Editor's Note: This text-based course is a transcript of the live seminar presented by Luis Camacho, M.A., FAAA, for Starkey Laboratories, Inc. Please download supplemental course materials.
Today we will be discussing infection control and the best clinical practices specifically geared towards the dispensing office, the dispensing audiologist or hearing instrument specialist offices, and how you may want to implement some practices for infection control and universal precautions. We will start with a basic overview of infection control. We will discuss some specifics in how we want to relate infection control to the hearing aid dispensing practice. Then we will conclude with discussion on universal precautions, how this is defined by the Occupational Safety and Health Administration (OSHA), and the different requirements that OSHA does put into place for any health care provider. At the end, there will be a few frequently asked questions about infection control and how it relates to the hearing aid practice.
Infection control involves developing and implementing consistent execution of procedures that are designed specifically to reduce cross-contamination in an office. A textbook definition is "the conscious management of the clinical environment for purposes of minimizing or eliminating the potential spread of disease (Bankaitis & Kemp, 2003, 2004). This is not about just controlling exposure of infection from person to person, but also from an environment to another person, or from a particular item, tool, piece of equipment to another person. There are a variety of things we need to take a look at in terms of trying to control the spread of potential disease.
Why has Infection Control Become a "Hot Topic" Again?
This is not a new area of study or interest to the health care-providing services in this country, but there are a number of issues that bring about interest in infection control periodically throughout history. Going back a few decades to the 80's, the emergence of AIDS and HIV spurred a new interest in infection control. If we go back to this time last year, the threat of the H1N1 flu virus also brought about another interest in infection control. With H1N1 being all over the news, I saw many places with dispensers for hand cleanser. This was something everyone became more aware of, and we specifically need to be very aware of this in a health care-providing service.
The nature of the dispensing office allows us to use tools that come in contact with many different types of people throughout the day. Staff and patients are interacting with different pieces of equipment and many other people where there is the potential for infectious diseases to be present. The scope of our practice today is also very wide. Throughout the day, you may see dozens of people that may have health concerns that you may not know when they present to the office, but should be aware of. With our varied patient load, you might have older patients, younger patients, some healthy, some sick. You have to be aware that you may be spreading or potentially spreading infection from one person to the other as people are moving in and out of your office during the day.
What does this mean? Does this mean we all have to don the hazmat suit before we walk into the office and then be sprayed down at the end of the day? Hopefully we have not gotten and will not get to the place in the world where that extreme level of precaution is needed just to fit hearing aids to people and allow people to hear better throughout their daily activities. We do not have to take these extreme measures, but there are a number of simple measures that we can take that will minimize the potential for you, the professional, to get an infectious disease or to spread an infectious disease from staff to patient or patient to patient.
Contact Transmission
When we talk about transmission of microbes, bacteria, viruses, etc., there are a number of different ways of transmitting or potentially transmitting these infectious diseases. Contact transmission is divided into three different areas. There is direct contact, where we directly transmit one microbe to another without any barrier such as with a handshake in person to person contact. Another form is indirect contact. This is when we transfer a microbe from a surface to a person such as a physician or audiologist looking into the patient's ear with an otoscope that may not have been disinfected or using the same speculum on more than one patient. The surface area is what transmits the potentially infectious microbe. Lastly we have the droplet transmission. This is actually transmitting through water droplets from coughing or sneezing. The microbe is present in some form of water droplet and it is then picked up by a person, and the infection is transmitted.
Modes of Transmission
There are other modes of transmission as well. There is vehicle transmission which is transmission of the microbe through a "vehicle" such as food, contaminated water, drinking glass, or bodily substances like cerumen. Another mode of transmission is airborne. Airborne transmission is when the microbe transmits through the air from one person to another. Lastly we have vectorborne transmission. This is transmission of a microbe via animal or insect. This is not a major concern for those of us in the dispensing practice. We do not have to worry as much about malaria being transmitted in our office here in the United States.
