Learning Outcomes
After this course learners will be able to:
- List the candidacy criteria for Baha systems for both Single-Sided Deafness (SSD) and Mixed and Conductive Hearing Loss.
- List three ways clinicians can demonstrate Baha systems to their patients.
- Identify important points for counseling a candidate and list resources that are available to support Baha candidates.
Introduction
Good morning everyone. Thank you so much for joining us to learn more about Baha Technology and Candidacy. My name is Mary Beth O'Sullivan. I'm an audiologist and a Professional Education Manager for Cochlear Americas. At Cochlear, we believe in creating the most up-to-date, relevant and clinically valuable content for audiologists. We welcome your suggestions for future courses. This course is part of our Foundations of Baha Implant series, which is designed for audiologists who are new to working with bone conduction and implants. I do invite you to check out some of our other courses offered through AudiologyOnline. Today's focus is candidacy.
We like to start every session with a reminder of our mission here at Cochlear.
- We help people hear and be heard.
- We empower people to connect with others and live a full life.
- We transform the way people understand and treat hearing loss.
- We innovate and bring to market a range of implantable hearing solutions that deliver a lifetime of hearing outcomes.
Personally, over my 20 years as an audiologist, I have shed many tears of joy and grief with patients as they go through the process of finding a solution that works for them. At Cochlear, our technology is constantly improving and enhancing the quality of life for our patients.
Indications for Baha Technology
Before we discuss the indications for Baha technology, it is important to understand how it works. The fundamental way that the Baha technology works is through osseointegration, the process by which living bone tissue bonds with titanium. We often think of bone as a hard, non-evolving material, kind of like rock. In fact, bone is a dynamic and growing tissue. The Baha implant is made of titanium, which is known as a scavenger metal because it actively tries to form a bond with other materials. That's why titanium is so effective for Baha implants. Living bone will form a bond with the titanium over time. As such, after surgery, we allow a period of time for that osseointegration to occur. This integration allows the strong bond which enables the sound transmission through the bone that is unique from other hearing interventions, such as hearing aids.
Why should clinicians and surgeons consider Baha Technology over other treatment options? Baha technology offers several unique advantages because of its ability to transmit sound directly to bone. First, it works independently of the ear canal and middle ear, resulting in direct transmission which allows for a clear and natural sound. Another unique benefit over other surgical treatments for hearing loss is that pre-operative testing is possible. A demonstration with a sound processor allows the recipient to experience the potential for improvement. You can predict with a certain degree of accuracy how someone will do after surgery. Coming up shortly, we will offer some suggestions for demonstrations and trials that should be helpful for you.
Another benefit of Baha is that it has high wearing comfort. Many patients forget they even have it on. Recipients enjoy that there is nothing in the ear and patients with single-sided deafness particularly appreciate that nothing is occluding the natural hearing of the good ear. Additionally, the procedure is safe and straightforward and the Baha Connect surgery can be potentially as short as 10 minutes. Finally, Baha offers a predictable outcome. As we mentioned, patients know what they are going to hear with the Baha before surgery, which adds peace of mind for you and for your patients.
There are two main groups of individuals who can benefit from the Baha system: those with conductive and mixed hearing loss (CMHL) and those with single-sided deafness (SSD). Relevant to our discussion today, it is important to note that the FDA has cleared surgical solutions for Baha in children five years of age and older. In order to fit them early, we need some nonsurgical options.
Baha System Candidacy: Conductive and Mixed Hearing Loss (CMHL)
First, we'll look at candidacy criteria for patients with mixed or conductive hearing losses. The Baha system can fit CMHL patients with these types of losses: those who have bone conduction pure-tone averages equal to or better than 65 dB. Bilateral fittings can be considered for these patients, but it does require symmetric bone conduction thresholds. I learned about Baha Technology when I started fitting patients 20 years ago. At that time, the mixed hearing loss option wasn't a good choice for Baha patients because we didn't have the technology for the external sound processor that we do today. Over the years, there have been improvements to the implant itself, as well as the external processor. In addition, digital technology and active feedback management (things that we take for granted now with hearing aid and Baha fittings) have allowed us to now accommodate a degree of sensorineural component that was not an option when we first did these 20 years ago.
Patients with conductive or mixed hearing loss are experiencing cytopathology in the outer or middle ear. Baha works by bypassing these and directly stimulating the cochlea. Some common forms of conductive or mixed hearing loss that can be treated with Baha include atresia, chronic middle ear disease, cholesteatoma, and congenital abnormalities. Especially for patients with draining ears, Baha can be a fantastic option over hearing aids. The Baha bone conduction implant bypasses the middle ear space and is effectively able to close that air-bone gap. Because of the advancements in technology over the years, we can now amplify sound for the sensorineural component as you would with a hearing aid. That means that a Baha device can treat a significant mixed loss without needing to account for the conductive component.
Let's take a look at some specific etiologies for conductive and mixed hearing loss. If you think about patients who are candidates for middle ear surgeries, their usual treatment might include things like tympanoplasty, ossiculoplasty, and stapedectomy. Those of you who are more in the medical realm probably see patients who fall into this category almost every day. Over 300,000 ear surgeries are performed each year in the U.S., not including myringotomy and tubes (Hall et al., 2017). That's over one thousand surgeries per day. The literature on this topic indicates that there's a 60 to 70% rate of successful hearing restoration where no additional hearing intervention is needed (Iniguez-Cuadra et al., 2010; Cox et al., 2017; Stankovic, 2008; O'Reilly et al., 2005). The rate drops from there when additional surgeries are performed. For example, revision stapedectomy cases show a decrease of approximately 35% in terms of resolving the hearing loss (Vincent et al., 2010). In these cases, often the surgery has resulted in an improvement in the air-bone gap, but the patient still has a hearing loss (Vincent et al., 2006). As an audiologist, you need to decide what to do next. Baha technology is a great option for patients who have undergone surgery that was not entirely successful or did not completely resolve their hearing loss.
