Editor's note: This text-based course is an edited transcript of the webinar, Third-Year AuD Clinical Externships: Strategies, Struggles, and Successes, presented by Shannon Van Hyfte, AuD, CCC-A.
Learning Outcomes
After this course, learners will be able to:
- Describe the process of placing a student in a third-year externship.
- Identify the process for one model of establishing an externship database.
- Describe methods for supporting student and site preparedness for externship placement.
Introduction
This is a topic that is near and dear to me, and I hope I'll be able to offer some strategies for those of you in the trenches, share some struggles, and provide some information that can enable more success for all of us. The program and model that I'll be presenting is the one that I use in my own program. I am going to talk a little bit more about how I got into this role, go through some terminology, review some requirement updates related to supervision and clinical education, then talk about the process and strategies that I use to help enable success. We all have struggles, so I'm going to acknowledge those and talk about how I've walked through some of those, and share some successes. Then I'll answer the question of why you might want to even go down this road of supervising someone in their externship, being a clinical educator, or consider being a host site. We will wrap up by talking about future directions.
Why this topic and why me? I would argue that this is a topic that matters to all of us in our profession. It matters because we need to have students who will be the future, providing meaningful experiences to other patients. We're the ones as current practicing audiologists who can enable that and make a stronger student. By providing meaningful experiences in your own settings and being engaged clinical educators, we're strengthening our future and all of our students. We're providing service to the profession as well as to these students by engaging in this externship experience. Why am I the one talking about it? I've been doing this for about 10 years. In our Purdue program, we have three semester-long experiences that occur in the third year of the AuD program. The first two years students have semester-long clinical placements in our on-campus clinic, which is a pretty busy clinic, but it's a different kind of setting than can be offered at a private practice, ENT, or other clinics. We have an average of around 10 third-year students in our cohort. I arranged for them to have a placement in the summer, fall, and spring of their third year.
Who should be here? I think many people could benefit from this course including university externship coordinators, past or current clinical educators, and those considering becoming clinical educators. I have fallen into a couple of those roles myself. I have been an offsite clinical educator supervisor, and I now am in the role of being the externship coordinator.
Terminology and Procedural Updates
We're going to go through some terminology and some procedural updates that have happened recently. I'm going to talk about the externship coordinator as the person that I am in my current role. This is the person at the university who's reaching out and coordinating the placements. The terms clinical educator, clinical instructor, externship supervisor, and clinical supervisor are all similar terms, but I feel pretty strongly about using the term clinical educator. I started this off by referring to the supervisor because it might be what people are most comfortable with regarding the terminology that's out there. I really am going to try and use the clinical educator term throughout the rest of this. I'll slip occasionally into that more comfortable term of supervisor but I really feel like, for those who are in the field and thinking about being a coordinator, it's far more than supervision, which suggests that you're overseeing or directing the work of others. Being a clinical educator is guiding and refining skills, helping to develop critical thinking, and asking questions. As a clinical educator, you are doing far more than a supervisor who, in some realms, is just watching over someone's shoulder. It could be argued but that's what that term implies. However, you're really contributing to the full education piece as a clinical educator. There is a reference at the end of this course to CAPCSD regarding the term clinical educator that helps explain why I think the term captures the crucial role that is being held in these offsite experiences.
Procedural FYI
Beginning January 1st, 2020, a couple of things changed in the realm of ASHA. I'm going to mention this because it's often a question I get from my externship clinical educators if whether or not they have their C's impacts their ability to take a student.
Universities
Effective January 1st, 2020, students applying for CCC-A no longer need to meet the required 1,820 hours of supervised experience under an audiologist holding their C's. They do have to comply with departmental standards and competency standards for knowledge and skills within ASHA. Our program did make the change to courses, knowledge, and skills, but we still hold the standard that for graduation a student needs to have 1,820 hours. If you would like to read more, the reference for this is at the end of the course. The answer to the question, when I have externship coordinators or externship clinical educators reaching out to me asking if they need to have their C's is no. I tell them that I really care about the experience they can provide. However, I do have clear communication as I share that information with our students.
Clinical Educators
The other procedural change that took place is that all CCC-A supervising audiologists need to have a minimum of nine months of experience post-certification AND two hours of professional development in the area of supervision post-certification.
