According to Wikipedia, the earliest citation of "red flag" used as a warning signal dates back to 1777 and was used to alert people about an impending flood. The term and the expression "to raise the red flag" is a common expression. The semaphore red flag (or red light) on railways means an immediate stop, while a red flag is frequently flown by armed forces to warn the public of live fire exercises in progress, and is sometimes flown by ships carrying munitions. Although the term sounds pretty ominous, it's a descriptive way to warn people about something. The term "red flag" is actually quite common in many professions, including meteorology, telecommunications, medicine and the military. Since it's such a descriptive term, we thought the term "red flag" may be applied to the hearing aid selection process as a way to provide both patients and audiologists with some advanced warning of a challenging situation involving the selection and use of hearing aids. This article is intended to introduce the term "red flag" to the hearing aid industry and explain how the findings of two easy-to-conduct pre-fitting tests can be plotted as a single point on the Red Flag Matrix for use in the hearing aid selection and fitting process.
Difficulty in background noise is the primary complaint of many hearing impaired patients and hearing aid users. Among the difficulties these patients experience are poor speech intelligibility in noise and annoyance from sound. Over the past several decades audiologists have relied on the standard battery of pre-fitting tests (i.e., word recognition is quiet and the pure tone audiogram) to make a determination about hearing aid candidacy and to help establish expectations with amplification. Although the standard pre-fitting battery of audiological tests are useful for quantifying the degree and type of hearing loss, their relatively poor face validity suggests these tests have substantial limitations in the counseling process. Specifically, the results of both pure tone audiometry and speech recognition testing in quiet have been shown to have a weak relationship at best to real-world hearing aid outcome. (See Taylor, 2008 for a literature review).
Another important consideration is patient comprehension of audiological test results. According to Margolis (2004) up to 80% of the information a clinician shares with a patient is forgotten immediately. An important ingredient of effective communication is the clinician's ability to convey technical information in a clear and concise manner. Combining two test scores as a single point on a matrix enables clinicians to communicate test results more effectively, which may lead to improved patient retention of the information.
An inability on the part of the audiologist to measure these "real world" problems with the traditional battery of pre-fitting tests, combined with poor patient retention of the results may contribute to non-use, returns for credit and lower than expected real-world hearing aid benefit. The purpose of this study was to investigate the clinical utility of a four quadrant matrix that could be used to plot the results of two commercially available tests, the Quick Speech in Noise (QuickSIN) and Acceptable Noise Level (ANL) tests. Our working hypothesis is that measuring speech intelligibility in noise with the QuickSIN and annoyance from sound with the ANL during the pre-fitting appointment, before patients begin using amplification, helps establish precise realistic expectations with each patient prior to their initial trial with hearing aids. Taken a step further, providing the patient with insight on their ability to understand speech in noisy listening conditions and annoyance from various environmental sounds may also contribute to more successful hearing aid outcomes. This concept is similar to how a surgeon would discuss a prognosis with a patient using pre-operation test results. Audiologists could use the results of the QuickSIN and ANL plotted as a single point of the Red Flag matrix to set the stage for those patients "at-risk" for non-use and poor benefit in noise.
The QuickSIN and Acceptable Noise Level Tests
Although various speech-in-noise tests have been commercially available for several years, survey data indicates they are seldom used by clinicians. Several reports have suggested that incorporating speech-in-noise tests into a routine battery of pre-fitting tests has clinical value. Wilson and McArdle (2005) and Wilson (2004) have reported that speech-in-noise scores cannot be predicted from speech in quiet scores for many patients. They concluded that speech-in-noise testing should be part of a clinician's routine battery of audiological tests. Wilson and colleagues' thread of research in this area would suggest that the scores on speech-in-noise tests provide valuable insight into speech understanding ability in everyday listening situations.
In addition to speech-in-noise tests being used to objectively measure speech understanding ability, these tests can also be employed to measure other facets of communication, such as annoyance from noise and subjective ability to understand speech. The Acceptable Noise Level test has been studied extensively (See Freyaldenhoven, Plyler, Theli, & Hedrick, 2007 for a review). Nabelek and colleagues (2006) have reported that annoyance is a predictor of hearing aid non-use.