Another common cause of conductive or mixed hearing loss is congenital aural atresia. The literature shows that the degree of hearing restoration is dependent on the severity of the atresia, which is no surprise (Chang et al., 2006). The majority of pediatric patients who have reconstruction will still require some form of amplification after surgery (Evans and Kazahaya, 2007). Again, when we look at revision cases, most of the patients who don't get hearing restoration with initial surgery will also not get restoration with revision surgery. That's something to keep in mind when considering how a Baha solution might fit into the treatment plan.
The Baha system is an excellent choice for conductive hearing loss, as the greater the air-bone gap, the more a Baha system will tend to outperform hearing aids (Snik et al., 2005; Mylanus et al., 1998). A study was done looking at the degree of loss and the benefits of Baha vs. hearing aids for mixed hearing loss (Johnson, 2013). Many of us were likely taught that conductive losses are pretty easy to fit with a hearing aid because you just have to turn up the volume. If the cochlear health is still viable and the communication between the cochlea and the auditory nerve is solid, you just amplify that and things are good, right? However, if that air-bone gap is greater than 30 dB, the fit becomes more complicated with a hearing aid. In the graph in Figure 1, we can see that the reported benefit declines once you have a greater than 30 dB conductive component. However, since the Baha intervention bypasses all of that and goes directly to the cochlea, it continues to perform just as well and you don't see that change in performance with that large degree of conductive component.
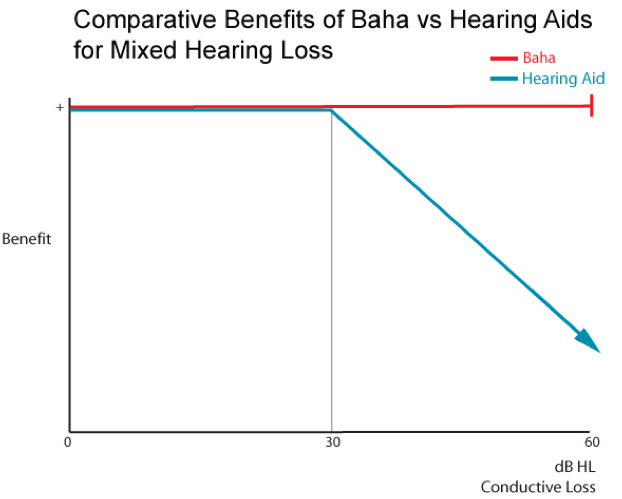
Figure 1. Benefits of Baha vs. hearing aids for mixed hearing loss.
In summary, the advantages of Baha with conductive and mixed hearing loss are as follows:
- Nothing is worn on the external ear, which is helpful in cases where drainage is present (Bouhabel et al., 2012).
- Baha does not need to be re-adjusted if air conduction thresholds fluctuate because gain is only required for the bone conduction thresholds. If there are varying degrees of fluid from one day to the next, that does not change the fit of the Baha.
- Preoperative testing (using a demo option) can be used to predict postoperative benefit (Monini et al., 2015).
- The use of Baha is associated with high user satisfaction and good long-term benefit. Once patients have this intervention, they are satisfied over a long period of time (Gardell et al., 2015; Rasmussen et al., 2012).
Baha System Candidacy: Single-Sided Deafness (SSD)
The other group who can benefit from Baha are those with single-sided deafness (SSD). This is defined by air conduction thresholds in the normal hearing ear and works via the contralateral routing of the signal. If you think about patients with SSD, they're missing the advantages that two ears provide. As we know, there are three main advantages of listening with two ears:
- Listening with two ears helps to overcome the head shadow effect, especially in the high frequencies. Having two ears means that you always have one ear towards the sound and can hear the complete signal.
- Our brains use the information coming into both ears to help us better understand speech in background noise. If one ear is not picking up sound for the brain, then it becomes quite difficult to hear well in noisy situations.
- Hearing with both ears helps in the localization of sound. We use both ears to find out where sound is coming from. If you think back to your psychoacoustics courses, in addition to frequency resolution, when both ears are employed, there is the significant benefit of spatial and temporal cues. This is important for challenging situations.
What is the impact of Single-Sided Deafness on daily living? You may be surprised to know that the effects of SSD are often overlooked and sometimes even minimized by the medical community because there is an impression that if people have one fully functional ear, they can go about their day just fine. However, data from a survey of people with SSD indicates that they commonly report the following difficulties hearing with just one ear:
- Lack of "stereo" hearing
- Difficulties as a pedestrian
- Social exclusion
- Cannot be part of a group
- Difficulty on the telephone
As a result of their SSD, a large number of respondents reported social difficulties such as "social exclusion" and "cannot be part of a group", because hearing in noisy group situations can be challenging. It is this feeling of exclusion that often leads people to seek treatment for SSD (Cochlear survey, article E80414A).
What are the common treatments for single-sided deafness? Unfortunately, the most common treatment is to do nothing. This is sometimes the patient's choice, but can also be the physician's choice to either not refer the patient or simply suggest that nothing can be done. CROS hearing aids are probably the next most common choice for patients. There have been significant improvements in CROS hearing aid technology leading to more patients using them, but they do have some limitations which we'll consider. Sometimes there are medical treatments possible. For example, in the case of sudden hearing loss, steroids may be used, and some forms of SSD may be mixed or conductive, in which case, surgery may be possible. Finally, we have bone conduction devices, such as the Baha system, as a treatment option for SSD. However, by far the most common treatment for patients with SSD is to do nothing, which can lead to social isolation and difficulty in groups.
Why choose a bone conduction treatment option for SSD? When a patient has a complete loss of hearing in one ear, we need to find a way of transmitting the signal to the normal hearing ear. Bone conduction is an elegant way to do that. With a Baha system on the poorer ear, sound is transferred across the head to the normal ear, leading to several advantages. One benefit is improved speech understanding in noisy environments (Hol et al., 2005). Additionally, by reducing the head shadow effect and bringing sounds to the brain from both sides of the head, the impact of noisy environments is reduced and your patients are able to hear better in any situation where noise is present (Hol et al., 2005; Lin et al., 2006; Pai et al., YEAR??; Wazen et al., 2003). Studies show that treatment with Baha can help reduce some of the psychosocial consequences of living with a hearing loss in one ear (Hol et al., 2005; Newman et al., 2008; Schroder et al., 2010). Imagine the listening effort involved in constantly having to turn your head towards the speaker or try to hear when there is noise coming to your good ear. Baha helps to lessen this effort, resulting in a better quality of life and long-term satisfaction for patients (Kompis et al., 2017; Maurizio et al., 2010).