The Process/Organization of Securing Placements
How does this whole process work? We use the Purdue model and it has worked well for us. To start, I begin planning a year ahead of time. That's not a misprint, it really is a year. Right now it is June of 2021. This fall, I will start working on dates for summer 2022, fall 2022, and spring 2023 placements. It starts a whole year early for a couple of reasons. Purdue is located in Indiana in a somewhat rural setting. We are one of three AuD programs in our state. All of them are vying for a limited number of sites. Thankfully, we have a lot of wonderful audiologists who step up to the plate and take students from across the state. There is a bit of jockeying going around as they figure out which student they have for which semester and if they can take another one. It simply takes time.
There are three semesters to organize so we strongly encourage our students at Purdue for their summer semester to explore and go outside of our general area which is the Lafayette, West Lafayette, or Indianapolis area. They could go across the country as long as I can make it happen. So if they want to go live with their grandma, aunt, or a college roommate and experience an audiology practice in that area, the country is their oyster to an extent. The process begins a year ahead of time and it begins with the student.
The other reason that it begins this early is that students need some time to think about this. I ask each student what their preference is for an experience or location and what it looks like for them. I also ask if they have a particular population they prefer to work with. Some of our students prefer to move to Indianapolis where we have more sites and drive back to classes. In their third year, classes are only on Thursdays and Fridays. Knowing these preferences helps me as I'm making these placements because there's some flexibility. We want the students to be at their placements two days a week and this allows them to have Monday, Tuesday, and Wednesday to play with and allows them to be able to do something else on the third day when they are not at their placement or in class.
My goal is to get students at least one of their top preferences and give them a variety of sites because they don't always know what they want even though they think they know what they want. Part of our role is to help guide them and give them some experience in different kinds of settings. I put all of this information that I gained from the students into a grid, as seen in Figure 1.

Figure 1. Grid of students and preferences for assignments.
For example, as seen in Figure 1, student A listed a preference for working with the pediatric population and moving to Indianapolis. Student B wants to gain experience with vestibular assessments, adults, and would like to see what the VA setting is like. Student C wants various experiences such as ENT and nonprofits but wants to remain local.
I'll set up a grid for the summer, the fall, the spring, and an area for notes. I have found that making this shareable with the other clinical faculty has been a wonderful resource for me. I will continue to do that in the future. I used to do this all on my own and then share it once the grid was filled out. I found that sharing it along the way is particularly useful and helpful, so I've embraced that option.
I've started a year early, reached out to the students, and gained their preferences so I know more about what they're thinking. Now begins the calls or emails to the sites that are on my database. I'm going to talk about the database and how you build it a little later. I would encourage that your call or email is true to you, which for me is lighthearted with a little dash of begging. It's often because I know the audiologists that I'm reaching out to, and I know their preference is email, so I tend to do the email. It's harder to say no to you if you call, so if you're trying to win over a new site or a new facility, I highly encourage the phone call. It tends to be more effective for me.
My email will often be something to the effect of hello, it's me again. Would you consider taking another wonderful Purdue AuD student for the fall 2022 semester? We would ideally be looking for two days a week between the days of Monday and Wednesday. The student has a particular interest in _____. If I'm reaching out to a VA it would be adults or a for a pediatric site, children and pediatrics. I have learned that you need to match the student with a high interest in pediatrics with the pediatric site. Do not make the mistake of matching a student who says they have absolutely no interest in children at a pediatric site and encouraging that placement. That's not going to go well for anyone.
My other tip is that you keep a record of every communication. While I may still be sending these out via email, I am then noting that I sent the email. I could go back in my email and look, but I like having it all in one place. I have made the mistake and miss-recorded something and it always comes back to embarrass or haunt us, so I try to avoid that now. I've done this old school with paper and pencil and just kept a file folder with me and I've updated to the digital age. I do whatever works best for that cohort, but I keep it consistent whichever way it goes.
So then what happens when you get a yes or a no? I'm going to start with what happens when you ask the placement for consideration and get a no. When that does happen, I try to find out why they were declining me because that's helpful information to understand. If it's because there's turmoil at their practice, they're just too busy and can't take a student, or because they're short on space, sometimes those things settle down and it's important for me to recognize that. I'm also good about relaying that back. The next time I ask them, I can say that I know things were really busy and ask if things have settled down or if they have considered having a student. Then what's really important is that I add that contact to my calendar a year from now when I'll ask again. Persistence pays off.
