Hearing aid manufacturers are ever increasing the technology and functionality of hearing aid software to better serve the fitting needs of patients and hearing care professionals. With growing evidence placing importance on in-ear measures, many hearing aid manufacturers have integrated in-situ measures within their products. One such feature is in-situ pure-tone threshold measurements.
The in-situ audiometry feature now available on leading hearing instruments and software platforms enables hearing care professionals to perform audiometry using the hearing aid as the transducer to present the stimuli with the expected acoustic parameters in place. The aim of this study was to evaluate how well the audiometry data obtained using in-situ audiometry matched the thresholds that would otherwise have been obtained using conventional audiometry. Threshold data was obtained for 15 test subjects with known degrees of hearing loss diagnosed by way of conventional audiometry using the in-situ audiometry offerings from three hearing instrument manufacturers. Thresholds obtained using the two test methods were not different on a statistically significant level. The in-situ audiometry hearing-aid functionality offers a means to conveniently measure patient hearing sensitivity with resulting thresholds comparable to thresholds otherwise obtained with conventional audiometry.
Introduction
Pure-tone audiometry provides the hearing care professional with frequency and ear-specific information regarding the hearing sensitivity of the patient. Pure-tone audiometry thresholds are the gold standard for describing hearing acuity, and have been central to clinical audiology for several decades. Systematic descriptions of determining pure-tone thresholds through audiometry are described in the literature dating back to the late 1920s (Bunch, 1929) with only few changes being made in the decades that followed (Bunch, 1943; Carhart & Jerger, 1959). Other tests have since been added to the overall test battery to increase sensitivity to peripheral and central auditory system dysfunction (Hall & Mueller, 1997; ASHA, 2006). A more recent addition to clinical practice has been the introduction of hearing instruments offering in-situ functionality.
In Situ Functionality
In situ is a Latin term that, by definition, means "in the natural or original position or place." Audiologically, in situ has typically referred to measurements performed in the ear canal with the expected acoustic parameters set in place (i.e., earmold characteristics and residual ear canal volume) using the hearing instrument with which the patient has been or will be fit (Frye, 1982). As such, in-situ testing encompasses probe microphone measurements of gain and output, but can also include the assessment of audiometric data. The in-situ audiometry feature enables hearing care professionals to perform audiometry using the hearing aid as the transducer to present the stimuli.
In-situ measurements have been commercially available in hearing instruments for several years. Early implementations included the ability to measure most comfortable levels (MCL) and uncomfortable loudness levels (UCL) while taking into account the residual volume of the aided ear (Kiessling, 1987). More recent implementations of the in-situ audiometry feature allow hearing threshold measurements to be performed. The feature can be used to find the hearing thresholds of a patient for the purpose of fitting a hearing aid.
O'Brien and colleagues (2010) found that when real-ear to dial differences (REDD) were used and testing was performed in an environment with controlled ambient noise levels, in-situ audiometry generated valid and reliable measures of air-conduction thresholds. The measured thresholds can be translated into gain targets in the same way as thresholds obtained using conventional audiometry, and as such, should equate to the thresholds that would have been obtained with a conventional audiometer and calibrated transducers. Several of the in-situ audiometry feature offerings currently available from hearing instrument manufacturers claim a widely-used audiometry standard as the specification followed to ensure uniform performance and test results, comparable to the results obtained using currently accepted conventional audiometric procedures (ANSI, 1996).
When performing conventional audiometry, reliable test-retest values are expected to be within 10 dB (>99% for the frequencies 500 to 6000 Hz) of each test session, provided that no fundamental physiological changes have occurred within the auditory system between the test sessions (Schmuziger, Probst, & Smurzynski, 2004). Previous studies have established that unaided test-retest threshold reliability with in-situ audiometry is equivalent to the test-retest reliability expected when performing conventional audiometry (Smith-Olinde, Nicholson, Chivers, & Highley, 2006). The literature does not offer data that highlights performance of in-situ audiometry for different categories of hearing impairment and across hearing instrument manufacturers. The purpose of this study was a preliminary evaluation of the performance of the in-situ audiometry feature offered by three of the leading hearing instrument manufacturers, and to compare those findings to those obtained with conventional audiometry.
