Learning Outcomes
After this course learners will be able to:
- Describe the most common complaints from patients following the hearing aid fitting.
- Describe the outcomes of research when the patients are allowed to select the best fitting for themselves.
- Describe the processes of hearing aid acclimatization and how it might impact the hearing aid fitting.
- Provide examples of how machine learning is used in today’s hearing aids.
- Describe common changes that might be made by the Signia assistant, and how patients reacted to these changes.
V2.1: What Post-Fitting Problems Are Common?
It is well known, that following a successful clinical fitting of hearing aids, and a welcome patient report at that time that “all is well,” many patients will subsequently report “problems” once the hearing aids are being used in everyday listening situations. Some of these problems do not directly relate to the hearing aids or their programming, but rather, unrealistic expectations. For example, it is not uncommon on follow-up visits for patients to report that the hearing aids do not work in background noise as well as they had hoped. This often is a patient whose optimum SRT-50 in background noise is ~10 dB SNR or worse, who wants to understand in a restaurant with an SNR of +2 dB. This then becomes a counseling issue.
On the other hand, there are some post-fitting issues that are real and expected, and fortunately are relatively easy to fix. One of these is these is the programmed gain for various input levels. If we only look at average-level inputs, we know from background data used for the development of the NAL-NL2, that 1 standard deviation for preferred gain is around 5 dB. This suggests that about 1/3 of the patients that we fit, will have a preferred gain level that is either higher or lower this +/- 5 dB window. If patients are not able to make this correction themselves, this is something that might need post-fitting attention.
Reports from Hearing Aid Users
We of course do not need to speculate on what post-fitting issues might exist, as this has been documented in several research studies. For example, in one of these studies, based on previous pilot work by the authors, a list of 26 potential post-fitting problems were presented to hearing aid users, who then selected which of these problems applied to them (Bennett et al, 2020). The mean response was that ~10 of the identified problems were experienced by the average user. The top ten problems identified by the most users are shown in Figure 1.
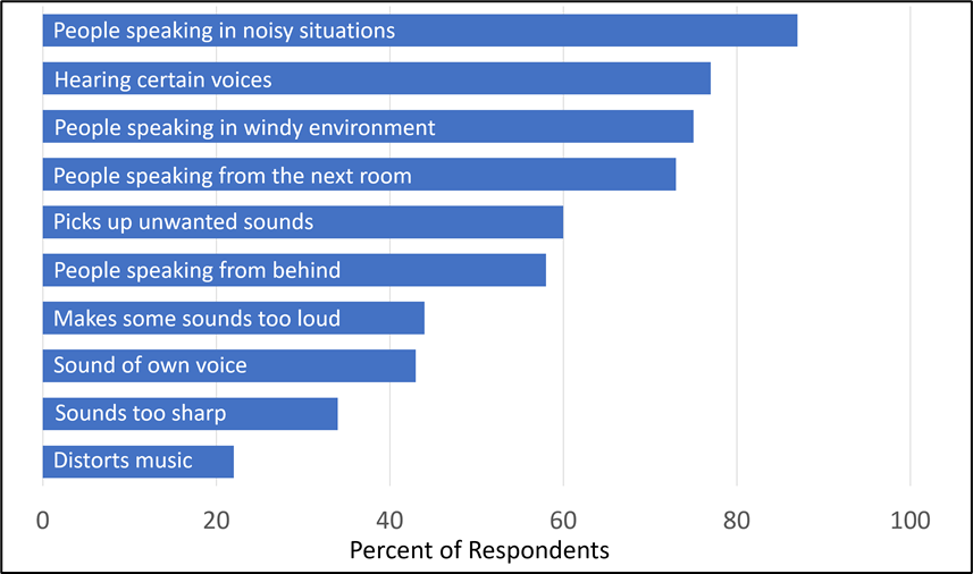
Figure 1. Based on pilot data, hearing aid users responded to a questionnaire that identified 26 potential post-fitting problems. Shown here are the top ten problems identified, and the percent of respondents who identified each.
Not surprisingly, the leading problem identified was picking up people speaking in noisy environments (87% of respondents), and the top four issues appear to involve either audibility or background noise. As would be predicted, the authors report that the number of problems inversely related to the patient’s report of benefit from and satisfaction with hearing aids. While meaningful, these results probably make the post-fitting situation look worse than it really is, as these were not complaints generated by the patient, but simply provided to them on a check list. Moreover, we know that most adults with normal hearing also have problems picking up a speaker in a noisy environment. And also, the recent MarkeTrak 10 survey revealed that 76% of hearing aid owners (those with relatively new hearing aids) are “satisfied” with their ability to follow conversations in background noise (Carr, 2020).
Reports from Audiologists
Another method to determine what problems exist following the hearing aid fitting, and how the patient describes them is to survey audiologists. One approach to this, used by a group of researchers, was to present to clinical audiologists fitting hearing aids 16 different potential post-fitting problems. The audiologists (n=>300) then reported what they believed the patient would say if these problems existed (Jenstad et al, 2003).
The top ten comments are shown in Table 1. The same complaint could be expressed for different fitting problems. These are not necessarily the top 10 complaints, as the responses were somewhat driven by the fitting problems that were used as examples.
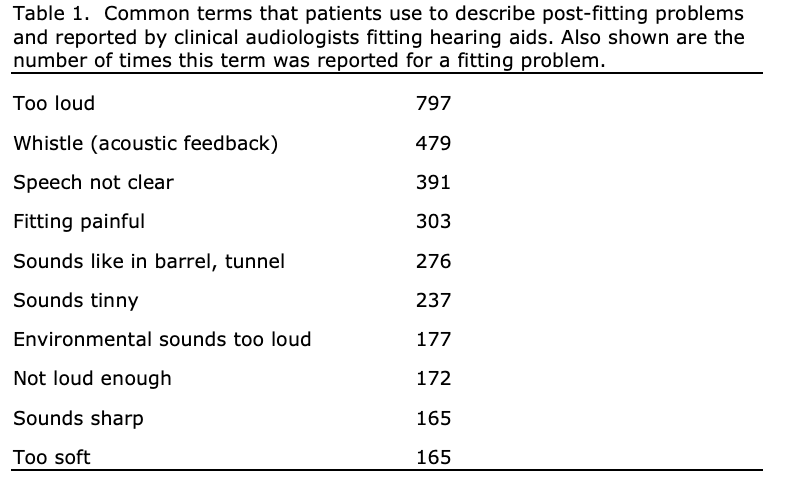
Since the time that this research was conducted, changes in hearing aid technology and fitting practices probably has reduced the frequency of four of these issues:
- Advances in adaptive feedback suppression have greatly reduced the “whistle” complaint.
- The use of open fittings and own voice algorithms have significantly reduced the complaints of “hollowness” and “echo effects.”
- The common use of WDRC with low compression kneepoints has resulted in MPO settings that are quite low (maybe too low; Mueller et al, 2021) and the loudness complaint isn’t as common.
- Finally, the reduced use of custom instruments, smaller hearing aids and instant-fit coupling systems have eliminated many of the previous comfort issues.
Today, we of course would need to add connectivity issues to the list, which many HCPs report has risen to the #1 post-fitting problem. Each year, rechargeability (or lack of it) also keeps rising as a problem, partly because of the more common use of this feature, but also due to malfunction.
Recent research examined what post-fitting issues might arise when TeleCare and remote programming was used as the communication mechanism, rather than an office visit (Froehlich et al, 2019). Both new and experienced hearing aid users were fitted bilaterally, and studied over a one-month field trial. During the trial, communication sometimes was initiated by the clinicians, in other instances, by the patients. In total, there was an average of 12 messages exchanged for each patient. Of the multiple messages, 40% of the patients reported issues, that to be solved, would require programming changes. Interestingly, understanding speech in background noise was not one of the leading complaints. The three most common fitting issues were: sounds too sharp, whistling (feedback) and poor sound quality/distorted. It’s important to note, that in this research, all participants were fitted to the DSL5.0 prescriptive method, which compared to other fitting algorithms, tends to have more high frequency gain. This very likely could have contributed to the complaints of too sharp, and also the feedback issues.
What Post-Fitting Issues Can (Should) Be Fixed?
When considering the post-fitting problems that we have mentioned here, some practical questions need to be asked:
- Is this a problem that can be fixed through follow-up programming, or is it a counseling issue?
- Will fixing the problem create a new problem?
- Does the patient know what is best for them?
- Will the problem solve itself over time through acclimatization?
Regarding what problems are important to address, it is helpful to review what factors tend to lead to success with amplification. In a study of 160 individuals who had been fitted with hearing aids in the past two years, Australian researchers analyzed over 50 variables which could contribute to benefit and satisfaction with hearing aids (Hickson et al, 2014). What they found was that of the leading 5 variables, only one was related to the actual programming of the hearing aids—individuals whose gain was programmed close to NAL targets for soft speech had more satisfaction than those who were under-fit. An interesting finding, given that patients rarely complain that soft sounds aren’t loud enough, and in fact, the complaint of “soft sounds too loud” is relatively common. This of course begs the question . . . do patients know what is best for them? Something which we will review later in the paper. The other high-ranking factors, not directly related to programming, that were shown to be statistically influential were positive support, findings from the HHIE, and attitudes toward hearing aids (Hickson et al, 2014).