If I get a yes, aside from doing a sigh of relief, then I start the memo of agreement which is when the site agrees to the placement. It is not binding, but it is a legal document that allows us to send a student to a site. The terms of the agreement are very basic. It is informative and lets the site know that the students carry professional liability insurance. It comes from the legal representative at our university. I'm always very careful to say it does not bind them to keep the student, and so forth. It just allows us to have a working relationship. If I'm working with a hospital, usually they want us to sign their documents rather than vice versa. Our team works well with that so it's not usually much of a hiccup.
We've started with the student, gotten their preferences, and I've started making calls. As I start getting yeses I can add them to the grid for the summer, fall, and spring, to ultimately put forth to the whole clinical faculty team. Because of the high number of students, I don't personally work with every single student that comes through our program for a whole semester-long experience. I may have them in class or work with them on hearing screenings day, but I don't have that detailed information about personalities and things like that so it's really helpful to have the team of all of us come together.
I do know my placements very well. I know their preferences and the kind of students that work well. It's about making a good match. When the faculty confirms that this is going to be a good match, then I write confirmation letters of placement because the placement said yes, the faculty said yes, and everyone's in agreement. This is the first time that I introduce students to their clinical educators at the off-site clinic, via email. It's the first time the students get any contact in the process.
Figure 2 is an example of my grid that is building. Student A who wanted pediatrics and an Indianapolis setting was able to get a children's hospital in Indianapolis, then they're off to an ENT, and finally a private practice. They'll see a variety of patients that way and will have opportunities to see different kinds of practice management and different settings. The student who said they wanted to work with vestibular patients who are adults is going to work at a private practice, a balance center, and a VA. There's certainly an argument for forcing them into a little bit of pediatric experience to make sure that that's not something they want, but it should be a conversation with the student. Student C who wanted to stay local is going to get to say local and go to a nonprofit, an ENT, and then a private practice setting. Our goal is to provide students with variety in their settings while honoring some of their top preferences.
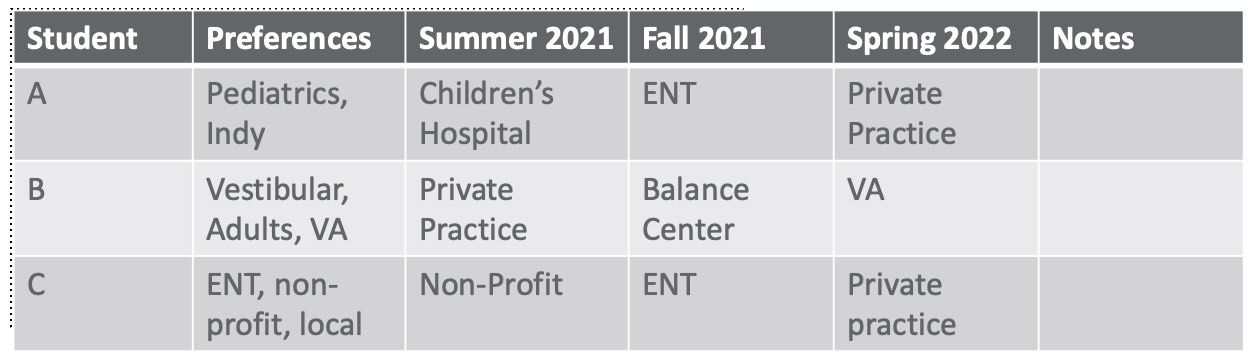
Figure 2. Expanded grid of students and preferences.
The organization of all of this is key to sanity. As referenced previously, Figure 2 is the grid for how that's building and working out. When it's my private grid, I put specific information in there regarding who my contact is at that particular site, their name, email, and phone number. At one stop, I can see exactly what kind of content information I need for each assignment. Ultimately, I also group all of my externship letters, once I've read written all of them, into a folder that I keep organized on my computer. I have this broken down by each semester, so it's all very quick to access. This also became really important during COVID. At our university, we needed to have a plan in place for what happened if you went down for an extended period of time with illness. It's been a positive thing going forward to keep everything very organized and accessible by all the clinical faculty.
