Learning Outcomes
After this course learners will be able to:
- Describe the components of Signia TeleCare.
- Describe the conceptual model of user engagement with technology.
- Describe the relationship between the use of Signia TeleCare and acceptance of hearing instrument technology.
Introduction
Options to offer services and solutions based on electronic processes and communication have in recent years been increasingly explored within the entire healthcare industry. Depending on the specific processes and technologies involved, such solutions are often referred to using umbrella terms like eHealth, mHealth, connected health, telemedicine or telehealth, but more field-specific terms have also been introduced. Within the field of audiology, the term teleaudiology has often been used (Gladden, 2018). While teleaudiology covers different types of solutions and use cases, a key element is always the use of the internet and/or mobile phones (or other types of wireless communication) to establish a connection between caregiver and patient.
One key incentive for researching and developing telehealth has been to offer cost-effective solutions that address the needs of patients living at a long distance from their caregiver, e.g., a Hearing Care Professional (HCP) in the case of hearing aid related teleaudiology solutions. Many of these benefits have been unfolded in Signia TeleCare, which offers a wide range of features that not only allow for hearing-care treatment over a distance but also includes features that provide convenience and strengthen the hearing aid fitting process compared to the more traditional fitting approach.
Signia TeleCare
Signia TeleCare directly addresses one of the most essential parts of the fitting process: The time period between the initial fitting and the first follow-up visit where the hearing aid wearers often are left on their own and where the communication with the HCP usually is minimal. The TeleCare features include options for the wearer and the HCP to communicate real-time using text, audio and video calls, the ability for the wearers to rate their listening experience each day (allowing the HCP to react if low ratings occur), a series of interactive hearing lessons that guide the wearers in specific situations and collect feedback for the HCP, and if required, the ability to perform remote fine-tuning of the hearing aids. The app usage flow of the Hearing Lessons feature is shown in Figure 1, as an example of how TeleCare at the same time is able to guide and set the expectations of the wearer, assess the fitting and provide the HCP with valuable information.
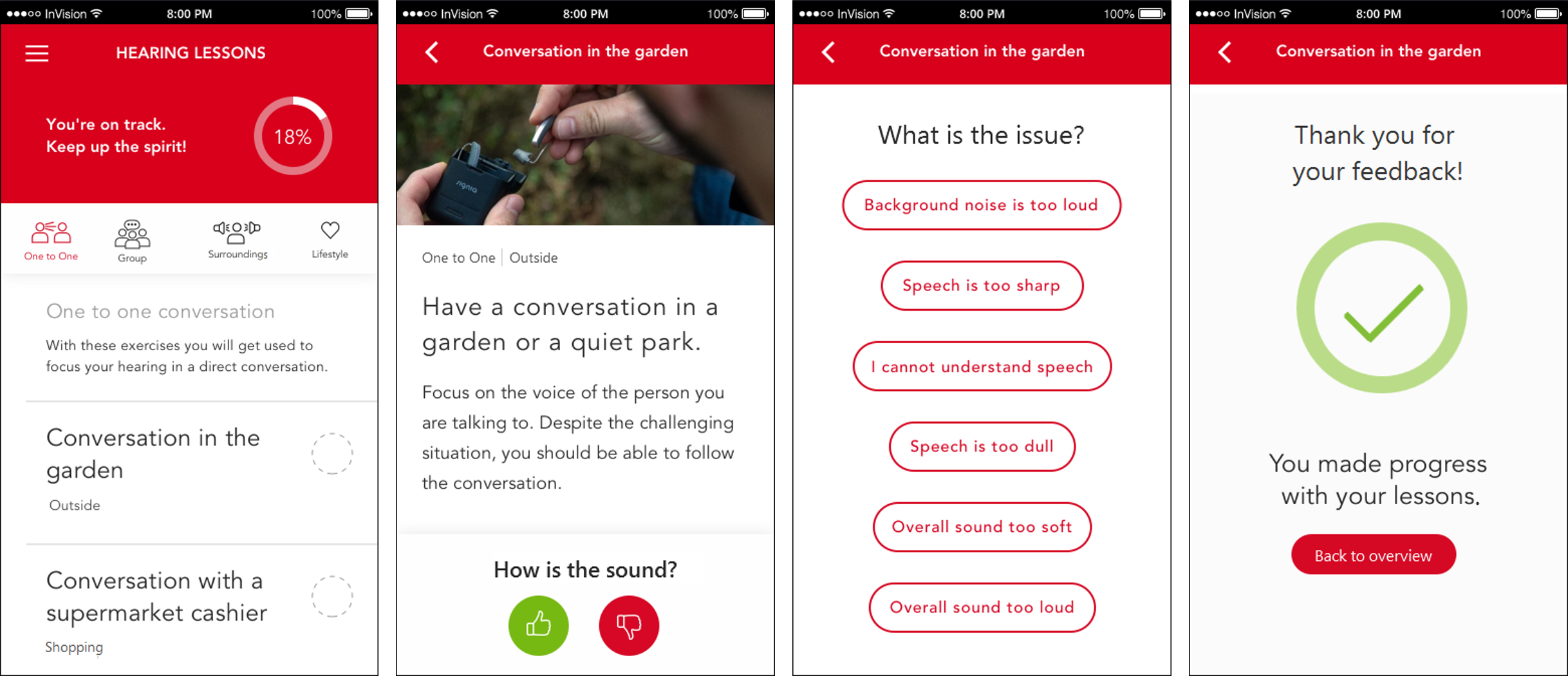
Figure 1. App user interface of the Hearing Lessons feature in Signia TeleCare. Lessons are available for different specific listening situations determined by the HCP (either by picking from a list or by choosing a suggested set of situations). When a situation is selected in the app, the wearer gets a listening task, receives information about what to expect from the hearing aids and is asked to state a preference for the sound. In case of dislike, the wearer is asked to state a reason, which will be sent to the HCP.