Routes of Transmission
How do we typically get these microbes into the body? There are a few main areas such as the eyes, ears, nose and mouth. These are open body orifices where we can have easy introduction of infection into the body. These areas are typically the ones we should be concerned about in terms of protecting ourselves from the spread of infection. We do not typically think of cerumen as being a worrisome issue with infectious disease. We all know that cerumen is the body's way of keeping the ear canal clean. We do not usually think of this as being a transmitter of potential infection. Standardly it is not a bodily substance we should worry about, unless there is contamination of the earwax. This contamination can come from mucous possibly from a middle or outer ear infection, or from blood. If you do have the introduction of blood or mucous to cerumen, this substance now becomes a potential transmitter of disease. Due to the nature of how cerumen looks, it is very hard to visually know whether or not the ear wax has been contaminated with blood or mucous. Cerumen can be dark and is obviously waxy in nature. Since you do not know by visual inspection if the cerumen is contaminated, you should be treating all cerumen as if it were an infectious substance. You should take general precautions any time you are dealing with cerumen management, cleaning of a hearing aid, etc.
Opportunistic Infections
In the dispensing practice, we are concerned mainly about opportunistic infections. An opportunistic infection is a disease, bacteria, or virus, that is present waiting for a person who has a somewhat weakened immune system or someone who is immunocompromised. As a healthy young adult, which many of us are who are dispensing and fitting hearing aids, we may not personally have to be as concerned about an opportunistic infection. However with many of our patients we need to be concerned about these infections. The majority of us are working with the elderly population or the pediatric population. The very young and the elderly tend to have less robust immune systems. Therefore these opportunistic infections can be very problematic for those populations. Also if you are working with someone who is suffering from a disease such as HIV, the hallmark of that virus is a reduced immune system. Again we are talking about organisms, bacteria, etc. that are very commonly found in our environment. These organisms are in and around our environments at all times. However with a strong immune system, we do not have to be as concerned about cross-contamination as with our patients who have reduced immune systems. If you do not utilize the appropriate infection control, you, in effect, could be opening the door to people with compromised immune systems to a rather severe infection. In many cases if someone is suffering from the following diseases, they could contract an opportunistic infection which would take advantage of their weakened immune system. These immunocompromising diseases could be:
- AIDS
- Diabetes, type I and type II
- Hepatitis, specifically Hepatitis B
- SARS (Severe Acute Respiratory Syndrome)
- Tuberculosis
We do not typically see people with tuberculosis these days in the United States. However diabetes is a very common disorder in this country and it does weaken the immune system as well. This is one of the many reasons why we should keep control of and manage the spread of infection in our office. Doing so would minimize the potential effects on our patients, ourselves and our staff members.
An interesting fact specific to our patients, hearing aid patients, is that the external ear canal is very prone to infection. It is skin surface that is the most prone to infection on the body. This comes down to the ear canal being a very moist, dark, and warm area that can be conducive to bacterial growth. We ask our patients to wear their hearing aids as much as they can throughout the day. By doing this, we create a dilemma as we are closing off the ear canal and creating a perfect "laboratory" for the growth of fungus or bacteria. Cerumen's role is to try to inhibit this growth. It is the cleaning mechanism of the ear canal. We change the environment by closing off the ear canal with hearing aids, cell phone headsets, or iPod® ear plugs. We need to be aware of the fact that the ear canal can be a perfect environment for continued growth of potential infectious items.
We have all taken hearing aids back to the office to clean and check. It does go through our minds that something could be growing on that hearing aid. There have been some studies done regarding this. It has been found that if you have otitis media or otitis externa there could be some mycobacterium possibly on the hearing aid or maybe staphylococcus present. With otitis externa, you can also have the presence of pseudomonas. Pseudomonas is a bacteria that can cause respiratory infections, skin infections such as dermatitis, or urinary infections. We know for a fact that these otitis media and otitis externa infections are very common in our hearing aid offices. Within those particular disorders, there can be other infectious agents present which could be spread to you the professional, another staff member, or another patient in your office if you are not following strict precautions for infection control. Specifically, a study was done back in 2002 (Bankaitis) on hearing aid related infection control. In this study, they looked at physician stethoscopes, hearing aids, the tools and other things that are present within hearing aid dispensing offices. They found a rather large list of microbes that were present in that dispensing environment as seen in figure 1. Listed also are the associated infections or diseases that are common with these microbes.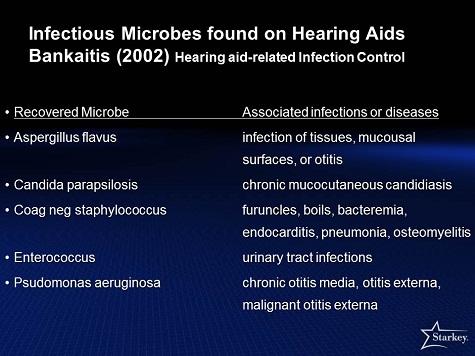
Figure 1. A list of infectious microbes found on the surface of hearing aids.
