Editor's note: This text-based course is a transcript of the webinar, Clinician's Guide to Misophonia, presented by Jenna M. Pellicori, AuD, CCC-A.
Learning Outcomes
After this course learners will be able to:
- Identify associated risk factors, pathophysiology, and characteristics consistent with a clinical diagnosis of misophonia.
- Differentiate between other decreased sound tolerance and psychoacoustic disorders such as hyperacusis, phonophobia, recruitment, tinnitus, and central auditory processing disorder.
- Determine clinically significant misophonia based on qualitative/quantitative characteristics and assessment measures.
Introduction
I want to thank you all for taking the time to be here for the discussion on misophonia. I hope you all enjoy today's presentation and take something meaningful away from the course content.
What is Misophonia?
The term misophonia was derived from the Greek root words miso and phon, which translated to hatred of sound. The term was first coined in 2001 to differentiate misophonia from other decreased sound tolerance disorders that they saw clinically. You may also hear the condition less commonly referred to as Selective Sound Sensitivity Syndrome (Johnson, 1999). In general, misophonia is best described as a neurophysiological and behavioral condition characterized by an immediate adverse physical and emotional response to specific repetitive pattern-based sounds regardless of their loudness, which ultimately leads to maladaptive behaviors and nervous system arousal.
According to a study, the most commonly reported age of onset is approximately 12 years old (Kumar, 2016). However, cases have been identified throughout the lifespan raging from five years old into late adulthood. We also know the condition can lead to several psychosocial implications like anxiety, depression, social isolation, and reduced quality of life as well.
Auditory & Visual Triggers
In regards to terminology, patients commonly refer to the repetitive stimuli that elicit an adverse response as triggers. Auditory and visual triggers are both common, although auditory triggers typically occur first, with visual triggers developing over time. Auditory triggers are often soft repetitive pattern-based sounds produced in the context of typical everyday behavior, which is often very difficult to avoid, like chewing or keyboard typing and breathing. They're often human-generated sounds. However, occasionally, individuals have also reported triggers towards animals and mechanical noises. Each individual with misophonia typically has their own unique set of triggers, and the meaning, context, and interpretation of the behavior will often influence the response. For instance, your mother's chewing may be a trigger, but your sister's trigger may not. One of the mysteries of misophonia is that people seem to be more commonly triggered by individuals that they maintain close relationships with, like family members and spouses and close friends. In regards to visual triggers, researchers had proposed the term misokinesia, which translates to hatred of movement and is used to describe repetitive visual stimuli like hand tapping and leg swinging, which results in that averse, an adverse response (Schröder, Vulink, and Denys, 2013). In 2015, Dozier had surveyed participants with visual triggers and noted that open mouth chewing was the most common visual trigger cue reported amongst participants. It's important to note that visual triggers are often paired with auditory triggers, meaning visions that occur immediately before, during, or following an aversive auditory stimulus are most common. If the sound of chewing is an auditory trigger for someone, then the sight of the jaw movement associated with chewing may become a visual trigger. As an example, in a crowded room where the auditory component could be completely inaudible, the sight of jaw movement alone or food entering the mouth may elicit the misophonic response. Some research has questioned whether misokinesia is its independent condition or if it's possibly a variation of misophonia, but more research is still needed to further define this.
Auditory Brain & Nervous System
As audiologists, we are experts in the auditory system. We know that vibrations are collected at the level of the pinna and transmitted via mechanical energy through the middle ear space, which is then converted into electrical energy in the inner ear and travels along the eighth cranial nerve to the brain. Once the signal arrives at the brain, now unconscious brain centers work to assign meaning to sounds by filtering out relevant sounds like speech from noise.
Non-salient. The system also works to differentiate between threatening and non-threatening stimuli as well. If a sound is not meaningful or doesn't represent a threat, it's typically referred to as non-salient, and a healthy auditory system will subconsciously filter it to the background and react with less intensity, which is a process known as auditory gating. With that said, some researchers have proposed that there is a lack of auditory gating in patients with misophonia, meaning that they have difficulty inhibiting responsitivity to meaningless repetitive stimuli. Instead, the response continues to intensify or increase.
Salient. On the other hand, if the brain perceives the sound as meaningful or salient, then our attention will be drawn towards that stimulus. If this stimulus is perceived as threatening, which is commonly the case with misophonia, then our survival mechanisms will kick in via the sympathetic nervous system, which we also know as the fight or flight response.
The fight or flight response is essentially an acute stress response set off by the emotional processing centers of the brain as a defense mechanism. This stress response, in turn, results in a conditioned physical and emotional reflex response, which are outside of the individual's control and cause several physiological changes like flushing, sweating, and increased heart rate. I once had a patient tell me that they brought an extra shirt with them to school every single day because, throughout the day, when they were exposed to different types of triggers, they would sweat profusely. They ended up having some adaptive mechanisms and trying to accommodate for those triggers by having the extra shirt to help out there.
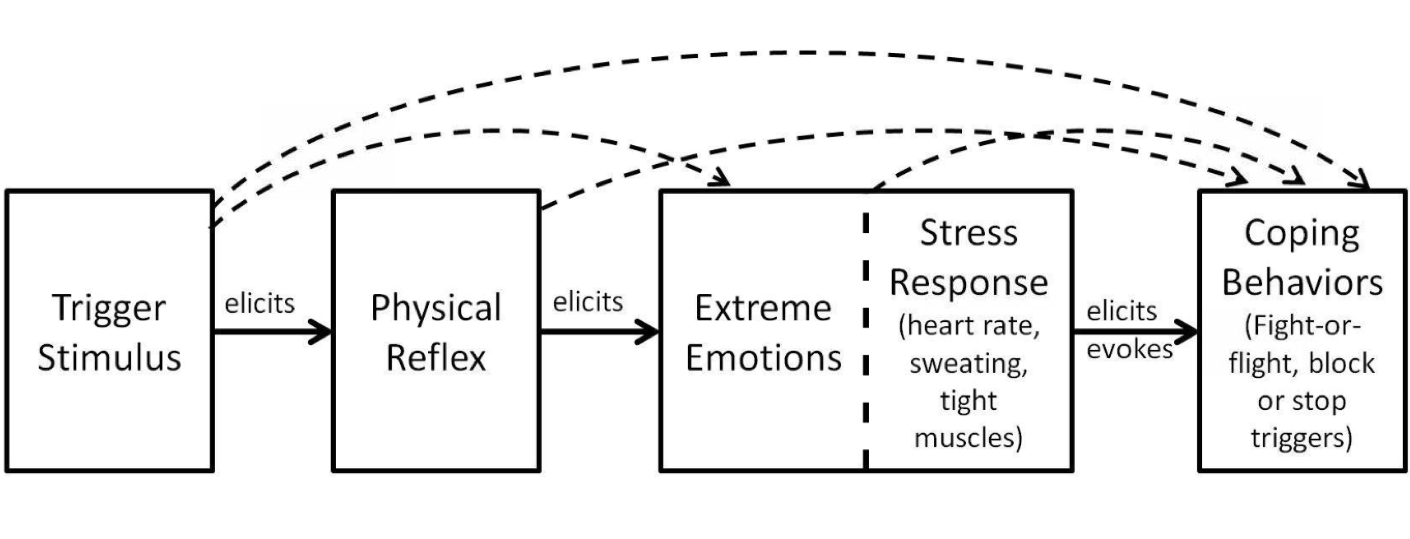
Figure 1. Hypothetical Misophonic Response Chain by Tom Dozier, 2015.
