 From the Desk of Gus Mueller
From the Desk of Gus Mueller
Like most things in the practice of audiology, the selection and fitting of hearing aids is evidence based. We use the research literature to base our decisions of what prescriptive methods to use, how these methods are best verified, and what real-world self-assessment inventories provide the most valid measure of outcome. Likewise, without well-designed, peer-reviewed published studies, we would have no way to really know if new features and algorithms truly provide patient benefit. Keeping up with the hearing aid literature, however, is not an easy task as over 100 articles are published each year. To do the math for you: If you obtained your degree just 10 years ago, but haven’t been doing much reading, you’re already behind by over 1000 articles!

Gus Mueller
Twelve years ago, Catherine Palmer, Bob Turner and I decided to help out a little. Each year since we have had a session at the annual Academy of Audiology meeting where we present 15-20 of our favorite hearing aid related articles of the past year. It’s usually well received, as attendees often then feel “okay” about going back to their office and filing away the journals stacked on their desk. It seemed appropriate, therefore, to share our review of the past year with 20Q readers, and Catherine was kind enough to write up our thoughts, and appropriately, added a few more of her own.
Catherine Palmer, PhD, is an Associate Professor in the Department of Communication Science and Disorders at the University of Pittsburgh and serves as the Director of Audiology and Hearing Aids at the University of Pittsburgh Medical Center. She teaches the graduate level amplification courses at the University of Pittsburgh and serves as Editor-in-Chief of Seminars in Hearing. Dr. Palmer is internationally known for her applied research related to hearing aid selection, fitting and verification. Dr. Palmer opened the Musicians’ Hearing Center at the University of Pittsburgh Medical Center in 2003. This work has included a partnership with the Pittsburgh Public Schools and the Pittsburgh Symphony that promotes hearing protection for young and professional musicians.
As I mentioned, Catherine, Bob and I have been doing the Hearing Aid Journal Club featured session at the Academy meeting for 12 years. Each year, Catherine volunteers to talk about the pediatric articles, partly because it provides the opportunity for her to show photos of her two sons—now 18 and 16. There was even more reason to show their photos at the most recent Academy meeting, as both of them had research posters accepted. Who knows, maybe in the next year or two we’ll be reviewing their publications . . . or it could be yours!
Gus Mueller, PhD
Contributing Editor
May 2014
To browse the complete collection of 20Q with Gus Mueller CEU articles, please visit www.audiologyonline.com/20Q
20Q: A Review of 2013 Hearing Aid Research—Tips for the Clinician

Catherine Palmer
1. What prompted you to review all these articles? Sounds like a lot of work.
It is a lot of work, but well worth the effort. As you might know, Gus Mueller, Bob Turner, and I have been doing Hearing Aids in Review as a Featured Session at the Academy of Audiology annual conference for the past twelve years, so this is an annual event for me. Our goal is to look through the past year’s hearing aid articles and find the handful that provide findings that can be used by clinicians Monday morning. There are a lot more hearing aid articles out there than you might think. This year we found 214 articles from 26 journals, and from this, picked a set that we believed had a message that would be most useful for clinicians. It is a completely arbitrary process and I’m sure there are some very good, useful articles out there that we didn’t review, but I can tell you about the ones we did choose.
2. Is there a certain way that you organize the material?
We typically put all of the articles into one of six categories. Our categories represent how you might think about a hearing aid fitting from start to finish and include: Pre-fitting Assessment, Signal Processing and Features, Selection and Fitting, Verification, Pediatric Issues, and Real-world Outcomes.
3. Okay, let's start with pre-fitting—any interesting articles in that area?
There was one that we liked that wasn’t specifically related to pre-fitting testing, but more related to pre-fitting decision making. Many of us have been faced with patients who are not sure if they want to purchase one or two hearing aids even after we’ve explained all the benefits of listening with two ears. We have to decide if we should push them to start with two, knowing that they could always choose to ultimately go with one, or would a more reasonable approach be to have them adjust to using only one, and then add the second one at a follow-up visit? Lavie and colleagues (2013) looked at the question of fitting bilateral hearing aids in a simultaneous versus sequential manner. Thirty-six new hearing aid users (64-88 years of age) with bilateral symmetrical sensorineural hearing loss were put into one of two groups. Twelve were fit bilaterally on the first day and 24 were fit sequentially with one hearing aid for a month before adding the second hearing aid. Participants were interviewed every 10 days and a compliance score was given. Data logging of hearing aid use was recorded as well. Compliance scores were based on use of hearing aid(s), patient report of good hearing, comfort with hearing aids, and satisfaction. After the first month, the compliance score for both groups was the same (75%). There was no change for the simultaneous group after the second month. For the sequential group, however, 17 of 24 participants had reduced compliance following the fitting of the second hearing aid. The data logging revealed that the simultaneous group had the same amount of use for both months. In the second month, the sequential group reduced use for the ear originally fitted and had an even lower use for the second ear fitted. Although the authors suggested that there may have been deprivation (the so called “unaided ear effect”), a more likely explanation comes from a number of participants expressing disappointment in the benefit provided by the second hearing aid compared to only having one. If you have found some benefit with one hearing aid you may expect that same degree of change or increased benefit from the second aid (e.g., expecting a doubling of benefit) which is not likely with the addition of a second hearing aid. For me, the take-away message here is that if you have a patient who is a candidate for bilateral amplification, you would be wise to fit them bilaterally from the beginning to increase the likelihood of success with bilateral amplification.