In the confirmation letter that I write I thank the clinical educator for being willing to provide the placement for the student and remind them of several things. These include the dates the student will be there, the student carries their own insurance, the student's requirements of being on or off our campus or at the clinic, as well as how to record their observations, their hours, their evaluations, what hours can be counted, and so on and so forth. I also share my contact information. I'm sharing this information as a resource because I think those things can be helpful and useful especially if you're starting out with this role of finding externship placements.
Now that everyone has been introduced, the students can now contact the site. Only after I have introduced them can they reach out. We do not allow our students to contact the site beforehand. I feel that I'm in a better position of being able to explain what our students could bring, what they can offer, what they will need, and pitching that. I also think that every audiologist is so busy that no one has time to handle lots of phone calls from various students from all over the place. That is one way that we've streamlined and tried to show our professionalism to our clinical educators in the field.
As far as my follow-up with the sites at this point, I go quiet. I've appreciated that they said thank you. I've got everything that I need at that moment which is just a verbal commitment that they'll take my student. Then about a month out, I reach out to still make sure that they're on board and that they're ready. We have an online system that we use for data holding with the clinic hours and evaluation. We ensure that they have access to that system. We also make sure any other paperwork needed is in place.
Some of our hospitals' BAs have paperwork that the students need to complete and sometimes there's a part that I need to complete. Then because of COVID, I needed to gather everyone's COVID policy and make sure the students were aware of it. Our university wanted to make sure that our students were prepared, had PPE or anything else that they might need, and that they were aware of what they were going into.
Ongoing Items
As far as ongoing items, monthly reflections are something that we ask of our students. On-campus clinic students send a weekly reflection of their experiences including what they've learned. We've carried this out to our externship experiences, but instead of a weekly level have backed it off to a monthly level. We ask students to look at big takeaways such as practice management, or perhaps one patient was a big takeaway because they learned something new about diversity, patient care, or patient management.
We ask that these are no more than one page in length and that they email the clinical faculty as well as their clinical educator that is offsite. It opens up communication and has sometimes revealed that students aren't taking away what the clinical educator thought they should be taking away. It opens up a dialogue for that conversation. Sometimes it's been that more clarification is needed. Sometimes it's just good for clinical faculty to be aware of what's going on at the offsite practices so that we can be sure that going forward we're preparing students well.
As an externship coordinator, I will email the clinical educators at midterm and final to encourage them to have written as well as verbal communication with the student on their progress. The final is the only one that's absolutely required that I have, but I really encourage it at the midterm. This gives the students who are used to frequent feedback the feedback they need about where they need to continue to put forth some effort and to compliment them on areas where they've grown. Then at the very end of the semester, students complete a survey to give me feedback about that site experience. They also complete some paperwork related to accreditation. That's the process, start to finish as well as a little bit of information along the way of some of those little details of how they all come together.
Strategies for Success for the Coordinator, Clinical Educators, and for Preparing Students
I'd like to share some strategies for success for the coordinator role, for those of you in the clinical educator role or thinking about being in the clinical educator role, and how we can prepare students to be successful in this transition as well.
Coordinator
As the coordinator, I find it very critical to build the database. This takes time and patience, but it's really important for our students to have experience in various settings such as VA, ENT, private practice, balance, early intervention, hospital, non-profit, and educational. The more setting options you have to offer, the richer your students' education.
It's really important to connect with professionals in your area by attending CEU events and going to lunches. I always say yes when I'm invited to do a guest lecture or a panel discussion with a student group because inevitably they'll be reaching out to other professionals and I can meet some other people that way. I think it helps to be involved in in-person and social media groups, that are both professional and community-minded because you'll meet additional people that way and connect to those audiologists, ENTs, and others that can give you an in. Persistent, polite, and frequent asking may eventually get you in a new site. If there is a site that I continue to get a no, that's ok. It will happen. But I continue to ask and someday it may change. It only strengthens my program to keep reminding them that we're here and that we would love that experience for our students.