Outlined in Figure 1 is a schematic that illustrates the hypothetical misophonic response chain. The horizontal lines are meant to indicate causation, and the potential for more complex interactions is demonstrated by the arch data binds. The response chain begins with exposure to a specific auditory or visual stimulus, eliciting an aversive conditioned physical reflex response, including muscle tension. Which then fosters an immediate overemotional response, including feelings of anger and disgust or rage.
The physical reflex and extreme emotional responses, in turn, result in physiological changes via the sympathetic nervous system as part of the stress response that we discussed earlier, causing symptoms like elevated blood pressure, pressure in the chest, and sweating, which often leads to maladaptive behaviors like fleeing from the environment and verbal aggression.
Literature Review
Now that we have a basic understanding of the misophonic response chain, I'd like to transition to a brief literature review so we can continue to get a more in-depth understanding of some of the implications of misophonia.
Misophonia: Physiological Investigations and Case Descriptions (Edelstein et al., 2013)
Edelstein and associates were the first to study psychophysiological measurements in patients with misophonia. They measured sweat production using skin conductance responses to indicate physiological arousal and sympathetic nervous system reactivity towards specific auditory and visual stimuli. They had found that subjective aversive ratings and skin conductance responses were both elevated in response to auditory-only stimuli in the misophonic group versus the control group. They did not observe any difference between groups towards visual-only stimuli. Interestingly, the authors also found that patients with misophonia were unaffected when trigger cues were self-produced and confirmed that most triggers were related to other people's behavior. They also documented several common coping mechanisms, including mimicry, avoidance, self-distraction, positive internal dialog, and verbal request to stop the behavior.
A Large-Scale Study of Misophonia (Rouw & Erfanian, 2017)
In 2017, Rouw and Erfanian published a large-scale study that surveyed over 300 online participants with culturally diverse backgrounds, including up to 36 different nationalities. They used subjective self-assessment rating scales to determine how common physical sensations and physiological responses were amongst those with misophonia. They noted the three most commonly reported physical reactions included clenched or tightened muscles, increased body temperature, blood pressure, and heart rate, and perception of increased pressure within the body. Other physical sensations were also reported throughout the literature, but to a much lesser extent, like sweaty palms and difficulty breathing. Interestingly, the participants noticed that triggers were worse when they were tired and improved when they were able to locate the sound source. Unfortunately, as many as one-fifth of the participants reported suicidal thoughts, highlighting the emotional vulnerability of this population.
The authors also evaluated how trigger sounds affected quality of life, with 88% reporting avoiding others, 87% noting difficulty with attention, and 74% commenting that they felt hyper-focused on the noise that should have otherwise been filtered to the background. In regards to the symptom progression, 77% indicated that their symptoms became progressively worse since the time of onset. Participants were also asked if any family members displayed similar symptoms or behaviors. Almost a quarter or 22% specified that yes, indeed, they did. An interesting case study was published in the Brazilian Journal of Otorhinolaryngology in 2018, which documented a family with 15 members across three generations, ranging in age from nine years old to 73 years old, that were identified as having behaviors and symptoms consistent with the diagnosis of misophonia as well.
Furthermore, the authors inquired about coexisting conditions. The most commonly reported conditions included anxiety-related disorders, which co-occurred at a 13% prevalence, in addition to tinnitus, post-traumatic stress disorder, and attention deficit hyperactivity disorder, which each had a 12% co-occurrence. Then lastly, I wanted to mention that the authors documented that 50% of patients with misophonia also noted that certain specific sounds occasionally evoked pleasurable feelings and sensations, which likely describes an experience known as ASMR, which we're gonna touch on here in a moment.
Autonomous sensory meridian response (ASMR). I wanted to include some brief information on the autonomous sensory meridian response, also known as ASMR. Because contrary to misophonia, those with ASMR experience feelings of deep relaxation and euphoria to specific sensory stimuli, often of the auditory modality. You may have even seen or heard of ASMR clips trending online with individuals recording themselves eating pickles or whispering into highly sensitive microphones in hopes of eliciting a relaxive and positive experience, which is sometimes accompanied by tingling sensations throughout the body.
So in 2016, Craig Richard had presented some preliminary data, which showed women were more likely than men to experience ASMR and that participants most commonly reported feelings of relaxation, calming effects, and induced sleepiness in response to sensory provoking stimuli. Another study in 2018 used fMRI to evaluate patients with ASMR versus controls and revealed functional brain changes within the population (Lochte et al., 2018). Differences were observed in three primary brain areas responsible for emotional arousal, processing rewards, and reinforcing positive stimuli. We will touch on brain changes in those with misophonia as well. But before we do, I wanted to mention that some researchers and clinicians have proposed the idea of a spectrum-like disorder from an audio physiological standpoint, where those without any extreme reactions to sound fall somewhere in the middle. Then those with ASMR and misophonia could fall into separate and distinct ends of the spectrum. The strange thing about ASMR is that many of the same sounds that are considered soothing and satisfying have the complete opposite effect in those with misophonia, resulting in feelings of anxiety and anger.
The Brain Basis of Misophonia (Kumar, 2017)
In 2017, Kumar had published a groundbreaking study highlighting that misophonia is an organic brain-based disorder. The research supported increased autonomic nervous system arousal and physiological responsitivity, as well as demonstrated functional brain differences in patients with misophonia. Kumar found increased activation of the anterior insular and abnormal functional connectivity within the ventromedial prefrontal cortex, posterior medial cortex, and several brain regions involved in emotional processing and regulation. The increased activation of the bilateral anterior insular cortexes was a key finding because it's considered a core hub of the salience network, which is responsible for interoceptive awareness and emotional and attentional processing, where we subconsciously differentiate between threatening and non-threatening or relevant and non-relevant stimuli. He hypothesized that individuals with misophonia misinterpret and assign higher salience or meaning to trigger cues that control. Also, greater myelination of gray matter was observed in the ventromedial prefrontal cortex, which is a brain area that plays a key role in processing and regulating emotions like fear, empathy, and rapid decision making. It's also a core hub of the default mode network, which is involved in the retrieval of memories and associative learning and influences several other brain areas responsible for emotional regulation like the amygdala, which processes threat detection. The study ultimately concluded that aberrant functional connectivity results in an altered perception of body state awareness and abnormal salience assignment towards certain sounds, which causes patients to misinterpret trigger sounds in a way that they perceive as threatening or toxic.
Diminished N1 Auditory Evoked Potentials to Oddball Stimuli in Misophonia Patients (Schroder et al., 2014)
In 2014, Schroder and colleagues conducted the first neurobiological study using auditory evoked potentials to explore the involvement of the early auditory processing system in patients with misophonia. They used auditory evoked potentials being an oddball paradigm to assess the integrity of the central auditory nervous system, meaning that participants actively listened to repetitive auditory stimuli with randomly occurring rare oddball deviant tunes interjected throughout the assessment. The authors found a smaller amplitude for the recorded and N1 neural generator marker in patients with misophonia versus health controls, but no significant differences were observed for the P1 and P2 components.
N1 primarily represents the patient's subattentive ability to detect a change, which allows us to reflexively alter our focus towards more relevant auditory information. Ultimately, the study suggested the possibility of a basic impairment in auditory processing and auditory attention abilities amongst those with misophonia. Although further research is required to rule out some confounding variables as it relates to mood and psychiatric conditions, the author suggested that this finding may lead to a possible neurophysiological marker for identifying the condition later on.