Making Meaningful Changes
As we observe the post-fitting issues that patients report, we see that many of them possibly could be resolved through programming changes (if we determine that that is the best for the patient). It’s important to consider, therefore, what degree of change makes a difference? If we want to fix the “too tinny” problem, is that a 2 dB change? A 5 dB change? Or a 10 dB change? Fortunately, this has been examined in systematic research studies.
In one study with direct clinical implications, 32 experienced hearing aid users made judgements (better, worse, or the same) regarding changes in gain in the speech signal, relative to their prescribed gain (Caswell-Midwinter & Whitmer, 2021). There were 18 experimental adjustments. These were both increments and decrements of 4 dB, 8 dB and 12 dB for three different frequency bands: low frequency, mid-frequency and high frequency. There also were three “control” adjustments, where the speech signal was not changed (0 dB for all three bands). Participants compared each adjustment to their standard fitting 10 times, totaling 210 comparisons.
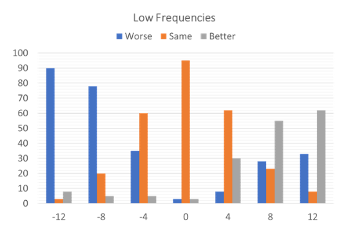
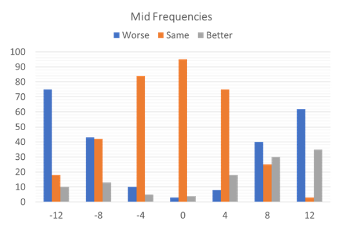
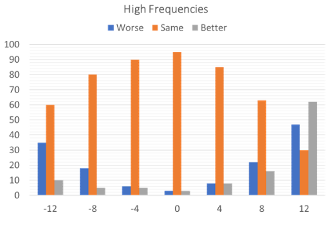
Figure 2. The preference data for all judgments made across all participants, showing what percent of time a given alteration in the signal was rated better, worse, or the same. The judgments are shown in three different panels (left to right): Low Frequencies, Mid Frequencies and High Frequencies (adapted from data of Caswell-Midwinter & Whitmer, 2021).
Figure 2 shows the preference data for all judgments made across all participants, showing what percent of time a given alteration in the signal was rated better, worse, or the same. The 12 dB low frequency increment was the adjustment with the most “better” responses, and the 12 dB low frequency decrement was the adjustment with the most “worse” judgments. High frequency adjustments resulted in the most “no different” responses. Importantly, when the control was presented (no difference between the two speech samples), in nearly 100% of the cases the participants reported “no difference,” suggesting good reliability for this measure (see Figure 2).
The findings of this study which perhaps are the most relevant to clinical practice relate to the ratings for the high-frequency band, as this is the frequency region that often is adjusted. Note that when the signal was reduced by 8 dB, 80% of the ratings were still “no different,” and there were 58% “no different” ratings when the signal was increased by 8 dB. This suggests, that if we are to make changes based on complaints from the patient, in most cases large changes will be necessary before a true perceptual difference will be observed. This finding prompted the authors to conclude: “The scale of gain adjustments necessary to elicit preferences, along with the low agreement and reliability in descriptors for these adjustments questions the efficiency and efficacy of current description-based troubleshooting, especially with short speech stimuli (Caswell-Midwinter & Whitmer, 2021; page 427).”
These data then beg the question, how much should we rely on patient comments and judgments when we make changes to the hearing aid programming. Are there comments valid? Do they know what is best for them?
V2.2: Reliance on Patient Judgments
In general, when a patient has a specific complaint following the initial fitting, and this complaint can be resolved, or at least partially resolved with hearing aid programming, it is tempting for most HCPs to try to take care of the issue. For example, it could be that after programming the hearing aids to appropriate audibility for soft sounds, the patient returns to the clinic stating that these sounds are too loud and bothersome—things like “I can hear the sound of a pen when I’m writing” or “I can hear myself walk on carpet”. This is pretty easy to fix with programming, but should it be fixed? Are patients the best judge of what is best for them?
Trainable Hearing Aids
One area of research which provides some insight regarding the “patient decides” topic, is the use of trainable hearing aids. That is, the hearing aid “trains” to new gain settings based on the patient’s volume control adjustments while using the hearing aids for several weeks in the real world. In one of the earlier studies with trainable hearing aids, a crossover design was used to study participants who were initially fitted to either 6 dB above or 6 dB below NAL targets (Mueller et al, 2008). The participants trained the gain for two weeks, returned and were fitted to the other condition, and trained for two more weeks. The two primary research questions were as follows: (1) Will the subjects tend to train toward the NAL prescription targets? (2) Will the starting point influence the end point for gain training?
When the participants were initially fitted 6 dB above the NAL, they tended to train down a little, to 2 to 3 dB above the NAL. When the same participants were fitted 6 dB below the NAL, they trained to about where they started, ~5 dB below the NAL. These trends were not influenced by what condition the participant had first. The authors concluded that there appears to be a wide range of “acceptable” gain for most participants (~7-8 dB on average), and the starting point for training can have a significant impact on the final trained gain—when fitted below target, the patients appeared to be satisfied to stay below target.
There is a belief among some HCPs, that when hearing aids are replaced, the gain and output should be set to what the patient has gotten used to. A second study with trainable hearing aids questioned whether experienced hearing aid users will train to the gain that they had previously used when fitted to the NAL prescription using new trainable instruments (Mueller and Hornsby, 2014). The participants specifically selected for this research were those who were satisfied hearing aid users, but who had been using hearing aids that were programmed about 10 dB below NAL targets for soft speech and 5 dB below for average speech inputs. The hearing aids used in this research had compression training, so it was possible to train the gain for soft, average and loud inputs independently.
As shown in Figure 3, following real-world training, the participants did not train to their previous use gain, but rather trained to gain similar to that prescribed by the NAL. Overall findings showed that 55% of the participants were using 10 dB or more gain for soft inputs following training than they had previously been using.
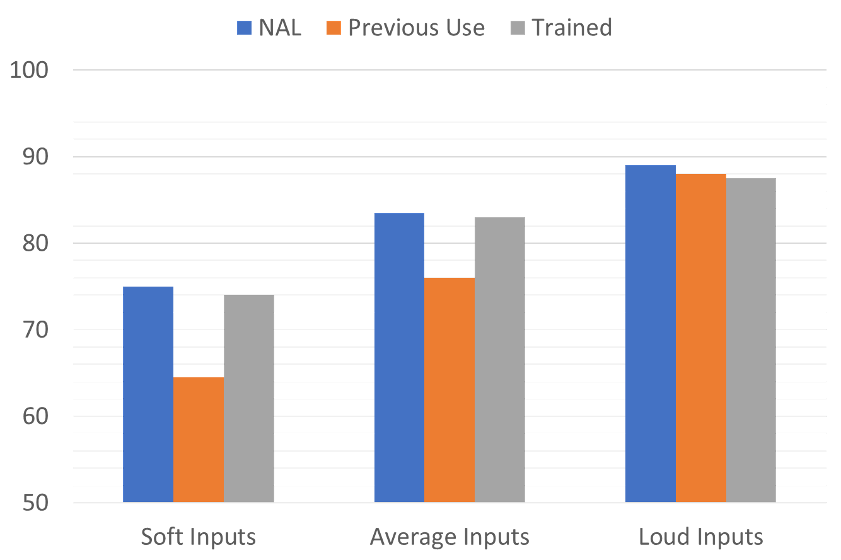
Figure 3. Shown are the mean output values (average of 2000 to 4000 Hz) for three conditions: the individualized NAL programmed output, the output used by the participants prior to the study, and the output trained by the participants after real-world hearing aid use (adapted from Mueller and Hornsby, 2014).
Selecting the “Best” Hearing Aid
One large research project that examined the ability for patients to select the “best” hearing aid is the NIH-funded study from Larry Humes and colleagues (Humes et al, 2017). This study looked at the efficacy of hearing aids for older adults and compared those fit using audiology best practices versus those obtained via an alternative “OTC-like” approach.
While it was referred to as an OTC approach, it was quite different than going shopping on aisle 7 at your neighborhood pharmacy. The “counter” was at a major university clinic, 135 (41%) of the potential participants were rejected, and the hearing aids were premier open-fit RIC hearing aids from a major manufacturer. The Consumer Decides group (sometimes called the OTC group) did some listening trials with three different pairs of hearing aids, pre-programmed to NAL-NL2 targets for different degrees of hearing loss. They then selected what they believed was the best for them. This group was then compared to a separate group that were fitted by audiologists using best practices (NAL-NL2 targets verified with probe-mic measures).
One aspect of the study that relates to our discussion here is the comparison of the hearing aids selected by the participants versus the hearing aids that would be deemed appropriate by an audiologist, based on the patient’s degree of hearing loss and the NAL-NL2 fitting algorithm. This comparison is shown in Figure 4.
