Although we cannot be certain, it appears that we are in the midst of a sea change in the way audiologists and hearing instrument specialists deliver care to patients. Not only do we live in a world where a reasonably good amplification system can be provided through a smartphone app (Amlani, Taylor, Levy, & Robbins, 2013), but professional hearing aid services are now scaled across hundreds of locations around the country with incredible operational efficiency. Additionally, as all of health care strives to reduce costs and improve quality, hearing care professionals of all stripes are tasked to provide value to patients, while maintaining healthy margins in order to sustain their business. Professionals have never been more challenged by a constellation of circumstances like the ones we face today.
The objective of this article is to provide a path forward for the independently owned hearing care practice. Using the best available knowledge, gathered from both inside and outside the industry, the aim is to help these independent hearing care professionals devise a coherent strategy that, when put into action, will combat the competitive forces changing the industry. Leveraging the traditional strengths of independent business, fondly referred to by many as the “mom and pop store,” this paper will review five drivers of a business strategy centered on customer intimacy, which is one of three dimensions of customer value first described by Treacy and Weirsema (1995) in their seminal book The Discipline of Market Leaders. By following the five strategic imperatives described in this article, independent hearing aid practices will be poised to thrive in the new era of healthcare.
Let’s begin by reviewing why many audiologists and hearing instrument specialists got into the hearing care business in the first place: the individual struggling with hearing and communication problems. Acquired hearing loss of adult onset is the third most chronic medical condition in the United States (Tinetti, Fried, & Boyd, 2012), and its debilitating condition is best described as a “triple threat” for the following reasons (J. Bakke, personal communication, July 27, 2013).
- Clinically significant hearing impairment is a disability with several debilitating consequences. This is an indication for effective remediation in its own right.
- Hearing loss interferes with a patient’s ability to be treated for other medical conditions because it hinders an individual’s ability to engage with their family doctor and understand their treatment advice and recommendations.
- Emerging research suggests that hearing loss may accelerate some disabilities such as cognitive dysfunction and vestibular impairment. The prevalence, co-morbidity and disabling effects of hearing loss underscore the need for aggressive preventive programs that identify conditions, such as hearing loss, which threaten health outcomes.
Perhaps the best way to describe the ill-effects of hearing loss is that it is a hidden handicap causing its sufferers long-term emotional pain and social isolation (Bouton, 2013). Although one in five Americans over the age of 15 suffers from hearing loss and are described as indifferent to the negative consequences of their conditions (Weinstein, 2013), for those seeking remediation, quality-of-life improvements are often the result (Mulrow, Aguilar, Endicott, Tuley, Velez, et al., 1990). Since an individual’s reaction to hearing loss is so personal and wonderfully diverse, it is only logical for patients to seek the help of a thoughtful, caring and nurturing professional who provides services in a comfortable environment.
To the reluctant, and oftentimes ambivalent, hearing-impaired individual, there eventually comes a time when help for their condition can no longer be placed on the back-burner. In a product-driven industry, individuals seeking a solution to their handicapping condition often are left to choose between various amplification devices advertised in local media. In a market rife with price-driven advertising, hearing-impaired individuals too often find the lowest price spotted in the newspaper very alluring. Given their relentless push to drive out costs and eliminate inefficiencies, big-box retailers are able to offer these low prices, but they may be poorly equipped to meet the varied and highly personal needs of the individual suffering from hearing loss. Thus, there is an opportunity for the independent practice to differentiate their offering in a relatively crowded marketplace.
Standing Out from the Crowd
Big-box retailers and other large corporate entities are formidable opponents for the independent practitioner. Their high in-store foot traffic, economies of scale and buying power allow them to excel operationally. This has proven to be a successful business model in many sectors of the economy, including hearing care, and it has a place within the marketplace, if for no other reason, there is a segment of the market desiring this type of delivery model. The operational advantages of the big-box retailer, however, may also be its Achilles heel, as it is nearly impossible to deliver an extra-ordinary level of personalized care and service in the relentless pursuit of low-price leadership and efficiency. It is the ability of the independent hearing care professional to make deep and lasting connections with individuals suffering the long-term effects of hearing loss that differentiates an independent practice from big-box retailers. Experts agree there is always a substantial number of consumers in any market desiring highly personalized service and an independent practice – who truly understands the delicate needs of the individual suffering from hearing loss is the best equipped to deliver it (Treacy & Wiersema, 1997).