Previous research with Signia TeleCare has been encouraging. For example, in a study of new hearing aid wearers, findings revealed that TeleCare facilitates improvements in hearing aid fitting outcome: high levels of ability and satisfaction for the user’s nominated listening situations, and findings on the IOI-HA substantially higher than normative values (Froehlich et al., 2018). In subsequent research, Signia TeleCare was found to be beneficial for new hearing aid wearers with mild dementia and their caregivers. These new hearing aid wearers reported high levels of satisfaction, and the caregivers reported less stress involving the care of the hearing aids (Jorgensen et al., 2019a,b).
In this paper, we report on an investigation regarding the relationship between the level of TeleCare user engagement, measured by the number of interactions with some of the key features during the first weeks of hearing aid use, and the subsequent decision made by the wearer on whether to keep the hearing aids following their initial purchase decision. The hypothesis was that wearers’ use of the TeleCare features reflects user engagement and a feeling of ownership of their own fitting, which will lead to an increased likelihood that the wearers decide to keep the hearing aids. The data we’ll present were gathered during use of TeleCare in routine hearing aid fittings of a large sample of wearers conducted by a multitude of HCPs around the world.
User Engagement
Based on a comprehensive literature study, O’Brien & Toms (2008) proposed a conceptual model to explain user engagement with technology. Even though the model was created based on observations of user engagement with other types of technology and was not specifically focusing on use of hearing aids, it may be applied to explain the engagement processes involved when a person with hearing loss is being fitted for the first time. The model operates with four overall stages of engagement:
- Point of engagement
- Engagement
- Disengagement
- Re-engagement
For each stage, there will be several different attributes that determine whether the user stays at a given stage or moves on to the next. For example, in the Engagement stage, attributes like awareness, interactivity, and feedback (from the technology) determine whether the user remains engaged or becomes disengaged.
In the context of a hearing aid fitting, the four stages could be translated to different points or periods of time in the fitting process. In principle, the point of engagement could happen even before the potential hearing aid wearer steps into the HCP office, but if it has not happened before, it should happen during the first visit as part of the interaction between the wearer, the HCP and the hearing solution being offered.