4. Haven't you talked about bilateral versus unilateral fittings in the past?
Yes, this has been a topic of interest in recent years. For example, Walden and Walden (2005) stirred up quite a bit of interest when they reported that based on QuickSIN scores, many patients performed better with one hearing aid rather than two in a laboratory setting. I picture McArdle and colleagues (2012) thinking about these results for a few years and deciding they just couldn’t live with them, so they designed a study to see if they could find an explanation for this finding. They found that the majority of their participants did best in the bilateral condition with only 20% doing better in the unilateral condition. Plugging the non-test ear had a significant impact on reversing the finding between the two studies. It’s probable that people with mild to moderate hearing loss actually were getting a bilateral signal in the Walden and Walden study for the unilateral condition, because their unaided ear was not plugged. It’s important to point out that in this study, the QuickSIN sentences were presented at 70 dB HL, a considerably higher level than normally used for aided bilateral versus unilateral comparisons.
Another related study that we reviewed recently was by Robyn Cox (2011), who looked at real-world preference for unilateral and bilateral fittings. Ninety-four participants with bilateral symmetrical sensorineural hearing loss were fitted bilaterally and participated in a 12-week field trial. At the conclusion of the trial, 46% chose to use only one hearing aid. Interestingly, the people who chose to use two had better real world outcomes.
5. Interesting stuff. So what pearls did you find in the area of signal processing?
There were quite a few good ones in 2013, but let’s start with the telephone. As you know, telephone communication is essential for everyone whether it is for work, pleasure or safety. Picou and Ricketts (2013) tested six telephone listening strategies with 18 adults (49-88 years) who had moderate-to-severe sensorineural hearing loss. The strategies included: acoustic telephone with and without the contralateral ear plugged; unilateral telecoil with and without the contralateral ear plugged; unilateral wireless streaming; and bilateral wireless streaming. They evaluated speech recognition, ease and comfort of listening in each condition at two levels of noise. They reported that acoustic telephone listening does not go well in noise. Unilateral telecoil and unilateral wireless streaming improved performance but bilateral wireless streaming worked the best. The signal-to-noise ratio achieved by each strategy predicted the results.
6. A colleague informed me that you talked about Iowa Interstate 80 in your Academy presentation? I’m wondering how this fits into hearing aid signal processing?
Well, I’m always fond of articles with some “real world” face validity, and sometimes you just need an Interstate to make that happen! Lots of patients talk about having a difficult time communicating in the car. Wu, Stangl, Bentler, and Stanziola (2013) decided to literally take this issue to the streets. They looked at five signal processing schemes for communicating in an automobile. These included omnidirectional, conventional adaptive directional, back directional, side-transmission, and side-suppression signal processing implemented in one of three hearing aids. Twenty-five adults with bilateral sloping sensorineural hearing loss (44-84 years old) listened to pre-recorded signals from a traveling van. The auto/road noise and sentences of the connected speech test (CST) were recorded through hearing aids in KEMAR’s ears while he sat in the passenger’s seat (that may go without saying) of a standard van moving at a speed of 70 mph on Iowa I-80 between exits 249 and 284 (location given in case you want to replicate this study; the world’s largest truck stop is at Exit 284). The sentences were presented from the side and back of the hearing aids for the recordings. Listeners then heard these recordings through headphones and speech recognition performance and preferences were assessed. Their findings (Table 1) indicated that the newer signal processing schemes were preferred for back and side sound presentations as compared to the omnidirectional or conventional adaptive directional signal processing. Now, it might be obvious that speech from the back would not be processed effectively with conventional directional. Consider that for some instruments, however, if you have them programmed in the automatic directional mode, they indeed would be in conventional directional for this listening situation.
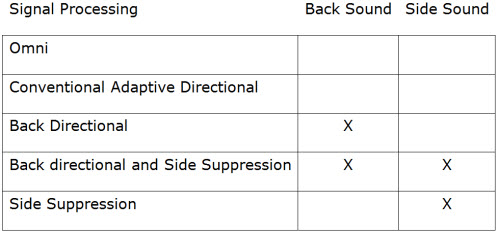
Table 1. The “X” indicates that the particular signal processing was superior to Omni and Conventional Directional Signal Processing in either the Back Sound or Side Sound configuration.