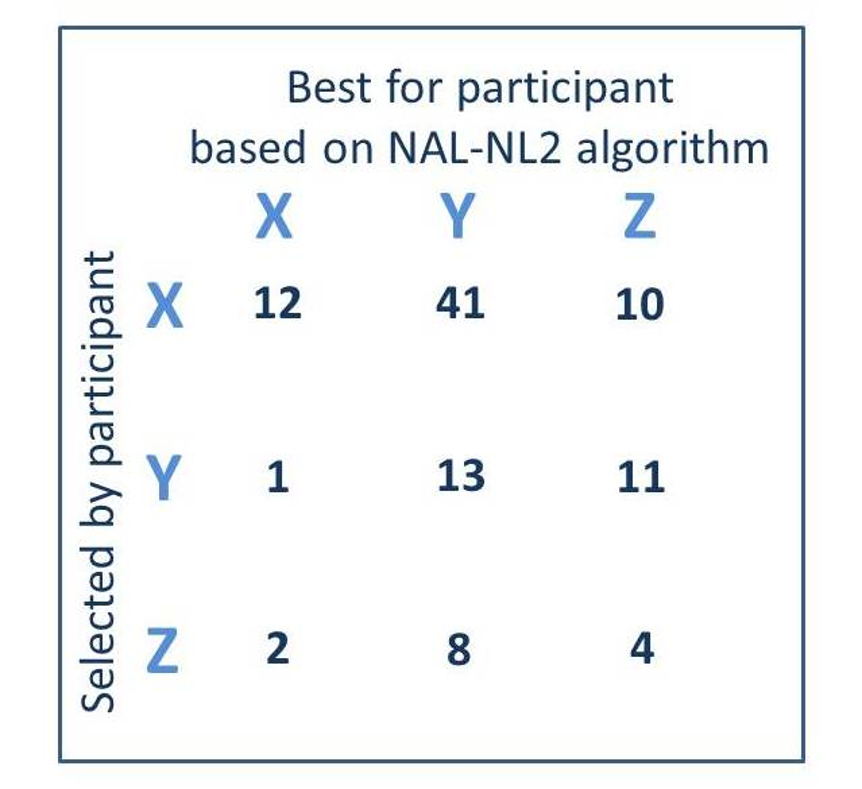
Figure 4. A comparison of the hearing aids (X, Y, or Z) selected by the participants (read horizontally) vs. the hearing aids that would be deemed appropriate based on the NAL-NL2 fitting algorithm (read vertically). Each cell represents the totals (right and left) for the 51 participants fitted bilaterally (adapted from Humes et al, 2017).
Figure 4 shows the combined right and left ear findings for 51 participants of this group (102 fittings). Recall that the hearing aids were pre-programmed, so it was possible to determine which one of the three hearing aids (X, Y, or Z) would be most appropriate for each participant based on their hearing loss (read vertical on the Figure). We can then compare this with what the participant selected (read horizontal on the Figure). If agreement was present, the big numbers would be in the diagonal, but they are not. Note that in 63 cases the consumer picked hearing aid X, whereas, based on the audiologists’ selection, this hearing aid only would have been selected for 15 of the fittings. Overall, the consumer picked the “wrong” hearing aid about 70% of the time. The researchers published the average aided Speech Intelligibility Index (SII) for the Consumer Decides (OTC) group. As you might guess, consumers tended to under-fit themselves, as their as-worn average SII was around .60 for average speech inputs. We’d expect an SII of approximately .66 for this degree of hearing loss for a NAL-NL2 fitting.
Another study related to OTC products examined the ability of participants to self-program their hearing aids (Sabin et al, 2020). Participants were first fitted to the NAL-NL2, and then this fitting was adjusted based on subjective preferences—the requested adjustments typically were a reduction in gain. After using the NAL-NL2 fitting for a week, a sub-group of individuals were then fitted with hearing aids set at 0 dB REIG, and using a self-programming device, adjusted the hearing aids to their preferred settings during a real-world home trial. For overall gain, the resulting values selected by this group were, on average, only ~2 dB lower than the NAL-adjusted gain previously selected in the clinic. Viewing band-specific gain, the values selected by the self-fit group were, on average, within 5.6 dB of those selected in the clinic, and did not vary systematically across frequency. This suggests that given the right fitting tools and hearing aids, and the experience of real-world listening, patients may select a reasonable fitting for themselves, although self-programmed gain for soft inputs was missing from the article. And also, recall that these individuals used properly fitted hearing aids prior to the re-set to 0 dB REIG.
What About the Placebo Effect?
When discussing the merits of allowing the patient to pick what is best for them, we cannot ignore the placebo or bias effect, which has been studied considerably related to hearing aid fittings. Bias, either from the clinician or the hearing aid user, can influence patient perceptions, and even performance.
One study that clearly showed the strong biasing affects that are present by simply labeling hearing aids was completed when digital hearing aids were just becoming popular. This study used a two-month real-world trial (Bentler et al, 2003). For one month, participants wore hearing aids labeled “state-of-the-art digital;” the other month they wore hearing aids labeled “conventional,” although in reality they were wearing the same hearing aids. At the end of each month the participants completed a battery of speech recognition and self-report measures.
When the results for the two different month-long trials were compared, there were no differences in speech recognition scores across the two conditions; however, labeling clearly affected self-perception. When the hearing aids were labeled “digital,” the self-report subscales of the APHAB were rated significantly higher. When asked to state a preference for continued use, 33 (83%) of the 40 participants expressed a preference for the fitting that had been labeled “digital.”
In a similar study of hearing aid bias, participants compared two devices that were acoustically identical, except one was described as "new" and the other as "conventional." Participants completed a speech-in-noise test, sound quality ratings, and rated overall personal preference for both hearing aids (Dawes et al, 2013).
The results of this study revealed that when using the “new” hearing aids, participants had significantly better mean speech-in-noise performance (70.9% versus 66.8%) and sound quality ratings (8.1 versus 7.4). This suggests that in addition to differences in self-reported outcomes and general preferences, the placebo effect can be so strong that patients may actually try harder (and consequently perform better) on objective outcome measures! A significant proportion of participants (75%) expressed an overall preference for the "new" hearing aids.
Finally, it’s useful to go back to the large Humes et al study mentioned earlier (Humes et al, 2017). In addition to the Best Practice and Consumer Decides groups, there also was a Placebo group. For this group, the hearing aids were carefully fitted using probe-microphone measures so that insertion gain was 0 dB. That is, the gain of the instruments was just enough to compensate for open ear insertion loss that might have occurred due to the placement of the fitting tip. The participants did not have any control of gain, so during the entire field trial, the hearing aids were used at 0 dB gain. At the beginning of the study, all participants from all three groups purchased their hearing aids, and at the end of the study, a refund was offered. For the Best Practice group, 81% chose to keep their hearing aids. The total was 53% for the Consumer Decides group. But the interesting finding, was that 36% of the Placebo group choose to keep their hearing aids—recall, the hearing aids had 0 dB gain.
While we all recognize the importance of “listening to our patients,” we must keep in mind that what they are telling us might not be what is best for them.
V2.3: The Role of Acclimatization
As we have discussed already in the paper, new hearing aid users, and to some extent previous users who have obtained new hearing aids, often have adjustments that they believe are necessary following the initial fitting. It’s important for us to decide if these changes are in the patient’s best interest, as sometimes they are not. Entering into this decision process is the fact that many hearing aid users require a period of time to adjust to new amplification or to changes in amplification; a process often termed auditory adaptation or acclimatization. This adjustment process can be related to the loudness levels of speech, changes in the spectrum of speech, environmental sounds, or other acoustic events. In many instances, a careful balance must be maintained between providing the patient with the appropriate gain and frequency response that will allow acclimatization to occur, but at the same time avoiding hearing aid settings that will discourage the patient from using the hearing aids.
Some Terminology
As reviewed by Mueller and Powers (2001), there are several terms which can be used to describe the auditory perceptual changes a patient might experience following the use of hearing aids. To some extent, the use of a given term might depend on whether we believe that actual brain plasticity is occurring.
Acclimatization. Adapting to a new environment, in this case, auditory. This seems to be a reasonable term, as it is also used to describe how the human body acclimates to temperature, altitude, and other environmental conditions. From an auditory standpoint, Stuart Gatehouse (1992) was one of the first to use the term acclimatization to describe his observation that there was improved speech recognition following hearing aid use. Today, the term is used widely to explain adaptation to hearing aid use in general.
Adaptation. The process of adapting to something, such as environmental conditions (in this case, auditory); the responsive adjustment of a sense organ. This, too, is a reasonable term, and some believe more descriptive of what is happening than calling it acclimatization. It has long been used in reference to the eye—for example, adaptation to varying light conditions.
Adjustment. Making or becoming suitable; adjusting or accommodating to circumstances. This term also describes the process quite well; however, we make so many adjustments to hearing aids that it might be best to avoid this term just to reduce confusion.
Auditory learning. Acquiring new auditory skills or abilities related to perception, cognition, and memory. Although learning does not account for all the factors of hearing aid adaptation, stimulus learning probably is related to some of the acclimatization effects (Robinson & Summerfield, 1996).
So, we have several terms that can be used to describe the patient’s experience of adjusting to sounds processed through hearing aids. The concerns of most clinicians is not so much what we call it, but does it really happen, and how does it impact the need for post-fitting hearing aid adjustments?
Why and How It Happens
Acclimatization refers to a combination of things to which the patient may have trouble adjusting to. These range from low-level ambient noise which is now louder, to louder-than-usual soft sounds, to loud sounds that now sound too loud, to the newly acquired audibility of high-frequency speech signals, to the renewed awareness of environmental sounds that were long forgotten. The underlying mechanisms that allow acclimatization to occur may not be the same for all of these conditions.