I'd like to address localization again for a moment. As most audiologists know, in order to localize a sound, two cochleas are required. Baha does not completely restore localization to a patient. It can, however, allow them to hear sounds coming from that side of the head, resulting in the ability to lateralize where the sound is coming from (e.g., to know that someone is calling them from the right or from the left, even if they're not quite sure exactly where the speaker is standing). I'm often surprised when patients say that their Baha helps them know where the sound is coming from because I know that they're not truly localizing with their Baha, but even knowing which side of the head a sound is coming from can be helpful.
To illustrate the positive benefits of localization, when I was in the clinic, I worked with a patient who was a nurse. She had lifelong sensorineural deafness on one side of her head. Because she had grown up with that condition, she felt like she was functioning just fine with her SSD. However, when she became a nurse, she took a position in the operating room of a hospital. In an OR situation, everyone's mouths are covered by masks and they aren't necessarily shouting. In this role, it is critical that she hears exactly what the surgeon needs so she can hand him the correct tool or treat the patient. That's when she came to us looking for an option. She had perfect hearing in her good ear, so she didn't want to occlude it by using a CROS technology option. With Baha, she did phenomenally well. She needed to be able to hear the speech on both sides and Baha was a perfect solution for her.
Why might a patient consider a Baha as a treatment option instead of using CROS hearing aids? There are many reasons to choose Baha, including:
- The Baha system is a discrete solution worn on one side, while CROS hearing aids require users to wear devices in both ears. People love not having to wear something in both ears and even not having anything inside either ear. It's nice to have that off-the-ear option.
- Baha allows wireless streaming to be mixed with the environmental mic from the bad side, while many CROS systems require turning off the mic on that side in order to utilize the wireless streaming technology (Phonak CROS II wireless compatibility, 2017). With Baha, users have a binaural streaming option.
- Baha 5 sound processors are the first Made for iPhone solutions for individuals who have single-sided deafness and allow for easy streaming from iPhones and other wireless devices, offering a seamless hearing experience that's integrated with their lives.
- The Baha system bypasses the outer and middle ear and sends a clearer, crisper sound directly to the inner ear. You do not need to overcome any kind of occlusion effect (Gustafsson, 2015).
- Several studies have demonstrated that the Baha system provides better speech understanding in noise than CROS hearing aids (Niparko et al., 2003; Hol et al., 2005).
Determining Candidacy for Bone Conduction Solutions
Now that you have a good understanding of the types of hearing loss, we will look at determining candidacy. There are four main steps to deciding if Baha is a good treatment solution for your patients:
- Bone Conduction Thresholds. The first step is to look at bone conduction thresholds and compare them to the indications.
- Demonstration and Testing. The next step is the demonstration, which is unique to Baha over other surgical treatment options. We'll discuss how you can use the demonstration to help select the best device for someone, as well as predict how they'll do after surgery.
- Device Selection. Third, we have device selection. If you attended the Foundations Course on Baha Technology, you know that there are many options available to our recipients (e.g., the type of surgical device they have, the type of processor). All of these options can be determined ahead of time so you can counsel your patients about what to expect.
- Counseling. Finally, the last step is counseling. For those of you who are newer to working with Baha, this can sometimes be the most challenging step. You might feel confident in comparing someone's thresholds to the Baha indications and even performing a demonstration, but talking a patient through what to expect if they move forward can be a bit more daunting. Our goal today is to make sure you have the information you need to feel more confident in counseling and talking to your patients about Baha.
In the downloadable handouts for this course, you will find materials that will help you with the candidacy process for your patients. The first item is the Comprehensive Candidacy Guide (a.k.a., the Baha candidacy Bible). It contains all the information you need to help determine Baha candidacy, for both adults and children. [Note: If you are interested in learning more about Baha for pediatric populations, there is another course available on AudiologyOnline titled "Baha Systems for Children with Mixed and Conductive Hearing Loss"]. The second handout is a one-page checklist that you can use for individual candidates. It provides space for you to record the type of candidate: mixed, conductive, or single-sided deafness, the thresholds, and even the processor selection. Some centers will use this as part of the patient's chart to record the candidacy process. Feel free to keep both of these resources on hand as you work with your candidates. If you have additional questions, of course, you can always reach out to your clinical territory manager who is happy to be part of that process.
Bone Conduction Thresholds
First, let's focus on bone conduction thresholds and what they can tell us about a potential candidate. Obviously, this is the first piece of information we usually have about a candidate. One thing that's important to remember is that the different indications focus on different thresholds.
For mixed and conductive hearing loss (MCHL), the indications focus on the bone conduction thresholds which must be 65 dB or better to qualify for Baha as a treatment option. In this example (Figure 2), while the air conduction thresholds fall outside of the candidacy criteria, it's the bone conduction thresholds that we're looking at, and these fall well within the fitting range. This person may be a Baha candidate. Remember our discussion about the 30 dB air-bone gaps or poorer? Those with less of an air-bone gap may still choose Baha for other reasons. In this case, that air-bone gap means that this will be a challenging fit with hearing aids because this is greater than 30 dB between the bone conduction score and the air conduction score. This person will likely have better performance with a Baha than with a hearing aid.
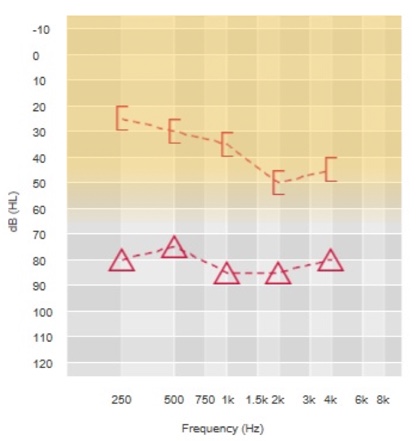
Figure 2. Bone conduction thresholds for determining Baha candidacy: MCHL.