7. Seems like there are always some good hearing aids studies coming out of the University of Iowa.
I agree. For many years we’ve seen the articles from Ruth Bentler, and now Wu seems to be publishing his fair share, too. His research consistently asks important questions, which then lead to answers that help inform clinical practice. For this reason, I’ve selected another Wu article. Wu and Stangl (2013) decided to take a look at how the Acceptable Noise Level (ANL) test is impacted by three signal processing techniques - wide dynamic range compression (WDRC), digital noise reduction (DNR), and directional microphones (DIR). Most importantly (in my opinion), Wu hypothesized that the ANL would be predicted by the signal-to-noise ratio that reached the eardrum of the listener, and that any impact that these signal processing schemes have is related to how they enhance or decrease signal-to-noise ratio.
In case you haven’t thought about the ANL test lately, here is a quick review. The ANL is the lowest signal-to-noise ratio a listener is willing to accept while listening to speech presented at their most comfortable listening level while still following the speech. The highest noise level that the listener will “put up with” is subtracted from their MCL, which then gives you the ANL (which is a signal to noise ratio; SNR). There has been some research indicating that the ANL is highly predictive of hearing aid success, as defined by full time use (Nabalek, Freyaldenhoven, Tampas, Burchfield, & Muenchen, 2006). So impact on the ANL would be important, e.g., if a signal processing scheme worsened the aided ANL, that might predict compromised hearing aid success. Twenty-five adults with sensorineural hearing loss (35-82 years of age) used hearing aids set to NAL-NL1 targets of the average hearing loss of the group. The ANL was measured monaurally in the sound field across seven listening conditions (mix of signal processing schemes and location of noise either front or back). Wu and Stangl (2013) found WDRC worsened the ANL (1.5 dB) while DNR and DIR improved ANL by 1.1 and 2.8 dB, respectively. They concluded that WDRC creates a noisy sound image which has benefits in terms of audibility for soft sounds but it changes the SNR. Their suggestion is to use DNR with WDRC and thereby cancel out the negative effect, which is what we typically do. The addition of DIR produced a positive effect.
Now, you might be asking, did the participant’s ANL actually change, or was it simply the result of processing changes of the earcanal SPL SNR? Fortunately, the authors answered this question. The hearing aid output SNR was measured for each condition. You are probably wondering how in the world one can measure the SNR once the signal and noise have been simultaneously processed by the hearing aid. I have three words for you: Phase Inversion Technique (actually Wu and Stangl had these three words for you). Anyway, you present two speech-plus-noise signals to the hearing aid sequentially. The speech components are identical but the noises are out of phase. Adding and subtracting the two recordings give the extracted speech and noise signal after hearing processing. They found that the hearing aid output SNR could predict the pattern of ANL changes caused by the various signal processing schemes. So in the ANL task, it appears that the listener is adjusting the noise related to the signal to maintain a constant SNR at the eardrum across listening conditions. This is a powerful finding for the clinician because it supports the premise that everything we can do to enhance SNR for the listener will increase the likelihood of successful device use, and more importantly, successful communication. This goal of enhancing SNR is also consistent with the Picou and Ricketts (2013) telephone findings that I mentioned earlier.
8. One signal processing feature that I’m still trying to understand is frequency lowering. Did you find any good articles on that topic?
There was one that I liked. Arehart, Sousa, Baca, and Kates (2013) took an interesting approach to this topic. When you think about it, every type of advanced signal processing, in some way distorts the original signal reaching the hearing aid. Of course, the impaired system distorts it even more. The question always is: Does the particular distortion do more good than harm for communication? Frequency lowering is no different. It is definitely a form of distortion that makes inaccessible sound accessible to some users. Arehart et al. wanted to find out if individuals’ working memory impacted their ability to make use of this newly accessible sound.
Working memory allows a person to actively store task-related information while concurrently carrying out other relevant processing. These resources are considered to be both finite and limited. The authors were interested in working memory because they hypothesized that listeners may need to allocate a greater share of processing resources to the recovery of degraded information (in this case, the frequency-lowered signal), leaving fewer resources available for successfully processing the linguistic content of the message.