As Figure 1 shows, businesses can create customer value and create a competitive advantage along three distinct dimensions: product leadership (the best product), operational excellence (the best total cost), or customer intimacy (the best total solution). This theory is known as the discipline of market leaders (see https://www.business-wisdom.com/articles/ArtclDisciplineOfMarket.html). Research has shown that market leaders make a deliberate choice to be the best at just one of these three dimensions, while offering an acceptable level of competence along the other two dimensions. The most successful businesses make a conscious decision, after carefully assessing their marketplace, to offer unprecedented and unique value along one of these three dimensions. Regardless of your chosen discipline, customer satisfaction, word-of-mouth referrals and profits are the by-product of the execution of this strategy.
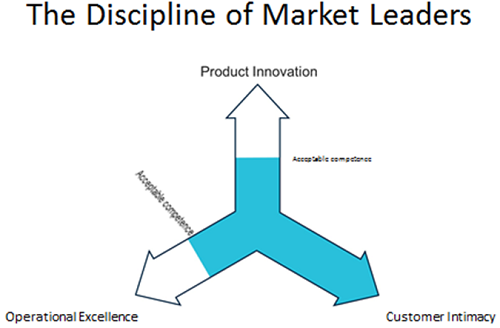
Figure 1. The Three Value Disciplines. An acceptable level of competence is needed in the two disciplines businesses choose not to lead in.
In order to compete against the growing presence of big-box retail chains, it is imperative for the independent practice to put customer intimacy at the center of their value proposition. After all, it is the personal guidance and expertise, tailored to each individual that you see that sets the independent apart for others offering a similar service. A by-product of this strategy will be higher patient satisfaction, increased word-of-mouth referrals and more annual revenue (Treacy & Wiersema, 1997). In order to bring to life the customer intimacy value proposition, practices must provide a more compelling patient experience that stands out from the din of ordinary. A systematic review of several businesses – many of them outside the hearing care marketplace, reveal the following five key drivers of customer intimacy (Treacy & Wiersema, 1997).
Customers, Primary Care Physicians, and Independent Businesses
The first key driver of customer intimacy is the ability to form deep, long-standing relationships with three distinct groups: customers, primary care physicians and other independent businesses within your community.
Regardless of the size of your market, there are likely to be several other independent businesses. The pillar-of-community mindset allows you to reach out and establish a network with all small, independent community businesses, from the local flower shop to the local barber. All independent business have more than a few things in common. Unlike big-box retailers, independent businesses typically are involved in all aspects of service delivery, from the negotiation of price with their vendors to interaction with customers to washing the floors. This level of involvement is a natural path to developing a support system with other likeminded independents. This support system is often an avenue for receiving word-of-mouth referrals, because independents are naturally inclined to support their fellow independents.
One important core group of community members are primary care physicians (PCPs). Given the rise of Accountable Care Organizations, PCPs are playing a more active role in orchestrating the care of patients. This is especially true of patients that are more likely to need the services of a hearing care professional, such as those that are elderly or suffering from a co-morbid, chronic medical conditions. Independent hearing care providers have the agility to foster deep, long-standing relationships with PCPs, and this advantage will only become more pronounced as healthcare policy continues to move from a procedure-based system to a preventive-care, value-based system.
Every business enterprise must make conscious decisions about their competitive advantage, quality of their service and price. Big-box retailers tend to pursue a competitive advantage through scaling and buying power. In their pursuit of scale, quality of service is achieved through standardization, while buying power is used to optimize their profits. Independent practices, on the other hand, must operate differently. The natural advantage of the independent is their holistic approach to running their business and the heart of this all-inclusive approach is the ability to form deep, long-standing relationships with the three groups shown in Figure 2.