In some cases, you may find the thresholds to be on the borderline of what you might expect to be able to treat. One way to get a better idea of how the patient will do with an actual Baha device is to fit the processor using the Baha Fitting Software. Within the software, there's a measurement called BC Direct that will give you the patient's actual responses to a Baha device. We'll discuss this more in the fitting module, but this is another example of where fitting the processor to the patient during the demonstration can provide you with information about how they'll actually do with their device, which can prove very helpful.
To determine candidacy for someone with SSD, we do something a little different. For SSD, we compare the air conduction thresholds of the good ear to the indication, which says that air conduction pure-tone average for the good ear has to be 20 dB or better. Figure 3 shows a classic example of single-sided deafness within the fitting range. You can see that the right ear air conduction falls within the indications for implantation. Remember that the indication does not specify the poorer ear thresholds, only the better ear thresholds. The point of that is making sure that the sound that is transmitted across the head to the better ear is going to be optimally utilized.
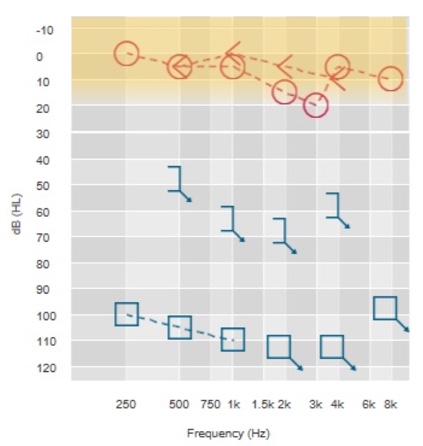
Figure 3. Air conduction thresholds for determining Baha candidacy: SSD.
Demonstration and Testing
Next, as we discuss demonstration and testing, we first need to review some terminology.
- Demonstration. The demonstration shows the patient a quick glimpse of Baha technology. You may pre-program the device and let them try it on. This is generally a limited experience where the processor may be set to "demo" mode and placed on the patient's head using the test rod or headband. In many clinics, the demo may be completed by a surgeon, an audiologist, or a technician.
- Evaluation. The evaluation is performed by the audiologist and utilizes sound field testing in order to objectively describe a patient's benefit of Baha. This requires a full fitting of the sound processor. Speech perception testing is completed.
- Trial. The Baha trial may be done in conjunction with a demo or evaluation. In the trial, the patient would either take the processor away for a period of time in the real world (e.g., wear it over lunch in a restaurant) or possibly even bring it home for a trial. In general, the Baha would be fit using the software for a trial, especially one that would be gone longer than a few hours to just give the most accurate experience possible.
Any of these methods might be used to determine candidacy for a patient. It really depends on the patient, their etiology, the clinic, and the questions that are being asked about candidacy. In some clinics, all patients undergo a full evaluation, and in others, an evaluation may be completed only if there's a question about the potential benefit or reserved for those with SSD. Some clinics may always recommend a home trial, while others may reserve it for unique circumstances. It's up to each individual clinic to determine the methods that work best with their patient population and clinical needs.
Demonstration. The first option is the Baha demonstration. The test rod pictured in Figure 4 is the best device to use for a quick demonstration. The sound processor can be snapped into the test rod and then held against the patient's head. The main reason that the test rod is better than using older test bands is that it's compatible with the Baha 5 technology and will likely result in a better demonstration.
Figure 4. Sound processor and test rod.
Baha demonstrations can be greatly enhanced by setting up the sound processor ahead for different types of candidates. Entering bone conduction thresholds of 10 dB in the software will set the processor up nicely for a conductive hearing loss. For a mixed hearing loss, you can take that program and increase the overall gain by 5 dB. For a demo with SSD, decrease the mixed program by 5 dB in the low frequencies. These programs can then be saved as programs 1, 2 and 3 and used as needed for quick demonstrations. The Baha 5 Power is a great device for these demonstrations because it has a volume rocker so the gain can be adjusted as needed for individual patients.
Evaluation. Let's turn our attention to a more complete Baha evaluation. These can be very useful to establish benefit before surgery (Monini et al., 2015; Snapp et al., 2010). They help provide realistic expectations of surgery and help you to identify the best surgical candidates based on performance. Another nice aspect of this type of testing is that the choice of processor can be confirmed prior to surgery. The idea is that we're using the testing with and without the Baha to compare the two conditions and determine benefit. You can think of it the same way you might think of evaluating someone for different hearing aid technology, where you might test them with different types of hearing aids or compared to an unaided condition to determine the best treatment pathway or even just help you with counseling.
For evaluation, the first thing we need to do is fit the SoundArc or Softband to the patient's head with a demo processor. We'll describe the full fitting procedure more in our module on fitting, but essentially you're fitting the patient as if they were going to actually use the device. The next step is to fit the sound processor in the fitting software. As you'll learn in the fitting module, one of the most important things to do here is measure the BC Direct thresholds in the software. This measures hearing thresholds using the Baha sound processor itself and is very helpful in personalizing the program for an individual patient. You can think of it almost as a "real ear" for Baha. Finally, for an evaluation, we'll want to perform some kind of objective testing in the sound booth to determine what benefit the person is getting from the device.
Let's review how we might do an evaluation in the booth for someone with conductive and mixed hearing loss. For objective testing, we want to compare how someone does with the Baha and without. You can use words or speech-in-noise for testing. Primarily, we see clinics using speech-in-noise. What we would recommend is that you complete a functional listening evaluation. Perform testing once in the unaided condition, and then again in the aided condition with the Baha, and then you can compare the two results. Importantly, studies have shown that preoperative testing with the headband is predictive of benefit after surgery so you can be confident in counseling the candidate about the benefit they can expect (Monini et al., 2015). We're often asked which speech materials to use for testing. There's no specific Baha speech test. You can use any materials that might demonstrate a benefit for the patient. Examples might be single words, such as the W22 or NU6, or speech-in-noise, such as the QuickSIN or AzBio test. Whatever you choose, ensure the patient can complete the test unaided, but not hit the ceiling effect so you can compare results.