Methods
Nine male and six female hearing impaired test participants (aged between 31 and 81 years) with a known, bilateral, symmetrical hearing loss in the three categories of: mild-to-moderate, moderate-to-severe and severe-to-profound hearing loss were included in this pilot study (N=5 in each group). Individual hearing thresholds were obtained using the in-situ feature commercially available in the software and supported products from three different hearing aid manufacturers. Hearing instruments were coupled to the ear using double or power domes (receiver-in-the-canal (RIC) device types) or occluding Comply Snap Tips with #13 tubing (receiver-in-the-aid (RITA) device types). Test participant thresholds were verified with conventional audiometry, performed using the GN Otometrics AURICAL Audiometer Module in combination with a TDH39 transducer and ME70 circumaural fixtures from Madsen Electronics. The choice of circumaural earphones rather than insert earphones was due to limitations in availability of transducers at the test site.
The test order for the two methods and manufacturer devices was randomized based on a Latin square. All testing was performed in one session with a scheduled break between each test method. All testing was performed in a sound-treated booth with double sound-treated doors. The psychoacoustic method utilized for both the conventional and the in-situ audiometric testing was the modified Hughson-Westlake method with a 5 dB step size (Carhart & Jerger, 1959).
In-situ testing was performed for all octaves available for testing through each manufacturer's software platform, ranging from 250 Hz to 8000 Hz. However, some manufacturer software did not offer in-situ audiometry testing below 500 Hz or above 4000 Hz; resulting data, therefore, is only displayed for this limited frequency range.
Results
The spread in data distribution shown in Figure 1 (min, max and median values) was seen for 500, 1000, 2000 and 4000 Hz. Data is displayed for conventional audiometry and for each manufacturer's in-situ audiometry offering (labeled as Man 1, Man 2 and Man 3). The mild-to-moderate group was the only one that was tested with Manufacturer 3. A Kruskal-Wallis test was conducted on the data in order to ascertain if a significant statistical difference existed between the threshold data obtained using the in-situ feature implementations and the threshold data obtained using a conventional audiometer. The results of the statistical analysis are plotted in Figure 1.
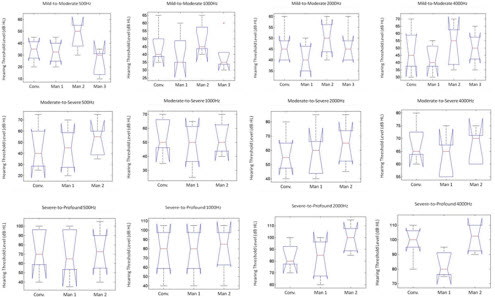
Figure 1. The across-subject differential values at 500, 1000, 2000 and 4000 Hz. Median values are denoted by the red line, the edges of the boxes show the 25th and 75th percentiles, and the whiskers mark the maximum and minimum values of the data set. Click Here to View Larger View of Figure 1 Graphs (PDF)
Although average tendencies are of interest, it is clinically more relevant to know what to expect for an individual patient, as this could significantly impact the hearing aid fitting. Therefore, the in-situ threshold data was also evaluated based on the variation from conventional audiometry thresholds obtained for each individual test ear included in the study. In order for the variation observed between test methods to be clinically insignificant, the in-situ threshold data would be expected to fall within the test re-test variation of 10 dB currently accepted when performing conventional audiometry (Smith-Olinde, et al., 2006). The threshold data obtained using in-situ audiometry was within 10 dB of the threshold values obtained using conventional audiometry for the three manufacturers as reported below (Figure 2). Note the low number of ears for manufacturer 3.
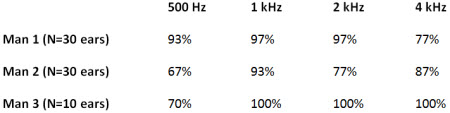
Figure 2. Calculated level to which in-situ test thresholds were within a 10 dB test-retest reliability of conventional audiometry measures.
