
Cox, R.M., & Rivera, I.M., (1992). Predictability and reliability of hearing aid benefit measurement using PHAB. Journal of the American Academy of Audiology, 3, 242-254.
Crandall, C.C., Kricos, P., & King, W. (1997, September 22-24). Long Term Consequences of Hearing Aid Utilization. Conference Reports. National Institutes of Health, Bethesda, Maryland.
DigiCare (2006). Annual Report to the Board of Directors. DigiCare Hearing Research & Rehabilitation, P.O. Box 19610, Colorado City, CO 81019, January 16, 2006.
Edmunds, A.L. (2006). Ototoxicty. eMedicine from WebMD. Retrieved January 15, 2007, from www.emedicine.com/ENT/topic/topic699.htm.
Facts and Comparisons (2006). Drug Facts and Comparisons 2006, 60th edition. St. Louis, MO: Wolters Kluwer Health.
Goddard, T. (2006). The Senior Citizen Protection Manual. Retrieved May 10, 2006, from www.azag.gov/seniors/spm.html#14.
Haar, G.T. (2003). The Importance of Ototoxicity. Retrieved January 10, 2007, from www.vin.com/proceedings.plx?cid=wsava2003&pid=6566&0=Ge
Herbst, K., & Humphrey, C. (1980). Hearing impairment and mental state of the elderly living at home. British Medical Journal of Clinical Research, 281, 903-905.
Hoover, B.M., Stelmachowicz, P.G., & Lewis, D.E. (2000). Effect of earmold fit on predicted real ear SPL using a real ear coupler difference procedure. Ear and Hearing, 21, 310-317.
Humes, L.E., & Wilson, D.L. (2003). An examination of changes in hearing-aid performance and benefit in the elderly over a 3-year period of hearing-aid use. Journal of Speech, Language, and Hearing Research, 46, 137-145.
Jahne, A.F., & Cook, E.W. (1997). Medical Issues Related to CIC Fitting. In M. Chasin (Ed.), CIC Handbook (pp. 53-68). San Diego, CA: Singular Publishing Group, Inc.
Jenstad, L.M., Van Tassell, D.J., & Ewert, C. (2003). Hearing aid troubleshooting based on patients' descriptions. Journal of the American Academy of Audiology, 14(7), 347-360.
Johnson, A., & Hawke, M. (1988). The nonauditory physiology of the external ear. In J. Santos-Sacchi (Ed.), Physiology of the Ear (pp. 41-58). New York: Raven Press.
Kavanaugh, K. (2007). Ear Canal Photographs. ENTUSA. Retrieved April 26, 2007, from www.entusa.com/external_ear_canal.htm
Kemp, R. J., & Bankaitis, A. E. (2000). Infection control for audiologists. In H. Hosford-Dunn, R. Roeser, & M. Valente (Eds.), Audiology Diagnosis, Treatment, and Practice Management, Vol. III. New York: Thieme Publishing Group.
Kochkin, S. (1999). Reducing hearing instrument returns with consumer education. The Hearing Review, 6(10), 18-20.
Magelin, G. (2004, February 4). Comments Opposing the Etymotic and Gudhear Petitions Docket Numbers 2003P-0362 and 2003P-0363. Testimony before the Division of Dockets, Food and Drug Administration, Rockville, MD.
Merck (2006). Function of Biotin. Retrieved April 26, 2007, from www.merckserono.net/servlet/PB/menu/1284910/index.html
Nafe, J.P., & Wagoner, K.S. (1941). The nature of pressure adaptation. Journal of General Psychology, 25, 323-351.
Naiberg, J., Berger, G., & Hawke, M. (1984). The pathologic features of keratosis obturans and cholesteatoma of the external auditory canal. Archives of Otolaryngology—Head & Neck Surgery, 110(10), 751-756.
Nemes, J. (2007). As communication technologies converge, dispensers have new opportunities. The Hearing Journal, 60(2), 17-20.
Oliviera, R., Babcock, M., Venem, M., Hoeker, G., Parish, B., & Vasant, K. (2005). The dynamic ear canal and its implications: The problem may be the ear, and not the impression. The Hearing Review, 12(2),18-19, 82.
Oliviera, R., Hammer, B., & Stillman, A. (1992). MRI of the external auditory canal. Audiology Today, 4(2), 48.
Oliviera, R., Hammer, B., Stillman, A., Jons, C., Margolis, R., & Holm, J. (1992). A look at ear canal changes with jaw motion. Ear and Hearing, 13(6), 464-466.