Twenty-six adults with sensorineural hearing loss (62-92 years of age) repeated low-context sentences played in quiet and in varying levels of noise. Signal processing included no frequency compression and three compression ratios paired with three cut-off frequencies. The signals were amplified using NAL-NL1 prescriptions and were presented under headphones. Working memory was assessed with the Reading Span Test (RST). The amount of distortion in each condition was quantified by the Hearing Aid Sound Quality Index (HASQI) that assigns a number from 0 to 1 based on similarity of the original signal to the processed signal (1 being identical). The authors found that people with good working memory (defined by >.37 on the RST) did better across levels of distortion and signal to noise ratios (until -5 dB SNR, when everyone did poorly). They found that those with poorer working memory still received benefit from amplification and this particular signal processing feature, but not as much as those with good working memory. So as long as we talk about benefit from signal processing in relative terms to how the person performs without audibility, these findings suggest there is benefit to be had, but working memory mediates the absolute benefit.
9. So, if I understand this correctly, it appears that the types of subjects that are included in hearing aid studies could impact the benefit of different signal processing schemes?
Absolutely. And in fact, we included a slightly different type of review at the end of the Signal Processing/Feature section this year that looked at the very question you are asking. What factors will impact the findings of research studies related to signal processing? Here are a few examples.
Dawes, Hopkins, and Munro (2013) report data that are in line with data we reviewed from Bentler, Niebuhr, Johnson, and Flamme in 2003. Subjects have a tendency to prefer the hearing aid that is labeled as the new technology. So one can imagine that whatever the “other” aid is, will be perceived as less helpful. This could be last year’s technology or a competitor’s technology. The results can be predicted by how you labeled the hearing aids. The way to prevent this is to blind the study. A double-blinded study means that the participant does not know what condition he is listening to and the researcher collecting the outcomes data does not know either. Clinicians definitely want to put more faith in evidence coming from double-blinded studies.
In another example of how test procedures impact outcome, Wu, Stangl, and Bentler (2013) set up an experiment to test the new anti-cardioid algorithm that was designed to improve hearing from the back when the speech signal of interest is coming from behind the person. They compared this to omnidirectional and traditional direction by having individuals repeat HINT sentences presented from behind with the noise in front. The first iteration of this study found that the new technology did not work. Upon further investigation Wu and colleagues found that they had created a test situation that did not engage the technology appropriately. When they made a slight change in the presentation of the test sentences (adding a short introduction phrase), they found the results that were what would be expected based on the physical measurements of the microphone’s response. Researchers have to be vigilant to make sure they are actually creating listening situations where the signal processing they are trying to evaluate is actually activated appropriately. This type of study that is conducted in a laboratory setting is testing the efficacy of a signal processing scheme. Efficacy tells us if the signal processing can work under the ideal conditions it was meant to work under. Testing efficiency is a different matter. This is when we are testing the signal processing in the real world with very little control over the communication environment. To tie all this together—the Wu “Interstate I-80” study that I talked about earlier, was an efficiency study of the same instrument used in this efficacy study.
Another interesting study, that directly addresses your question, was one conducted by Ng, Rudner, Lunner, Pedersen, and Ronnberg (2013), who looked at the impact of working memory and the benefit derived from digital noise reduction. Participants were assessed on their ability to repeat and recall the last word of sentences under two noise conditions with and without noise reduction. Working memory was tested by the Reading Span Test. They found that noise reduction can reduce the adverse effect of noise on recall for speech but only for persons with good working memory capacity. So, if you carefully measure working memory and only include individuals with good working memory you will find that your noise reduction technology works, but if you randomly assigned subjects into your study you might not find an effect because of the mix of working memory in the groups. Most studies carefully control the degree of hearing loss between their groups when evaluating signal processing, but these data indicate that other participant variables that may impact results.
10. So what can we do about this?
As researchers, we need to be vigilant about understanding the participants who are in our studies. There are times when we may want to take all comers because we are looking at the benefit of a signal processing scheme on average. In other studies, we may want to know about the impact of signal processing with a specific group. As soon as you create a group you are in danger of missing important differences among the members you are testing. For the clinician, this is why being a critical consumer of the research is essential. You have to decide if the study you are reviewing applies to your particular patient as you engage in evidence based practice.
11. So what else was new in the signal processing area?
Well, trainable hearing aids aren’t new, but Keidser and Alamudi (2013) looked at the efficacy and reliability of training a hearing aid in everyday environments. For clinicians interested in using a trainable hearing aid as part of their fine-tuning protocol, these data are helpful. Twenty-six older adults with an average PTA of 53 dB HL were fit with hearing devices set to NAL-NL2 prescription. They wore the devices for three weeks and trained the devices from the prescribed fitting for three weeks. Nineteen participants were reset to the prescriptive fitting and trained again to check reliability of training. For the last two weeks, participants could compare the prescription to the trained response. Training was implemented through the user manipulating a remote control that enabled changes of the compression characteristics in four frequency bands and in six sound classes. About half the participants made too few changes to be able to distinguish between the prescribed and trained response. More daily adjustments lead to training across more sound classes. Those who did make noticeable changes had higher overall satisfaction. Outcomes from the repeated training sessions were significantly correlated for two thirds of the participants. So, the authors concluded that individuals are reasonably reliable in this activity, but at least 50% don’t really make significant changes even when given the opportunity. In fact, the most interesting data from this study show the average deviation from the NAL-NL2 prescription for the entire group, and these data indicate that on average, individuals don’t deviate more than 5 dB through 4000 Hz from the NAL-NL2 prescription for moderate and loud inputs. The deviations are slightly larger in the higher frequencies for soft inputs which would make sense because these would be the sounds least likely to be accepted by new hearing aid users. So, it looks like fitting to an evidence-based prescriptive formula continues to make good sense and produce good results. Allowing individuals to train the hearing aid may increase satisfaction without deviating substantially from a fitting known to provide the audibility needed to communicate successfully.