A plausible assumption would be that an engaged wearer is much more likely to accept and keep the hearing aids than a disengaged wearer. Disengagement, whatever the cause may be, is certainly not a facilitator for the process of adjusting to new hearing aids, which is an inevitable part of any fitting. Assuming that the wearer is engaged when leaving the HCP’s office after the initial fitting, the challenge is, therefore, to keep the wearer engaged–to remain at Stage 2 without entering Stage 3 (disengagement)–and, if the wearer actually enters Stage 3, to move the wearer into Stage 4 (re-engagement) as quickly as possible. It is exactly this challenge that Signia TeleCare addresses. It includes tools that can be used during the first few weeks following the fitting to keep the wearer engaged, tools that can help to identify wearers who show signs of disengagement, and tools that can help re-engaging wearers who have become disengaged.
Analysis of TeleCare Data
An analysis study was designed to examine data on the use of Signia TeleCare that had been gathered during routine hearing aid fittings. These real-life data provide detailed knowledge about how TeleCare was used in the period after the initial fitting. By connecting the usage data to each participant’s decision on whether to keep the hearing aids, it is possible to obtain insights into how the engagement of the wearer offered by TeleCare relates to hearing aid acceptance.
The data presented in this paper originate from the use of TeleCare in a sample of 22,810 participants around the world. They came from 36 different countries, with the United States providing the largest group with 4,501 participants. The participants were only retrospectively included in this data analysis and were not part of a research project per se. That is, they simply were individuals seeking help for their hearing loss through the use of amplification. All participants were registered as users of TeleCare during the initial fitting. This means that they had installed the Signia App (or the myHearing App) on their smartphones and that the connection to their HCP had been established. The participants were fitted with a variety of hearing aid types.
Not surprisingly, the use of TeleCare varied considerably across the participants. In one extreme, a subset of 2,199 participants (corresponding to 9.6% of the sample) did not interact with the TeleCare features at all during the weeks following the fitting, even though they had the opportunity. There may be various reasons for this lack of use. One reason could be that these wearers were quite happy with the fitting of their hearing aids and therefore did not feel the need for the additional help offered by TeleCare. Adjustment to hearing aids is a very individual process, and for those wearers who accept their new hearing aids very quickly, sometimes almost in the moment they are switched on, the urge to explore the TeleCare options may be limited. In such cases, the lack of use may not reflect lack of user engagement but rather a successful first fit and good initial counseling.
This explanation is to some extent supported by the fact that around three out of four participants (76%) in this subset decided to keep their Signia hearing aids without using TeleCare. This is in line with previously reported numbers on return rates (Várallyay & Herbig, 2016). The remaining 24% of the subset, however, did not keep their hearing aids. For these individuals, it could be speculated that the decision to return the hearing aids was caused by lack of user engagement or by issues related to the specific fitting of the hearing aids. In both cases, using one or more of the TeleCare options could potentially have changed the decision. We will investigate this potential by exploring the data on the 20,611 participants who did use one or more of the TeleCare features after the initial fitting.
Results
We examined each TeleCare feature separately, but in all cases, we used the 76% acceptance rate for the TeleCare non-user group as a baseline, to which the acceptance rates for different subgroups of TeleCare users were compared. For each feature, we divided the participants into three subgroups depending on how many times they interacted with the corresponding feature between the initial fitting and the first follow-up visit: 1-2, 3-5, or more than 5 times. The number of participants in a subgroup varied across both groups and features.
First, we examined the number of lessons taken using the Hearing Lessons feature, which was shown in Figure 1. This feature allows the HCP to set up a range of specific real-life situations for the wearer to explore (or a set of default situations can be chosen). The app provides information about the situation and what to expect from the hearing aids. The wearer is asked to evaluate the situation, and the evaluation is sent automatically to the HCP who thereby will be able to react if a problem is indicated. Panel A in Figure 2 shows the acceptance rates for subgroups with different numbers of lessons taken, plotted together with the baseline (no TeleCare use). The plot shows that higher acceptance rates are observed for more lessons taken. However, the number of interactions needs to exceed five before the increase in acceptance rate becomes substantial. Since following a lesson may be seen as an educational activity, which does not directly affect the auditory listening experience (unless the HCP intervenes), it seems plausible that it takes some lessons before an impact on user engagement–and thereby on the wearer’s wish to keep using the hearing aids–can be observed.