Misophonia is Associated with Altered Brain Activity in the Auditory Cortex and Salience Network (Schroder et al., 2019)
Schroder and colleagues also conducted a study with the intent to measure neural, physiological, and behavioral responses to auditory and visual stimuli in patients with misophonia versus controls. They had presented three conditions during functional magnetic resonance imaging, including video clips with misophonic cues, violent or disgusting cues, and neutral cues. They did this while using electrocardiography to monitor physiological changes and also implemented self-assessment measures to monitor emotional responsitivity as well. The findings revealed that both auditory and visual stimuli were responsible for eliciting over emotions and physiological arousal, like increased heart rate or rage in misophonics. The responses also appeared to be associated with the increased activation of the auditory cortex and salience network. Again, the salience network surveys and detects which sensory stimuli are relevant and deserving of our attention.
Also, they observed hyperactivity within the right superior temporal cortex, which plays a key role in auditory attention and processing emotionally salient auditory stimuli. The authors also reported that, while disgusting or offending video clips were deemed offensive by both groups, which is what we would expect, the misophonic video cues were only judged aversive by the misophonic group. They summarized their findings by noting that misophonic cues provoked adverse emotions and physiological arousal and that repeated exposure to the same cues over time likely amplifies the emotional salience network where our brain differentiates between emotionally relevant and irrelevant stimuli to permit for an adequate behavioral response. The authors also noted that this process likely reflects a conditioned response where initially neural stimuli become increasingly intensified and aversive, causing hypervigilance. This is further evidenced by the sensitization of the auditory cortex.
Misophonia Diagnostic Criteria for New Psychiatric Disorder (Schroder & Vulnick, 2013)
Lastly, in 2013, Schroder and colleagues proposed the first diagnostic criteria for misophonia with the intent to classify the condition as an independent psychiatric disorder. Over the years, there are many authors who have suggested revisions and requested clarifications to the content. Diagnostic criteria consist of six requirements, including the presence or anticipation of a human-generated sound, which elicits an adverse emotional and physical response, beginning with irritation or disgust and instantly turning to anger. The authors also noted that common trigger stimuli were assessed, and the top three responses have included 81% triggered by eating sounds, 64% by loud breathing or nasal sounds, and 60% by finger or hand sounds like pen clicking or keyboard tapping.
The second criterion was that the emotional response provokes an immense sense of loss of self-control with potentially aggressive outbursts. The third was that the individual was aware that the emotional response and disgust were disproportionate, unreasonable, and deemed excessive. The fourth document attempts to avoid triggers. If unable to do so, then the individual may experience intense discomfort, anger, or disgust. The fifth criteria suggested that the emotional response and avoidance tendencies caused significant interference and distress to daily living when forced to interact with others. The last specified criteria were that the person's reaction was not better explained by an alternative medical or psychological condition, like obsessive-compulsive disorder or post-traumatic stress disorder. It should be noted that, unfortunately, these diagnostic criteria have not been widely implemented or universally accepted to date. As I said, there are many authors who have suggested revisions and clarifications. To the best of my knowledge, from a content perspective, this is the only diagnostic criteria that have been proposed.
Auditory Conditions and Differential Diagnosis
I cannot stress enough the importance of a team-based approach in assessing and managing patients with misophonia. Because there are no validated assessment measures or biomarkers available for diagnosing the condition, it's primarily a diagnosis of exclusion at this time. Meaning it's important for providers to collaborate and work together to ensure proper differential diagnosis and effective management. From an audiologic perspective, we are going to discuss differentiating misophonia from alternative based conditions, including decreased sound tolerance disorders like hyperacusis, phonophobia, and recruitment.
Audiologic differential diagnosis:
- Decreased Sound Tolerance Disorders (DST)
- Misophonia
- Hyperacusis
- Phonophobia
- Recruitment
- Tinnitus
- Central Auditory Processing Disorder (CAPD)
- Sound Intolerance
Hyperacusis
Hyperacusis refers to an abnormally reduced tolerance to ordinary environmental sounds, like fire alarms or vacuum cleaners, where sounds that would not typically be considered unbearably loud are perceived as painful. In 2014, Jastreboff had described hyperacusis as a subconscious mediated response, which is the result of changes within the auditory system secondary to increased gain.
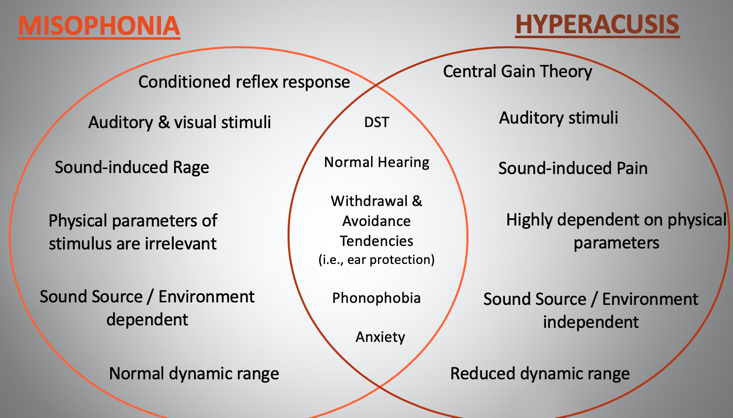
Figure 2. Differential diagnosis between misophonia and hyperacusis.
In Figure 2, we could make some direct comparisons between the two conditions. In regards to differences, misophonia is best categorically classified as a neurophysiological and behavioral condition with a conditioned reflex response. In contrast, hyperacusis is an auditory based condition related to central gain changes within the auditory system. Furthermore, hyperacusis is typically limited to auditory stimuli. However, misophonia, the offending stimulus may be auditory and visual, or much more rarely may even occasionally affect other senses as well. The physical and emotional responses also differ. We know misophonia often elicits anger, disgust, anxiety, and rage, and physiological arousal, like sweating and increased heart rate, as part of that sympathetic nervous system response. Whereas hyperacusis is usually accompanied by aural fullness, ringing in the ears, and pain and discomfort. In regards to physical parameters, in misophonia, offending stimuli are typically human-generated repetitive pattern-based sounds regardless of loudness, whereas, with hyperacusis, stimuli are typically produced by inanimate objects, like fire alarms and toilets flushing, and are highly dependent on the physical parameters of the sound like the timbre, amplitude, or spectrum. We also know that the context and environment affect the misophonic response, meaning you may be triggered by your father's sniffling but not your mother's. Whereas with hyperacusis, the patient is expected to respond identically in all scenarios once the physical parameters of the stimulus have been met. Where, for example, the sound has reached a certain intensity or threshold.
Loudness discomfort levels can also be extremely helpful in differentiating between the conditions. LDLs indicate the intensity level, which a patient reports to be uncomfortably loud. While norms differ in the literature, generally speaking, normal LDL are typically referenced around 90 dB or greater. When testing is positive for a diagnosis of hyperacusis, LDLs and the dynamic range are typically reduced. However, in patients with misophonia, LDLs, and the dynamic range are expected to be normal unless the two conditions are co-occurring.
Finally, although misophonia and hyperacusis are independent conditions, they do share some overlap. For instance, both conditions fall under the umbrella term of decreased sound tolerance disorders and may result in psychosocial implications and maladaptive behaviors like anxiety and withdrawing from activities in an attempt to avoid specific sounds. In addition, neither condition appears to have a direct correlation with peripheral hearing damage. Lastly, I wanted to mention an interesting finding from Emory Tinnitus and Hyperacusis Center from 2013, which found that, out of approximately 200 patients with decreased sound tolerance disorders, approximately 28% of those participants had a comorbid diagnosis of misophonia and hyperacusis, suggesting that the two conditions may frequently coexist.