In relation to acclimatization associated with the reintroduction of high-frequency signals, we can consider the theory of space allocation (Palmer, 1995). That is, if only a small portion of the speech signal has been present over time, the space allocation for processing this signal in the auditory cortex may have been reduced. If the patient is fitted appropriately and a wide range of speech signals are now present, more space may be allocated for the processing of these new signals. We certainly have electrophysical evidence showing that visual processing can invade the temporal lobe when hearing loss is present—and how the temporal lobe can be reclaimed when appropriate amplification is used (Glick & Sharma, 2020; Sharma, 2021). “Appropriate” meaning real-ear verification of required audibility. There is some evidence that when individuals are under-fit, which is what happens when the manufacturer’s fittiing is used, the temporal lobe will not be reclaimed as efficiently (Sharma, 2021).
Although neurophysiology concepts might not appear to be directly related to the everyday fitting of hearing aids, if, when, and how acclimatization occurs for a given patient does influence our overall hearing aid fitting strategies.
Acclimatization to Loudness
As we discussed earlier, a common complaint among hearing aid users, especially new users, is that sounds are too loud. The question then becomes, if patients are fitted to a validated prescriptive method that has been designed to equalize or normalize loudness, will users acclimatize to these renewed loudness sensations? One study that has examined this used aided loudness scaling via a self-assessment scale. The patients completed the Profile of Aided Loudness (PAL) self-assessment inventory before and after a 30-day trial with the hearing aids. The PAL is a 12-question inventory related to the patient’s loudness perceptions of everyday sounds (four questions each for different soft, average, and loud sounds) (Mueller and Palmer, 1998; Palmer et al, 1999). Using the PAL, two different studies have shown findings that have clinical implications (Mueller and Powers, 2001):
- In the first of these studies, two groups of participants completed the PAL—new users and experienced users. Both groups recently had been fitted with new hearing aids, verified to the NAL prescriptive targets. Their ratings are shown in Figure 5. PAL norms (young normal hearing adults) for soft, average and loud are ~#2, ~#4 and ~#6 respectively. Note that the experienced users rated soft sounds somewhat too loud, but were okay for average and loud. The new hearing aid users also were okay for average and loud, but observe that for soft sounds, the patients rated these listening situations nearly the same as average-level sounds—close to a #4. This suggests that the complaint of “the hearing aids are too loud” is mostly because of the perceptions of soft sounds.
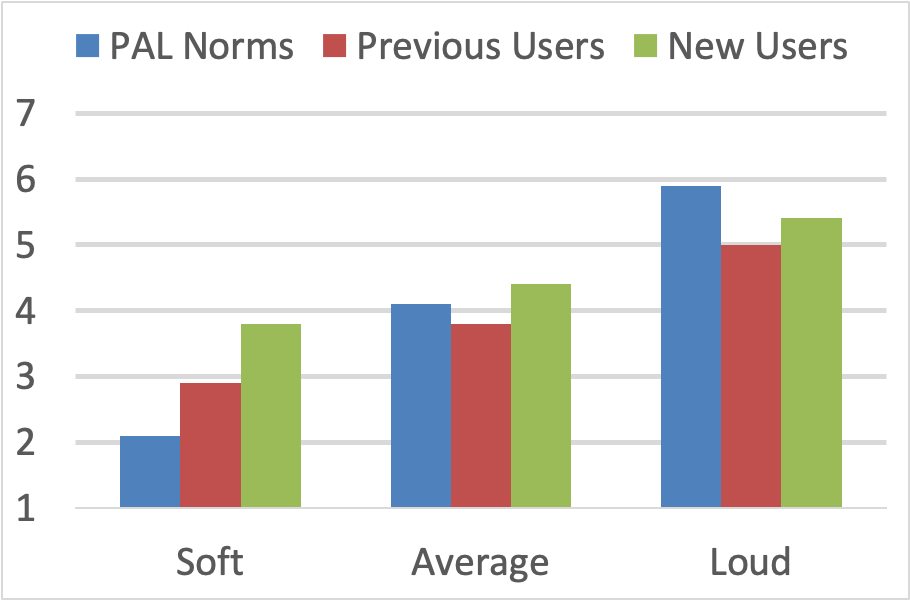
Figure 5. Shown are the mean PAL ratings for environment sounds that normal hearing adults judge to be soft (#2), average (#4) and loud (#6). Ratings shown for new hearing aid users and for experienced users, both fitted bilaterally with new hearing aids (adapted from Mueller and Powers, 2001).
- A second related study examined the potential acclimatization for soft sounds. Again, two groups of hearing aid users were fitted, but in this study they were followed for eight weeks. The results are shown in Figure 6. Note that the experienced group were rating soft sounds appropriately (#2 on 7-point scale) after only one week of hearing aid use. The new users, however, were still rating soft sounds #4 after a month of heaing aid use, but did approach the desired #2 rating at the end of the 8-week trial. Clearly, for soft sounds, at least for this group, the adjustment period is gradual, but importantly, does happen. We therefore, recommend the following adage for all new hearing aid users: YOU HAVE TO HEAR WHAT YOU DON’T WANT TO HEAR TO KNOW WHAT YOU DON’T WANT TO HEAR!
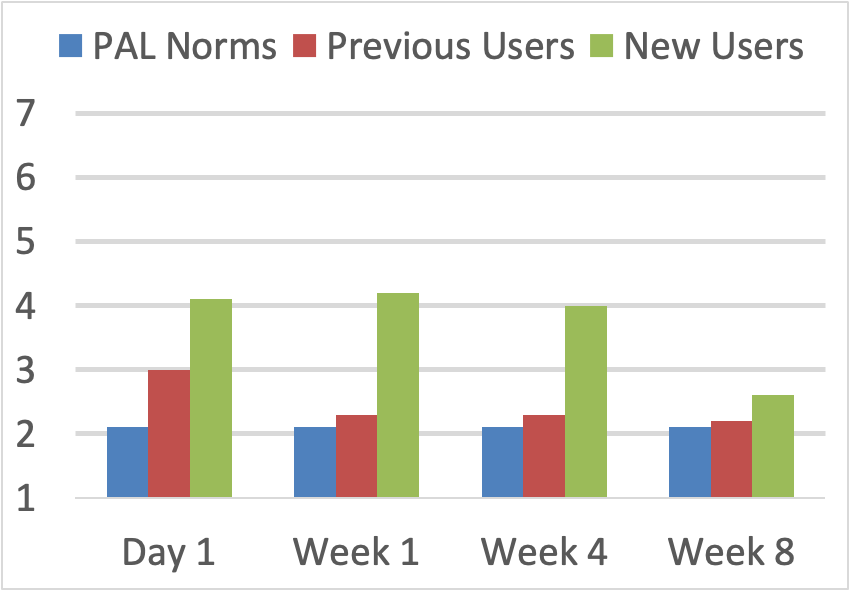
Figure 6. Shown are the mean PAL rating for environmental sounds judged to be soft (#2) by normal hearing young adults. Ratings displayed for both new users and experienced users at Day 1, 1 Week, 4 Weeks and 8 Weeks following the bilateral fitting of new hearing aids.
Effects on Loudness Discomfort Levels
Decades ago, there were some who had the belief that new hearing aid users should go through “tolerance training” so that they could withstand higher hearing aid outputs. To no one’s surprise, this training was not very effective. There is some limited evidence that LDLs might be increased slightly with training, although the amount has been small and simply might be representative of a practice effect of the loudness rating task (Mueller and Powers, 2001)
It of course, is not practical to fit individuals with output that exceeds their LDL, as excessive output is one of the leading causes of hearing aid rejection. Research has shown that when hearing aids are initially programmed so that the maximum output corresponds to the patient’s LDL, the unaided LDL does not appear to increase significantly after prolonged hearing aid use (Bentler et al, 1993; Bratt et al, 2002). Acclimatization for high level outputs, therefore, does not appear to be a major area of concern (unless the hearing aids are initially programmed incorrectly).
Improvements in Speech Understanding
Perhaps the most common “after the fitting” complaint is dissatisfaction regarding the expected improvement understanding speech in background noise. It is not surprising, therefore, that the area of acclimatization which has drawn the most interest surrounds the question if speech recognition improves following hearing aid use. This is something, of course, that both clinicians and patients hope is true. Whether true or not, the concept often is used in counseling for new users who are “on the fence” regarding whether they should return their hearing aids. Some initial studies suggesting that improvement in speech understanding can be expected had design flaws—that is, the use-gain for the participants was not well controlled. It was possible, therefore, that the post-fitting improvement was not related to brain plasticity, but was simply because the patients were using more gain and had more audibility for the speech signal. In recent years, the question of acclimatization leading to improved speech understanding has been studied several times, with mixed results.
In one study, speech recognition in noise was assessed after one week of the fitting, and again 12 weeks post-fitting (Dawes et al, 2014). Participants were new hearing aid users fitted both unilaterally and bilaterally, and a control group of experienced hearing aid users. The results showed a small mean improvement (4%) in speech recognition; however, this improvement also was present for the experienced group, suggesting that it was a practice effect for the speech material. The new users did report significant improvement over time in aided performance compared with the control group.
The same research group later conducted a similar study with somewhat different findings (Dawes et al, 2017). Again, speech recognition in background noise was assessed for a group of new users and a control group of experienced users. At the end of 30 days, a subset of new users with moderate hearing loss who wore their hearing aids at least 6 hr/day had significantly improved speech in noise recognition (~3-dB SNR) compared with the control group. Improvements were associated with more consistent hearing aid use, more severe hearing loss, and self-report of background sounds being less distracting. There was no association between improvements in speech understanding and cognitive ability.