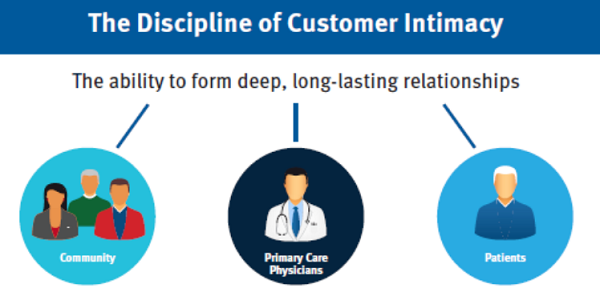
Figure 2. Three groups – community, PCPs and patients – need to be reached to achieve pillar-of-community status.
Patient-driven, Comprehensive Service Delivery Process
The second key driver of customer intimacy is the consistent use of a patient-driven, comprehensive service delivery process. Due to big-box retail’s ability to provide exceptional value along the dimension of operational excellence, independent practice must rethink how they deliver services if they expect to differentiate their offerings to the market. Gone are the days when an independent practice could simply hang a shingle, advertise their digital technology and conduct routine service delivery. Quite simply, that value proposition is no different than what is offered by a big-box retail chain.
Independents must innovate in the area of customer intimacy if they expect to thrive in a more competitive business climate. Making the conscious decision to become a market leader along the dimension of customer intimacy is likely to require innovation in how services are delivered to patients. One area rife for new ideas to be put into action is with the routine delivery of hearing aids. When properly executed, the selection and fitting of hearing instruments is often time-consuming and complex for the service provider, but with some creativity, it can be turned into an engaging and memorable series of personal interactions for the patient. By intertwining a theme, using memorabilia and signature moments into a standardized, evidence-based process, each patient can not only be successfully helped, but emotionally touched in a profound way. The consistent use of a comprehensive service delivery process is a key driver of the customer intimacy value proposition strategy. Customer intimacy leaders in a range of healthcare industries have made the conscious decision to design and create truly memorable patient experiences, while simultaneously relying on evidence-based practice principles that allow patients to make informed decisions about their hearing care.
The three best practices that will allow you to become recognized for service that stands out from the pack are to develop a theme, stage memorable experiences along six staging areas, and blending evidence-based practice with personalized service. To learn more about how the concepts of patient experiences can be applied to an independent audiology practice, see Taylor (2012).
Develop a theme. A theme is nothing more than an organizing principle that guides behavior of you and your staff. It influences every element of the patient experience across six staging areas. An effective theme is one that is easily identified by a wide range of patients. Using the senses of sound, sight and touch, you can bring your theme to life. Since it is incumbent upon every practice to create their own theme, work with your entire staff to identify it. Some common themes used in medically-oriented practices include movie musicals, televisions shows from the 1950s and old movies. Since we are in the business of improving hearing, you may want to be find a theme that has a lot of opportunities to use sound. As you may have gathered, theming is much more than re-decorating your waiting room. An effective theme is interwoven throughout the patient journey along the six distinct staging areas shown in Figure 3.
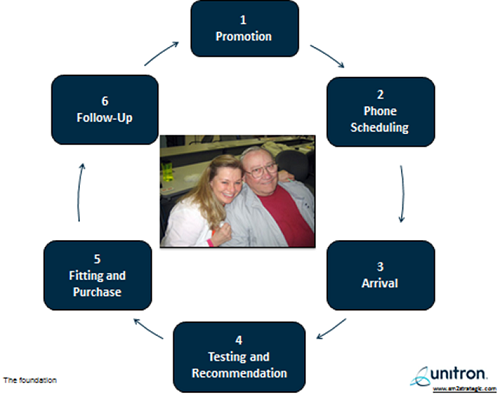
Figure 3. The six patient staging areas of patient-centered care.
Stage memorable experiences along six staging areas. From a patient’s perspective, there are six critical components to their interaction with a patient. Each one of these so-called staging areas (also called “touch points”) is an opportunity to contribute to a transcendent patient experience. Customer intimacy leaders are able to successfully orchestrate a memorable patient experience along these six staging areas (Figure 3) with the use of memorabilia and signature moments. Signature moments are really nothing more than your ability to take a routine clinical procedure and through the judicious use of memorabilia and effective communication skills turn them into occasions that patients are more likely to talk about after leaving your office.