Pagana, K.D., & Pagana, T.J., (2002). Mosby's Manual of Diagnostic and Laboratory Tests, Second Edition. St. Louis: Mosby, Inc.
Persaud, R.A.P., Hajioff, D., Thevasagayam, M.S., Wareing, M.J., & Wright, A. (2004). Keratosis obturans and external ear canal cholesteatoma: How and why we should distinguish between these conditions. Clinical Otolaryngology & Allied Sciences, 29(6), 577-581.
Peterson, M. E., and Bell, T.S. (2004, January). Factors Influencing Hearing Aid Return and Exchange Rates. The Hearing Review, 11(1). Retrieved on March 5, 2006, from www.hearingreview.com/issues/articles/2004-01_01.asp.
Pirzanski, C., & Berge, B. (2002, March 18). Ear Impressions: Art or Science? Audiology Online, Article 336. Retrieved April 26, 2007, from the Articles Archive on www.audiologyonline.com Direct URL access at www.audiologyonline.com/articles/article_detail.asp?article_id=336
Ramsdell, R.S. (1978). The psychology of the hard-of-hearing and the deafened adult. In H. Davis & S.R. Silverman (Eds.), Hearing & Deafness. New York: Holt, Rhinehart & Winton.
Resnick, S.B. (1999). Breakdown in the fitting process; An idiopathic approach to Fitting: A Matter of Perspective. Retrieved November 9, 2005, from www.vard.org/mono/ear/resnick.htm
Robert, W., Funnell, J., & Laszlo, C.A. (2005, January 2). A critical review of experimental observations on eardrum structure and function. McGill University, Biomedical Engineering Unit and Department of Otolaryngology. Retrieved November 1, 2005, from funsan.biomed.mcgill.ca/-funnell/AudiLab/ear.html
Rose, D.E., (2006). The return of the earmold. The Hearing Review. Retrieved April 26, 2007, from www.hearingreview.com/issues/articles/2006-08_03.asp
Ross, M. (2005). Why People Won't Wear Hearing Aids. Rehabilitation Engineering Research Center on Hearing Enhancement. Retrieved May 9, 2006, from www.hearingresearch.org/Dr.Ross/why_people_wont_wear_hearing_aids.htm
Ross, M. (2001, November/December). Developments in research and technology. The Journal of Self-Help for Hard of Hearing People. Retrieved March 27, 2006, from www.hearingloss.org/html/ear_molds.html
SADL. (2006). Satisfaction with Amplification in Daily Life (SADL). University of Memphis, School of Audiology and Speech-Language Pathology. Retrieved May 2, 2006, from www.ausp.memphis.edu/harl/sadl.html
Schweitzer, C., & Jessee, S.K., (2006). The value proposition of open-fit hearing aids. The Hearing Review. Retrieved April 26, 2007, from www.hearingreview.com/article.php?s=HR/2006/09&p=3
Slattery, W. H. III, & Saadat, P. (1997). Postinflammatory medial canal fibrosis. American Journal of Otolaryngology, 18, 294-297.
Stakeholder Forum. (2001). Stakeholder Forum on Hearing Enhancement, Earmolds: Problem Statement. Retrieved April 27, 2007, from cosmos.buffalo.edu/t2rerc/pubs/forums/hearing/forum/earmolds/problem_statement.htm.
Sweetow, R.W., Bratt, L.A., Miller, M., & Hendeson-Sabes, J. (2004). A time-cost analysis with patients who purchase, return, and exchange hearing aids. The Hearing Review, 11(1). Retrieved April 27, 2007, from www.hearingreview.com/issues/articles/2004-01_02.asp
Van Hecke, M.L. (1994). Emotional responses to hearing loss. In J.G. Clarke and F.N. Martin (Eds.), Effective counseling in audiology: Perspectives and Practices (pp. 92-115). Englewood Cliffs, NJ: Prentice-Hall, Inc.
Weighland, J., Bodkin, K., Madell, J.R., Rosenfeld, R.M., & Press, I.L. (2002). By the numbers: A statistical analysis of hearing instrument returns. The Hearing Review, 9(1), 22-28, 49.
Winter, H., Schweizer, J., & Goerttler, K., (1983). Keratin polypeptide composition as a biochemical tool for the discrimination of benign and malignant epithelial lesions in man. Archives Dermatology Research, 275(1), 27-34.

