With the proliferation of audiology practices incorporating "balance services" in their practice names and scope of practice, it is incumbent on audiologists to ensure that balance assessment services are comprehensive, and that rehabilitation options are fully explored.
Some practices will pursue opportunities to provide comprehensive balance services. Others may choose to limit their participation to basic preliminary evaluations and then refer patients for complex diagnostics and rehabilitation services to other community resources (balance centers, otolaryngologists, neurologists, physical therapists, etc.).
Regardless, patients are best served when the audiologist recognizes that balance assessment must include site-of-lesion tests, functional impairment measures and rehabilitation protocols.
DIAGNOSIS AND TREATMENT:
Historically, the diagnosis of an individual's balance problem has been based on physical examination and history, and limited "site-of-lesion" tests, designed to localize and confirm the presence of structural and physiological pathology. The "gold standard" components of the site-of-lesion tests include; ENG, ABR, nerve conduction tests, MRI, etc.
The major limitation of these site-of-lesion tests is that they assess structural and physiological changes within individual sensory or motor components in isolation, rather than in the functional context of balance control. Therefore, site-of-lesion test results often correlate poorly with functional impairments and the underlying balance disorder. Simply stated, the correlation between clinical presentation and site-of-lesion test results is variable.
For example, ENG test results may be normal, despite a clinical balance deficit.1, 2 Whether normal or abnormal, ENG results do not predict a patient's balance function, just as a pure tone audiogram does not predict a patient's communication ability in everyday situations.
Effective diagnosis of balance problems requires the documentation of pathology and the functional impairments of balance control. An effective diagnostic test of balance control impairments should objectively differentiate between a number of possible sensory, motor, and central integrative functions in the context of active posture control tasks — not just the structure or function of individual components in isolation.
Computerized Dynamic Posturography (CDP) is the only available diagnostic test of balance control that provides a comprehensive differential diagnosis of sensory, motor, and central integrative functional impairments of balance control. Importantly, the equipment and training necessary to provide CDP evaluation and subsequent diagnosis requires a significant financial investment and it may, therefore, not be appropriate for many private practice settings. However, there are alternative standardized measures that require a much more modest investment in training and equipment.
Preliminary assessment using the modified (computerized) Clinical Test of Sensory Interaction on Balance (mCTSIB) can be effective in identifying individuals with mild or severe balance problems. The mCTSIB is a standardized test, using four different test conditions. The patient stands on a small forceplate, and data regarding their position and postural sway is analyzed by a computer, either as a separate system or sharing the same computer with more current ENG systems. The mCTSIB was designed to provide clinical information similar to the Sensory Organization Test (SOT) protocol of CDP. The mCTSIB has similar sensitivity to the SOT to detect sensory balance impairment, but it lacks the specificity to sort out the underlying components.
The advantages of using the mCTSIB are that it can provide objective data regarding postural control,1, 3 it requires little time to perform and it can be added to a clinical protocol for minimal financial investment. There is an extensive bibliography of research literature on the SOT and the mCTSIB. (see the reference library at www.onbalance.com)
The Limits of Stability (LOS) is an additional brief standardized test of a patient's voluntary motor control of posture. It can be performed with the same forceplate and computer used for the mCTSIB. The LOS provides data about the patient's ability to control voluntarily their postural movement. LOS data have been shown to be predictive for fall risk.4
The test results from the mCTSIB and the LOS can be utilized to target treatment protocols, based on impairments having the greatest impact on daily life activities. Additionally, the mCTSIB and the LOS allow the clinician to monitor treatment progress and functional outcome of a well-organized vestibular rehabilitation protocol.
Effective treatment is clearly related to, and dependent on, the differential diagnosis. If the differential diagnosis is not correct, or is incomplete, a successful and effective treatment protocol is unlikely.