Blending evidence-based practice with personalized service. Customer intimacy leaders know that they must go the extra mile if they are to be better and different than their big-box retail chain competitors. Another underpinning of tireless, personalized service is the use of evidence-based principles that guide the patient-provider interaction. 2010 MarkeTrak data (Kochkin, Beck, Christensen, Compton-Conley, Fligor, et al., 2010) indicate that providers using a comprehensive clinical protocol, including the use of verification, validation and speech-in-noise testing, are much more likely to create highly satisfied patients on a more consistent basis. Another recent study (Stika, Ross, & Cuevas, 2002) indicated that 77% of patients were “definitely satisfied” or “satisfied” with the service received from their hearing care professional. However, this same study showed several significant gaps in the service delivery process. For example, fewer than 10% of patients reported that they were asked to complete a self-report of hearing aid outcome or to participate in group counseling and orientation meetings - two procedures that have been associated with higher levels of patient satisfaction. Clearly, there is an opportunity to differentiate based on personalized service delivery.
Based on the reports cited above, a comprehensive clinical protocol may include:
- QuickSIN to measure unaided signal-to-ratio (SNR) loss
- Use of solution-based interviewing questions
- Needs assessment using TELEGRAM
- Use of a patient journal to document outcomes over first two weeks of use
- Verification of match of prescriptive target using probe microphone measures
- Validation of relative benefit 30 days post fitting
- Provision of aural rehab and auditory training sessions in either an individual or group format
The delivery of a comprehensive service delivery process goes beyond the face-to-face interaction of the clinician with the patient at the time of the testing and fitting. As Figure 3 suggests, there are six critical interaction points, and several of them involve other important members of the practice’s customer facing team. Moreover, we have all come to expect that digital processing power will incrementally improve. This is truly a godsend for our hearing-impaired patients who rely on us to provide them with the most innovative technology at a fair price. The problem, however, is that all service providers have better and faster technology compared to just a few years ago - and this paradigm is not going to change anytime soon. The antidote to faster, smarter and cheaper digital processing power is personalized service, and the only proven way to orchestrate it is to create and execute a comprehensive service delivery process based on these cornerstones:
- Personalized Service
- Warm, Friendly & Inviting Environment
- Engaging & Knowledgeable Staff
- A Brand Centered on YOU -- Not the Device
Quality Face Time with Patients
The third key driver is quality face time with patients. Many patients would agree that quality face-to-face time with the service provider is one of the most essential aspects of receiving high-quality care. In a frantic rush to see as many patients as possible, medical professionals often forget that their ability to engage in an unhurried dialogue with patients is one of the cornerstones of an outstanding service delivery process. Leaders in the dimension of customer intimacy know that spending a few extra minutes with each patient is more likely to result in a successful outcome and more word-of-mouth referrals. Additionally, research from the medical arena supports that notion that face-to-face communication enhances the effectiveness of the professional’s intervention.
Specifically, Zolnierek & DiMatteo (2009) conducted a meta-analysis of more than 100 studies and found that physicians who practiced patient-centric communication with their patients were more likely to follow their recommendations. Although it may be stating the obvious, it is the responsibility of the entire customer-facing team to enhance their “face time” with patients.
One way to increase the level of “face time” with individual patients is through the use of motivational interviewing. Motivational interviewing is perhaps best described as a method of asking open-ended questions to patients as you attempt to facilitate behavioral change in the individual. An excellent source for learning more about motivational interviewing is Greer Clark and English’s (2013) new book, Counseling-Infused Audiologic Care.
Specifically, both research and real-world experience suggest hearing aid dispensing practices that enhance their interactions with patients in three key areas are more likely to have higher levels of patient satisfaction and greater profitability. By taking the time to rethink the workflow of your practice and coach your customer facing employees, including front office professionals (FOPs), you will be on your way to becoming a customer intimacy leader in your marketplace. The three best practices listed below are designed to help you differentiate your practice with personalized customer service.
Warm and friendly phone rapport. These days it seems like everyone complains about the quality of service they receive over the telephone. If you are lucky to actually talk to a live voice, the service representative is likely to be residing in a location that is several time zones away and not well versed on your personal situation. Answering the phone effectively is a skill that can differentiate your practice. Like everything, personalized telephone service requires planning, training and managerial oversight.