I think it's also important as the coordinator to work ahead and have a plan B. Inevitably when you're working a year ahead, somebody's going to leave their job. Somebody is going to have a baby or go on medical leave. Things will happen. It happens all the time. I often have everything set and a site that says, hey, if something falls through, I can take a student. I have a plan B ready to go if something falls through.
I set a calendar reminder for everything. I've mentioned it earlier, but be patient and persistent. It takes time to build your database and get into the flow of this. Choosing your pairings wisely based on academic growth and personality is really important. If I have a very energetic student, I need to find a careful match, versus a very studious quiet student. It needs to be a good blend for that particular site and setting for it to be successful. A personality match is a real struggle. I'm going to talk about that in a little bit. I also think that as the externship coordinator, I need to enable my clinical educators, who I'm partnered with, to be successful by providing them some guidance, sharing CEU resources, and sharing articles of interest. I try not to overload them, but share resources kindly as they come up, and give them some resources so they feel empowered. If they want that additional information they can have it.
Clinical Educator
Now I'm going to talk about some strategies that can help the clinical educator be successful in that role or more successful in that role. One thing is considering how the clinical educator onboards students and communication. We're in the field of communication and communication really is key. I have found that when working with students you can't overstate anything. Be very specific about hours, dress code, introductions, and your communication preferences. What I mean by this is, our clinic is open from 8:00 to 5:00. I want you to be here at 7:40 and you plan to be here until 5:20. That's perfectly appropriate to state what the hours are and what your expectations are so the student can meet those expectations.
Dress code is my most hated topic and the one I have to talk about the most. We recently went to wearing scrubs in our own clinics so I feel like a lot of that conversation has whittled away, but I still need to have this conversation with students as I prepare them to go out in the field. For introductions in our on-campus clinic, our students introduce themselves with their first and last name and that they are AuD students.
You may have a different way you want them to introduce so be specific in describing what you want. Identifying communication preferences is also important. For example, do you prefer email, text, or phone calls? How do you want the students to communicate when they're not in clinic and when they need to reach you for something like a missed day? If your practice has a handbook it's a really great idea to provide that ahead of time so the student can have an opportunity to review it. Expect that they have reviewed it.
Part of the onboarding should include goal setting. By this time students should be really good at goal setting as they've been doing it for the fall, spring, summer, fall, and spring semesters. They should be pretty comfortable identifying where they have strengths and where they have areas of needed growth. I encourage you, as the clinical educator, to write those down for reference. I know that as I work with my students on campus I need to write those down and then reference them at midterm and at final at a minimum. Sometimes more often than that if needed. It's really helpful to have those written down and to show the student this is what we talked about. It also gives you a sense of some third-year goals. Often students are working on increasing their time management for particular skills, demonstrating greater independence and counseling, and integrating test results in a meaningful manner for the patient. Those are common kinds of things that my third-year students tend to identify as goals and things that they're trying to work for.
Sometimes it's related to report writing which can be a challenge as it looks different on campus and with different off-campus sites. I would say that successful placements start when the student has an opportunity to observe you as the clinical educator for the first day or two. It takes time to figure out the flow and what the expectation is. It can be helpful for the student to watch how you move a patient into your setting, do the testing, gather the forms, hear what you're saying in counseling and how you counsel, and then move the patient back out of your testing area. You don't think about those things yourself, but they are very different for a student coming into your practice. Letting them observe that helps to increase their confidence for a day or two but then they're going to be anxious to do something.
Immediately following those two days, there should be very heavy, 100% supervision for 1-2 weeks then you can evaluate their progress. Our students are really confident in some areas and quite skilled. I find even in the second year, I'll take a step or two out of the booth. I'm still close, but I could answer an email or something and then check back in. You've got to be careful of insurance and the kind of patient you're seeing and so forth and follow those rules, but there can be some more independence that way.
Feedback is another thing that's really important. I ask my on-campus students how they prefer to have feedback. Is it in the moment when I see something that I would want to go a different way or that I need to talk to them about, or is it after the appointment? I talk to my students about how sometimes there is not an option. If you are testing an infant, I only have so much time until that baby's going to wake up. We are going to move quickly so you're going to be corrected or guided at the moment if that needs to happen. But there are times where it's not wrong and the patient is not being harmed in any fashion. Let's talk about how you could do that more efficiently. Those are things I can talk about after the moment. I do try to get the student's preference ahead of time so that I can adjust accordingly.