12. Were there any other articles regarding the use of prescriptive methods?
We’ve heard a lot recently about the NAL-NL2 and the DSL 5.0. The verdict seems to be that either prescription will work quite well along with some minor fine–tuning. Most importantly clinicians should use one of the two evidence based formulas for generating targets for their fittings. But, I bet you haven’t seen anything about the prescriptive requirements for conductive and mixed hearing losses for a while. In fact the first recommendation for how to deal with a conductive component in a prescriptive formula came from Lybarger in 1963. He suggested the formula: 25% ABG + AC (AC: air conduction; ABG: air bone gap) to determine gain for a given frequency. This “rule of thumb” carried through and was included in the National Acoustics Laboratory (NAL) prescriptive formula (Byrne and Dillon, 1986). In the most recent iteration of the NAL-NL2 formula, the equation 75% ABG + BC (BC: bone conduction) is used. These two formulae actually are algebraically equivalent expressions of hearing loss. Johnson (2013) set out to calculate the prescribed maximum power output (MPO) for a set of case examples with various conductive components to illustrate the differences in using one versus the other formula. What he found was that although the formulae are algebraically equivalent, they do not produce the same maximum output. The underlying reason rests with the use of AC thresholds in the original formula for determining compression ratio in newer nonlinear formula for nonlinear hearing aids as opposed to using the BC threshold. When faced with the need for a nonlinear prescription, the 75% ABG + BC will give a more appropriate (higher) MPO. This is the math used in the new NAL-NL2.
13. I assume you found some articles regarding verification? Let me guess, it still matters that speech signals are audible?
Yes, indeed it does. Unfortunately not everyone has the message yet so we’ll keep talking about it and producing examples that help people understand that audibility is the basic treatment for hearing loss and fitting a hearing aid requires verifying that sounds at a variety of input levels across a range of frequencies have been made audible.
14. So what are the examples this year?
Well, let’s go back to frequency lowering first. One of the issues we see in the various publications thus far is inconsistency in how the frequency shifting is set and verified. McCreery, Brennan, Hoover, Kopun, Stelmachowicz (2013) provided a method for optimizing audibility for non-linear frequency lowering; in their study the lowering scheme was non-linear frequency compression (NLFC). They compared performance across a set of simulated hearing losses (three degrees of high frequency hearing loss) in a group of listeners. The input signal was: not processed (conventional); processed using the default nonlinear frequency compression settings based on the hearing loss; or using the optimized NLFC settings that they suggested in their article. Hint: the optimized settings are more aggressive and make more high frequency sound audible in the lower frequency range.
In terms of objective performance, the optimized NLFC outperformed the default and non-processed setting (no difference between the latter two). This clearly points out that audiologists will want to verify the real-ear audibility that is obtained when engaging frequency lowering rather than depending on default settings. This of course is just another reason why probe-microphone measures are essential, and can be your best friend (see Mueller, 2014, Mueller, Alexander and Scollie, 2013).
Speaking of needing to verify, we also reviewed a study by Magnusson, Claesson, and Persson (2013), which examined the benefit of directional technology in open canal (OC) fittings. My interpretation of their findings is: If you don’t program the hearing aids so that you have audibility based on evidence-based targets, you will find that OC hearing aids with omnidirectional microphones don’t provide better performance than the unaided condition. And you also will find that directional microphones don’t help when the signal is not audible in an OC fitting (or any other fitting for that matter).
The authors set out to compare unaided, omnidirectional microphones, and directional microphones in either an open or closed fitting by testing speech recognition in noise for 20 hearing-impaired adults with no hearing aid experience. In the methods section you see, “The hearing aids were programmed based on the audiometric configuration of each subject and the fitting approach (open or closed) using a first fit with Phonak adaptive formula.” We know from our review in 2013 that that hearing aids that are producing appropriately audible signals (matching output to evidence based real ear targets) produces superior performance as compared to the manufacturer’s first fit—about an 8 dB improvement on the QuickSIN (Leavitt and Flexer, 2012). We also know that a validated fitting (compared to a manufacturer’s fit) provides more benefit, and is preferred by the majority of hearing aid users (Abrams, Chisolm, McManus, McArdle, 2012). In addition, Aazh, Moore, and Prasher (2012) reported that target gain and output can be met with open fittings, although about 70% are underfit by 10 dB or more using the manufacturer’s fitting. So, one can expect poor results, sometimes no better than the unaided condition, when audibility is not achieved. Making sounds audible and comfortable with as little distortion as possible is the goal of a hearing aid fitting. Simply stated, this article had a good teaching point, but perhaps not the one intended by the authors.