Combining an objective measure of speech understanding in noise with a subjective component, Saunders & Cienkowski (2002) developed the Performance-Perceptual Test (PPT). Using the Hearing in Noise Test (HINT), the PPT is a two-step process. First, an objective score on the HINT is obtained. This is followed by a second run of the HINT in which the patient is asked to subjectively rate their ability to understand at various signal-to-noise ratios (SNRs) on the HINT. The clinician then compares the objective HINT score to the subjective HINT score, which is called the Performance Perceptual Discrepancy (PPDis). Results are placed into three possible categories: "Under estimators" (those that understand speech better than they think), "Over estimators" (those that overestimate how well they understand speech in noise) and "Accurates" (those that accurately assess their ability). Saunders and Forsline (2006) have devised an entire counseling protocol based on the results of the PPT.
A recent study by Mueller, Johnson and Weber (2010) suggests that the QuickSIN, ANL and PPT tests provide useful, non-associative information about the patient's communication ability, and recommends that all three of these tests be conducted during the pre-fitting appointment. Given these research findings, it is reasonable to include some type of speech-in-noise testing into the pre-fitting battery. The challenge for the clinician, however, is incorporating all three speech-in-noise tests into their pre-fitting battery of tests. For example, the PPT uses the HINT, which is rarely used clinically for various reasons; therefore, it may not be practical to conduct the PPT in a clinical setting.
From a commercial standpoint, expert opinion suggests the routine use of speech-in-noise tests. The Hearing Instrument Association's Hearing Aid Delight study (Rogin, 2009) reveals a relationship between computer-based testing and patient satisfaction. In addition, Sweetow and Sabes (2010) proposed the use of a functional communication assessment, in which two objective and two subjective measures of the residual auditory system are used. For these reasons routine testing of speech intelligibility in noise and annoyance from sound would be warranted prior to prescribing amplification.
Our purpose was to investigate the feasibility of incorporating these research findings into a simple, executable clinical procedure that would enable clinicians to make better hearing aid selection and counseling decisions without adding significantly more time to the appointment. Due to their relative ease of use and availability, the QuickSIN and ANL were integrated into one clinic's routine battery of pre-fitting tests. Table 1 summarizes the essential details of each test. 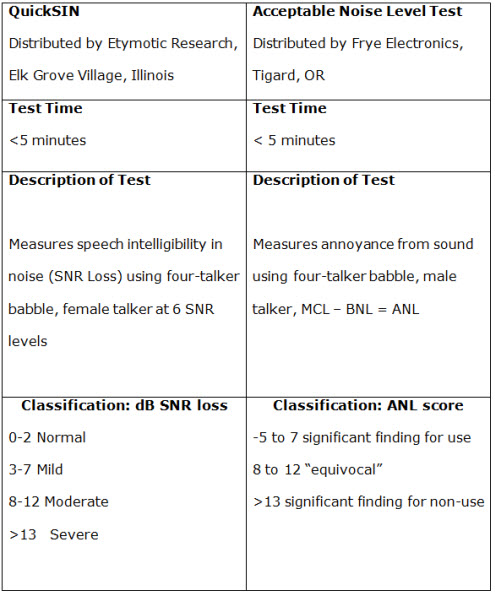
Table 1. Summary of QuickSIN and ANL tests
Methods and Results
Forty-seven randomly selected patients received a comprehensive audiological evaluation from the Hearing Evaluation Services of Buffalo, NY. Twenty-two of the 47 patients were current hearing aid users and another 11 of them were considered hearing aid candidates. This evaluation consisted of pure tone and immittance audiometry, word recognition in quiet, and speech-in-noise testing with the QuickSIN and the Acceptable Noise Level test. Word recognition testing was conducted in each ear separately, and both the QuickSIN and ANL were conducted binaurally. The mean tests results along with ranges are shown in Table 2.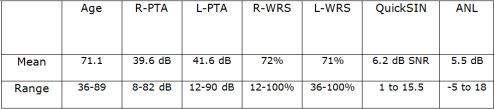
Table 2. Summary of test results for 47 patients.