The personalized in-person greeting. Another way to enhance your face time with patients is to adapt workflow so that FOPs spend a bit more time personally greeting patients when they arrive in your office. In an audiology practice you often work directly with individuals who are nervous and apprehensive about their inability to hear. Of course, this is a natural by-product of hearing loss of adult onset. An important role of the FOP is to recognize some of the normal behaviors of an adult with gradual hearing loss, such as denial, avoidance, and even hostility, and have some communication strategies to put patients at ease about their appointment.
Taking the time to fine-tune the details of how the FOP should greet a patient upon arrival is critical to any office culture that wants to be a market leader in customer intimacy. When a patient arrives in your office, he should be greeted as if he was a well-respected Hollywood actor or a member of the British royal family. In addition to proper eye contact, the FOP needs to stand up and acknowledge the patient at the check-in desk. Smiling and shaking their hand are other components of a warm greeting.
The final stages of the in-person greeting should comprise providing a warm verbal greeting, asking the patient to provide any information, such as insurance card, and guiding the patient to a seat in the reception area. It also helps to advise the patient of activities they can do in the reception area and about how long they may have to wait to see the audiologist. Of course, when patients have been waiting more than about 15 minutes, the FOP needs to personally check with the patient to see if anything is needed. In short, patients need to be greeted in your practice like you would greet a good friend you have not seen in a long time.
Personalized counseling. In an era of automation and artificial intelligence, there is still no substation for face-to-face human interaction. Perhaps the most competitive advantage of the independent practitioner is their ability to personalize their counseling approach in order to meet the individual needs of the patient. Individualized counseling is typically spread over several face-to-face visits with the patient.
The relationship between quality “face time” and higher patient satisfaction is well known. MarkeTrak data (Kochkin, 2003) suggests that clinicians who spend an average of approximately two-and-a-half hours of collective time with each patient are more likely to have patients with higher levels of patient satisfaction. This “face time” is spread over the course of three to four appointments and is comprised of the initial hearing evaluation/consultation, the hearing aid fitting and one or two follow-up appointments during the 30-day evaluation period. In general terms, customer intimacy leaders would be best served to design their office so that they can spend time with patients in the following increments.
- Initial Evaluation / Consultation: 60 to 90 minutes
- Hearing Aid Fitting: 60 Minutes
- Routine Follow-up Appointments: 30 minutes each (typically two visits)
Optimizing “face time” is not simply about spending more time with patients. As this MarkeTrak study (Kochkin, 2003) suggests, practices that spend too much time with patients run the risk of having below-average patient satisfaction ratings, likely because patients lose faith in your ability to solve their problem.
Like artisan farmers and craftsman, customer intimacy leaders recognize that the “right” amount of quality time spent face-to-face with each patient will vary depending in their specific needs. A by-product of optimizing the quality of the face-to-face interaction is higher overall patient satisfaction and a greater number of word-of-mouth referrals. Compared to big-box retail operations that have been designed to use a cookie-cutter approach in order to optimize efficiency, customer intimacy leaders recognize that their true value rests with a keen ability to take the time to gain a deeper understanding of the needs of each patient.
Using Analytics to Improve Productivity
The fourth key driver of customer intimacy is using analytics to improve productivity throughout the employee growth cycle. In today’s uncertain economic climate, one of the primary goals of any business is to hire and motivate the best people for each job with the practice. The most successful companies know that matching the right candidate to the performance requirements of each job is a huge strategic advantage that ultimately reduces long-term costs and optimizes productivity. Practices that make the conscious decision to lead on the dimension of customer intimacy understand it is imperative to find and keep the best people, because the sustainability of their practice greatly depends on the quality of their people. The objective of this paper is to show how computer-based job performance modeling and real-time collection of key performance indicator (KPI) data improves both organizational performance and practice productivity in three distinct ways.
Job matching. Traditionally, managers and practice owners have largely relied on some combination of the job interview and reference checking to arrive at a hiring decision. Although these are certainly necessary parts of the hiring process, studies suggest that only 10% of a person’s behavioral style and ability can be observed using these methods. When a comprehensive cloud-based career profiling and job matching tool is added to your hiring process, research demonstrates that the probability of hiring a highly engaged and productive employee jumps from 40% to 75% as shown in Figure 4. Customer intimacy leaders in several industries routinely use job matching tools to make better hiring decisions.