Discussion
The results of the analysis showed no statistically significant differences between mean conventionally-obtained hearing threshold levels and the hearing thresholds obtained with any of the in-situ audiometry features from three different manufacturers. The statistical analysis was performed for each frequency individually. The null hypothesis was that the data obtained using in-situ audiometry and conventional audiometry comes from the same distribution with identical medians. The individual p values calculated from the statistical set confirm this hypothesis at a significance level of 5 % at each frequency; the differences between test methods were not statistically significant. (Mild-to-Moderate: 500 Hz, p=0.07; 1000 Hz, p=0.17; 2000 Hz, p=0.35; 4000 Hz, p=0.71; Moderate-to-Severe: 500 Hz, p=0.68; 1000 Hz, p=0.81; 2000 Hz, p=0.64; 4000 Hz, p=0.57; Severe-to-Profound: 500 Hz, p=0.85; 1000 Hz, p=0.97; 2000 Hz, p=0.14; 4000 Hz, p=0.14). The results from the two audiometry test methods could, in other words, have come from the same test methods.
It should be noted that although no statistically significant differences were found between the average results obtained with the different test methods, some manufacturer implementations of the in-situ audiometry functionality result in threshold data that are more closely matched to the threshold data obtained using conventional audiometry on an individual basis (See Figure 2). In other words, these data indicate that the hearing care professional can expect more consistent results with two of the three tested implementations.
How much does this matter? Variations exceeding 10 dB from the conventional audiometry thresholds may have significant clinical implications for hearing aid fitting. Differences as large as 20 dB between in-situ audiometry and conventional audiometry were observed, consistent with the findings reported by O'Brien, et al. (2010). These differences could easily translate to gain prescriptions differing by 5 to 10 dB as well as differing compression ratios. This could lead to over- or under amplification as a result of artificially high or low thresholds. Of course, it is important to point out that in many cases, it might be that the in situ derived threshold is correct, and the traditional audiometric threshold is not. This would be especially true for patients with real-ear to coupler differences (RECD) that significantly deviate from average. Verification of hearing instrument gain, capturing the unique acoustic response of the individual ear through probe tube testing, is therefore important irrespective of how the thresholds used to calculate the gain target were derived (Digiovanni & Pratt, 2010).
For the purposes of this study all testing was performed in a sound treated room. In-situ audiometry testing may be performed in a setting where there is no access to a sound treated room. It would be reasonable to assume that the presence of excessive ambient noise levels would result in artificially elevated low frequency thresholds. Some manufacturers offer a tool in the fitting software that measures the level of ambient noise present prior to threshold testing being conducted. This tool will inform the hearing care professional if noise levels are too high for threshold testing to be carried out. The hearing care professional should remember that although testing is being performed using the hearing instruments as the transducer, the same precautions apply as is the case when conducting conventional audiometric testing.
In addition to the above stated considerations, some limitations exist when performing in-situ audiometry compared to conventional audiometry. Each hearing instrument unit is calibrated and verified for performance within the manufacturer guidelines when released from production, and the in-situ audiometry feature can be expected to perform optimally. However, components are known to drift in function with time and consistent patient use. This drift in performance may cause the in-situ audiometry feature to decline in performance over time, as the actual output delivered by the device for a particular dial reading may not match the originally-calibrated values.
Recent research has found that leakage of low frequency energy from the ear canal occurs with in-situ audiometry testing when using either open or instant-fit tips, resulting in significantly higher low frequency thresholds compared to conventionally measured thresholds (O'Brien, et al. 2010). It would therefore result in more accurate threshold data if utilizing average or individually measured real-ear to dial difference (REDD) values.
Another limitation pertains to the inability to perform masking with current in-situ audiometry offerings. The use of the hearing instrument as the transducer can be viewed as similar to the use of insert headphones, allowing an asymmetry of 55 dB HL to exist before the risk of cross-hearing arises (Munro & Agnew, 1999).
