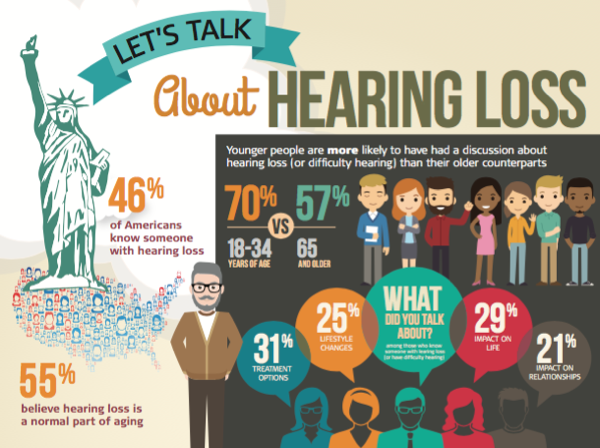
MED-EL Survey Explores Connection Between Age, Stigma and Motivating Factors for Having Hearing Checked
AudiologyOnline: MED-EL recently released new survey results that found that nearly half of Americans - 46% - know someone with hearing loss or difficulty hearing, and 64% have had a conversation with that person about it. Most adults said that they would feel comfortable talking with someone they knew if they thought they may be experiencing hearing loss or difficulty hearing. Do you think this could signal a potential shift in overcoming stigma that has traditionally surrounded hearing loss?
Barbara Weinstein, PhD: I think that we have to get the conversation moved forward if the tide is going to turn. The stigma is associated with wearing hearing aids. Some people say it makes you look like you’re old because you’re equating age with hearing loss. As more people begin to do something about their hearing, like using “starter” amplifiers and more people use new devices paired with smartphones, that’s going to normalize the idea of wearing something on your ear and getting hearing loss treated. For millennials, it’s a natural thing to have something in your ear. For older generations, as more people use technology, the stigma will diminish.
I’d also like to add, that since dementia is such as frightening prospect, and hearing loss has now been associated with dementia, this becomes a wake-up call for older adults to seek treatment, stigma aside.
(Click image to access full pdf)
AudiologyOnline: Compared to one in five adults (22%) who said that they would be offended if someone they knew approached them because they thought they were experiencing hearing loss or difficulty hearing, the majority – 78% - disagreed with this statement. How does this compare with your experience with older adults? Are Boomers speaking more openly and directly about hearing loss than the generation before them?
Dr. Weinstein: While some people might have a hard time admitting that they have difficulty hearing, most people around them notice that communication is growing more difficult. The first conversations surrounding hearing loss are usually with family members, particularly in the case of older adults.
Speaking from personal experience, I’m very sensitive to when one of my friends or family is clearly struggling with hearing and communicating. With friends, I usually notice that they are having trouble within 15 minutes. And, I always say something. They’re usually surprised that I picked up on their hearing loss. They’ll say, “How did you know? How can you tell? No one’s ever said anything…” In every case, they went on to address their hearing loss, they come back to me and say “you’ve saved my marriage.” This is the case for men and women alike.
I think that it’s not always obvious to people with hearing loss that most people around them can tell that they have a hearing problem – or wrongly assume that they are withdrawn or that something is the matter with them when they give answers that don’t make sense. What audiologists try to communicate is that by getting the right help, either through a hearing aid or cochlear implant, they can remain engaged, active and vital.
AudiologyOnline: To that point, one of the survey highlights was surrounding the large role that family members play in helping to motivate people with hearing loss or difficulty hearing to seek evaluation, particularly among older adults: 79% of adults 65 and over said that if a family member or loved one approached them about having their hearing checked because they were experiencing hearing loss or difficulty hearing it would motivate them to do so. How important is encouragement and support from family members in terms of hearing evaluation?
Dr. Weinstein: By far, the strongest association with hearing aid satisfaction is a strong social support network. For people with milder hearing loss, if you have someone with you during your evaluation, the evidence is clear: the likelihood increases that you will get the help that you need, and be more satisfied with that help.
As audiologists, we should be asking our patients to bring a family member for evaluations and appointments every time, as they have such an important role to play in the outcome.