I also encourage clinical educators to communicate verbally daily and weekly in writing. I'm going to give you a suggestion for a way you could do that quickly if that would be helpful. Semester midterm and final semester evaluations go to the student and the externship coordinator. That one always has to be written. That one's a non-negotiable for our particular program. I encourage clinical educators to address problems early so that they don't have to be addressed often.
Common problems tend to be communication-related, including a misunderstanding of hours or personality issues. A very energetic student can sometimes be uncomfortable for a patient who's hesitant or more subdued or quiet. Talking those through early is going to help everyone's life going forward. Realize that as a clinical educator, you have the externship coordinator in your back pocket to help you with any troubles that persist.
Purdue uses a daily feedback sheet for our on-campus students. A sample of this checklist can be seen in Figure 3. We use it as a check and minus kind of thing and it's a prompt to pay attention to some of the different skills the students did for the day. I'll use this form for the whole day for when if we see five or six patients because at the very bottom it has an area to note strengths, focus areas, and things we talked about for the day. I think that's what's most valuable to the students. They don't care as much about the checks and so forth. That's to remind me of what I need to be doing. It's the strengths and focus areas that seem to be particularly helpful. It's helpful for me at midterm and final evaluations to be able to look back and reference that.
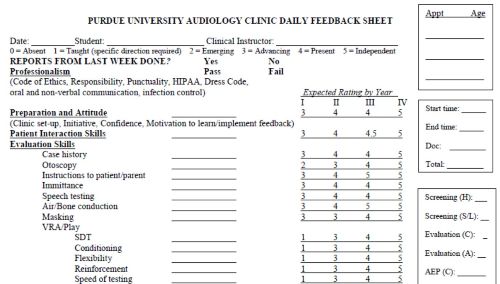
Figure 3. Purdue daily feedback sheet sample. (Click here to view this image in a larger PDF file.)
I think it is important as a clinical educator to seek CEU opportunities to grow in supervision skills. I noticed AudiologyOnline has more than ten courses on different aspects of supervision. There are many opportunities to grow in your clinical supervision skills. There's also SIG 11 in ASHA that has some resources and you can even do outside learning. Sometimes it's reflecting on that continuum model of supervision. There's a continuum model of supervision by Jean Anderson that talks about how when a student begins, it's 100% direct supervision.
With additional growth and understanding, that declines so the student takes on more and more of a role so that eventually they are independent, self-reflective, and self-corrective. What's good to keep in mind is that while this happens, we also need to take a step back and recognize that the student can be at different levels on that supervision model for different skills. Perhaps the student is very comfortable with diagnostics, but not very comfortable with hearing aids or the kind of hearing needs that you've worked with at your practice. Perhaps they're further along and more self-reflective for the skills related to diagnostics, but they still need a lot of guidance when it comes to the hearing aid section or amplification portion. It's good to keep in mind that the growth stages could be very different stages as these students come through.
Students
Let's talk about some strategies that are going to help the students be successful. Professionalism is key. The very first thing that I talk about regarding professionalism is professional dress. Students need to be empowered to ask the site about the dress code and what's acceptable. If there is time, it's helpful for students to see examples of professional dress and be allowed time to ask questions, as there are usually a lot of questions about dress code. We have a very specific dress code at the Purdue audiology clinic and students have ample time to ask. Every change of season brings in a new change of questions. Every change in fashion trends brings new challenges. For example, part of our dress code also has a lot of examples of what not to wear and what to wear.
| Don't Wear | Do Wear |
| Shorts/jeans/capris | Dress slacks |
| Tight/transparent tops | Blouses/shirts |
| T-shirts | Dresses |
| Dangling earrings | Name badges |
| Open-toed/athletic shoes | Closed shoes |
| Short tops with low pants | Long tops (NO visible midriff) |
| Leggings | Skirts |
| Mini skirts | Hair ties to keep long hair back |
| Low-cut/sleeveless blouses | |
| Long hair without a tie | |
| Perfumes |
We are very specific about what our expectations are for our clinic. They may be some of the most restrictive. We say that if you can pass our dress code, then you're going to do fine in any other setting. We give so many examples and talk about dress code a lot, but there are reasons behind why all of these things have appeared. I'm sure there are reasons you have in your own clinical settings as to why you have certain dress code rules. Scrubs have made life a lot simpler as far as this goes in our clinic.