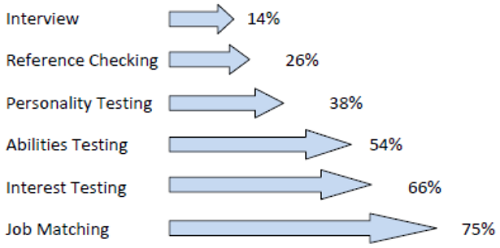
Figure 4. The blending of each of these tools and procedures to the hiring process improves your chances of hiring the best person for each job in your practice. Source: Profiles International. Used with permission.
Career management. Once a manager has made a hiring decision, opportunities to maximize that employee’s potential do not stop. Historically, even the most effective managers have relied on intuition to guide and coach their staff to peak performance. This instinctive approach, however, leaves much to chance. Recent research (J. Gibbs, personal communication, October 26, 2013) suggests that 78% of productive employees leave a job due to poor relationships with their manager. Managers that first understand their thinking and behavioral style are better equipped to begin the process of understanding the thinking and behavioral style of their employees. Cloud-based profiling tools can also be effectively used to assess the thinking and behavioral style of their entire staff.
According to Figure 5, several dimensions of thinking and behavioral style can be profiled and compared to the thinking and behavioral style of top-performing audiologists, hearing instrument specialists and front-office staff from around the country. Keeping in mind there is no “wrong” answer, you can gauge the personal style of your staff in relation to top-performers along 14 dimensions. The information gathered from a career profiling tools allows you to provide customizable coaching that is in alignment with the social style of the individual employee. This type of precise coaching and performance management, when combined with effective communication, allows you to develop better relationships with your staff, improve performance and reduce turnover.
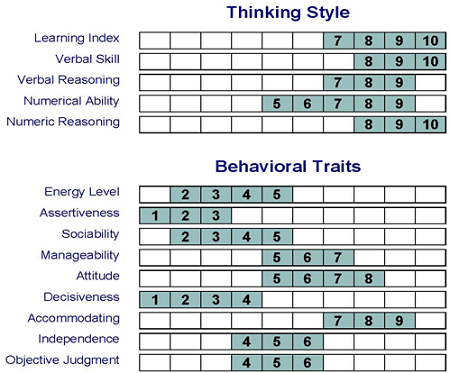
Figure 5. The 14 dimensions of a career profiling tool. Source: Profiles International. Used with permission.
Key Performance Indicator management. Computer-based analytics can also be used to measure key performance indicators (KPIs), which form the backbone of data-driven decision making. KPIs such as conversion rate, appointments per day and return rate can be measured and compared to industry standards. Managers can use this information to make better decisions about how they want to operate their business. Recent reports have shown that practices utilizing cloud-based systems to capture daily KPIs are 30 to 40% more productive (B. Savage, personal communication, December 23, 2013).
Practices that use computer-based profiling tools have the ability to work smarter, not harder, to improve the overall productivity of their business. This starts with your ability to match the right person for the performance requirements of your practice. This is especially critical for customer intimacy leaders that set themselves apart from the competition because their staff offers the most comprehensive and personalized “human touch.” Although it may seem to be somewhat paradoxical, independents in a range of industries that lead on the dimension of customer intimacy effectively utilize computer-based profiling and KPI tools throughout the employee growth cycle to better understand the human side of their business.
Use of a Service-Based Pricing Strategy
The fifth driver of customer intimacy is use of a service-based pricing strategy. Historically, the hearing care industry has relied on margin-based pricing to determine what customers will pay. A margin-based strategy implies that the office manager negotiates the cost of goods for each device purchased from a manufacturer, and then carefully calibrates the retail price that will allow the practice to cover expenses and make a marginal profit. This is a perfectly fine strategy for establishing your prices, but it may not be the best for unlocking the true value of professional services provided to patients. Now that independent providers are feeling the squeeze from big-box retailers and their incredible operational efficiency, it is time to reconsider this traditional way of pricing, which is no longer very effective. Service-based (also called value-based) pricing is an alternative to margin-based pricing.