We are not trying to scare everyone as to what infectious diseases are floating about in your offices, but there is the potential to have all of these different microbes present in any health care office. In many cases, we do not think of ourselves as health care providers when, in fact, we really are.
Universal precautions are guidelines that have been established by the Center for Disease Control (CDC) and they are the foundation of infection control. We will cover the different steps and recommendations given by the CDC under the umbrella term of Universal Precautions. This will include personal protective equipment, hand hygiene which is probably the most important thing we can do to minimize the spread of disease, cleaning and disinfecting procedures for surfaces, tools, and equipment we use in the office, sterilization of critical clinical instruments, and appropriate waste disposal or how to handle anything that has come in contact with potential infectious agents that we will dispose of at the end of the day.
Step I: Personal Protective Equipment
Personal protective equipment includes safety glasses, masks and gowns.
It is important to use the masks and safety goggles when we are performing hearing aid or earmold modifications such as grinding. During modifications, there is potential for something to become airborne and to get in your eyes. Many times we do not think about hearing aid/earmold modifications in terms of infectious agents, we think of maybe a piece of the hearing aid would break off and fly into our eye. Anytime you are grinding or buffing on something that might have ear wax on it, you could create an airborne transmission of an infectious agent.
Gowns are not as commonly used in our profession, but they should be available for patients whom you know have an infectious agent. This could come about in a hospital while you deal with a patient with a spreadable disease or known infections. You need to protect yourself doing an ear impression or cerumen management. You should consider having this equipment on hand. Whether or not you use them for every patient is a decision you should make based on your patient base or the clientele you are working with, and the clinical environment you are in. It does not hurt to have these items on hand if and when needed.
Gloves, however, are a very important part of the practice, to be available for you at all times. They should be worn in appropriate situations. If you have a patient with an open wound such as a bleeding ear canal, if you are cleaning and disinfecting instruments, or any time you are submerging or removing instruments from a sterilization fluid, you will want to have gloves on to protect your hands from contamination. Your hands are mostly likely to become contaminated with substances such as cerumen. You want to protect them from any ingress of infection throughout the day. It is very important to have the gloves fit appropriately. A properly fitting glove fits very tight. It is not loose at all. It should also be tight around the wrist. You are keeping the potential of infectious agents to move in and underneath the glove. An example of an improperly fitting glove is one that is loose around the wrist. A glove will not protect very well if there is a potential for an infectious agent as it could get down under the glove.
Gloves should be one-time use items. They are disposable which keeps us from cross-contamination. If you put on gloves for one patient because you are worried about blood in their ear canal and you keep those gloves on when modify an ear mold, the gloves have done nothing for protection. You now have potentially cross-contaminated from one patient to the other. You have protected your own hands from that contamination, but the gloves themselves become a transmission agent. Gloves should be disposed of after one use.
Step II: Hand Washing
Hand washing is the number one action you can take to minimize the potential spread of infection in your office. We have been told growing up and especially last year with the H1N1 virus, that we should wash our hands regularly. In the clinical office, hand washing must occur before and after an appointment, after you have used your gloves, and then as needed especially after touching a patient's hearing aids, ear molds, or after modifications. It should be a regular action throughout the day. There is a recommended technique by the CDC. It has six different steps. They are applying soap and water, rubbing the hands together while lathering the soap, thoroughly washing the back of the hands, between the fingers, the fingernails. You should rub your hands together for at least 20 seconds. The CDC says if you sing the song "Happy Birthday" twice to yourself, this would be an appropriate length of time to be scrubbing your hands. Rinse off with water and then dry your hands using a disposable paper towel or a hand air dryer. You should not use a towel that is reusable as there is the potential for cross-contamination.
"No rinse" agents have become quite common today as well. These are appropriate for hand washing as well. "No rinse" agents also have a specific technique for using them. They recommend having no jewelry on your hands. Many facilities recommend not wearing any jewelry at all throughout the day while doing clinical work because of the potential for cross-contamination. You should apply the appropriate amount of a "no rinse" agent to your hands. Rub your hands together, between your fingers, and the back of the hands. You will rub your hands together until the solution dries out. You will not use a towel of any sort as these products are designed for evaporation. Using a towel could lead to potential cross-contamination.