Of the 47 patients participating in this study, 22 wore hearing aids. A summary of these results are shown in Table 3. 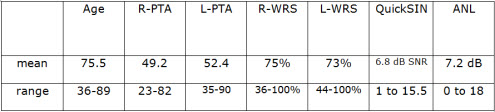
Table 3. Summary of test results for 22 hearing aid users
The Red Flag Matrix
Using the published normative results of QuickSIN and ANL studies (summarized in Table 1), the Red Flag Matrix was developed in order to more precisely identify patients who might be considered at-risk for struggling with speech intelligibility in noise or annoyance from sound prior to receiving hearing aids. The point of intersection of the four quadrants is 7 dB. This intersection point is based on QuickSIN and ANL research. According to Killion & Niquette (2000) QuickSIN scores of 7 dB or less indicate a near-normal or mild SNR loss and well-fitted directional microphones is thought to bring aided speech intelligibility scores back to into the normal or near-normal range. ANL scores of 7 dB or less is considered a predictor for full-time hearing aid use according to Nabelak and and colleagues (2006).
After the results of the two tests are obtained, the clinician can plot a single dot on the matrix, which represents the QuickSIN and ANL score as a single point. The lower left hand quadrant of Figure 1 (Q1) is labeled the "in the clear" zone because both the unaided QuickSIN and ANL scores are in the near normal or mild SNR loss range. When results fall into this quadrant, the patient would expect minimal problems with intelligibility and annoyance in background noise when amplification is used.
The upper left hand quadrant of Figure 1 (Q2) are patients with near normal or mild SNR loss QuickSIN scores and elevated ANL scores (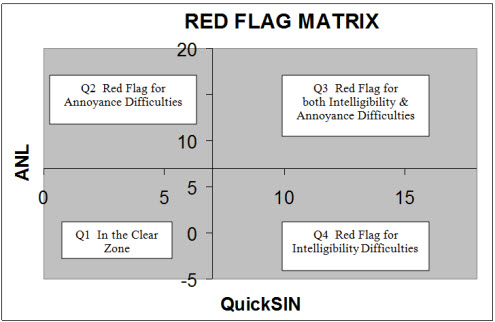
Figure 1. The Four Quadrants of the Red Flag Matrix
The upper right corner (Q3) of the Red Flag Matrix denotes patients with significant SNR loss on the QuickSIN (>7 dB) and a significant ANL scores (>7 dB). Based on published research, hearing aid users with these scores are at-risk for difficulties with annoyance and speech intelligibility in noise. Finally, the lower right hand corner (Q4) are patients with no measurable annoyance problems, but a significant SNR loss. Q4 patients would be at-risk for difficulties with speech intelligibility in noise, but no indication of a problem with sound annoyance. 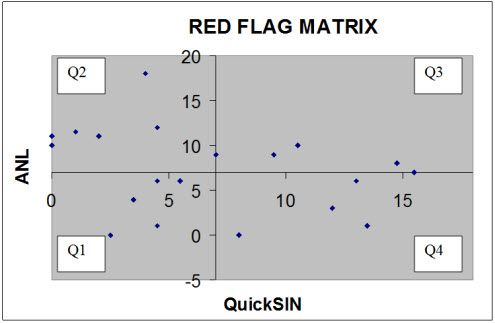
Figure 2. Current Hearing Aid Users
Figure 2 shows the results for 22 current hearing aid users on the Red Flag Matrix. Table 4 shows the dispersion of scores. Although hearing aid benefit and satisfaction was not measured, considering all 22 patients are full time hearing aid users, we can presume some level of satisfaction and/or benefit is being achieved. Results plotted on the Red Flag Matrix for each of the 22 hearing aid users would suggest that a poor score (red flag) on either test is not necessarily equated with poor outcomes. 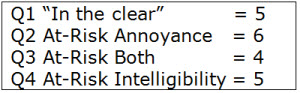
Table 4. Dispersion of Scores
The results from 11 hearing aid candidates for the QuickSIN and ANL are plotted on the Red Flag Matrix in Figure 3. Five of the candidates fell into Q1 suggesting they have no red flags for annoyance or intelligibility in noise. Four candidates are in Q2, suggesting they may be at-risk for annoyance problems. Two candidates were in Q4, indicating a red flag for speech intelligibility in noise difficulties. 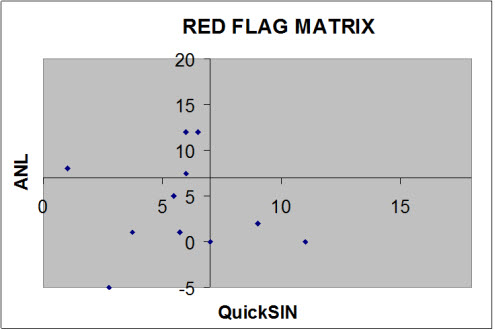
Figure 3. Results for 11 current hearing aid candidates
Potential Uses of Red Flag Matrix
The purpose of this study was to evaluate the feasibility of conducting the QuickSIN and ANL during the pre-fitting appointment and plotting the results as a single point on a four quadrant matrix. Based on our preliminary experience with the Red Flag Matrix it is a tool that provides specific insights into common communication problems not readily quantified by the traditional battery of pre-fitting tests. We believe it has the potential to be an essential tool for dispensing audiologists for the following reasons.