AudiologyOnline: Additionally, 66% of Americans said that a major life event (e.g., marriage, birth of a child/grandchild, health scare) would motivate them to get their hearing checked if they were experiencing hearing loss or difficulty hearing. How often do you encounter these sorts of scenarios? What other motivating factors do you typically see?
Dr. Weinstein: There are a number of motivating factors. People start to notice that they are not enjoying going out anymore, they start to avoid situations, are not as active, and it all starts to add up before they take action. Oftentimes, the stress associated with communicating in challenging listening situations creates a lot of anxiety and causes people to withdraw before moving to the next stage of their journey.
One of the tipping points is definitely understanding grandchildren – that’s a biggie. People want to be able to communicate with their grandchildren.
Prodding by spouses is another motivator. Spouses will tell me, “You have no idea how hard it is to live with someone with hearing loss.” The hearing loss creates a lot of stress on partners and family and this is borne out in the literature. This goes back to the sentiment that a hearing loss intervention can save someone’s marriage, a comment that I’ve heard a number of times.
In terms of someone who is facing a health crisis, physician-patient communication is so important for shared decision making. If a person with hearing loss can’t communicate effectively with their providers, they are losing power and losing a say in decisions. We know from the literature that people with hearing loss go to medical appointments less frequently, and that accessing healthcare is more of a burden. People with hearing loss can feel marginalized.
Sadly, research has shown that people wait an average of 7 to 10 years before they take action to address hearing loss. The longer someone waits, the greater the burden of hearing loss and the more difficult the adjustment may be My hope is that with changes in affordability, accessibility and design of new technologies and with a life course approach to hearing loss this may all change. Audiologists must also broaden their scope so we remain part of the solution.
AudiologyOnline: The survey also found that one of the leading topics of conversation among people who have had a conversation about hearing loss was about treatment options (31%). A fairly large percentage – 37% - indicated that they weren’t sure about treatment for hearing loss once hearing aids no longer provide a benefit. How familiar are people with implantable devices? What is a good option for someone who might be “in between” a hearing aid and cochlear implant?
Dr. Weinstein: Personally, I think that one of the big issues is that health care professionals don’t understand how valuable an intervention like a cochlear implant can be, so they don’t have conversations with their patients. Health care providers don’t know how successful cochlear implant recipients can be, and that, even with older patients, contraindications are very low.
Misinformation about what’s covered by Medicaid, Medicare and private insurance is another variable that leads to confusion. I’m aware of several instances where patients were clearly cochlear implant candidates from an audiology standpoint, but their ENT told them that they weren’t because their insurance didn’t cover implants. So, the patients walked away saying that they weren’t candidates, instead of saying, “I’m a candidate, how can I get an implant covered?”
Another issue is that an audiologist may be reluctant to lose a hearing aid patient to a cochlear implant center. Their patients will keep coming back for more, when they’re not really getting the help that they need. This is a big issue, as it’s not in the best interest of the patient’s well-being. Most people want another, more powerful, hearing aid. But they’ve gotten to a point where these don’t help anymore, so a more in-depth conversation needs to take place whether or not this person is ready for a cochlear implant, physically, as well as emotionally. It’s possible to have hearing aids and cochlear implants as a part of the same conversation. In fact, many people with cochlear implants use a hearing aid in the non-implanted ear.
If hearing loss has progressed beyond hearing aids, but the candidate has residual hearing in lower frequencies that they want to utilize, audiologists can explore options like electric-acoustic stimulation such as the SYNCHRONY EAS (Electric Acoustic Stimulation) Hearing Implant System. EAS can be a great option for older adults who are not benefitting from hearing aids.
Implantables are the future and audiologists need to get more comfortable with the idea that they can work with implant patients. EAS allows for the opportunity to keep patients and continue to work with them.
AudiologyOnline: Thanks Dr. Weinstein. Interested readers are referred to MED-EL's press release for more information, and to the infographic, “Let’s Talk About Hearing Loss”
Background
This survey was conducted online within the United States by Harris Poll on behalf of MED-EL USA from June 28-30, 2017 among 2,264 U.S. adults ages 18 and older. This online survey is not based on a probability sample and therefore no estimate of theoretical sampling error can be calculated. For complete survey methodology, including weighting variables, please contact [email protected]