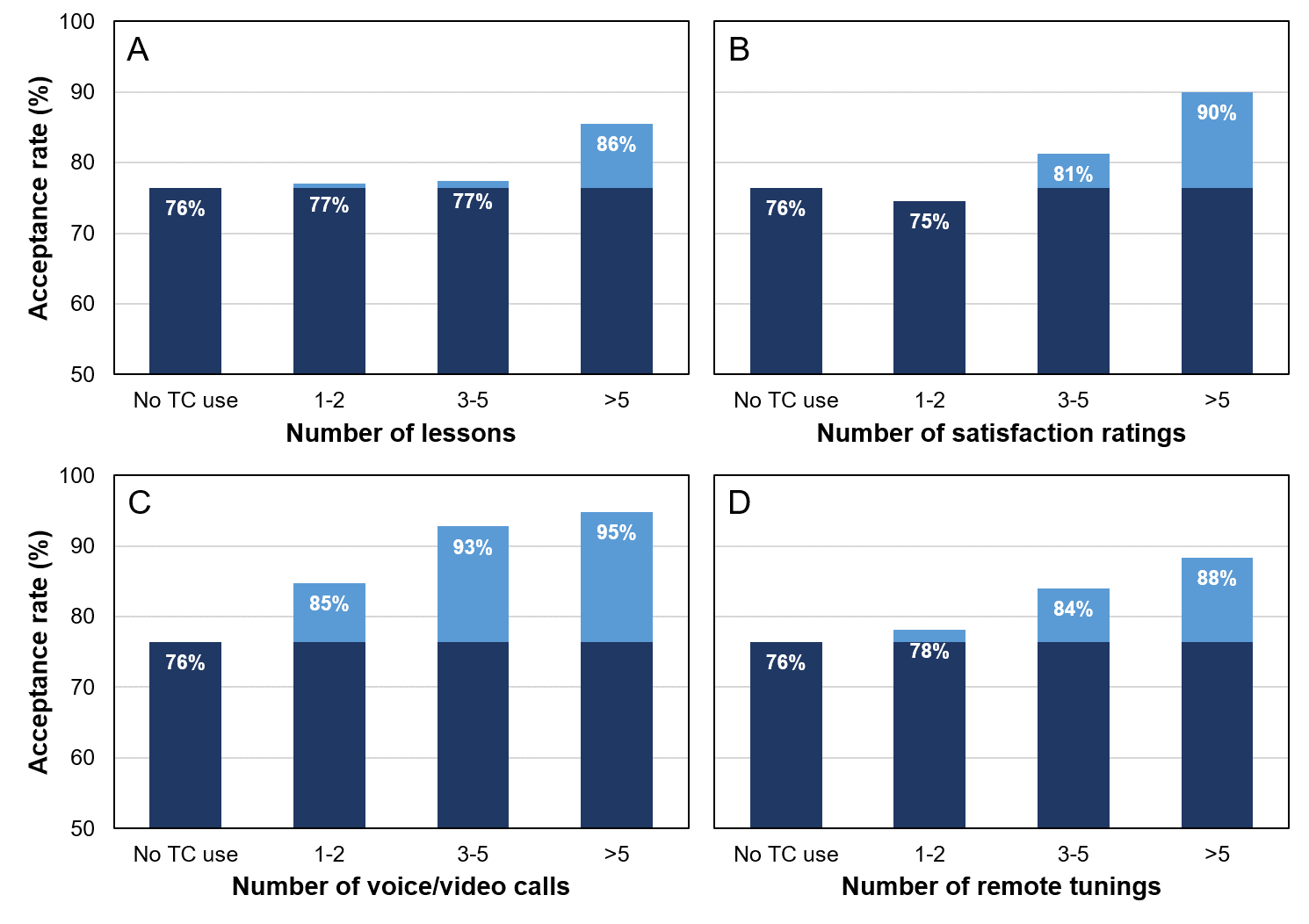
Figure 2. Acceptance rates observed for different levels of interaction with four TeleCare features: A) Hearing Lessons, B) Daily Ratings, C) CareChat, and D) Remote Tuning. The baseline acceptance rate of 76% (“No TC use”) is indicated in each plot. In each panel, the increase in acceptance rate relative to the baseline is indicated with a lighter shade.