Step III: Cleaning and Disinfecting Surfaces in the Office
Another step of universal precautions is cleaning and disinfecting the surfaces in the office. "Touch and splash" surfaces which are parts of the office that people touch such as the door knobs, toys in the waiting room, headphones, etc. You should clean and/or disinfect any surface in the office that could potentially pick up an infectious agent. We break down the cleaning techniques into three different modes of cleaning. The Environmental Protection Agency (EPA) has different ratings for cleaning fluids and cleaning equipment. Cleaning itself is the removal of gross contamination or contaminated areas. This would be wiping down the surfaces with soap and water or some other agent used for general cleaning, but not necessarily for the killing of germs.
In other areas we should take the next step which is disinfection. Disinfection is done using a cleaning agent that is a hospital grade disinfectant that has been designed to killing a large percentage of bacteria and viruses in the environment. Examples would be to disinfect by wiping down the ear phones on the headsets with a wipe, or wiping down the counter with a hospital grade disinfectant in your hearing aid lab.
The last category is sterilization or killing 100% of germs in the environment. This could be done using a sterilization fluid to sterilize your specula during the day, your OAE tips, your middle ear analyzer tips, etc. There are different categories of cleaning and you need to be aware of what you should use for different types of tools, equipment, and surfaces in the office.
When it comes to disinfectants, you can have hospital grade disinfectants in a variety of forms. There are liquid forms that you would pour and mix with water to clean surfaces. There are spray-on disinfectants as well as towelettes. These types of cleaning agents can be found readily these days in medical supply stores or you could contact your local doctor's office to find where they get their hospital grade disinfectants. We use these disinfectants for "non-critical" items such as wiping down headphones after every patient use and disinfecting ear molds. Many of us have ear mold cleaning fluid that we get from suppliers. You should also disinfect any instruments that are not typically contaminated with bodily fluids such as your desktop or the clipboards you hand out to patients.
Step IV: Sterilization
Sterilization is the maximum step when it comes to cleaning. This is for critical instruments. Critical instruments are tools that potentially come in contact with bodily substances. Again in the clinical/hearing aid dispensing office we are typically talking about ear wax. These instruments would be curettes for cerumen management, specula for the otoscope, tips for the middle ear analyzer, OAE tips, or anything that used in the ear canal or exposed to ear wax. You will want to sterilize these tools if you are not a using disposable version.
You have a few options for sterilization. You could use an autoclave. However typically the equipment we use in the clinical hearing aid office is made of plastic, silicone, etc. The autoclave will melt those types of equipment. You will not be able to autoclave many of the tools we use in the hearing aid office. A hearing aid office will typically utilize "cold" sterilization. This is a soaking fluid with EPA-approved sterilization fluid in it. You can drop your tools into this fluid directly after each use and keep them in it for a number of hours or overnight. Then the audiologist would come in with gloves on, remove the tools from the sterilization fluid, rinse them off, and then lets them air dry. They would then change the sterilization fluid that day. This is probably the most common way of sterilizing the reusable pieces of equipment in a hearing aid dispensing office.
Step V: Infectious Waste Disposal
We also need to think about infectious waste disposal. Typically in the hearing aid office the infectious waste would be ear wax. After you have cleaned a hearing aid with kleenex, wipes, etc., you could probably just throw the kleenex or wipes in the garbage can or waste disposal basket in the lab or dispensing office. You do want to make your staff aware that there are dirty kleenex in the garbage can. You do not want people digging in the garbage for anything because of the wax potentially being present there. The only time you will need to take major precautions for waste in the hearing aid office is if there is a significant amount of blood. If you did have someone who had a small laceration in their ear canal maybe during an ear impression and they are bleeding, you could have oto-dams covered with blood in your garbage can, etc., these need to be disposed of separately. You might want to have a unique garbage can with a plastic liner just for these situations. You may want to have it wrapped up in plastic, double bagged, and set aside. If you do have a situation where you have this type of potential of bodily fluids, other than typical every day ear wax, you should handle it in a different manner of disposal.
Engineering controls are procedures that are designed to isolate potential pathogens in the environment. This could be a unique room that you have for all your sterilization, ear mold impressions, etc. You have engineered the setup of your office to minimize the contact cross-contamination keeping certain types of work done in certain isolated areas of the office. If you have reusable instruments, you want to know that they are put in one place at the end of the day and are sterilized in a specific location. Labeling is very import precaution as well. If you have an area you are doing sterilization, you want to have some form of labeling to let people know that this is where sterilization of instruments is done.