Yet another similar acclimatization study has added support to the improved SNR notion (Wright & Gagne, 2020). In this research, as with the other studies cited, a group of new users and a group of experienced users (controls) were fitted with new hearing aids. Speech recognition in noise and listening effort were assessed on eight different occasions during a 10-month field trial. The new hearing aid users showed improvement over time in speech in noise performances (~2 dB SNR)—this effect was observed following one month of hearing aid use. There was no improvement for the previous users, and no significant change over time for either group for listening effort.
In summary, we have at least two well-designed studies showing that due to acclimatization, an improvement in SNR is possible. There is not a direct relationship between SNR improvement and percent correct, however, for some listening situations, a 2-3 dB SNR improvement could result in 20-30 percent increase in speech understanding. A noticeable difference for many hard of hearing individuals.
V2.4: How Machine Learning Can Help
So at this point, we have several questions. Can we wait for the assistance of acclimatization? What if acclimatization doesn’t happen? Does the patient know what is best for them? Can patients reliably differentiate changes in hearing aid processing? All important questions, but help in dealing with this is available from AI (artificial intelligence) and machine learning.
Some Terminology
To get us started, let’s review three terms related to artificial learning that commonly are used in regard to hearing aid technology:
- Artificial Intelligence (AI) in the simplest terms, refers to systems or machines that mimic human intelligence to perform tasks and can iteratively improve themselves based on the information that they collect. This includes the theory and development of systems that are able to perform tasks such as visual perception, speech recognition, decision-making, and translation between languages. It was in 1952 that Arthur Samuel wrote the first computer learning program. The program dealt with playing the game of checkers. Samuel’s work revealed that an IBM computer improved the more it played, studying which moves made up winning strategies and incorporating those moves into its program. Forty-five years later, the game was chess, and IBM’s Deep Blue beat Garry Kasparov, the world’s champion at the time. And, in 2011, IBM’s Watson beat its human competitors on the popular television game show Jeopardy.
- Machine learning is about extracting knowledge from the data. It is a subfield of artificial intelligence, which enables machines to learn from past data or experiences without being explicitly programmed. Machine learning enables a system, including hearing aids, to make predictions or decisions using historical data without being explicitly programmed. Machine learning usually uses a massive amount of structured and semi-structured data so that a machine learning model can generate accurate results or give predictions based on that data. As more and more data are provided, they are then added to the teaching set and in turn, improves accuracy. In essence, the machine is learning. This could be related to recognizing a photo, a person’s voice, learning how to talk with a human voice, learning to drive a car or . . . learning what hearing aid programming works the best for a difficult listening situation!
- Deep Learning or Deep Neural Network is part of a broader family of machine learning methods based on artificial neural networks with representation learning. The word "deep" refers to the number of layers through which the data is transformed. Deep learning systems have a credit assignment path depth—the chain of transformations from input to output, which describe potentially causal connections between input and output. Deep models are better able to extract features than shallow models, and hence, extra layers help in learning the features effectively. Deep learning helps to disentangle abstractions and pick out which features improve performance. To put it simply, if Amazon or Facebook suggests that you buy something that just happens to be very similar to what you had Googled days earlier, Deep Learning has been used!
Machine Learning in Hearing Aids—Early Success
It’s debatable whether a computer will ever “think” in the same way that the human brain does, but machines’ abilities to see, understand, and interact are changing our lives. It is no surprise, therefore, that today we frequently see mention of AI, machine learning or neural networks when new technology in hearing aids is introduced or promoted. But is this something that has just come about in the last few years? Not really.
Siemens/Signia introduced the first commercially available machine learning hearing aids back in 2006—the Centra Model S.1 These hearing instruments had trainable gain. That is, the hearing aid would “learn” from the user’s VC (or remote control) adjustments what gain was preferred. This training effect did not alter the maximum or minimum gain of the instruments, but rather, the start-up preferred gain when the hearing aids were first turned on. In these instruments, all VC changes were averaged, with greatest emphasis on the most recent changes (the layered neural network learning we discussed earlier). For most users, the optimum target typically was reached after one or two weeks of hearing aid use, with most learning occurring in the first week. Independent gain learning was possible for different memories, so that preferences for listening in quiet, noise, or music, also could be learned.
Research with this first machine learning hearing aid was very favorable (Chalupper & Powers, 2006; Mueller et al, 2008). While individuals typically started with a fit at or near prescriptive targets, the machine learning of the Centra allowed for expected deviations from average and personal preferences to be accounted for. Moreover, this machine learning took place in the user’s daily listening conditions, not in a clinic or office, providing the much-needed real-world effect.
With the revolutionary Centra product, it was possible to train gain, and to conduct this training for different programs/memories—this was referred to as DataLearning. One limitation, however, was that the training was for overall gain. It would be possible that for a given patient, average gain initially was “just right,” but if loud sounds were too loud, the patient might train down overall gain, and as a result, average inputs would then be too soft. This potential limitation was soon corrected, as in 2008 the Siemens/Signia Pure hearing aid was introduced, which had advanced machine learning dubbed SoundLearning—level-dependent gain learning in four independent bands, allowing for the first time, additional learning for frequency shaping (Chalupper et al, 2009).
One of the early studies with this innovative machine learning involved the fitting of over 30 individuals, all new hearing aid users, with hearing aids programmed to the NAL (Palmer, 2012). An interesting finding, was that after 30-60 days of hearing aid learning, the average use-gain for average inputs for the group was essentially identical to what originally was programmed based on the NAL prescription. However, in blinded ratings, 2/3 of the participants favored the “learned” response. Given that the NAL is a fitting for “average,” we would expect that an equal number of the participants were fitted either over or under their preferred listening levels. If the hearing aids learned their preferred settings (more or less gain), it’s probable that the patients would prefer this learned fitting, yet the average gain for the group would stay the same.
A second study using this technology clearly showed how machine learning can not only improve patient satisfaction, but also can lead to potential life-altering improvements (audibility of soft sounds) in the programming of the hearing aids (Mueller & Hornsby, 2014). We briefly mentioned this research earlier, but will include it again here, as it directly relates to machine learning. In this investigation, the machine learning hearing aids were fitted to individuals who were experienced users, but who had been using hearing aids fitted considerably below NAL targets (e.g., ~10 dB for soft speech, ~5 dB for average speech). Following a few weeks of learning, on average, the individuals trained the hearing aids to within 2-3 dB of prescriptive gain for soft, and within 1 dB of prescriptive gain for average, again illustrating the benefits of input-level-specific learning (see “before and after” average output findings in Figure 7). At the conclusion of the learning, nearly ½ of the participants were using 10 dB or more gain for soft inputs than they had been using prior to the use of the new hearing aids.
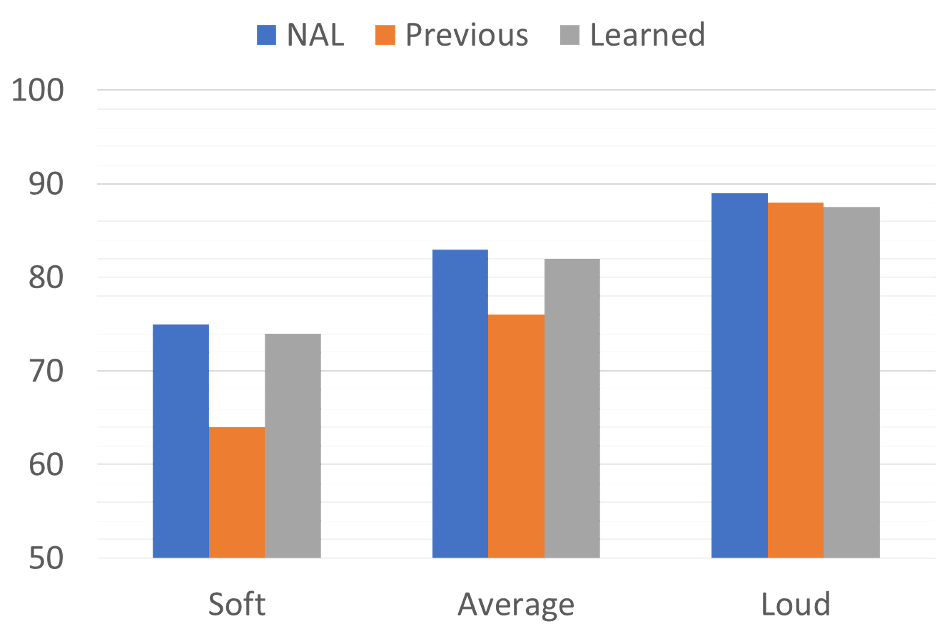
Figure 7. Average output (2000-4000 Hz) for the NAL-NL2 prescription, previous use, and following machine learning, for soft, average and loud inputs. Note that following learning, average output matches that of the desired NAL-NL2 fitting (adapted from Mueller and Hornsby, 2014).
The Advancements Continue
In 2010, the Siemens/Signia machine learning advancement led to the link between compression learning and signal classification. That is, as a given signal was classified into one of six distinct categories, the use gain, or frequency-specific gain adjustments made by the patient automatically generated deep learning within that specific categorization. This learning would then continue automatically whenever that categorization would occur, and all six categories would be trained accordingly. This meant that the user no longer had to change programs to take advantage of the machine learned settings (Mueller, 2014). Considerable research with this learning algorithm was conducted at the Australian National Acoustic Laboratories (Keidser & Alamudi, 2013). Their findings revealed that after a few weeks of hearing aid use, the learning was individualized for each of the six conditions, illustrating differences in preferences for such diverse situations as speech in background noise, listening to music, or communication in a car.