Next, we analyzed the data on the Daily Ratings feature that prompts the wearers to make daily ratings of their satisfaction with the hearing aids. The ratings are available to the HCP who receives an automatic notification if the ratings indicate that the wearer is not satisfied. Panel B in Figure 2 shows the changes in acceptance rate for different number of satisfaction ratings made. As in panel A, the trend is that the acceptance rate increases with the number of interactions. In this case, a slight decrease in acceptance rate is observed for the group who only provided 1-2 satisfaction ratings. Even though the decrease is small (1 percentage point) and may–at least partly–be ascribed to statistical uncertainty, it could indicate that making just a few satisfaction ratings does not reflect sustained user engagement. If the first few ratings have been low–and the HCP has not reacted on them – the wearer may have reached the stage of disengagement and have given up the use of not only TeleCare but also the hearing aids. When more satisfaction ratings are provided, we observe substantial increases in the acceptance rate, which reach an average of 90% for the group of participants with more than 5 ratings.
We also examined the use of the CareChat feature that enables real-time communication between wearer and HCP using voice or video calls. This allows wearers to explain their situation-specific listening experiences and challenges either while being in the actual situation or within a few days, giving the HCP a much better change to address critical issues, via counseling or fine-tuning, than what is possible when trying to solve the same issues at a later time in a clinical setting. Panel C in Figure 2 shows the acceptance rates observed for different numbers of CareChat interactions (voice/video calls) made between the initial fitting and the follow-up visit. Again, we see a correlation between number of interactions and acceptance rate, but for the use of CareChat, a more substantial increase in acceptance is observed for the group with just a few (1-2) interactions. Higher acceptance rates are also observed for the other levels of interaction. For the group who completed more than five interactions, the acceptance rate reached an impressive level of 95%, but it should also be noted that an acceptance rate of 93% was observed for the subgroup with 3-5 interactions. The fact that the highest overall acceptance rates are observed for the users of the CareChat feature is not surprising and just underlines the importance of the direct HCP-wearer interaction in the journey towards a successful fitting.
Finally, we examined the number of fine-tuning sessions completed using the Remote Tuning feature. The option to make remote adjustments allowed for a faster reaction when a need for a changed hearing aid setting was expressed, as compared to setting up an extra appointment or waiting for the scheduled follow-up visit. The acceptance rates for different numbers of fine-tuning sessions are plotted in panel D in Figure 2. The data show a rather clear trend towards higher acceptance rates for higher number of fine tunings. While the increase in acceptance rate is rather limited (2 percentage points) for 1-2 fine-tuning sessions, it becomes more substantial for the subgroups who had completed at least 3 sessions. This suggests that cases where wearers need multiple fine-tunings to accept their new hearing aids–often resulting in some wearers giving up and returning the hearing aids if they have to go back to the clinic each time–may be addressed more effectively with TeleCare where fine-tunings are faster and more convenient to complete for both HCP and wearer.
These Remote Tuning data do not include information about the number, type, and magnitude of the adjustments made during the sessions. Thus, the data do not differentiate between cases where a session consisted of one minor adjustment and cases where more substantial adjustments were made. However, even small adjustments may make a difference on the wearer’s experience of the hearing aids and thereby have a significant impact on the user engagement. It seems reasonable to assume that performing more fine-tuning sessions will increase the likelihood of successfully addressing an issue that, if left unaddressed, could lead to limited satisfaction and engagement, and eventually result in a decision to return the hearing aids. Moreover, the simple act of making these changes remotely creates confidence in the skills and professionalism of the HCP, which indirectly relates to hearing aid acceptance.