Work controls are now profession-specific procedures. They are different from engineering controls where the work place is setup in a special environment or layout. A work control for the hearing aid dispensing office consists of what procedures should be followed to reduce the risk of cross-contamination. This can include wearing gloves when appropriate or changing the manner we do specific procedures. For example if we are performing cerumen management, we want to put gloves on, whereas we may not wear them during a hearing aid fitting.
Another important part of the safety in our offices is having on-hand material safety data sheets (MSDS). These sheets are information labels for every potential hazardous chemical found in the work environment. If we are working with sterilization fluid, we need to have a MSDS for that particular cleaner. In the hearing aid office, you could be working with chemicals for hearing aid modification, and you will need a MSDS for those particular chemicals. MSDS sheets should be kept on-hand in case of an accident to provide information on how to handle a problem with this particular chemical. The MSDS sheets can be obtained from the manufacturer of that particular chemical, cleaning agent, etc. OSHA does require that these forms are stored somewhere nearby the particular chemicals you are dealing with. For instance, if your sterilization fluid is kept in your lab, you should have the MSDS for that fluid in a cabinet within your lab. We do have MSDS sheets available for any product sold by Starkey. If you were to purchase impression material from us, a monomer or polymer for hearing aid modifications, different adhesives such as ear mold glues, you can get those MSDS sheets from us. It is simply a matter of calling customer service and requesting the MSDS for that particular product. This is true for any supplier as well. OSHA makes it quite clear that MSDS sheets are required literally for any chemical that you may have in your office.
OSHA is the regulatory agency that is responsible for safety protocols in the workplace. This is a United States governmental organization that puts together requirements for safety and health in work place situations. These requirements include infection control. They do require a written infection control plan in any health care setting. The hearing aid dispensing office is categorized as a health care setting. OSHA does have a number of requirements that we will discuss, including:
- Employee exposure classification: Employees have to be categorized for the potential of exposure to infectious agents
- Hepatitis B (HBV) vaccination plan and records of vaccination
- Infection control training plan and records
- Infection control implementation protocols
- Post exposure plans and records: You must have a plan for what happens if there has been exposure to an infectious agent (post exposure) and records documenting the follow up of that case.
Exposure Classification
There are three categories of employee exposure classification: Category I, Category II, and Category III. Category I would be staff members that have the highest potential for exposure to infectious agents. In many cases this would be the clinical audiologist or hearing aid dispenser. Category II would be staff members with slightly less risk, and this is the the typical category for the hearing aid dispensing office, whereas category I could be in a medical facility setting (physicians' office, hospital, etc.). Category II could be the clinical audiologist, dispensing audiologist, hearing instrument specialist, students, interns, etc. Category III refers to those with the lowest risk, including administrative staff, front office staff, bookkeeping and others who are not typically in direct patient contact from the point of view of cleaning hearing aids, etc. Categories I and II are required to practice all of the infection control procedures. They are the front line when it comes to implementing the infection control protocols.
Hepatitis B
Hepatitis B is the most common form of Hepatitis in this country. One in 20 persons is exposed to Hepatitis B, and healthcare workers including hearing aid dispensers and dispensing audiologists are regularly exposed to Hepatitis B.
All Category I and II employees must be offered the HBV vaccination in the office at no charge. The employer needs to maintain records of this vaccination for the full duration of their employment plus another 30 years.
Training Plan and Records
OSHA mandates that you have a training protocol put in place in your office. When you hire a new employee, that employee must be trained on the infection control protocol within 90 days of being employed. There must also be an annual retraining and update of any new information for all staff. These records must be kept for each employee with information that they were trained, when they were trained, and when the reinforcement training occurred.
Implementation Protocols
OSHA does require development of protocols in case of exposure. For instance, some questions to be answered could be what should be done in your office if someone got sick in the waiting and vomited, or what if someone develops a nosebleed and there was quite a bit of blood in the office. You need to have a protocol for what happens if there is the potential for exposure to infectious agents. The number one part of the protocol includes directing the staff members to avoid direct contact with bodily fluids and blood. For example, if someone gets a bloody nose in the front office, no one should run out there and start cleaning up the patient. There have to be protocols that indicate not to touch the bodily fluids, to first put on gloves, and that provide specific cleaning details, etc.