The key to understanding service-based pricing is thinking like a customer. Characteristics such as convenience, performance and, above all, service determine how much customers are willing to pay for something. The more we value a certain attribute (and the harder it is to find reasonable next-best alternatives) the more we are willing to pay for it. If you pride yourself on offering premium levels of personalized service and attention, then you need to develop a pricing structure that reflects it. Service-based price strategy may be your antidote to the incredible buying power and awe-inspiring operational efficiency of large retail chains.
The key to shifting from a margin-based to a service-based pricing strategy centers around your ability to create itemized bundles of services that accurately reflect your unique value proposition. If you have made the conscious decision to lead on the dimension of customer intimacy, then these itemized bundles need to signal to the market that your practice offers unsurpassed “high-touch” service and professionalism, in addition to innovation products. Here are the five essentials of implementing a service-based pricing strategy.
Determine your competitive advantage. In relation to your direct competitors, identify the things you do better or differently that cannot be easily duplicated by others in your market. Customer intimacy leaders typically hold a decisive competitive advantage around the quality of “face time” spent with patients and the overall professionalism of their comprehensive service delivery process. An independent practice’s competitive advantage oftentimes can be very unique, so take some time to identify it.
Optimize your cost-of-goods within three to four product tiers. With the help of your “numbers person,” strive to optimize the dollar value you pay manufacturers for products. Unlike big-box stores and retail chains, independent practices lack economies of scale, and that is okay. You may still have some genuine opportunities to lower your cost-of-goods by committing more business to fewer manufacturers and negotiating better prices with them. In addition to a thorough analysis of COGs, identify your breakeven point. Finally, strive to simplify by tiering all products you dispense into three or four price points.
Create a list of value-added features. Most practices stop at the second point above, and that is fine if you are using a margin-based strategy. However, you may be missing real opportunities to add patient value and increase your margins. By creating a list of all of the additional items patients might be willing to pay more for or need, you are taking a critical step in creating service packages that reflect your competitive advantage in your marketplace. Here is an example of such a list.
- Remote control
- Companion microphone
- Wireless accessories
- Dry & Store Global II unit
- Additional warranties
- Comprehensive aural rehab services
- Additional batteries
- Unlimited service visits
Determine your minimum service bundle offering. Sometimes known as your “line in the sand,” this is the first big step toward establishing service-based price bundles. Rather than making the device the center of your pricing strategy, this step allows you to place service and professionalism upfront. Importantly, this is your opportunity to ensure that your service bundles reflect your competitive advantage. You can complete this step by asking yourself, “What is the minimum level of service and technology that I am willing to offer patients in my marketplace?” Of course, your answer to this question is unique to the mission and vision of your independent practice. An example of one practice’s service minimum service bundle looks like this.
- Diagnostic evaluation (unbundled and billed to insurance, if applicable)
- Pair of devices (entry-level technology)
- 1 year of follow-up office visits
- Group hearing aid orientation classes
- One-year warranty/loss & damage
Notice that the service components of office time and group orientation classes are bundled with a pair of devices. The basic idea here is that you are packaging items that you know to be effective for the typical patient - face time with you, an aural rehab support group and a bilateral fitting of entry-level product.
Create three to four itemized service bundles. Once you have created your value service bundle at a relatively low price point, the next step is to scale up to an additional two or three service bundles. The main idea here is to add more technology, additional services as well as other perks that patients may want or need. Here’s an example of three service bundles from one practice. Independent practices are encouraged to be on the constant lookout for novel and exciting items they can add to the premium service bundle. Notice that there are just three bundles, and as the price increases both the product and the service becomes more sophisticated:
Level 3: Premium Service Package
- 2 Devices – premium level technology
- 3 year warranty and supply of batteries
- 3 year comprehensive care plan – unlimited office visits
- 2 wireless accessories
- Dry and Store unit $_________
Level 2: Mid-Level Service Package
- 2 Devices – mid-level technology
- 2-year warranty and supply of batteries
- 2-year comprehensive care plan – unlimited office visits
- 1 wireless accessories
- Dry and Store unit $_________
Level 1: Economy Service Package
- 2 hearing aids – entry level technology
- 1-year warranty
- 1-year comprehensive care plan $_________
Pricing is a complex task requiring input from financial as well as billing and coding experts. I urge readers to seek their involvement whenever you begin the process of updating or changing your price strategy. Whatever your final service bundles shape up to be, strive to keep them simple. Customer intimacy leaders in all businesses recognize the urgent need to use price as a signal to the market that your offer is remarkable and distinct from your competitors. In our industry, this can be done by creating itemized bundles that wrap professionalism and service around innovative products per the example above.