Phonophobia
Next, I want to touch on the psychological condition known as phonophobia, which is often a consequence of decreased sound tolerance disorders like hyperacusis and misophonia. The word phonophobia originates from the Greek words for sound and fear and is often used to describe a negative reaction towards the sound in general, which results in feelings of fear and anxiety. Even the anticipation of the auditory stimulus can elicit emotional and physiological arousal due to the anxiety that the thought of the sound provokes. Similar to misophonia, phonophobia does not appear to be the direct result of abnormalities within the peripheral auditory system. However, the limbic system does seem to play a role in the patient's response and reaction. As an example, someone who served in the military and was surrounded by explosions may automatically perceive a loud bang as a threat when they return home, which in turn activates the limbic system and fosters feelings of fear and anxiety due to the association with the sound. It's not necessarily the acoustics or sound source itself that elicits the response, but often, it's the recollection of the sound source and the patient's psychological state that influences how they respond with phonophobia. Similar to misophonia, phonophobia can also cause withdrawn avoidance tendencies and maladaptive behaviors as well.
What I want you to take away is that phonophobia is the generalized fear of sounds regardless of the intensity level or pattern of the sound, whereas misophonia is the hatred towards specific pattern-based sounds. Neither condition has been described as a primarily auditory-based disorder. However, enhanced connections between the auditory system and limbic system are thought to play a critical role in the response that both of the conditions elicit given their close proximity.
Recruitment
We know that hearing loss is a typical part of the aging process. As patients age, we are more prone to peripheral damage to the cochlea. It wouldn't be unreasonable then to assume that naturally, over time, as a patient with misophonia ages, they may acquire some degree of hearing impairment as well. With that said, the typical onset of misophonia, which we discussed earlier, is in early adolescence. Although research is limited, most studies and clinical evaluations have revealed normal peripheral hearing in this population. While the two conditions may coexist, there doesn't appear to be any direct correlation between peripheral hearing loss and misophonia.
With that in mind, many of us are aware that a common consequence of hearing loss is recruitment, which is another decreased sound tolerance condition. Recruitment is a phenomenon that typically arises from damage in the inner ear organ of hearing and ultimately leads to a reduced tolerance of loud sounds due to a smaller dynamic range of hearing. Meaning the range from the softest sound that someone is able to hear to the loudest sound that someone is able to tolerate shrinks. This causes the patient's perception of sound to be exaggerated despite very small changes in the amplitude. One explanation for this is in regions where the hearing is normal, healthy cochlear hair cells which are still in the inner era are basically recruited to take over the job of the damaged hair cells in the region where the hearing loss is present. When normal hair cells in that nearby area or critical band take over the job of these damages hair cells, this causes an abnormal growth perception of loudness.
Nonetheless, as part of the diagnostic process, it highlights the importance of differentiating between the two conditions. One key way we can ultimately do this is through case history reports and routine audiologic evaluations, including pure-tone ear testing and loudness discomfort levels.
Tinnitus
Tinnitus, on the other hand, refers to a ringing. A phantom perception of sound in the absence of an external sound source. Many researchers believe that tinnitus is the reaction of the auditory brain trying to compensate for damage originating in the inner ear or auditory pathway, resulting in a phantom perception. As we mentioned, this is contrary to misophonia, where peripheral damage doesn't appear to put a patient more at risk for developing the condition or alter its severity.
One similarity between the conditions is that both can lead to behavioral and psychological problems, like difficulty with concentration, attention, depression, and anxiety. The limbic system also seems to play a crucial role in both conditions as well, and in regards to tinnitus, it influences how and why a person may perceive or experience bothersome tinnitus. In 2002, Jastreboff reported that the two conditions commonly coexist, with one study noting that 60% of patients with tinnitus identified as having misophonia as well. With that said, many of us are likely familiar with the concept of tinnitus retraining therapy as a treatment approach for tinnitus, which was proposed by the Jastreboffs and includes elements of habituation, desensitization, and counseling. Although there are several different approaches to managing tinnitus, I wanted to bring this specific example up because we'll be revisiting it a little bit later on in the course.
Central Auditory Processing Disorder (CAPD)
We know individuals with CAPD struggle to process information in the same way as others because something adversely affects the way the brain is recognizing and interpreting speech sounds and contours. CAPD can manifest itself in a multitude of ways, like confusing similar sounds and words or mishearing information and difficulty in the presence of background noise. With that said, one commonly referenced similarity between the conditions is in the area of auditory figure-ground performance or speech and noise. We know that, in a healthy auditory system, our brain attends to relevant auditory information such as the speech signal of interest, but we automatically and reflexively filter the noise to the background, which we commonly refer to as the cocktail party effect. However, patients with CAPD often report difficulty filtering out pertinent speech information from noise.
Paradoxically, those with misophonia appear fixated and hyper-focused on specific sounds in the background like chewing, rather than the noise itself. Typical trigger sounds like chewing or sniffling are often viewed as sounds that individuals should be able to effortlessly ignore or tune out so they can continue to focus on more relevant auditory information in an environment. However, most patients with misophonia will report difficulty in doing this. Many patients report feeling hyper-vigilant towards sounds, which should be easily ignored. One major difference between the conditions is that there's no reported autonomic nervous system arousal in patients with CAPD. Whereas we know in misophonia, patients frequently experience an involuntary fight or flight response to specific auditory stimuli. I wanted to reiterate from earlier that there are multiple studies supporting basic impairments in auditory processing abilities and sensitization of the auditory cortex in patients with misophonia. I think it would be very interesting to evaluate how these patients perform on traditional subjective CAPD measures like the SCAN-C or A as a point of comparison to some of these electrophysiologic studies.
Sound Intolerance
I wanted to briefly touch on generalized sound sensitivity or sound intolerance concerns, since it's a very common complaint, especially in pediatrics. We commonly hear of children covering their ears with their hands to avoid loud, overwhelming sounds like vacuums and toilets flushing. In most instances, children often outgrow these avoidance and intolerance tendencies. As audiologists, we also know there are several health conditions that can worsen sound intolerance or sensitivity concerns like anxiety and recurring ear infections, migraines, seizure disorders, and neurodevelopmental disorders like autism. While specific medical conditions can exasperate auditory sensitivity, it's important to rule out a sensory integration disorder when there are concerns for other sensory defensive behaviors, like texture aversions or light sensitivity. Because in these instances, when the peripheral hearing system is otherwise normal, the sound sensitivity concerns may be secondary to the child's overall sensory profile rather than indicate a true decreased sound tolerance disorder like misophonia. These patients will likely benefit from occupational therapy or psychological evaluation to assist in promoting self-regulation strategies and managing psychosocial implications. Generally speaking, auditory training therapies, desensitization exercises, exposure therapy, cognitive behavioral therapy, and positive reinforcement strategies have been effective in alleviating concerns for sound intolerance.
Alternative Conditions
Aside from differentially diagnosing auditory related conditions, it's equally important to differentiate between alternative psychological, behavioral, and neurological conditions, especially because the literature suggests many symptoms overlap with several other disorders. With that in mind, as literature continues to emerge, researchers are agreeably admitting that no one condition seems to account for all of the characteristics and behaviors specific to misophonia.
- Sensory Processing Disorder (SPD)
- Oppositional Defiant Disorder (ODD)
- Obsessive Compulsive Disorder and Related Disorders (OCD)
- Neurodevelopmental Disorders (i.e., ASD)
- Generalized Anxiety Disorder (GAD)
- Attention Deficit Hyperactivity Disorder (ADHD)
- Post Traumatic Stress Disorder (PTSD)
Some of the conditions listed in the literature as requiring a differential diagnosis include sensory processing disorders, especially as it relates to a subtype of SPD known as sensory over-responsitivity, oppositional defiant disorders, obsessive-compulsive disorders, autism spectrum disorder, generalized anxiety disorder, and post-traumatic stress disorder. It's important to know that this isn't a comprehensive list by any means. There is a multitude of other conditions, which may have symptom overlap or coexist as well. As an example, you may have a child present clinically with a mood disorder, tinnitus, OCD, and misophonia, which can present a unique challenge to management and intervention, but it also reinforces why a team-based approach is so critical to diagnostic assessment and also therapeutic intervention for these patients.