Own Voice Processing (OVP)
To this point, we’ve been talking about machine learning that might not be complete until after a week or two of hearing aid use. In 2017, Signia introduced a new machine learning algorithm that only takes a few seconds (Hoydal, 2017). This unique learning algorithm was labeled own-voice processing (OVP)—but importantly, it’s not just processing, it is also voice recognition. OVP is accomplished by training the hearing aids to recognize the wearer’s voice, which requires about 10 seconds of live speech from the user while wearing the hearing aids. Using bilateral full-audio ear-to-ear communication, the hearing aids “scan” the acoustic path of their own placement relative to the wearer’s mouth. Based on this analysis, the hearing aids are able to detect when speech is coming from the wearer versus his/her surroundings, even if speech is coming from a conversation partner situated directly in front of the wearer. Additionally, if the wearer’s voice changes for some reason, the detection remains precise, because it scans the unique sound propagation pattern as sound travels from the wearer’s mouth to the hearing aid microphones, rather than the frequency characteristics of the wearer’s voice.
Research with this new machine learning algorithm has clearly shown the benefits. Satisfaction with the sound of one’s own voice increases substantially, even when fitted with closed ear canal couplings (Powers et al, 2018). This is true to the extent that when OVP is activated in a Signia device with a closed earmold, own-voice satisfaction is substantially higher than when fitted with a competitor hearing aid using an open-mold. This is displayed in Figure 8.
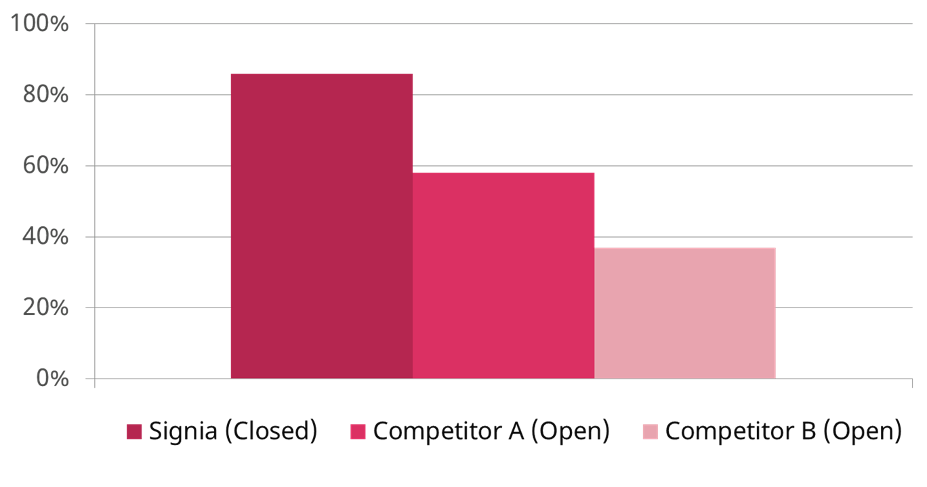
Figure 8. Shown is the percent of participants who were “satisfied” with the sound of their own voice for three different fittings: Signia OVP with closed earmold, Competitor A with open ear tip, and Competitor B with open ear tip. Note that satisfaction with OVP with closed was significantly higher than the competitors with open fittings (adapted from Powers et al, 2018).
In other research with OVP, hearing aid users reported that the sound of their voice also was significantly more natural when OVP is activated (Froehlich et al, 2018). And, perhaps most importantly, when OVP is used, new hearing aid users report that they are more engaged in conversations (Powers et al, 2018). When the COSI was used as the metric, and items related to “more talking” were selected as COSI fitting goals, there was a significant increase, and moreover, this increase in communication was associated with improved quality of life (See Figure 9).
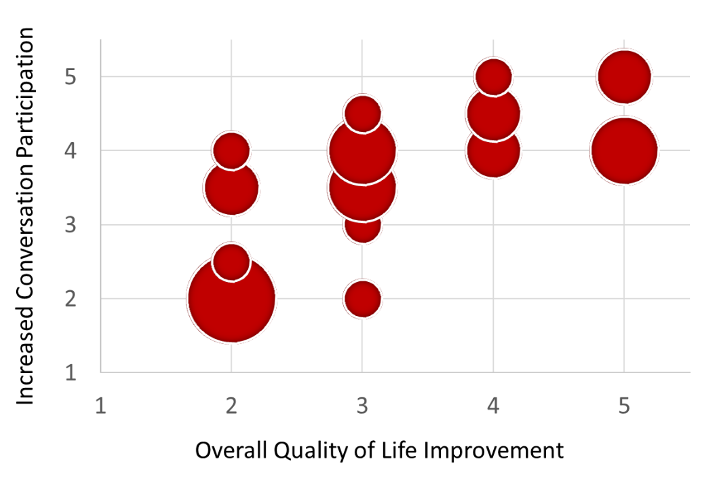
Figure 9. The relationship between COSI improvement (more communication) and overall quality of life following the fitting of hearing aids equipped with OVP (adapted from Powers et al, 2018).
The two decades of Siemens/Signia research described here led to the development of the most sophisticated hearing aid machine learning, the Signia Assistant.
V2.5: The Signia Assistant
In the previous section, we discussed the evolution of machine learning in Signia products, beginning with simple gain training, moving to compression and SoundLearning, to listening situation learning, and then finally, the innovative own voice processing. In 2020 Signia took machine learning one step farther and introduced the Signia assistant.
Neural Network of Signia Assistant
In the development stages, considerable training material was used for the deep neural training of the Signia Assistant (Hoydal & Aubreville, 2020). This included information about the environment (overall level, acoustic classification, etc.), individual hearing loss factors, and known programming alterations that impact speech intelligibility and sound quality. The Assistant was provided with a vast number of examples that mimicked real hearing aid users giving positive or negative feedback to a change provided by the Assistant. Using this development process, when later interacting with the actual patient in the real world, the Assistant already had mastered thousands of “virtual hearing aid users.”
Given the background learning, the Signia Assistant is expected to solve the majority of problems experienced by the user in the days following the fitting. There are individual preferences, however, that vary from the norm. To account for this, the Assistant incorporates previous interactions with the user, and can thereby identify which changes have worked successfully in previous similar listening situations. These personal preferences are taken into account for the next proposed solution. If the first most logical solution is not rated favorably, an alternative choice is provided. If the alternative solution proves to be better over time, and this happens for a large majority of hearing aid wearers, this choice climbs the hierarchy of the neural layers, and becomes more likely to be used by the Signia Assistant in future similar situations. The deep neural learning of the assistant includes data from around the world, and fine adjustments are continually being made (Hoydal & Aubreville, 2020).
Individualization
A common request for improvement expressed by new hearing aid users is to hear their conversation partner better when background noise is present. Changes that could be applied by the Assistant would possibly include increase or decrease in gain, a change in the frequency response, more or less compression, directionality and/or noise reduction. The best solution, however, is highly individual, and might depend on the patient’s hearing loss, the type of noise that is present, the signal-to-noise ratio, the amount of reverberation, the individual’s cognitive capabilities, or his or her sound shape preferences. Furthermore, it is highly dependent on the specific listening situation, which is nearly always, different from the setting where the hearing aids were initially fitted.
The neural network of the Signia Assistant can identify that some hearing aid users have certain characteristics, that increases the likelihood for a certain solution. Factors such as hearing aid experience, certain hearing loss configurations, or sensitivity for noise, all are example of such characteristics. A group of users with a set of common attributes will then potentially be given changes to their hearing aid settings that vary from those that would be given to a different group. An example of how an individual might use the Signia Assistant is shown in Figure 10.
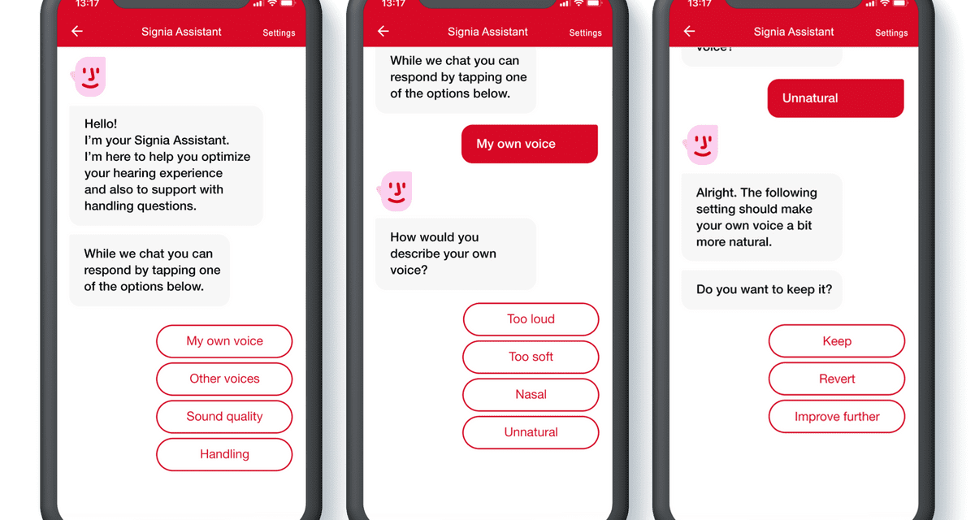
Figure 10. Example of how the Signia Assistant App might be used (progressive screen shots going left to right).