- Plotting the scores from the QuickSIN and ANL as a single point on a matrix can lead to more precise patient counseling. By plotting the score as a single point and placing that single point in one of four points on the matrix, patients have an easy-to- understand visual representation of their results in relation to other patients.
- Using this approach, patients can be informed of being at-risk for non-use or less than expected benefit in noise with amplification prior to using hearing aids. Because the results of the individual patient can be compared to the normative data collected on the QuickSIN and ANL tests, patients are informed of their results using an evidence-based approach. If a red flag is present for problems with sound annoyance or speech intelligibility in noise, implications can be discussed in a straightforward manner with patients.
- More precise or systematic decisions about hearing aid technology and special features can be made during the selection process. In theory, patients who fall into Q4 are challenged by both annoyance and intelligibility issues. Currently, to our knowledge there are no hearing aids with automatic switching algorithms, which have the ability to simultaneously optimize performance for both comfort and clarity. Therefore, patients who fall into Q4 might be strongly advised to use manual or remote control of their instruments. Patients with scores in Q4 would be encouraged to utilize manual control allowing for manipulation of multiple features that optimize for both comfort and clarity in background noise.
- Aided scores on the QuickSIN and ANL could be plotted on the matrix and compared to the unaided condition, thus the Red Flag Matrix could be used as an informal outcome measure. Comparing the aided to the unaided score on the matrix could be a meaningful patient demonstration of improvement with amplification, using tests that simulate real world listening.
References
Freyaldenhoven, M., Plyler, P., Thelin, J., & Hedrick, M. (2007). The effects of speech presentation level on acceptance of noise in listeners with normal and impaired hearing. Journal of Speech, Language & Hearing Research, 50, 4, 878-85.
Killion, M. & Niquette, P. (2000). What can pure tone audiometry tell us about a patient's SNR loss? The Hearing Journal, 3(3), 46-52.
Margolis, R. (2004). What do your patients remember? The Hearing Journal, 57(6), 10-17.
Mueller, G. Johnson, E., & Weber, J. (2010). Fitting hearing aids: A comparison of three pre-fitting speech tests. AudiologyOnline Article #2332. Retrieved on June 24, 2011 from the Articles archive on www.audiologyonline.com
Nabelek, A.K., Freyaldenhoven, M.C., Tampas, J.W., & Burchfield, S.B. (2006). Acceptable noise level as a predictor of hearing aid use. Journal of the American Academy of Audiology, 17(9), 626-639.
Rogin, C. (2009). Top 10 Reasons for hearing aid delight. AudiologyOnline Recorded Course #14615. Retrieved on April 1, 2011 from the eLearning Library on www.audiologyonline.com
Saunders, G.H., & Cienkowski, K.M. (2002). A test to measure subjective and objective speech intelligibility. Journal of the American Academy of Audiology, 13(1),38-49.
Saunders, G.H., & Forsline, A. (2006). The Performance-Perceptual Test (PPT) and its relationship to aided reported handicap and hearing aid satisfaction. Ear and Hearing, 27(3), 229-42.
Sweetow, R. & Sabes, J. (2010). Auditory training and challenges associated with participation and compliance. Journal of the American Academy of Audiology, 21, 586-593.
Taylor, B. (2008). Audiologic Predictors of Real-World Hearing Aid Success: An Evidence-Based Review. AudiologyOnline Article #2098. Retrieved from the Articles archive July 8, 2011 on www.audiologyonline.com
Wilson, R. (2004). Adding speech-in-noise testing to your clinical protocol: why and how. The Hearing Journal, 57, 2, 10-18.
Wilson, R. & McArdle, R. (2005). Speech signals used to evaluate functional status of the auditory system. Journal of Rehabilitation Research & Development, 42, 4, 79-94.