Discussion
The data showed a general correlation between the number of TeleCare interactions and the hearing aid acceptance rate. This trend was observed for all four TeleCare features included in the data analysis. Since the analysis only looked at the use of each feature in isolation, the results do not provide information about possible underlying interactions between features and interactions with other variables that could affect the decision to keep the hearing aids. Thus, based on these data alone, it is not possible to state that one TeleCare feature is more important than the other. However, with the highest acceptance rates observed in the analysis of the CareChat data, it seems reasonable to conclude that this type of support of the direct HCP-wearer communication is an important and useful element of TeleCare.
With data collected from many countries and reflecting a multitude of fitting approaches, there is a variety of sources that can affect and introduce variance in the data. The underlying data do for example reveal different average acceptance rates for different countries. However, the overall trend is the same across countries: The more use of the TeleCare features, the higher the likelihood that hearing aid wearers keep their hearing aids.
All in all, the data presented support the assumption that use of the Signia TeleCare features has a positive impact on the user engagement, as reflected in the increase in acceptance rate compared to the group of participants who did not use the features. The TeleCare features provide various tools to positively affect attributes like interactivity and feedback that engage hearing aid wearers in their own hearing aid fitting, as suggested by the model of user engagement discussed earlier. Furthermore, the TeleCare features allow for early interaction by the HCP in case a wearer moves from being engaged to being disengaged. Avoiding the disengagement stage is key in optimizing the likelihood for a successful fitting where the wearer decides to keep the hearing aids.
Summary
The data presented in this paper show a correlation between TeleCare usage and hearing aid acceptance rate. This indicates that the hearing aid wearers who use TeleCare immediately following the initial fitting are more likely to keep the hearing aids than the wearers who do not use TeleCare (but have the option to do so). While the general trend of ‘the more TeleCare use, the higher the acceptance rate’ was observed for all the examined TeleCare features, the most substantial increase in acceptance rate was observed for use of the CareChat feature. This finding highlights the importance of the direct interaction between HCP and wearer, and it shows how this interaction is facilitated by TeleCare. All in all, the data suggest that TeleCare offers features that positively affect user engagement and thereby increases the likelihood that the wearer accepts the hearing aids.
References
Froehlich, M., Branda, E., Apel, D. (2018). Signia Telecare facilitates improvements in hearing aid fitting outcome. AudiologyOnline, Article 24096. Retrieved from www.audiologyonline.com.
Gladden, C. (2018). Teleaudiology – The future is now. AudiologyOnline, Article 22121. Retrieved from www.audiologyonline.com.
Jorgensen, L., Van Gerpen, T., Powers, T.A., Apel, D. (2019a). Benefit of Using Telecare for Dementia Patients with Hearing Loss and Their Caregivers. Hearing Review, 26(6), 22-25.
Jorgensen, L., Van Gerpen, T., Powers, T.A., Richter, L. (2019b). Implementation of TeleCare for New Hearing Aid Users with Mild Dementia. AudiologyOnline, Article 25795. Retrieved from www.audiologyonline.com.
O'Brien, H.L., Toms, E.G. (2008). What is user engagement? A conceptual framework for defining user engagement with technology. Journal of the American Society for Information Science and Technology, 59(6). 938 - 955. doi: 10.1002/asi.20801.
Várallyay, G., Herbig, R. (2016). Signia TeleCare – the Future of Hearing Care Starts Now. Signia White Paper. Retrieved from https://www.signia-library.com/scientific_marketing/signia-telecare-the-future-of-hearing-care-starts-now/.
Citation
Froehlich, M., Branda, E. & Apel, D. (2020). User engagement with Signia TeleCare: A way to facilitate hearing aid acceptance. AudiologyOnline, Article 26463. Retrieved from https://www.audiologyonline.com