Single-Sided Deafness testing in the sound field is a little bit different. We know that the greatest benefit for Baha comes in cases where the noise is on the "good" side and the signal that the person wants to hear is on the "bad" side. That's how we set up the test. As this diagram shows, testing is best completed in a booth where you can direct speech to the Baha side and noise to the good side. Just like in conductive and mixed hearing loss, we test the patient twice: once unaided, and once aided. The difference seen between the unaided and aided conditions predicts the postoperative benefit that can be expected (Snapp et al., 2010). This type of formal evaluation can be especially helpful for Single-Sided Deafness, especially since a lot of times an informal demo is done in a quiet room and the patient can't really tell whether it will help them. This can also demonstrate how the patient's central auditory system is already compensating for the unilateral loss. There are few patients who will basically do the same with and without Baha. These folks are not good candidates unless there's some specific reason they have to hear from that side. It's very important to do this testing ahead of time to find out what the benefit will be.
Trial. Our third option is for a trial. This is something we know a lot of our clinics perform and is a very common part of the preoperative assessment for many candidates. A Baha trial simply refers to fitting the patient and having them try it in real-world situations. Perhaps they take the device for the day or even for a few days or a week. The SoundArc can be extremely useful in this situation because it will be more cosmetically appealing and the patient is more likely to want to wear it for a home trial. If you haven't done trials like in the past, this may be something to consider for your clinic. We found that this is an excellent choice when there's a borderline situation. If the candidacy is not clear or you're unsure if the patient will benefit, give them a short trial to help them decide. The patient is best suited to decide whether they're seeing a benefit. Even a short trial of just a few hours over lunch can often help them determine if they are benefiting from the Baha.
Device Selection
Device selection is the next step in the candidacy process. There are many different choices for treatment with Baha solutions. During the candidacy process, we can use that information to help determine which surgical or nonsurgical option to select. You will find more information about the different technologies in our technology module, but as a review, there are two different surgical options for Baha: the Baha Attract, which is a magnetic connection without an abutment, and the Baha Connect, which provides a direct connection through a hearing abutment.
In terms of audiological performance, the main difference between the two systems is their available output. Figure 5 shows a graph which demonstrates the force output of different types of systems on an artificial mastoid. In the gray is the Baha Softband. This has the lowest available output because we have to send the signal across the skin and lose about 10 to 15 dB of gain because of that. This is why doing candidacy evaluation using a SoundArc or Softband is so effective. If a patient has a successful fitting during these nonsurgical options, then we know we will have even more gain available after surgery. If anything, it underestimates their benefit. The blue line is the Baha Attract. You will notice that it is slightly better than the Softband, especially in the high frequencies. This is because even though the sound is transmitted across the skin, the patient still has an osseointegrated implant to transmit the sound through, so they get a bit better gain than they would with a nonsurgical option. Finally, in yellow is the Baha Connect. This is one of the biggest advantages of the Connect because the sound processor is connected directly to the abutment and the implant and the patient has the highest available gain for their device. An example of how this plays out with the patient might be in the selection of a sound processor. Someone who uses a Baha 5 Power to get enough gain on a Softband, for example, might be able to use the smaller Baha 5 if they get a Baha Connect, but may still need to buy a Baha 5 Power on the Baha Attract. This has implications for counseling and can help you guide patients to decide which option is right for them. As mentioned before, the BC Direct thresholds are the best measurement to use. What you see with the Softband or SoundArc gives you a good prediction of how the patient will do, especially with the Baha Attract since the gain profiles are so similar.
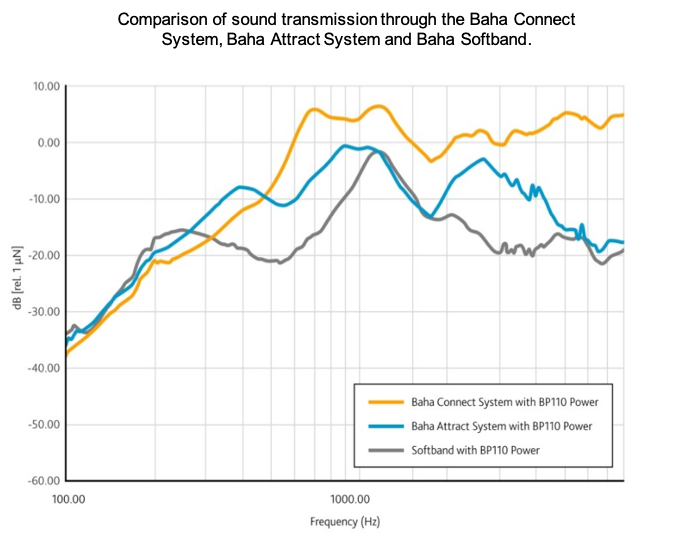
Figure 5. Comparison of sound transmission through the different Baha systems.
In addition to the choice of surgical option, you will also need to choose the processor for your patient (Figure 6). This is not a final decision. All processors have the ability to be exchanged at the time of activation if during the initial fit you realize a different processor is needed, but the bone conduction thresholds can be used to predict which processor will work best for a patient. The Baha 5 is best for bone conduction thresholds up to 45 dB, the Baha 5 Power, up to 55 dB, and the Baha 5 SuperPower for your more severe mixed losses, up to that 65 dB bone line. Again more information about these processors is available in the module on technology. As with hearing aids, if the bone conduction thresholds fall within the last 10% of the fitting range, you might consider putting the more powerful device so you have enough headroom if any more power is needed over time.
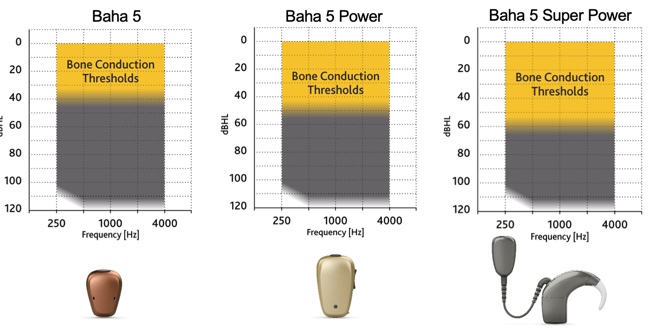
Figure 6. Baha processors.