Vestibular rehabilitation is similar to "aural rehabilitation." For example, with aural rehabilitative protocols, the audiologist's role is to improve communication ability for the patient, even though the underlying hearing loss cannot be treated or corrected through medical or surgical means. This too, is the goal of vestibular rehabilitation. The audiologist manages and treats the balance disorder, after medical and surgical options have been ruled out.
Use of postural control information and results provided by the SOT and mCTSIB to diagnose and treat balance disorders substantially improves health outcomes. Recent controlled outcome studies have shown that treatment interventions are most effective when based on results of these postural control tests.5, 6, 7, 8 This complete assessment of postural control provides clinically beneficial information that other available diagnostic tests (e.g., site-of-lesion tests) alone cannot provide.9 In order to provide a truly comprehensive evaluation of balance, audiologists should be involved in the identification and management of balance and dizziness disorders. This opportunity and the need were defined for Audiology Online in the recent article and discussion by Dr. Lewis Nashner, New Opportunities in the Management of the Dizzy, Balance Disordered Patient (Audiology Online, October 2000).
THE ROLE OF THE AUDIOLOGIST:
The methodology employed in the management of patients with complaints of dizziness and/or balance disorders has evolved from the need for site-of-lesion test information only (ENG, ABR, MRI, etc.), to include the postural control component (CDP, mCTSIB, LOS).
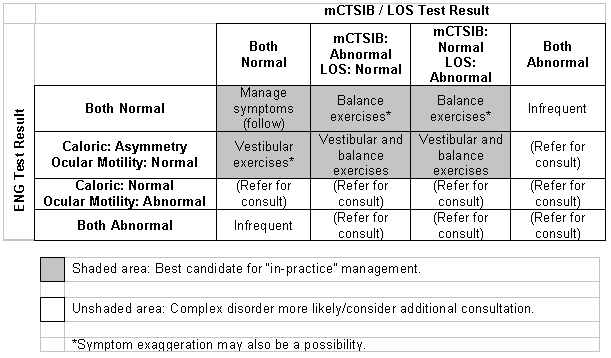
Diagnostic test results enable a physician to answer several questions, including the presence of an acute lesion and the state of patient compensation. By incorporating results from the patient's history and examination, ENG results, and postural control information, the clinician can quickly and effectively identify those patients that can be effectively rehabilitated in the office. This same comprehensive approach (Table 1) objectively identifies patients with more complex problems, which may warrant referral to a balance center, or to a physical therapy program. Test results and the clinical decision matrix (Table 1) will help define the appropriate recommendations for most patients.
Table 1. Clinical Decision Matrix
Scope of Practice Issues:
Balance assessment has been established as within the scope of practice of the audiologist. ASHA's Scope of Practice (see "additional references" below) states "...audiologists provide comprehensive diagnostic and rehabilitative services for all areas of auditory, vestibular and related disorders." The AAA Scope of Practice (see "additional references" below) states audiologists are "...uniquely qualified to provide a comprehensive array of professional services related to the assessment and habilitation/rehabilitation of persons with auditory and vestibular impairments..."
Additionally, it is important to note that balance assessment is reimbursed when performed by a qualified audiologist as a diagnostic evaluation.10
In the same way that other professionals limit their practices to their own personal areas of expertise, the audiologist involved in balance assessment and treatment must also practice within their fund of knowledge. Personal scope of practice limitations may exist when the clinician has not obtained specific post-graduate continuing education, or has not had the appropriate academic and clinical background to perform vestibular assessment and rehabilitation11
The personal scope of practice of each audiologist will define how recommended diagnostic testing and vestibular rehabilitation services will be made available. If additional medical evaluations, vestibular or balance rehabilitation services are not available within an individual practice, the patient can be referred to other resources within the community.
If your practice does not provide additional rehabilitation services, your patients will need to know where those services can be obtained in their community. It is very important to establish referral relationships with qualified rehabilitation clinicians who possess appropriate clinical certification and are amenable to quantified assessment and intervention methods.