Research Validation
Following the implementation of the Signia assistant, several research questions needed to be answered. Some simply revolved around the usability of the app—could hearing aid users easily make the changes that they desired? From an audiologic standpoint, of course, we wanted to know, do the changes work? And, as we discussed earlier in this article, can we be confident that the solution that the patient “approves” will make changes in the hearing aid performance that are for the best? For example, a patient might prefer a solution with less high frequencies because the sound is “less harsh”, when in fact this solution might reduce, rather than improve their speech understanding in background noise. All of these issues have been addressed in the design of the research studies.
In one of the early studies with the Signia Assistant, a group of individuals were fitted with Signia hearing aids which employed the Signia Assistant and corresponding smartphone app (Hoydal et al, 2020). The hearing aids initially were fitted to the NAL-NL2, and reference aided speech-in-noise testing was conducted. Following the initial lab testing, the participants were instructed on using the app. They then used the hearing aids for two weeks in their everyday real-world settings. They were instructed to use the app on demand in their daily life and were given a list of specific listening situations outside of their home to experience.
Following the home trial, descriptive data (logged by the hearing aids) was collected. Based on the hearing aids’ signal classification system, it was determined that the Signia Assistant was used: 51% in Quiet, 32% in Noise or Speech-In-Noise, 14% in Music, and 3% while in a car. The overall SPL when the Assistant was used was: 34% <55 dB SPL, 36% 55-65 SPL, 19% 65-75 SPL and 9% >75 dB SPL.
To ensure that the changes made using the Assistant did not negatively impact speech understanding, speech testing was conducted following the field trial, and these data were compared to pre-trial results. These findings are shown in Figure 11. Note that the post-trial repeated speech testing for the NAL-NL2 fitting, and the results for the Assistant fitting, are no different than the original results for the NAL fitting. This suggests that at least on average, the testing was reliable, and that changes made by the Assistant did not reduce speech understanding.
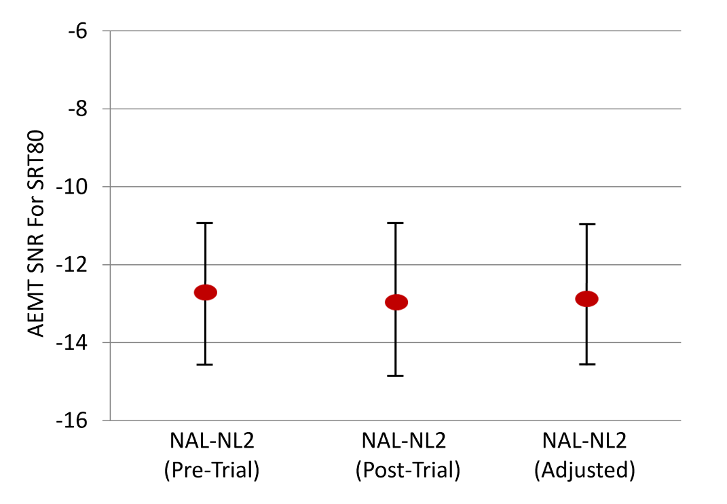
Figure 11. Group mean values for the speech recognition in noise (American English Matrix Test, SRT-80, noise at fixed 65 dB SPL) for the three different test conditions: NAL-NL2 (Pre-Trial), NAL-NL2 (Post-Trial), and NAL-NL2 (Assistant Adjusted). The error bars represent one standard deviation (adapted from Hodal et al, 2020).
In addition to the speech testing, the participants completed follow-up questionnaires and personal interviews to explore the overall benefit of the Assistant (Hoydal et al, 2020). These finding are shown in Figure 12. Observe that all ratings are very positive. Notable are the findings that 86% agreed that the Assistant increased their benefit with hearing aids, and 93% believed that the Assistant increased their satisfaction for difficult situations.
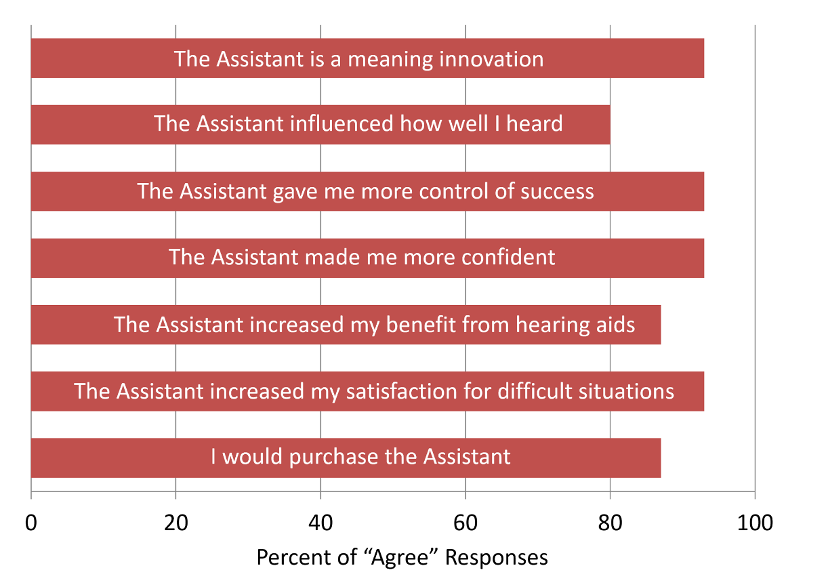
Figure 12. Participant’s ratings for the Questionnaire. Ratings made on a 7-point scale: 1=Strongly Disagree, 4=Neutral, 7=Strongly Agree. Percentages shown are the combined 5, 6 and 7 “agree” ratings (adapted from Hoydal, 2020).
The hearing aid users’ ability to effectively use the assistant also was assessed following the field trial, using a 5-point scale (Strongly Agree to Strongly Disagree). The results were very positive: 80% agreed that they had confidence in the system, >70% agreed that they would like to use it frequently, that it was not too complex, and that it was easy to use. Only 7% believed that it was too complex and difficult to use.
A second real-world study of the Signia Assistant involved a larger group of participants (n=58), and also sampled the views of the HCPs (n=41) who fitted the hearing aids (Hoydal et al, 2021). In general, satisfaction (6-point scale) with the Assistant was similar to previous research (See Figure 13). Agreement for all key items was >70%--importantly, 79% of the participants believed that the use of the Assistant allowed them to achieve the best possible setting for the hearing aid.
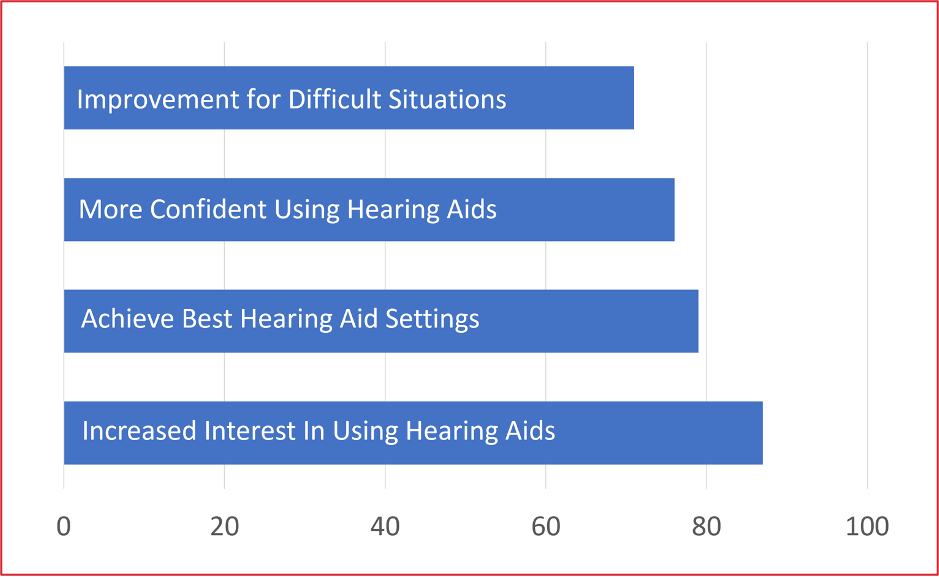
Figure 13. Percent of respondents agreeing (6-point scale) with different statements related to the field-trial use of the Signia Fitting Assistant (adapted from Hoydal et al, 2021).
In general, the Assistant is designed to be an extension of the skills of the HCP, not a replacement. It was important, therefore, to also sample the views of the HCPs who participated in this research. Those findings are shown in Figure 14. The majority of respondents believed that the use of the Assistant helped provide the best fitting, strengthened their professional competency, and perhaps more importantly, improved relationships with the patient.