15. I know you’ve been working on the new, updated pediatric amplification guidelines. Were they finally published?
Yes, they were finally finished and published last year. As you may know, for the last 12 years I’ve been showing pictures of my sons at the Academy meeting when I present the articles for the pediatric section. I was a little concerned that by the time we finally finished the guidelines, neither would still be children. They are now 18 and 16, and I did again show their pictures—this time it was to make the point that the next Pediatric Amplification Guideline (yes, it’s already time to start) will attempt to produce recommendations for separate age ranges. As I look at my two boys, they are more similar to adults than children in many ways, yet there are still issues related to educational settings to consider. So, the reader will find the new guidelines completely evidence based which is a great change, but clinicians will continue to have to extrapolate data from different age ranges to apply to any given pediatric hearing aid user.
16. If we are focusing on audiology and pediatrics, I suppose I should ask what research Ryan McCreery has been up to? I recall that you’ve included his work before.
You’re right, we often do. We include Ryan’s work because he asks important clinical questions and creates experimental designs that allow the clinician to use this information right away. We didn’t see Ryan at the Academy meeting this year because he was home with his wife producing a pediatric person – welcome to their new baby girl! Ryan is part of the large scale study called the Outcomes for Children with Hearing Loss (OCHL) and he was the senior author of a paper from these data that I think is important. McCreery, Bentler, and Roush (2013) reported the RMS error of the output of actual hearing aid fittings compared to the DSL 5.0 targets for 195 children with mild to severe hearing loss aged 5 to 85 months (7 years). In addition, they quantified the audibility achieved in the fittings using the Speech Intelligibility Index (SII) calculation. Fifty-five fittings (28%) had at least one ear that deviated from prescriptive targets by more than 5 dB RMS on average. One major, but not surprising, finding was that fittings based on average real ear to coupler difference (RECD) resulted in larger deviations from prescriptive target than fittings based on individually measured RECDs. And secondly, aided audibility was predicted by the proximity to the prescriptive target. So, better to meet target if your goal is audibility (which it is) and easier to meet target if you use measured RECDs to individualize the fitting to the patient’s ear canal characteristics.
17. Anything else in the world of pediatrics?
Yes, another big data study is coming from Australia and the authors reported some of their results in a special edition of the International Journal of Audiology (IJA): Longitudinal Outcomes of Children with Hearing Impairment (LOCHI). In an article from this edition, Ching and Dillon (2013) saw a unique opportunity to look at outcomes across a very large group of three-year-olds at a time when some of these children would have been in geographical areas with newborn screening and some would not. So the time of identification and intervention might vary, but the fitting protocols would be consistent because of the way audiologic services are delivered in Australia. This allowed the investigators to examine factors other than the hearing aid fitting and audiologic services that might be predictive of success for these children (N=451). They included a large test battery to evaluate various skills that require auditory input to develop. I want to highlight their findings related to predictor variables for global language outcomes. The factors that were revealed to be predictive of global language outcomes include: severity of hearing loss, gender (this is a consistent finding with normal hearing children as well), presence of additional disabilities, maternal education (this is consistent with normal hearing children). For children with cochlear implants, global language outcomes were related to age at cochlear implantation with a .5 standard deviation reduction in global language score from 12 to 24 months. Although none of these findings are surprising it is exciting to start to obtain larger data sets to help us predict outcomes and understand mediating factors in hearing and cochlear implant success. You’ll be interested in all 8 papers that were included with this one in the special edition of IJA.
18. I’ll look into it for sure. We’re winding down, so we probably should talk about hearing aid validation and real-world outcomes?
Good idea. One could argue that nothing but real-world outcomes matter to the patient and therefore the clinician, too. Unfortunately, one real-world outcome that we experience is patients who purchase hearing aids, but do not wear them. Non-use is not good for the patient or the profession. Linseen and colleagues (2013) examined the beliefs and feelings of eleven hearing aid owners who reported that they never or hardly ever used their hearing aids. The final conclusion was that individuals who had purchased hearing aids but did not use them have different feelings and beliefs that have led them to non-use. The authors present three themes that may describe the feelings of these individuals: those who simply do not think they are having difficulty, those who acknowledge having difficulty in at least some situations and reveal self-annoyance about not using the hearing aids, and those who feel angry and frustrated with their own non-use. These three themes of feelings are further mitigated by how significant others feel about their non-use. Although this study only included a very small number of subjects, the authors conclude that patient-centered care where the patient is a full participant from the beginning of a hearing evaluation and discussion of communication solutions may help prevent individuals from owning hearing aids they don’t use.