Post-Exposure Plan and Records
The post-exposure plan addresses what happens if someone is exposed to an infectious agent. You must have a plan in place for this particular instance. If exposure occurs, you have to confirm whether or not some form of disease has been transferred. If you had someone who was exposed to blood in your office, you have to setup a protocol to see if there was any type of infectious agent transferred. If that occurred, then you will have implement treatment for that particular infection and confirm the outcome of the treatment. Records need to be kept of the entire incident. This will include circumstances of exposure, the route of exposure, the treatment plan, and then the outcome of the treatment.
Implementation of the Infection Control Plan
It is important to know that all staff members need to understand the infection control plan and be able to implement the plan. This includes the clinical staff, but also the administrative staff as well.
When we talk about best practices for the dispensing office, the number one best practice is hand washing, both before and after each patient contact. Best practices also includes cleaning of tools and ear phones after each use. It is also important to use a device to accept hearing aids from patients and move them about the office. You may have patients who drop off their hearing aids for cleaning. You do not want the receptionist or front office staff putting the hearing aids in their hands. There needs to be some kind of plastic container that the hearing aids can be placed in, taken back to the lab, and the container can then be sterilized or disinfected after each use. It is very common for us to just accept hearing aids from patients in our hands, but we should really use a storage device instead. Using personal protective equipment when handling hearing aids or modifying them is a best practice as well.
Is bar soap acceptable for hand hygiene?
No it is not for a couple of reasons. Hand soap is not medical grade and is not an EPA-approved hospital grade disinfecting hand cleaner. Also since it is not in an enclosed container, hand soap or bar soap could potentially be a transmitter of cross-contamination. You really need to have hospital grade liquid hand soap in a closed container.
Why is it inappropriate to top off liquid soap?
This comes down again to cross-contamination. Opening and closing the liquid soap container or liquid hand disinfectant container means you are now exposing the cleaning fluid or material to potential airborne or droplet infectious agents. You should be using disposable dispensers.
Why do I have to implement hand hygiene after the removal of gloves?
This again comes down to cross-contamination. You have used the gloves to clean a hearing aid, modify a hearing aid, or to take an ear impression. In the process of taking them off, you could have contaminated your hands with whatever was on the gloves.
Do I always use gloves when handling hearing aids or impressions?
No. If you know the hearing aid is clean, you probably do not need to wear gloves. It is not practical in every situation to put on gloves when handling a hearing aid or ear mold. If you are performing a brand new fitting, taking a hearing aid straight out of the box and putting it in the patient's ear, you probably do not need to put gloves on. We all know that there are patients that come in who have very dirty hearing aids and for those patients, you should put on gloves when you clean their hearing aids. You may not have gloves on when the patient places their hearing aids into the receptacle and you carry them back to be cleaned. However you will then put your gloves on, clean the hearing aids, take the clean hearing aids, put them in a clean receptacle, take your gloves off, wash your hands, and take the hearing aids back to the patient.
Dispensing practices are considered health care providers and are under the regulation of OSHA. We are required to follow the OSHA guidelines for infection control and training procedures. We also need to follow the CDC Universal Precautions, which are recommendations for protection of cross-contamination. Hand washing is probably the number one recommendation and should be done by everyone in the office regularly throughout the day. Universal precautions also include general cleaning of surfaces, disinfecting of surfaces that could be exposed by hearing aids and ear molds, and sterilization of those pieces of equipment that are reusable such as specula and curettes. You need to implement an infection control plan for all staff; having it written down in the office is not enough. You should keep all the records of the training, what the protocol is, and follow up on any situation where there was the potential for infection. This was a brief overview of infection control and how it relates to the hearing aid dispensing practice, and I hope you have found it useful. If you have further questions regarding OSHA guidelines, please refer to the OSHA website.
Reference List
Bankaitis, A. & Kemp, R. (2002). Hearing aid-related infection control. In: M. Valente (Ed.), Strategies for selecting and verifying hearing aid fittings, 2nd edition (pp.369-383). New York, NY: Thieme Medical Publishers, Inc.
Bankaitis, A. & Kemp, R. (2003). Infection control in the hearing aid clinic. Boulder, CO: Auban.
Bankaitis, A. & Kemp, R. (2004). Infection control in the audiology clinic. Boulder, CO: Auban.