Another thing to select during this time is the wireless devices and accessories you would like for your patient (Figure 7). Every Baha system comes with one free wireless accessory. There are a few different choices. You have the MiniMic 2 or the MiniMic 2+. It's a portable remote microphone. The MiniMic 2+ is slightly larger and includes the ability to connect with telecoil, FM, and going to conference mode. If your patient has an iPhone and can take advantage of the direct-to-iPhone streaming of phone calls, the MiniMic is really an excellent choice. It could also be good for students or those who need to listen to speech at a distance as part of their work, perhaps a lawyer, bus driver.
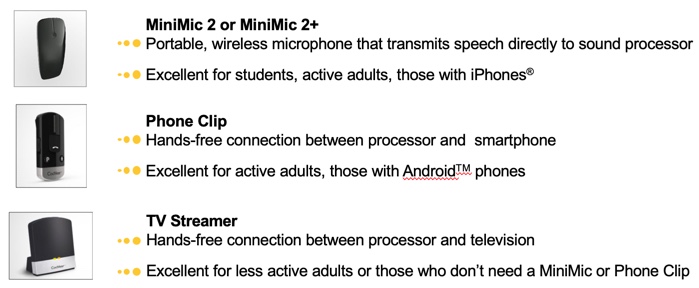
Figure 7. Baha wireless devices.
Also pictured in Figure 7 is the Phone Clip, which enables streaming between any Bluetooth-enabled device and the sound processor. It provides a hands-free option for phone calls and this is a great option for any adults with an Android phone or something other than an iPhone since these cannot stream directly to the sound processor at this time. It might also be good if someone is on the phone a lot, even if they have an iPhone since the Phone Clip will pick up the patient's voice for phone calls. In other words, it's hands-free. They don't have to hold the phone near their mouth to you have that conversation.
Finally, the TV Streamer provides a completely dongle-free connection to the television. It's a wonderful option for patients who might spend more time in front of the TV and are perhaps a little less active or maybe have a large family and they like to watch TV and there's always a bunch of sound in that room.
When selecting accessories, consider the listening needs of the patient and the daily situations they're in when deciding which device would be best for them. As with the processors, the accessories may be exchanged unopened at the time of activation if you change your mind.
Counseling
The final step in the process is to counsel the patient. Many of you who already work with hearing aids may be used to walking someone through their goals for treatment and how a hearing aid will help them achieve those goals. Working with Baha is no different.
There are some great formal tools and resources that you can use to help counsel patients. The COSI is one I especially like since it allows patients to create their own goals. For example, a patient may indicate as a goal, "I would like my hearing technology to allow me to ask my colleagues to repeat less often during work meetings." Then you can rate how high the need is before the intervention and how well the invention is working later. These goals can help you decide on unrealistic expectations, and then measure them against treatment. Another formal inventory you could use is the Abbreviated Profile of Hearing Aid Benefit (APHAB).
While there are some great formal tools, informal methods also work well. There's a section on the pre-op candidacy tool in your handouts that simply asks about the individual's hearing in different environments. While this is informal, it's a great way to set up expectations.
In general, you'll want to cover the advantages of the Baha system during counseling, explaining to the patient what they can expect. As a review, here are some of the advantages we've discussed thus far during this presentation:
- It can be worn off the ear.
- It has a high level of user satisfaction over CROS aids (Gardell et al., 2015; Rasmussen et al., 2012).
- The cost may be covered by insurance.
- There's a choice between a magnetic solution (Attract) and a direct connection (Connect) and can transition between them if necessary.
- The patient has access to wireless technology through the device.
It is important that candidates also understand the process. Each clinic in unique in how patients move through the process, so be sure you understand the next steps and how the patient will move through the process at your clinic. Who will take care of insurance pre-authorization? When will they be scheduled for their activation? Do they see the surgeon first or the audiologist? All of these will be helpful pieces of information to gather to be sure you are preparing the patient for what comes next.
Connect with a Cochlear Concierge
One last thing to mention about counseling for candidates is the ability to have your patients connect with a Cochlear concierge. This is our team of experts here at Cochlear who are available to answer questions, support candidates and connect them with volunteers who have Baha systems and can explain what it is like to be a recipient. You can consider the concierge to be an extension of your clinic, as they can assist in guiding the patient through their journey and provide that first-hand knowledge of what they can expect. To connect your patient to a concierge, we would suggest emailing the concierge ([email protected]) once you have the patients’ permission with their email and contact info. The concierge can then take it from there. You or your patient are also welcome to call the concierge directly (1-800-216-0228). This service is for both our Baha candidates as well as our Nucleus cochlear implant candidates, so feel free to utilize this for anyone who has questions about Cochlear’s hearing implant portfolio.
Case Studies
While it is important to cover indications and the process, examining some actual cases might help to put candidacy into perspective for you. These are not necessarily the easiest or most “obvious” cases, but often patients present with situations that don't make them clear Baha candidates. It is up to the hearing care professional to gather all the facts in order to help them make that decision.
Case Study #1: Roy
Roy is a 52-year-old man with a history of cholesteatoma in both ears. He wears an ITE hearing aid only in the left ear, but he doesn't wear it very much because he so often has drainage. He's a middle school teacher and finding that he's struggling so much, he's considering retiring early.
In this case, there are a couple of different things going on. Let's review Roy's audiogram (Figure 8). Currently, there is no intervention in the right ear, so we probably need to consider some options for the right ear. For Roy's left ear, the hearing aid isn't a good option because he's not able to wear it with all the drainage. The left ear seems like a great option for Baha and given the fact that he has a history of cholesteatoma in both ears, I would be hesitant to try a hearing aid on the right ear, worried that it would just have the same result as the left. Ultimately, I think Roy needs a solution for both ears and Baha Technology would be a great choice for Roy.