19. There seem to be a lot factors that can influence the outcome of hearing aid fittings.
Very true, and an area that is indirectly related to hearing aid outcomes is listening effort. An article on that topic that I liked was written by Ben Hornsby (2013). He has been looking at listening effort related to hearing aids for the past few years, and in his study from 2013 he was trying to quantify the impact of hearing aid use and advanced signal processing on measures of listening effort and auditory mental fatigue. Sixteen adults (47-69 years of age) with mild to severe sloping sensorineural hearing loss were fitted with hearing aids and used them in the real world for two weeks prior to being tested. In real-world use, participants were exposed to the basic condition, which included omnidirectional microphone settings, and the advanced condition, which included directional microphone technology with digital noise reduction. Interestingly, although these are the conditions the individual would have been listening to in the real world, the test condition purposely did not activate the directional microphone signal processing. The author hypothesized that there would be carry over from the real-world experience in terms of effort and fatigue. Individuals were tested at the end of the day in each session and each test session took one hour. The testing consisted of a dual-task paradigm that included word recognition (conducted at SNR producing ~70%), word recall (hold the last 5 words in memory), and visual reaction time (RTs; while listening, look for a visual signal on a screen and push a button). Subjective descriptions of listening effort were collected before and after each one hour test session. The findings indicated that:
- Word recall was better and RTs were faster in aided compared to unaided condition
- Word recognition and recall were resistant to mental fatigue
- Subjective and objective measures of listening effort and fatigue were not correlated
- Age and degree of hearing loss were not predictive
- RTs systematically increased over the duration of the speech task when listening unaided
- RTs remained stable over time in both aided conditions
20. So, considering all of the studies you reviewed, what can clinicians do with this information on Monday morning?
I think everyone who attends our Academy session is really just waiting for the last few slides where we list our suggestions of what to do on Monday morning based on our review of the literature from the past year. So, I’ll do the same thing relative to the articles that we discussed here.
- If you want your patients to be happy with a bilateral fitting, start them out that way.
- Two ears are better than one for telephone communication.
- New signal processing technologies help communication in cars compared to previous use of omnidirectional microphones and conventional adaptive directional microphones.
- The best thing you can do for your patient is improve SNR whether they are on the telephone or trying to listen in a noisy restaurant.
- Absolute benefit from amplification is mediated by characteristics of the individual – focus on relative benefits.
- When evaluating the “goodness” of different products and signal processing strategies, consider all the experimental variability that could have led to the conclusions.
- Trainable hearing aids need to be set to evidence based targets prior to individuals using training to fine-tune the fitting. In most cases, this will lead to an audible fitting with greater patient satisfaction because of the role of the patient in the fine-tuning.
- Know the prescriptive formula you are using for conductive loss.
- To benefit from any signal processing, the amplified signal has to be appropriately audible (on the other hand, distorted signal processing will not bother listeners if it is inaudible).
- Measure individual RECDs in order to have a better match to evidence based targets.
- The audiologist using the data to fit the hearing aid matters (simply doing “real ear” isn’t enough – you have to use the data and fit to evidence-based targets).
- Hearing aid non-users may have unique feelings about their non-use. Focus on the individual’s beliefs and feelings.
- Well fit amplification (regardless of advanced signal processing) reduces effortful listening and mental fatigue – it is reasonable to talk to patients about this benefit.
Acknowledgments
Needless to say, the presentation at the American Academy of Audiology conference each year wouldn’t happen without the dedication of Bob Turner and Gus Mueller, and I’ve used some of their contributions in this article. Each year the students in my lab work at gathering the articles. Special thanks go out to Dr. Jenifer Fruit who organized all of the articles for us this year. I’d also like to thank all the conference attendees who fill the room for this session every year and make it a pleasure to put together this talk.
References
Aazh, H., Moore, B., & Prasher, D. (2012). The accuracy of matching target insertion gains with open-fit hearing aids. American Journal of Audiology, 21, 175-180.
Abrams, H., Chisolm, T., McManus, M., & McArdle, R. (2012). Initial-fit approach versus verified prescription: comparing self-perceived hearing aid benefit. Journal of the American Academy of Audiology, 23(10), 768-778.
American Academy of Audiology (2013). Pediatric Amplification Guidelines. Available from www.audiology.org
Byrne, D., & Dillon, H. (1986). The National Acoustics Laboratory (NAL) new procedure for selecting the gain and frequency response of a hearing aid. Ear and Hearing, 7(4), 257-265.