Subjective Assessment
Case History Reports
I wanted to highlight our proposed protocol here at Nemours, so you would have it as a reference. We typically begin our appointments by inquiring about case history and having families complete self-assessment questionnaires. Case history reports should minimally cover the patient's medical, audiologic, and otologic background, risk factors, and prescribed medications that may be sensitizing medications, as well as developmental, social, educational, and therapeutic history. It's also important to inquire about sound sensitivity onset, behavioral and emotional reactions, coping strategies, and the patient's overall psychological state. We need to understand if there is potential for a comorbid diagnosis like anxiety, depression, or OCD, as well as self-harming tendencies, and determine if these concerns are currently inadequately being managed or addressed.
- Medical history (i.e., birth, genetics, surgical, medications)
- Developmental, social, educational, and therapeutic history
- Otologic and audiologic history (auditory concerns)
- Sound sensitivity behaviors, onset, management
- Psychological health
Psychological Screener Scales
As part of our self-assessment measures, we use a combination of psychological screener scales and misophonia rating scales, which we'll discuss in more detail shortly. We are very fortunate to have a psychologist on staff within our department who provides counseling and support to our families and works with nearly all of our sound sensitivity referrals. As part of our multidisciplinary approach, we jointly decided to implement anxiety and depression screenings as part of our case history intake so that we could better counsel families when a referral to psychology was warranted and also address some of the psychosocial implications that may be interfering with the quality of life.
Generalized Anxiety Disorder (GAD-7). We implemented the seventh edition of the Generalized Anxiety Disorder Scale questionnaire, which is simple and quick to administer assessment. It's also sensitive at detecting concerns for panic disorder, social anxiety disorder, and post-traumatic stress disorder. The child or family is instructed to rate how often the patient has been bothered by the seven scaled items over the past two weeks. Upon completion, the clinician will add up the scores from the four response categories labeled not at all sure, several days, over half the days, or nearly every day. Then we'll sum the individual columns together to obtain a total score ranging from zero to 21. A reasonable cutoff point indicating further evaluation or a referral to psychology for intervention is typically deemed as a score of 10 or more.
Personal Health Questionnaire Assessment Scale (PHQ-8). We also utilized the eight edition of the Personal Health Questionnaire Scale to screen for depression severity. This is another quick and simple assessment where the patient is instructed to rate how often the child has been bothered by the eight scaled items displayed over the past two weeks. The scoring system is identical to the anxiety screener we discussed where the clinician adds up the scores from their four response categories and then sums the individual columns together to obtain a total score ranging from zero to 24. At our clinic, we established a score of 10 or greater as warranting a referral to psychology. But I should mention that we offer psychological services to all of our patients being seen for sound sensitivity concerns, we placed higher priority and emphasis on referring patients with a score of 10 or more on either of the psychological screeners.
Assessment Questionnaires
Sound Sensitivity Questionnaire (SSQ). For clinical purposes, we decided to develop one comprehensive protocol to address misophonia, tinnitus, and hyperacusis, which we deem to be a part of our sound sensitivity clinic. We created a sound sensitivity questionnaire to quickly reference and highlight the patient's chief complaints and guide which clinical assessment and diagnostic measures would be most relevant to the appointment. This is typically one of the first forms completed by the family when they arrive. You can see in Figure 3, it starts with a brief medical history, highlighting some common risk factors and alternative conditions with potential symptom overlap, like sensory processing disorder and auditory processing disorder. Then the next section titled sound sensitivity history provides a glimpse into the primary sound sensitivity concerns. Question one is meant to be specific to tinnitus. Questions two and three are primarily directed towards phonophobia and hyperacusis, respectively. Questions four and five are directed towards misophonia. The questionnaire allows us to quickly identify the primary concerns. For instance, if a patient selects yes to one, four, and five in the sound sensitivity history section, then we suspect we may be dealing with a misophonia diagnosis further complicated by tinnitus, and we can then immediately pull the appropriate self-assessment measures for completion and proceed with the appropriate diagnostic protocols. You'll also see some common auditory behaviors and complaints at the bottom of the questionnaire, which we included, given the reports of possible central auditory nervous system involvement and difficulty with filtering out specific sounds as well.
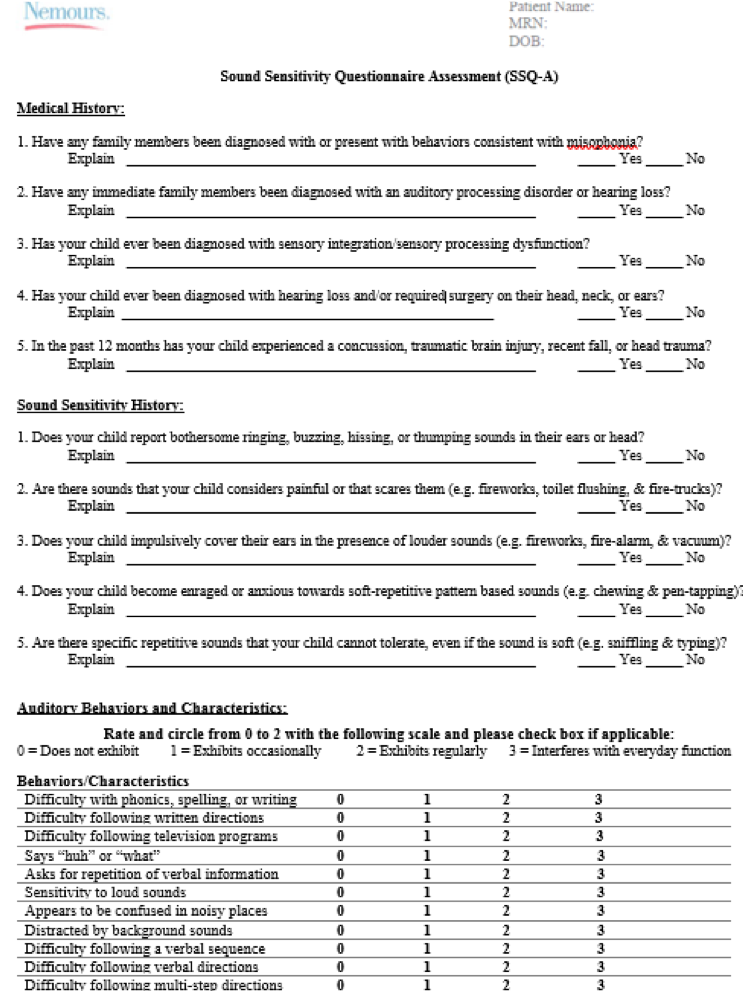
Figure 3. Sound Sensitivity Questionnaire
Misophonia Assessment Questionnaire (MAQ). Regarding the misophonia self-assessments, we utilize two measures, starting with the Misophonia Assessment Questionnaire developed by Marsha Johnson in 2013, which primarily focuses on the emotional and psychosocial impact of the condition. It's composed of 21 questions based upon how often each item applies to the patient and utilizes a rating scale from zero, not at all, to three, almost all of the time. The total score is calculated by summing together the total points from each column based upon their specified point values. The total scores can range from zero in the subclinical range to 63 in the extreme range, with higher scores indicating higher overall severity ratings.