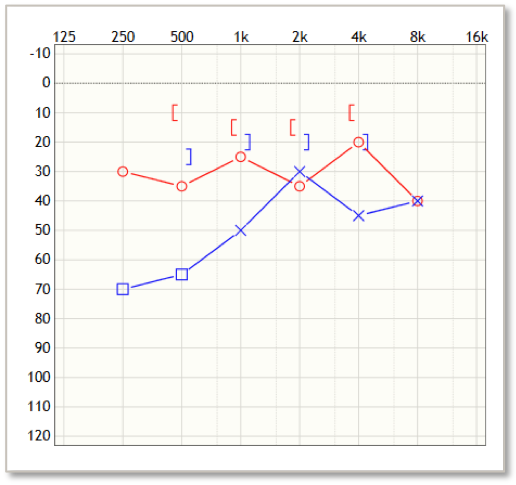
Figure 8. Roy's audiogram.
Case Study #2: Kira
This next case study is a little bit more complicated. Kira is a 36-year-old woman with a history of hearing loss since childhood and chronic middle ear disease. She has a history of tympanoplasty in both ears. No further surgeries are planned and she no longer has drainage from her ears. She is currently using in-the-ear hearing aids that are about six years old. She reports feeling like she can't get enough volume on the right side. This might be a case where an ENT might see the history of middle ear issues, notice that there is a conductive component and refer Kira to you for a Baha evaluation.
Would you recommend a Baha demonstration for Kira? A demo would be fantastic for her because if you look at her loss (Figure 9), we know that we have to have 65 dB or better bone line. Her struggle is mostly going to be in the high frequencies, which are a sensorineural loss. She would be very likely to experience minimal benefit from a Baha as an intervention. If she has in-the-ear hearing aids that are six years old, it's likely that she needs new amplification that better fits her loss. New hearing aids are probably a more appropriate solution than Baha.
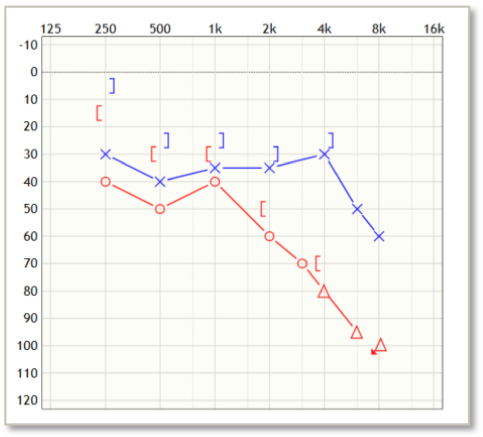
Figure 9. Kira's audiogram.
Case Study #3: Max
Max is a 37-year-old man with a long history of hearing loss in the right ear (Figure 10). He had surgery in the right ear as a child but has not had access to hearing on that side for most of his life. He did try CROS hearing aids but didn't like having the occlusion in the better ear. He works as a software engineer and spends time on the phone with global colleagues. He reports that he struggles to understand people with accents on the phone. He's also struggling more with hearing in noise, and his wife and coworkers feel that he should get some help.
What do you think? Would you recommend a Baha demonstration for Max? Let's assume that Max has the demo and scores the following:
Quick SIN Unaided = +9 dB SNR loss
Quick SIN with Baha = +3 dB SNR loss
Would you recommend Max proceed with the Baha surgery? Pending all medical clearances, I think that he's a straightforward candidate for Baha. This would be a scenario where it would be important to do that BC Direct testing on the Softband, just to be sure he's getting the full benefit in the trial of how he's going to perform. SSD is usually a pretty clear-cut case where the Baha would result in a positive outcome.
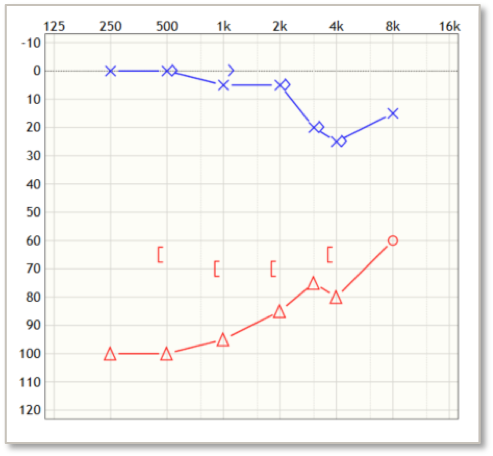
Figure 10. Max's audiogram.
Summary and Conclusion
This concludes our presentation. Thank you so much for your attention today. We encourage you to keep in touch with us. Our website contains a great deal of information for you. Our customer service is available if you want to order brochures or if you are seeing a patient with a cochlear implant who needs help. Don’t hesitate to reach out via phone or email to our Procare team. Finally, stay up to date with everything Cochlear by following us on social media. We always have good tips and tricks, as well as announcements about information available for you and your patients. Be sure to bookmark our YouTube channel for your candidates. Videos are a great way to help you say all the things you might be trying to say, as well as provide the patient with suggestions for their processors and access to patient testimonials.
References
Barbara, M., Biagini, M., Lazzarino, A. I., & Monini, S. (2010). Hearing and quality of life in a south European BAHA population. Acta oto-laryngologica, 130(9), 1040-1047.
Bouhabel, S., Arcand, P., & Saliba, I. (2012). Congenital aural atresia: bone-anchored hearing aid vs. external auditory canal reconstruction. International journal of pediatric otorhinolaryngology, 76(2), 272-277.
Chang, S. O., Choi, B. Y., & Hur, D. G. (2006). Analysis of the long‐term hearing results after the surgical repair of aural atresia. The Laryngoscope, 116(10), 1835-1841.
Cox, M. D., Trinidade, A., Russell, J. S., & Dornhoffer, J. L. (2017). Long-term hearing results after ossiculoplasty. Otology & Neurotology, 38(4), 510-515.Evans, A. K., & Kazahaya, K. (2007). Canal atresia:“surgery or implantable hearing devices? The expert's question is revisited”. International Journal of Pediatric Otorhinolaryngology, 71(3), 367-374.
Gardell, I. S., Andresen, K., Faber, C. E., & Wanscher, J. H. (2015). Bone-anchored hearing aids are effective and associated with a high degree of satisfaction. Danish medical journal, 62(7).
Gluth, M. B., Friedman, A. B., Atcherson, S. R., & Dornhoffer, J. L. (2013). Hearing aid tolerance after revision and obliteration of canal wall down mastoidectomy cavities. Otology & Neurotology, 34(4), 711-714.