Cox, R., Schwartz, K., Noe, C., & Alexander, G. (2011). Preference for one or two hearing aids among adult patients. Ear and Hearing, 32(2), 181-197.
Ching, T., & Dillon, H. (2013). Major findings of the LOCHI study on children at 3 years of age and implications for audiological management. International Journal of Audiology, 52(S2), 65-68.
Dawes, P., Hopkins, R., & Munro, K. J.(2013). Placebo effects in hearing-aid trials are reliable. International Journal of Audiology, 52(7), 472-477.
Hornsby, B. (2013). The effects of hearing aid use on listening effort and mental fatigue associated with sustained speech processing demands. Ear and Hearing, 34(5), 523-534.
Johnson, E. (2013). Prescriptive amplification recommendations for hearing losses with a conductive component and their impact on the required maximum power output: An update with accompanying clinical explanation. Journal of the American Academy of Audiology, 24(6), 452-460.
Keidser, G, & Alamudi, K. (2013). Real-life efficacy and reliability of training a hearing aid. Ear and Hearing, 34(5), 619-629.
Lavie, L., Banai, K., Attais, J., & Karni, A. (2013). Better together: reduced compliance after sequential vs simultaneous bilateral hearing aid fitting. American Journal of Audiology, 23, 93-98.
Leavitt, R., & Flexer,C. (2012). The importance of audibility in successful amplification of hearing loss. Hearing Review, December.
Linseen, A.M., Joore, M.A., Minten, R.K., van Leeuwen, Y.D., & Anteunis, L.J. (2013). Qualitative interviews on the beliefs and feelings of adults towards their ownership, but non-use of hearing aids. International Journal of Audiology, 52(10), 670-677.
Lybarger, S. (1963). Simplified fitting system for hearing aids. Canton, PA: Radioear.
Magnusson, L., Claesson, A., Persson, M., & Tengstrand, T. (2013). Speech recognition in noise using bilateral open-fit hearing aids: The limited benefit of directional microphones and noise reduction. International Journal of Audiology, 52(1), 29-36.
McArdle, R., Killion, M., Mennite, M., & Chisolm, T. (2012). Are two ears not better than one? Journal of the American Academy of Audiology, 23, 171-181.
McCreery, R., Bentler, R., & Roush, P. (2013). Characteristics of hearing aid fittings in infants and young children. Ear and Hearing, 34(6), 701-710.
McCreery, R., Brennan, M., Hoover, B., Kopun, J., & Stelmachowicz, P. (2013). Maximizing audibility and speech recognition with nonlinear frequency compression by estimating audible bandwidth. Ear and Hearing, 34(2), 24-27.
Mueller, H.G. (2014, January). 20Q: Real-ear probe-microphone measures - 30 years of progress? AudiologyOnline, Article 12410. Retrieved from: https://www.audiologyonline.com
Mueller, H.G., Alexander, J.M., & Scollie, S. (2013, June). 20Q: Frequency lowering - the whole shebang. AudiologyOnline, Article 11913. Retrieved from https://www.audiologyonline.com/
Nabalek, A., Freyaldenhoven, M., Tampas, J., Burchfield, S., & Muenchen, R. (2006). Acceptable noise level as predictor of hearing aid use. Journal of the American Academy of Audiology, 17(9), 626-639.
Ng, E.,Rudner, M., Lunner, T., Pedersen, M., & Ronnberg, J. (2013). Effects of noise and working memory capacity on memory processing of speech for hearing aid users. International Journal of Audiology, 52, 433-441.
Picou, E., & Ricketts, T. (2013). Efficacy of hearing-aid based telephone strategies for listeners with moderate-to-severe hearing loss. Journal of the American Academy of Audiology, 24(1), 59-70.
Walden,T., & Walden, B.(2005). Unilateral versus bilateral amplification for adults with impaired hearing. Journal of the American Academy of Audiology, 16, 574-584.
Wu, Y-H., & Stangl, E. (2013). The effect of hearing aid signal-processing schemes on acceptable noise levels: Perception and prediction. Ear and Hearing, 34(3), 333-341.
Wu, Y. H., Stangl, E., & Bentler, R. A. (2013). Hearing-aid users' voices: A factor that could affect directional benefit. International Journal of Audiology, 52(11), 789-794.
Wu,Y-H., Stangl, E., Bentler, R., & Stanzioloa, R. (2013). The effect of hearing aid technologies on listening in an automobile. Journal of the American Academy of Audiology, 24(6), 474-485.
Cite this content as:
Palmer, C. (2014, May). 20Q: A review of 2013 hearing aid research—tips for the clinician. AudiologyOnline, Article 12672. Retrieved from: https://www.audiologyonline.com