If you employ only a preliminary evaluation of postural control (the mCTSIB and LOS) within your practice, it is essential to establish a referral relationship with a comprehensive balance center for additional diagnostic and rehabilitative support. For example, Computerized Dynamic Posturography (CDP) would be indicated when a patient has poor results on the mCTSIB, when the chief complaint is unsteadiness/falling, or involves a medico-legal, workmen's compensation or disability determination.
The suspicion of multi-system involvement requires additional information provided by CDP to determine the relative contribution of each deficit to the patient's symptoms.9 Although the sensitivity to identify balance problems is similar for both SOT and mCTSIB, the SOT has the specificity to sort out the components of more severe balance problems.
CONCLUSION:
The acceptance and growth of balance assessment and vestibular rehabilitation as an integral component of the audiologist's scope of practice and area of expertise, represents a new and significant opportunity.
With the ever-increasing growth of our mature population, balance assessment and treatment represents new opportunities for effective diagnosis and treatment, and new professional responsibilities. The audiologist is well positioned to provide cost-effective clinical protocols to minimize the impact of pathology and maximize the patient's functional outcome as related to balance disorders.
References:
- Shepard NT, Telian SA (1996). Practical Management of the Balance Disorder Patient. San Diego, CA: Singular Publishing Group, Inc., 221pp.
- Stockwell CW (2000). Incidence of ENG abnormalities. Insights in Practice. ICS Medical Corporation. May, 2000.
- El-Kashlan HK, Shepard NT, Asher A, Smith-Wheelock M, Telian SA (1988). Evaluation of clinical measures of equilibrium. Laryngoscope 108: 311-319.
- Rose DJ, McKillop J (1998). "Assessment of balance and mobility functions: a reference study based on the Balance Master 6.0." NeuroCom International, Inc.
- Calder JH, Jacobson GP (2000). Acquired bilateral peripheral vestibular system impairment: Rehabilitative options and potential outcomes. J Am Acad Audiol 11: 514-521.
- Black FO, Angel CR, Pesznecker SC, Gianna C (2000). Outcome analysis of individualized vestibular rehabilitation protocols. The American Journal of Otology 21: 543-551.
- Stewart MG, Chen AY, Wyatt R, Favrot S, Beinart S, Coker NJ, Jenkins HA (1999) Cost-effectiveness of the diagnostic evaluation of vertigo. The Laryngoscope 108: 600- 605.
- Rose DJ, Clark S (2000). Can the control of bodily orientation be significantly improved in a group of older adults with a history of falls? JAGS 48: 275-282.
- Boismier T (2001). ENG and Beyond. Advance for Audiologists, March 2001.
- Medicare Transmittal B-01-34, April 30, 2001.
- Monsell EM, et al. (1997). Technology Assessment: Computerized Dynamic Platform Posturography. Otolaryngology-Head and Neck Surgery, ("AAO-HNS Tech Assessment") Vol. 117, No. 4, p. 395.
Additional References:
AAA Position Statements. "Audiology: Scope of Practice." See: https://www.audiology.org/Pages/default.aspx
ASHA "Scope of Practice in Audiology." ASHA Ad Hoc Committee on Scope of Practice in Audiology. https://professional.asha.org/library/scope_aud.htm.
Cohen H, Blatchly CA, Gombash LL (1993). "A study of the clinical test of sensory interaction and balance." Physical Therapy 73: 346-354.
Hageman PA, Leibowitz JM, Blanke D (1995). "Age and gender effects on postural control measures." Arch Phys Med Rehabil 76: 961-965.
Shumway-Cook A, Horak FB (1986). "Assessing the influence of sensory interaction on balance." Physical Therapy 66: 1548-1550.
Topp R, Mikesky A, Thompson K (1998). "Determinants of four functional tasks among older adults: an exploratory regression analysis." J Orthopedic Sports Physical Therapy 27: 144-153.
Weber PC, Cass SP (1993). "Clinical assessment of postural stability." Amer J Otology 14: 566-569.