Gustafsson, J. (2015). BCDrive performance vs. conventional bone conduction transducer. Cochlear Bone Anchored Solutions AB, 629908.
Hall, M. J., DeFrances, C. J., Williams, S. N., Golosinskiy, A., & Schwartzman, A. (2010). National Health Statistics Report: Ambulatory surgery data from hospitals and ambulatory surgery centers: United States (Vol. 29, pp. 1-20). CDC Report Number.
Iñiguez-Cuadra, R., Alobid, I., Borés-Domenech, A., Menéndez-Colino, L. M., Caballero-Borrego, M., & Bernal-Sprekelsen, M. (2010). Type III tympanoplasty with titanium total ossicular replacement prosthesis: anatomic and functional results. Otology & Neurotology, 31(3), 409-414.
Johnson, E. E. (2013). Prescriptive amplification recommendations for hearing losses with a conductive component and their impact on the required maximum power output: An update with accompanying clinical explanation. Journal of the American Academy of Audiology, 24(6), 452-460.
Kompis, M., Wimmer, W., & Caversaccio, M. (2017). Long term benefit of bone anchored hearing systems in single sided deafness. Acta oto-laryngologica, 137(4), 398-402.
Lin, L. M., Bowditch, S., Anderson, M. J., May, B., Cox, K. M., & Niparko, J. K. (2006). Amplification in the rehabilitation of unilateral deafness: speech in noise and directional hearing effects with bone-anchored hearing and contralateral routing of signal amplification. Otology & neurotology, 27(2), 172-182.
Monini, S., Filippi, C., Atturo, F., Biagini, M., Lazzarino, A. I., & Barbara, M. (2015). Individualised headband simulation test for predicting outcome after percutaneous bone conductive implantation. Acta Otorhinolaryngologica Italica, 35(4), 258.
Mylanus, E. A., van der Pouw, K. C., Snik, A. F., & Cremers, C. W. (1998). Intraindividual comparison of the bone-anchored hearing aid and air-conduction hearing aids. Archives of Otolaryngology–Head & Neck Surgery, 124(3), 271-276.
Myrthe, K. S., Bosman, A. J., Snik, A. F., Mylanus, E. A., & Cremers, C. W. J. (2005). Bone-anchored hearing aids in unilateral inner ear deafness: an evaluation of audiometric and patient outcome measurements. Otology & Neurotology, 26(5), 999-1006.
Newman, C. W., Sandridge, S. A., & Wodzisz, L. M. (2008). Longitudinal benefit from and satisfaction with the Baha system for patients with acquired unilateral sensorineural hearing loss. Otology & Neurotology, 29(8), 1123-1131.
Niparko, J. K., Cox, K. M., & Lustig, L. R. (2003). Comparison of the bone anchored hearing aid implantable hearing device with contralateral routing of offside signal amplification in the rehabilitation of unilateral deafness. Otology & neurotology, 24(1), 73-78.
O'Reilly, R. C., Cass, S. P., Hirsch, B. E., Kamerer, D. B., Bernat, R. A., & Poznanovic, S. P. (2005). Ossiculoplasty using incus interposition: hearing results and analysis of the middle ear risk index. Otology & Neurotology, 26(5), 853-858.
Pai, I., Kelleher, C., Nunn, T., Pathak, N., Jindal, M., O'Connor, A. F., & Jiang, D. (2012). Outcome of bone-anchored hearing aids for single-sided deafness: a prospective study. Acta oto-laryngologica, 132(7), 751-755.
Phonak CROS II wireless compatibility, downloaded from: https://www.phonakpro.com/us/en/support/product-support/hearing-aids/cros-ii/compatibility-cros-ii.html December, 2017
Rasmussen, J., Olsen, S. Ø., & Nielsen, L. H. (2012). Evaluation of long-term patient satisfaction and experience with the Baha® bone conduction implant. International journal of audiology, 51(3), 194-199.
Schrøder, S. A., Ravn, T., & Bonding, P. (2010). BAHA in single-sided deafness: patient compliance and subjective benefit. Otology & neurotology, 31(3), 404-408.
Snapp, H. A., Fabry, D. A., Telischi, F. F., Arheart, K. L., & Angeli, S. I. (2010). A clinical protocol for predicting outcomes with an implantable prosthetic device (Baha) in patients with single-sided deafness. Journal of the American Academy of Audiology, 21(10), 654-662.
Snik, F. M., Mylanus, E. A., Proops, D. W., Wolfaardt, J. F., Hodgetts, W. E., Somers, T., ... & Tjellström, A. (2005). Consensus statements on the BAHA system: where do we stand at present?. Annals of Otology, Rhinology & Laryngology, 114(12_suppl), 2-12.
Stankovic, M. D. (2008). Audiologic results of surgery for cholesteatoma: short-and long-term follow-up of influential factors. Otology & Neurotology, 29(7), 933-940.
Survey contained in ”Hear the other side” — A report on single-sided deafness. More information can be found at www.singlesideddeafness.com: A report by the advisory board for single sided deafness. Available from Cochlear — article E80414A.
Vincent, R., Rovers, M., Zingade, N., Oates, J., Sperling, N., Devèze, A., & Grolman, W. (2010). Revision stapedotomy: operative findings and hearing results. A prospective study of 652 cases from the Otology-Neurotology Database. Otology & Neurotology, 31(6), 875-882.
Vincent, R., Sperling, N. M., Oates, J., & Jindal, M. (2006). Surgical findings and long-term hearing results in 3,050 stapedotomies for primary otosclerosis: a prospective study with the otology-neurotology database. Otology & Neurotology, 27(8), S25-S47.
Wazen, J. J., Spitzer, J. B., Ghossaini, S. N., Fayad, J. N., Niparko, J. K., Cox, K., ... & Soli, S. D. (2003). Transcranial contralateral cochlear stimulation in unilateral deafness. Otolaryngology--head and neck surgery, 129(3), 248-254.
Citation
O'Sullivan, M. (2019). Foundations of Baha Implants: Candidacy. AudiologyOnline, Article 25450. Retrieved from https://www.audiologyonline.com