Amsterdam Misophonia Scale Questionnaire ("A-MISO-S"). We also utilize the Amsterdam Misophonia Scale developed in 2013 by Schroder and colleagues at the University of Amsterdam to measure the impact and fixation with trigger sounds. It's composed of six questions that provide insight into various categories like time spent preoccupied with the condition, distress levels, and avoidance tendencies. The rating scale ranges from zero to four for each question, and to score the assessment, you must sum together the total number of points from all of the questions. In the example provided, the total score would be 11. The total scores can range from zero in the subclinical range to 24 in the extreme range.
Audiological Assessment
Once we complete our case history and self-assessment measures, we proceed with our diagnostic evaluation, which begins with otoscopy and standard tympanometry to assess for outer and middle ear pathology. We also conduct ipsilateral and contralateral acoustic reflexes to evaluate the integrity of the stapedial reflex, as well as rule out concerns for auditory neuropathy and retrocochlear pathology. If there are concerns for hyperacusis, then we'll typically bypass acoustic reflexes and attempt to proceed with a limited ABR evaluation performed at a more comfortable listening level, again, to rule out concerns for neuropathy or retrocochlear pathology. We also conduct extended distortion product otoacoustic emissions to provide insight into cochlear outer hair cell function and integrity as well. We'll then proceed with the standard comprehensive audiologic assessment, including speech recognition and discrimination testing, as well as pure-tone air conduction testing from 250 to 8,000 Hz, including the inter-octaves. Bone conduction testing may be pursued at the discretion of the provider when there are concerns for peripheral hearing loss. We also conduct ultra high-frequency testing to provide additional information regarding the integrity of the peripheral hearing system from 9,000 to 20,000 Hz, because it gives us more information regarding the integrity of the cochlea, especially towards the more basal ends. It's also worth noting that many clinicians, including our facility, have referenced the potential for abnormally good ultra high-frequency hearing sensitivity in patients with misophonia, with the extended high frequencies appearing to possibly be more sensitive than would be expected in typical adolescents since we're a pediatric institution.
However, further research is still required to see if this is a valid and statistically significant finding. As part of the differential diagnosis, we perform LDLs to rule out concerns for hyperacusis. As a word of caution, we recommend only providing the modified Khalfa hyperacusis assessment when there are organic concerns for hyperacusis. Because clinically, we observe that the measure was sensitive to decreased sound tolerance disorders, but was not necessarily specific to hyperacusis. A patient with misophonia may score in the clinically significant range on the modified Khalfa even if there aren't clinical concerns for a diagnosis of hyperacusis. Lastly, in light of our previous conversations and discussions, we conduct a bilateral Bamford-Kowal-Bench Speech-in-Noise Test to quickly screen for concerns for auditory figure-ground deficits. I should also mention that we previously conducted cortical auditory evoked potential and OEE suppression testing on patients with misophonia as well. However, due to several interesting but abnormal findings, we moved this initiative over to our research department for the time being.
- Otoscopy
- Tympanometry (226 Hz)
- Ipsilateral & Contralateral Acoustic Reflex Testing
- Distortion Product Otoacoustic Emissions (DPOAE(s))
- Pure-tone air audiometric testing from 250-8,000Hz
- Ultra-high frequency assessment from 9,000-20,000 Hz
- Loudness Discomfort Level (LDL) Testing
- Positive for Hyperacusis Criterion (Goldstein & Shulman,1996):
- LDL is 90 dB or less at two or more frequencies
- Dynamic range is 55 dB or less at any frequency
- Subjective complaints about sound sensitivity as evidenced by the Modified Khalfa and/or case history reports
- Positive for Hyperacusis Criterion (Goldstein & Shulman,1996):
- Bamford-Kowal-Bench – Speech-in-noise Test (BKB-SIN)
Self-Assessment Tools
I want to quickly highlight the other self-assessment measures available for clinical use so you can reference them at your convenience. It is important to keep in mind that none of these self-assessment measures have been scientifically validated to date. We already discussed the implementation of the misophonia assessment questionnaire and Amsterdam Misophonia Scale, so we'll pick up from there.
Misophonia Coping Responses. The Misophonia Coping Responses questionnaire consists of 21 questions rated on a scale from zero, not at all, to three, almost all the time, and was developed by Tom Dozier in 2013. It's primarily recommended to be utilized as a counseling tool to gain insight into how the patient is coping with their triggers, as well as highlight some non-productive coping strategies. It's not meant to measure total severity, so calculating a total score is not necessary. The questionnaire's more so meant to help guide conversations with patients and families.
Misophonia Emotional Responses. Also developed by Tom Dozier in 2013, the Misophonia Emotional Responses questionnaire consists of 26 questions with an identical rating scale from zero, not at all, to three, almost all of the time. It was developed to identify maladaptive behaviors and gain additional insight concerning emotional responsitivity towards trigger sounds. This questionnaire was also developed to serve as a counseling tool and is not meant to provide an objective measure of overall severity, so you won't find a rating scale for this questionnaire assessment.
Misophonia Physiological Response Scale (MPRS). The Misophonia Physiological Response Scale was developed in 2015 by Nathan Bauman. This is a very quick and simple assessment to administer, where the patient is asked to select a level that most closely aligns with or describes their physical reaction towards trigger sounds. The levels can range from zero, no response, to 12, an immediate emotional reflex response, including rage. In Rouw and Erfanian's 2018 study, which we had discussed a bit earlier, they had also noted that the most common response level identified amongst patients with misophonia on the NPRS was level eight, which describes the physical sensation which equates to emotional pain and causes very strong reactions.
Misophonia Family/Significant Other Assessment Questionnaire. Marsha Johnson had developed the Misophonia Family/Significant Other Assessment questionnaire in 2014. It's meant to provide an understanding of how the condition impacts family dynamics and interpersonal relationships. Obviously, it's no secret that misophonia can have major detrimental consequences on family relations and interactions, including mealtime, family vacations, and travel. We also know that patients are more commonly triggered by individuals within their inner circle. It can serve as a viable counseling tool. The questionnaire consists of 18 questions with a rating scale from zero, not at all, to three, almost all of the time. The total score is calculated by summing the total scores from each response column based upon their numerical value, similar to the misophonia assessment questionnaire that we discussed earlier. Higher score suggests higher overall severity. Please note that you do need permission from the author to utilize this questionnaire clinically.
Misophonia Impact Survey (MIS). The Misophonia Impact Survey was developed in 2016 by Tom Dozier and is another counseling tool that evaluates the impact of the condition on interpersonal relationships, including family dynamics, social activities, work and school, and personal time. The survey consists of five simple severity rating scale questions ranging from zero, none, to 10, extreme. It's not necessary, again, to calculate a total score, the survey is meant to guide conversations and highlight how misophonia has affected relationships over the past couple of weeks.
Misophonia Questionnaire (MQ). The Misophonia Questionnaire was developed in 2014 by Wu and colleagues in association with the University of Florida as part of a large scale undergraduate study to assess symptom severity. The questionnaire consists of three sections or subscales. The first section consists of the misophonia symptom scale, which evaluates common trigger sounds in the individual's environment. The second section, the misophonia emotions and behaviors scale, surveys a person's reaction towards trigger cues, such as fleeing from the environment, or verbal aggression. Items from both scales are rated from zero to four, and the overall total score from these two sections should be summed together to provide a total score ranging from zero to 68. Higher scores, again, suggest overall greater severity. Then for the third section, the misophonia severity scale, patients are asked to pick the level which most closely matches their perceived severity using a 15 point scale. The literature suggests that a score of seven or higher on this section is considered clinically significant and suggests that the patient would likely benefit from some form of intervention.