Sticking with the theme of professionalism with our students, it is the externship coordinator's role to provide information regarding modes of communication and your expectations for those. It's also the clinical educator's role to be upfront with your expectations. As an externship coordinator, I talk to students about what non-verbal communication listening behaviors look like. For example, you're leaning up, not slouched, making eye contact, occasionally nodding your head, giving signs that you're paying attention, and what those signs look like.
We talk about written email communication and verbal communication. When I talk with students about verbal communication I remind them to use professional language and note the tone of their voice. That's often related to patients that we get a sing-song voice or vocal tone rising up when speaking to an older adult. That is inappropriate and sounds as though you're speaking down to that patient. I'll share examples of that when I talk with students.
In regard to written email communication, I have found it is best when students send me the initial communication they're going to have with their clinical educator so I can proofread it before they send it. This is the first time that they've sent this kind of professional communication. Usually, it's fine, but sometimes I have to have a conversation about what you're saying is this or what I'm reading is this. I know what you intend to say, but let's talk about it. Going forward I don't need to see drafts unless they want to run it by me, but I must be copied on all the communications. If something's not going well, I want to be able to see where things may have gone off track. They are expected to use no abbreviations in email, address the clinical educator professionally, and communicate succinctly.
I also think it's important that students know how your clinic and how you as a clinical educator would like disruptions to the schedule to be handled. Students are allowed to miss their externship for illness, funerals, and interviews. They need to know who to contact and how that communication should happen. Illness often can't be planned but it's nice to have as much notice as possible.
Finally, I encourage students to ask their clinical educator for clarification on any and all things that are unclear. It's often very eye-opening for a clinical educator to get some of the questions that they may get. There may be things that you thought were just known and sometimes it's surprising what's not just known. We work really hard at the university to recognize generational gaps and appreciate those differences. As instructors, we strive to teach in a way that is going to help our students learn and recognize those generational differences. It is my opinion that it is also important that students understand how to work well with those in other generations as well because these are going to be people that they're serving.
One of the things that I talk about is what initiative looks like to others. We could spend a lot of time talking about what it looks like to you or to me, but there are some general things that describe what initiative looks like. Most people think initiative looks like showing up a couple of minutes early, looking at a file early, and having your notepad and pen to take notes or ask questions or write down the answers. There are some things that look like initiative and those are things that we can talk about, such as offering to fill out a form. I think that that is an important conversation to have with students. It's okay for that to come from the externship coordinator and the clinical educator so that the student doesn't fail to meet expectations that they just didn't know were there.
As an externship coordinator, I also discuss ethics. I'm very specific regarding protecting our sites and not discussing pricing policies or particular things that set that site apart or make them unique. We value our sites and we do not want to damage that relationship in any way so we need to hold paramount things that are special and unique to that practice.
Struggles
Now let's talk about the inevitable struggles. I can't not talk about COVID. Our clinical educators were burdened both mentally and physically with keeping their patients safe and keeping themselves safe. Adding a student became too much for many of them. One thing that our university did was to offer to relieve the financial burden of PPE by providing that for our students. We were grateful for any site that was able to remain open. Most of those that stayed open were private practices at first. Hospitals were the last to come back on board because of so many protocols for them to keep everyone safe. It really was a struggle. But we did overcome it and all of our students maintained those three externship sites which was nothing short of a miracle during all of that.
I try to support the site that they're going to so they can be successful and try to avoid the struggle. One way is by encouraging sites to have an initial meeting with the students. So much miscommunication can be cleared up and avoided by having that. I encourage my clinical educators to communicate their expectations, both verbally and in written form. I have a sheet that I give every student. Here are my pet peeves that you need to know about. Then I also encourage clinical educators to be specific in their feedback to students. Don't assume anything. The more specific you can be, the more successful the student is going to be. Occasionally, we have a poor match. We do send strong students, but it just sometimes isn't a good match. It doesn't happen often thankfully, but when it does, we allow the clinical educators, who are our partners in all of this, to address the concern first. I am always prepared to bring the student in to talk about what kind of support and encouragement and things we need to do so that they will be successful. This also helps to gain their perspective on things. It's very important when dealing with that, that communication is very clear.