The Importance of Culture and Standards
Mastering the necessary skills required to be a market leader in the dimension of customer intimacy requires effort and commitment. Your ability to shift away from a transnationally-based workflow, similar to how big-box retailers operate, to one that takes a more artisan approach involves creating an office culture committed to bringing the five drivers of customer intimacy to life in your practice. Independent practices that foster a genuine curiosity for each patient are more apt to become customer intimacy experts. Best practices surrounding the creation of a culture committed to service excellence involves the behaviors listed below. The primary role of the manager or owner of the independent practice is to instill these behaviors in your staff. Thought leaders in this area suggest that the most successful businesses do three specific things in their pursuit of excellence.
- Vision – Clearly and simply articulate why your practice must build a thriving culture around the five drivers of customer intimacy.
- Alignment – Ensure that all staff members understand the practice’s vision and their role in creating it.
- Execution – Provide training, establish expectations and build trust within staff so that they can complete the day-to-day activities that result in becoming a customer intimacy leader.
References
Amlani, A. M., Taylor, B., Levy, C., & Robbins, C. (2013, April). Improving hearing aid adoption rates through smartphone applications. Learning Module presented at the annual meeting of the American Academy of Audiology, Anaheim, California.
Bouton. K. (2013). Shouting won’t help: Why I and 50 million other Americans can’t hear you. New York, NY: FSG Books.
Greer Clark, J., & English, K. M. (2013). Counseling-infused audiologic care. Upper Saddle River, NJ: Pearson.
Kochkin, S. (2003). MarkeTrak VI: On the issue of value: hearing aid benefit, price, satisfaction and brand repurchase rates. The Hearing Review, 10(2), 12-25.
Kochkin, S., Beck, D. L., Christensen, L. A., Compton-Conley, C., Fligor, B.J., Kricos, P.B., McSpade, J. B., et al. (2010). MarkeTrak VIII: The impact of the hearing healthcare professional on hearing aid user success. The Hearing Review, 17(4), 12-34.
Mulrow, C. D., Aguilar, C., Endicott, J. E., Tuley, M. R., Velez, R., Charlip, W. S., Rhodes, M. C., et al. (1990). Quality-of-life changes and hearing impairment: a randomized trial. Annals of Internal Medicine, 113(3), 188-194.
Stika, C. J., Ross, M., & Cuevas, C. (2002). Hearing aid services and satisfaction: the consumer viewpoint. Hearing Loss, 23(3), 25-31.
Taylor, B. (May, 2012). Modernizing your practice in uncertain times: testing and recommendation phase of the patient journey. Audiology Online, Course 20554. Retrieved from https://www.audiologyonline.com
Tinetti, M. E., Fried, T. R., & Boyd, C. M. (2012). Designing health care for the most common chronic condition – multimorbidity. Journal of the American Medical Association, 307(23), 2493-2494. doi: 10.1001/jama.2012.5265.
Treacy, M., & Wiersema, F. (1995). The discipline of market leaders: Choose your customers, narrow your focus, dominate your market. New York, NY: Perseus Books.
Weinstein, B. (2013). Tool kit for screening otologic function of older adults. American Journal of Audiology, 22, 179-182. doi: 10.1044/1059-0889(2013/12-0057).
Zolnierek, K. B., & DiMatteo, M. R. (2009). Physician communication and patient adherence to treatment: a meta-analysis. Medical Care, 47(8), 826-834. doi: 10.1097/MLR.0b013e31819a5acc.
Cite this content as:
Taylor, B. (2014, February). The discipline of market leaders: the five key drivers of customer intimacy. AudiologyOnline, Article 12446. Retrieved from: https://www.audiologyonline.com