Misophonia Activation Scale (MAS-1). Lastly, in 2010, part A of the Misophonia Activation Scale was created by Misophonia UK to evaluate emotional responsiveness. Then part B was devised by Natan Bauman to assess physical sensations associated with misophonia. For each section, the patient is asked to rate their experiences on a 10 point scale. Rouw and Erfanian's 2018 study had determined that level nine was most commonly reported by patients with misophonia for part A, which describes attempts to flee the situation over emotional responsiveness and conscious intent to not inflict violence on an inanimate object. For part B, level eight was most commonly identified, which describes a physical sensation best described as emotional pain.
Management Strategies
In regards to management, there are no empirically supported therapeutic treatments at this time, so patients and clinicians should be very wary of anyone claiming to have a cure. With that said, many anecdotal approaches are being implemented based on successful case studies and uncontrolled studies. Nevertheless, many providers and researchers do agree that a multidisciplinary approach to assessment and intervention is crucial.
Referrals & Multidisciplinary Team
The typical disciplines involved in patient care often include audiology, occupational therapy, psychology, and primary care providers as well. Neurology may also be consulted due to sudden changes in mood or sensory perception at the discretion of the provider.
Primary care physician. Let's begin by discussing the PCP's role. At this time, there's no evidence that pharmacological intervention is effective in treating misophonia. However, physicians may be helpful in providing treatment to address alternative coexisting conditions like anxiety or depression. They should also encourage healthy lifestyle habits for exercise, sleep, and diet, which can deescalate tension and stress, which otherwise may typically exasperate misophonia.
Occupational therapy. As for occupational therapists, they may be helpful in differentiating misophonia from sensory processing disorders and can provide strategies for improving self-regulation to better manage disruptive behaviors, emotions, and impulse reactions. Some researchers propose that misophonia may be a subtype of sensory over-responsitivity, in which case, a sensory diet may also be effective and best described strategic mix of sensory activities to help with emotional regulation. Then, auditory training therapies like Tomatis Method, iLs Safe and Sound Protocol, and the iLs Sensorimotor Focus track have also been proposed to improve sound sensitivities. Many of these auditory training programs focus on reducing stress and auditory sensitivity through nervous system regulation while enhancing resilience.
Psychology/Psychiatry. Psychologists also play a key role in teaching productive coping mechanisms and stress reduction strategies, like progressive muscle relaxation, hypnosis, guided imagery, and meditation. They also may implement several behavioral approaches, including cognitive-behavioral therapy, exposure therapy, counterconditioning, and systematic desensitization, which we'll discuss in more detail in a bit. Biofeedback techniques may also be introduced to improve upon self-regulation, which allows patients to see their physiologic responses in real-time so they can gain increased control over involuntary body functions like heart rate and muscle tension. It can also be used to monitor downregulation and effective coping strategies, as well.
Audiology. Last but not least, as audiologists, we play an important role in differentiating between alternative auditory conditions and psychoacoustic disorders. We also have a responsibility to counsel on the overuse of hearing protection due to the risk of auditory deprivation. In fact, we should be encouraging a sound-rich environment whenever possible because ambient background noise can be helpful in masking out or decreasing awareness towards trigger sounds. On the ear level, sound generators may also be appropriate for certain patients, which can eliminate concerns for auditory deprivation while also reducing exposure to trigger sounds by making them subaudible. We've had many patients with sound generators who have noted that, while it doesn't completely eliminate the response, it helps to take off the edge and make the response a bit more manageable and triggers more bearable. Lastly, we may choose to implement and counsel on misophonia retraining therapy, which is a modified TRT approach proposed by the Jastreboffs. In 2014, the Jastreboffs claimed an approximately 80% success rate with the implementation of their modified approach for treating patients with misophonia and noted that participants reported reduced symptom severity and improved quality of life measures.
Audiology | Occupational Therapy | Psychology/Psychiatry | Primary Care Physician |
Differential diagnosis between alternative auditory conditions |
| Stress reduction therapies and coping strategies | Assist in managing or treating co-occurring or co-existing conditions (i.e., anxiety & depression)
|
Misophonia Retraining Therapy (modified TRT) -
- Directive and Informational Counseling - Sound therapy implementation (i.e., sound generators) | Auditory training therapies (anecdotal) -
- Tomatis Method - iLs Safe & Sound Protocol - iLs Focus (Sensorimotor) | Behavioral Approaches -
- Cognitive Behavioral Therapy - Exposure Therapy - Counter-Conditioning - Systematic Desensitization | |
Hearing protection (i.e., musician earplugs) | Biofeedback |
Figure 4. Management strategies and the multidisciplinary teams.
Misophonia Protocol
The Jastreboffs proposed misophonia retraining therapy protocol focuses on eliminating the conditioned reflex response by pairing offensive sounds with something pleasant in order to produce a positive association with the trigger. There are four graduated sound protocol categories, and each has its own unique specifications regarding control over the environment, stimulus, and sound level.
Category 1. In category one, the patient has control over the sound source, stimulus, and sound level, and is asked to pick an enjoyable or pleasant sound like music or an audiobook. They should attentively listen to the stimulus at a comfortable level at least once per day for several weeks. However, they're asked to gradually and progressively increase the volume of the sound by a noticeable difference in weeks two and three.
Category 2. In category two, the patient still has control over the selected sound source and stimulus, but only partial control over the sound level. Someone who is close to the individual, like a parent or a spouse, will select what is deemed to be an appropriate sound level for the patient to listen to. The patient will then provide feedback at the end of each session so that the sound level can be adjusted for future sessions.
Category 3. In category three, the goal is to introduce a broader variety of sounds. The patient is asked to go into a louder external environment like a movie theater or a mall or somewhere they find enjoyable where they have control over the environment, but they don't have specific control over the stimuli introduced or the sound level. In this phase, the patient may choose to leave the environment when they are feeling overwhelmed by certain sounds. However, they should try to re-enter the environment after a short break, about 10 to 15 minutes long.
Category 4. Then in category four, the final stage, specific offensive trigger sounds are addressed, and the patient has no control over the stimulus or sound level. The goal is to combine offensive trigger cues with highly positive or enjoyable sounds and experiences while modifying the mixing point of the sound levels. The positive sound will initially take priority and will be set at a louder level, however, over time, the patient should gradually decrease the positive stimulus until it's eliminated and tolerance to the offensive sound increases or builds up. Patients are also encouraged to incorporate additional senses to further enforce the positive association like smell and sight as well.
- Category 1
- Patient controls selected stimulus and sound level
- Select and attentively listen to a pleasant sound at a comfortable level and gradually increase the sound level over 3 weeks
- Category 2
- Patient controls selected stimulus but have only partial control of the sound level
- Someone else selects what is deemed to be an appropriate sound level, and the patient provides feedback at the end of each session so that the sound level can be adjusted for future sessions
- Category 3
- Patient has some control of selected stimulus, but the sound level is no longer in their control
- Participate in enjoyable activities that expose the patient to a variety of additional sounds
- Patient may leave environments causing discomfort but should re-enter following a break
- Category 4
- Patient has no control over selected stimulus or sound level – this phase directly targets offensive stimuli and combines trigger cues with positive/enjoyable auditory stimuli and experiences
- Pleasurable sound will initially be set higher than the offensive sound; however, over time the enjoyable sound will be decreased as tolerance to the offensive sound increases until eliminated
Behavioral Approaches
From a psychological intervention point of view, obviously, psychological intervention is outside of our scope of practice, but I do think it's important to highlight some of the more commonly implemented behavioral approaches.