Successes
Now I would like to talk about the successes. In spite of COVID, using this model and this process for how sites are arranged with your plan B and so forth, we've had a growth in our number of sites. Every student I already mentioned maintained their three sites. We have amazing clinical educators who I call heroes. They have stepped up to provide these experiences and believe in the need for this, for our students, and for our profession.
Students have been able to gain experiences and have increased their appreciation of the process because there've been a lot of changes in the last year. In some cases, I've gone to plan C, D, and E. I think that they have a better appreciation for how the process works because I've shared it and been more open about that. The monthly reflections have been a huge success and have been well-received by everyone.
Why Supervise/Be a Host Site?
I'd like to pose a question and then answer it. Why would you want to supervise, or be a host site? Why become a clinical educator? Life is going well, why do I need to add a student?
Why Become a Clinical Educator?
I'm sure it would be a good feel-good to give back, but that sounds like a lot of stress. Students challenge you in a good way. I spoke with my partners, my clinical educator friends out there and asked, why do you take the student? They like that students keep them current. Students ask questions and challenge you in a good way. They say, well, why are you doing that? Why does that work? It helps you refine your own skills because when you're teaching a student, you are explaining it and are even more confident in things you're doing and in ways you're counseling. You definitely know you are doing evidence-based practice because the student will ask, why are you doing it this way?
Or they may say, I'm learning to do it this way, can you explain your way? We talk to our students about being open. There's a lot of right ways to do things. It's important to understand why the clinician or provider is doing things a particular way. It's rewarding and you do feel good about providing the service to your profession. You get to help shape a future professional and that feels good. Some of the clinical educators I talked to said it's professionally recharging to have a new voice around. That it's fun and enjoyable having the students there with you.
Why Become an Externship Site?
Why consider becoming an externship site? Maybe there are multiple practitioners at the site and you're on board but are wondering how to bring the site on board. It's a nice way to connect to other professionals. I have seen increased collaboration on cases and patients. I'm very comfortable referring patients who live far away from us to this particular site because I've had enough interactions and relations that I feel really good about the care they're going to get at that site and vice versa. We sometimes see referrals from some of the sites that we've partnered with. As an externship site, it can be a potential help for future job searches. You get a chance to see the students who are coming through then, as you're looking to hire, you may want to reach out to those graduates and see if they might want to come back.
Some of our current students work as office staff in some sites here and there. Not a lot but, they see value in having students and that younger generation coming in. It can be an opportunity for possible future collaborations like clinical research project ideas. Some of our students work with their clinical educators as evidence-based practice mentors. That's a wonderful opportunity for the student to have that site. Sometimes the clinical educator just really enjoys delving into a clinical question they've had. It can be good for business. Some programs advertise that they participate in student training or have an affiliation with the university.
Future Work, Directions, and Wrap-Up
There's always future work. I can always do more as an externship coordinator. I can always do more site visits, more follow-up phone calls, more reach out to new sites, and more in terms of thank yous, such as offering clinical educators CEUs, little trinkets, and showing our gratitude and appreciation more. I can always have more sites. I always need more educators. There's always more. I think that's the direction that those of us in a university role are always looking for. The more we have, then the less we're knocking on the door of the same site over and over again.
As I wrap up, this is just one model of how the semester-long externship placement might work. It's the model that works well for me. I'm always refining and adjusting and I'm open to change. The keys to success for my model when I'm working within it is that I stay organized but flexible, that I'm constantly working to expand that database of sites, and that communication with all parties is key including my students, my colleagues as clinical educators, and my colleagues as clinical faculty.
I did not address the student stipend or compensation issue today because it's a non-issue. These are semester-long experiences. This is just like having your on-campus clinic assignment, except it's an off-campus assignment and it's a different practice and so forth, but there is no compensation. It's a non-issue that becomes an issue with the fourth-year placement but not the one that I'm addressing here today.
References
Citation
Van Hyfte, S. (2021). Third-year aud clinical externships: strategies, struggles, and successes. AudiologyOnline, Article 27986. Retrieved from https://www.audiologyonline.com