Finally, and perhaps most importantly, in-situ audiometry features are not appropriate for diagnostic audiometry. They can test air conduction only, limiting their application to screening and specific hearing aid fitting applications. Because bone conduction cannot be tested, the software cannot account for possible conductive or mixed hearing loss pathologies that may exist, and may further preclude accurate hearing aid fitting if diagnostic audiometry is not performed to establish bone conduction thresholds. Moreover, the in-situ audiometry features should not take the place of routine diagnostic audiometry, but rather should be used as a reliable cross-check measure to encourage a more proper hearing aid fitting. These limitations should be taken into account when performing audiometry using the in-situ feature.
Study Limitations
An obvious limitation of this study was the small size of the data set. At the time of writing, a larger scale study including the in-situ audiometry feature from four hearing instrument manufacturers was being performed. Another limitation, dictated by the availability of calibrated transducers at the test site, was the use of TDH39 earphones when conducting conventional audiometry. The use of insert earphones would have resulted in similar residual ear canal volumes for the two test methods, and would have perhaps increased international applicability.
Conclusions
In-situ audiometry is a valid method for performing threshold testing by air conduction in cases where asymmetry between the ears of the audiology patient does not exceed 55 dB HL. Although some variation in achieving thresholds within 10 dB HL of the conventional audiometry thresholds exists between manufacturers, in-situ audiometry test results are reliable and appear to be comparable to the thresholds that would have been obtained for the same patient using conventional audiometry. This has the potential to add convenience and efficiency to the hearing instrument fitting procedure, as the ability to present stimuli using the hearing instrument as the transducer requires less equipment and less space, and can facilitate the provision of audiometry services where these currently are limited.
Acknowledgements
Thank you to my colleagues at GN ReSound A/S who contributed to this study and/or article: Jennifer Groth, Lotte Hernvig, Greg Olsen, and Tobias Piechowiak.
References
ANSI (1996). American National Standard Specifications for Audiometers. S3.6-1996.
ASHA (2006). Preferred Practice Patterns for the Profession of Audiology. Retrived from: www.asha.org/docs/html/PP2006-00274.html
Bunch, C. C. (1929). Age variations in auditory acuity. Archives of Otolanryngology, 9(6), 625-636.
Bunch, C. C. (1943). Clinical audiometry. St. Louis, MO: Mosby.
Carhart, R. & Jerger, J. F. (1959). Preferred nethod for clinical determination of pure-tone thresholds. Journal of Speech and Hearing Disorders 24(4), 330-345.
Digiovanni, J. J. & Pratt, R.M. (2010). Verification of in situ thresholds and integrated real-ear measurements. Journal of the American Academy of Audiology, 21(10), 663-670.
Frye, G. J. (1982). In situ and etymotic hearing aid testing. Hearing Instruments 33(2), 32-36.
Hall, J. W. & Mueller, H.G. (1997). Audiologists' desk reference. San Diego, CA: Singular Publishing Group Inc.
Kiessling, J. (1987). In situ audiometry (ISO). Hearing Instruments, 38(1), 28-29.
Munro, K. J. & Agnew, N. (1999). A comparison of inter-aural attenuation with the Etymotic ER-3A insert earphone and the Telephonics TDH-39 supra-aural earphone. British Journal of Audiology, 33(4), 259-262.
O'Brien, A., Keidser,G., Yeend, I., Hartley, L., & Dillon, H. (2010). Validity and reliability of in-situ air conduction thresholds measured through hearing aids coupled to closed and open instant-fit tips. International Journal of Audiology, 49(12), 868-876.
Schmuziger, N., Probst, R., & Smurzynski, J. (2004). Test-retest reliability of pure-tone thresholds from 0.5 to 16 kHz using Sennheiser HDA 200 and Etymotic Research ER-2 earphones. Ear & Hearing, 25(2), 127 - 132.
Smith-Olinde, L., Nicholson, N., Chivers, C., & Highley, P. (2006). Test-retest reliability of in situ unaided thresholds in adults. American Journal of Audiology, 15(1), 75-80.