Cognitive behavioral therapy. Cognitive behavioral therapy is considered to be one rational approach because the aim is to alter the negative thought processes, behaviors, and emotions towards the misophonic response while incorporating productive coping skills. It's also worth noting that in 2017, Schroder and colleagues reported that cognitive behavioral therapy was effective in reducing misophonia symptoms in 48% of patients who underwent eight biweekly sessions.
Exposure therapy (Habituation). Another common approach is exposure therapy, which a controversial form of intervention where individuals who have developed some sort of aversive, typically fear-based conditioned response undergo graduated exposures to foster habituation and coping skills until the physiologic response towards the stimulus is diminished or abolished. I can't tell you how many times I have been asked about this approach by patients, or I've heard parents say that they don't let their children leave the kitchen table because they need to learn to deal with it.
So why is it so controversial? Well, there's a couple of reasons, starting with the obvious, which is, if exposure therapy helped manage the condition, then wouldn't everyone be cured by their own daily exposures? Many trigger cues are fundamental to survival, like breathing and eating, yet it doesn't seem like our lifetime of exposure has been effective in reducing the response. In fact, we learned earlier that many individuals report worsening symptoms from the time of onset. Also, if you do take the time to look through some blogs or consult with someone who has undergone exposure therapy for misophonia, they often claim it strengthened trigger severity rather than reduced it. We also mentioned that exposure therapy seems to work best for learned responses, like OCD or phobias. While part of the misophonic response does seem conditioned or learned, we also know that there are physiological and functional brain differences in these patients and that the involuntary fight or flight response occurs within milliseconds before conscious processing even has a chance to occur. Simply put, exposure can't change physiology. There are also reported concerns for lack of auditory gating, which we discussed briefly at the beginning of our presentation, but refers to the ability to filter out irrelevant or non-salient auditory stimuli. However, in patients with misophonia, the threat seems to go up for as long as the sound is present and is often mistakenly perceived as highly salient, toxic, or threatening. Then exposure therapy also lacks memory reconsolidation, which means that memories aren't stable, and every time we retrieve a memory, it's altered slightly. With memory reconsolidation, the concept is to change the association between the stimulus and the nervous system by altering the memory. However, researchers are still trying to figure out a way to do this in a controlled, systematic fashion. Until then, some researchers claim exposure therapy won't work because it doesn't address the memory itself. Nonetheless, exposure therapy isn't always bad, and there are several case studies and testimonials that do report success with the implementation of exposure therapy. I encourage providers to use extra caution when implementing this and to make sure that it is completed in a safe, controlled, systematic fashion with graduated exposure until further research is done looking at its efficacy.
Counter-conditioning. Counter-conditioning is another common therapeutic approach that is commonly implemented, where the goal is to reduce or weaken the emotional response by gradually pairing aversive stimuli with more positive and pleasant stimuli, similar to misophonia retraining therapy. The aim is to foster a more neutral response with counterconditioning. Tom Dozier recommended a form of counterconditioning using a neural repatterning technique in 2015 to create an application called Trigger Tamer, which utilizes controlled minimal exposure to trigger cues paired with positive experiences and progressive muscle relaxation to weaken the emotional and physical reflex response. Several case studies have also suggested success with this method.
Systematic desensitization. Finally, systematic desensitization is frequently implemented and incorporates elements of relaxation training using an anxiety hierarchy and gradual exposure to aversive stimuli. The goal of desensitization training is to diminish the emotional response to an aversive stimulus through repeated exposure and experience while implementing relaxation techniques.
- Cognitive Behavioral Therapy
- Change the negative thought processes, behaviors, or emotions
- Counter-Conditioning
- Modify the negative emotional response to a stimulus into a more positive response – allowing triggers to be more bearable or less unpleasant
- Neural Re-patterning Technique - Trigger Tamer application (Dozier, 2015)
- Systematic Desensitization
- Relaxation techniques and controlled gradual exposure in order to foster a weakened or more neutral emotional response to the stimulus
- Exposure Therapy (Habituation)
- Emotional arousal and physiological responsiveness decrease naturally in response to repeated exposure to auditory or visual triggers
- Controversial treatment – no scientifically controlled validated research
Barriers to Treatment
Despite Schroder and colleagues' proposal in 2013, there is no universally accepted diagnostic criteria or validated objective measures or biomarkers to identify the presence or severity of the condition, primarily making it a diagnosis of exclusion at this time. Misophonia has also not been formally accepted or recognized by the DSM-V or American Psychiatric Association as an organic condition and is not recognized by ICD-10 as a billable condition. In addition, misophonia is not widely known or understood condition across disciplines. Having a basic understanding of the condition is essential to patient care. Something as simple as keyboard typing during an appointment may trigger our patients, so we do need to be mindful and thoughtful about how we approach these patients clinically. Furthermore, the medical community is faced with shortcomings and limitations in research, and there are currently no scientifically controlled studies regarding the efficacy of the therapeutic intervention. While several self-assessment tools have been developed, none are scientifically validated to date.
Further Research & Resources
In light of the barriers to treatment, I also wanted to highlight a few of the potential research initiatives, which could help to foster a greater understanding of the condition, including the need for genetic testing, since patients often report the potential for familial inheritance patterns. It would be interesting to see how and if environmental influences affect gene expression. Additionally, Brout and colleagues proposed the need to evaluate if coexisting psychological conditions could make an individual more prone to developing misophonia or impact condition severity (Brout et al., 2018). From an audiologic perspective, discussions regarding deconstructing acoustic patterns and properties of trigger cues would allow us to determine if there is something acoustically unique about these sounds. It would also be interesting to further determine if there is, in fact, a correlation between ASMR and misophonia and if the conditions may possibly exist along with some type of audio physiological spectrum. Lastly, pharmacological intervention for managing symptomology should be evaluated further, as well as the effectiveness of treating coexisting conditions and the impact this may have on symptom severity for misophonia. The list could go on and on because we are still learning a great deal about the scope of the condition, but additional research is critical to further developing universal diagnostic criteria and clinical practice guidelines. This is meant to be for your reference and includes a list of useful resources that you can review at your convenience and may be helpful for both clinicians and families interested in learning more about the condition.
- International Misophonia Research Network (IMRN)
- Misophonia International
- Misophonia Kids
- Misophonia Provider Network
- Misophonia Institute
- Milken Institute Giving Smarter Guide
- Allergic to Sound
- "Quiet Please" Documentary by Jeffrey Gould (2017)
Conclusion
In summary, as new research is emerging, misophonia is further being categorized as an independent organic condition with distinct differences that sets it apart from existing auditory and psychiatric disorders. Although many conditions present with symptom overlap, none of these conditions completely fit the mold and encompass all of the behaviors and characteristics specific to misophonia. We know patients with misophonia experience negative effective states in response to specific, often soft, repetitive, pattern-based sounds which elicit physiological arousal and increase sympathetic nervous system activity. In addition, functional brain changes have been identified, including aberrant connectivity between brain regions responsible for emotional regulation, memory, and associative learning, as well as hyperactivity of the salience network, which is essential for coding the importance or relevance of sounds. There are also several studies that suggest a basic impairment in the central auditory nervous system, as well as sensitization of the auditory cortex. Unfortunately, at the end of the day, misophonia remains a complex and poorly understood condition. Further research in the form of scientifically validated and rigorously controlled studies, as well as a multidisciplinary approach, are critical to further establishing universally accepted diagnostic criteria and therapeutic intervention strategies.
References
The reference list can be found in the course handout.
Citation
Pellicori, J. (2020). Clinician's guide to misophonia. AudiologyOnline, Article 27026. Retrieved from https://www.audiologyonline.com