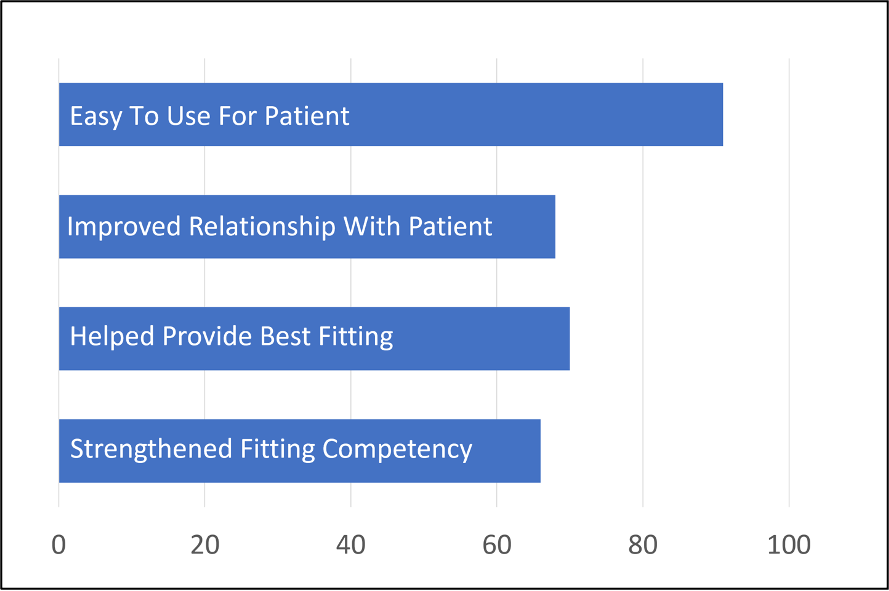
Figure 14. Results from HCPs who worked with the Signia Assistant in a field trial. Shown is percent of respondents who agreed with statements related to the use of the assistant (adapted from Hoydal et al, 2021).
In Closing
In this paper, we have reviewed several post-fitting issues that must be considered, including things like acclimatization, the placebo effect, and the question if we can trust the input we receive from our patient. Machine learning has become common in hearing aids, and the good news is that research clearly shows that the machine learning employed by the Signia Assistant not only results in improved fittings, but also strengthens the bond between the HCP and the patient.
References
Bennett, R., Kosovich, E., Stegeman, E., Ebrahimi-Madiseh, A., Tegg-Quinn, S., & Eikelboom, R. (2020). Investigating the prevalence and impact of device-related problems associated with hearing aid use. International Journal of Audiology, 59(8), 615-623.
Bentler, R. A., Niebuhr, D. P., Getta, J. P., & Anderson, C. V. (1993). Longitudinal study of hearing aid effectiveness: objective measures. Journal of Speech, Language, and Hearing Research, 36, 820–831.
Bentler, R., Niebuhr, D., Johnson, T., & Flamme, G. (2003). Impact of digital labeling on outcome measures. Ear and Hearing, 24(3), 215-224.
Bratt, G. W., Rosenfeld, M. A. L., Poek, B. F., Kang, J., Williams, D. W., & Larson, V. (2002). Coupler and real-ear measurement of hearing aid gain and output in the NIDCD/VA hearing aid clinical trial. Ear and Hearing, 23, 308-324.
Carr, K. (2020). 20Q: Consumer insights on hearing aids, PSAPs, OTC devices, and more from MarkeTrak 10. AudiologyOnline, Article 26648. Retrieved from www.audiologyonline.com
Caswell-Midwinter, B., & Whitmer, W. (2021). The perceptual limitations of troubleshooting hearing-aids based on patients' descriptions. International Journal of Audiology, 60(6), 427-437.
Chalupper, J., & Powers, T. A. (2006). Changing how gain is selected: The benefits of combining datalogging and a learning VC. The Hearing Review, 13(13), 46-55.
Chalupper, J., Junius, D., & Powers, T. (2009). Algorithm lets users train aid to optimize compression, frequency shape, and gain. The Hearing Journal, 62(8), 26-33.
Dawes, P., Hopkins, R., & Munro, K. (2013). Placebo effects in hearing-aid trials are reliable. International Journal of Audiology, 52(7), 472-477.
Dawes, P., Munro, K., Sridhar, K., & Edwards, B. (2014). Auditory acclimatization and hearing aids: Late auditory evoked potentials and speech recognition following unilateral and bilateral amplification. The Journal of the Acoustical Society of America, 135(6), 3560.
Dawes, P., & Munro, K. (2017). Auditory distraction and acclimatization to hearing aids. Ear and Hearing, 38(2), 174-183.
Froehlich, M., Powers, T., Branda, E., & Weber, J. (2018, April). Perception of own voice wearing hearing aids: why "natural" is the new normal. AudiologyOnline, Article 22822. Retrieved from www.audiologyonline.com
Froehlich, M., Branda, E., & Apel, D. (2019). Signia TeleCare Facilitates Improvements in Hearing Aid Fitting Outcomes. AudiologyOnline.
Gatehouse, S. (1992). The time course and magnitude of perceptual acclimatization to frequency responses: evidence from monaural fitting of hearing aids. The Journal of the Acoustical Society of America, 92(3), 1258-1268.
Glick, H. A., & Sharma, A. (2020). Cortical neuroplasticity and cognitive function in early-stage, mild-moderate hearing loss: Evidence of neurocognitive benefit from hearing aid use. Frontiers in Neuroscience, 14.
Humes, L., Rogers, S., Quigley, T., Main, A., Kinney, D., & Herring, C. (2017). The Effects of Service-Delivery Model and Purchase Price on Hearing-Aid Outcomes in Older Adults: A Randomized Double-Blind Placebo-Controlled Clinical Trial. American Journal of Audiology, 26(1), 53-79.
Hickson, L., Meyer, C., Lovelock, K., & Lampert, M. (2014). Factors associated with success with hearing aids in older adults. International Journal of Audiology, 53, Suppl 1, S18-S27.
Høydal, E. H. (2017). A new own voice processing system for optimizing communication. Hearing Review, 24(11), 20-22.
Høydal, E. H., & Aubreville, M. (2020). Signia Assistant backgrounder [whitepaper]. Retrieved from https://www.signia-library.com/wp-content/uploads/sites/137/2020/05/Signia-Assistant_Backgrounder.pdf.
Høydal, E. H., Fischer, R.-L., Wolf, V., Branda, E., & Aubreville, M. (2020). Empowering the wearer: AI-based Signia Assistant allows individualized hearing care. Hearing Review, 27(7), 22-26.
Høydal, E. H., Jensen, N. S., Fischer, R.-L., Haag, S., & Taylor, B. (2021). AI assistant improves both wearer outcomes and clinical efficiency. Hearing Review, 28(11), 24-26.
Jenstad, L., Van Tasel, D., & Ewert, C. (2003). Hearing Aid Troubleshooting Based on Patients' Descriptions. Journal of the American Academy of Audiology, 14(7), 347-360.
Keidser, G., & Alamudi, K. (2013). Real-life efficacy and reliability of training a hearing aid. Ear and Hearing, 34(5), 619-629.
Mueller, H. G. (2014, July). Trainable hearing aids - Friend or foe for the clinician? AudiologyOnline, Article 12774. Retrieved from: https://www.audiologyonline.com
Mueller, H. G., & Palmer, C. V. (1998). The profile of aided loudness: a new "PAL" for '98. The Hearing Journal, 51(1), 10–17.
Mueller, H. G., & Powers, T. (2001). Consideration of Auditory Acclimatization in the Prescriptive Fitting of Hearing Aids. Seminars in Hearing, 22(2), 103-124.
Mueller, H. G., Hornsby, B. W., & Weber, J. E. (2008). Using trainable hearing aids to examine real-world preferred gain. Journal of the American Academy of Audiology, 19(10), 758-773.
Mueller, H. G., & Hornsby, B. W. Y. (2014, July). Trainable hearing aids: the influence of previous use-gain. AudiologyOnline, Article 12764. Retrieved from: https://www.audiologyonline.com
Mueller, H. G., Stangl, E., & Wu, Y.-H. (2021). Comparing MPOs from six different hearing aid manufacturers: Headroom considerations. Hearing Review, 28(4), 10-16.
Palmer, C. V. (1995). Deprivation, acclimatization, adaptation: what do they mean for your hearing aid fittings. Hearing Journal, 48(5), 10, 41–45.
Palmer, C. V., Mueller, H. G., & Moriarty, M. (1999). Profile of aided loudness: a validation procedure. *Hearing Journal, *(6), 34–42.
Palmer, C. V. (2012, August). Implementing a Gain Learning Feature. AudiologyOnline. Retrieved from: https://www.audiologyonline.com
Powers, T., Froehlich, M., Branda, E., & Weber, J. (2018). Clinical study shows significant benefit of own voice processing. Hearing Review, 25(2), 30-34.
Powers, T. A., Davis, B., Apel, D., & Amlani, A. M. (2018). Own voice processing has people talking more. Hearing Review, 25(7), 42-45.
Robinson, K., & Summerfield, Q. (1996). Adult auditory learning and training. Ear and Hearing, 17(Suppl), 51S–65S.
Sabin, A., Van Tasell, D. J., Rabinowitz, B., & Dhar, S. (2020). Validation of a Self-Fitting Method for Over-the-Counter Hearing Aids. Trends in Hearing, 24(2).
Sharma, A. (2021). 20Q: Harnessing neuroplasticity in hearing loss for clinical decision making. AudiologyOnline, Article 27826. Available at www.audiologyonline.com
Wright, D., & Gagné, J. P. (2020). Acclimatization to Hearing Aids by Older Adults. Ear and Hearing, 42(1), 193-205.
Citation
Taylor, B. & Mueller, H. G. (2023). Research QuickTakes Volume 2: identification and management of post-fitting hearing aid issues. AudiologyOnline, Article 28676. Retrieved from https://www.audiologyonline.com