Computerized Dynamic Posturography (CDP) is well documented in the clinical and scientific literature as an objective method of differentiating sensory, motor, and central adaptive functional impairments of balance. Because balance is the functional expression of a highly adaptive system of multiple interacting components, the functional impairment information provided by CDP is complementary to the traditional diagnostic approaches to balance disordered patients (ENG, rotary chair, MRI, etc.) that focus on individual, isolated anatomical components.
In an estimated 50% of patients with chronic balance disorders, especially those who are older, there is no single localized cause, and the traditional diagnostic tests are inconclusive. In these complex patients, the specific impairment information provided by CDP reduces ambiguity and is the only objective information for selecting treatment pathways leading to improved outcomes.
CDP comprises three functional test protocols. The Sensory Organization Test (SOT) is designed to examine how well the patient uses information from the vestibular, visual, and proprioceptive systems to control balance. The Motor Control Test (MCT) evaluates the effectiveness of the patient's motor automatic reflex responses to restore balance following sudden, unexpected forward and backward perturbations of the support surface. The Adaptation Test (ADT) uses 'toes up' and 'toes down' rotations of the support surface to evaluate the patient's ability to adapt to unexpected support surface irregularities. The results of each test protocol are summarized in easily interpreted graphs in which the patient's scores are compared to age-corrected normative values. Because of potential interactions among sensory, automatic motor, and central adaptive impairments, both the sensory and motor test protocols must be performed to accurately differentiate among the various impairments to balance.
CDP impairment information is used in conjunction with the results and findings from the patient's history, physical examination, and other diagnostic tests to prioritize for treatment, the specific impairments having the greatest adverse impact on function and most likely to respond to treatment. When the history, physical, and other test results are inconclusive, treatment decisions can be driven by the CDP information alone. Importantly, when clinical results and findings are inconsistent with the clinical presentation or history, CDP can alert the clinician to problems including otherwise unsuspected pathologies and/or the patient's unconscious or deliberate attempt to exaggerate symptoms.
The following cases illustrate the contribution of CDP to the comprehensive balance evaluation and effective treatment planning.
CASE ONE:
This 35-year-old female with a chief complaint of dizziness described as 'bothersome' of one month's duration is a typical example of a case in which the history, physical exam, and other diagnostic tests are inconclusive and do not suggest the pathway to an outcome. She denies true vertigo, positional symptoms or feelings of being off balance. She describes a feeling of lightheadedness, with occasional nausea, particularly after riding in the car. Antivert and valium were prescribed, without effect. The audiogram showed normal hearing bilaterally. Physical examination in the ENT office indicated normal balance testing (Rhomberg, and Hallpike). Video nystagmography results were within normal limits for caloric, oculomotor, positional and positioning tests. CDP results are shown below: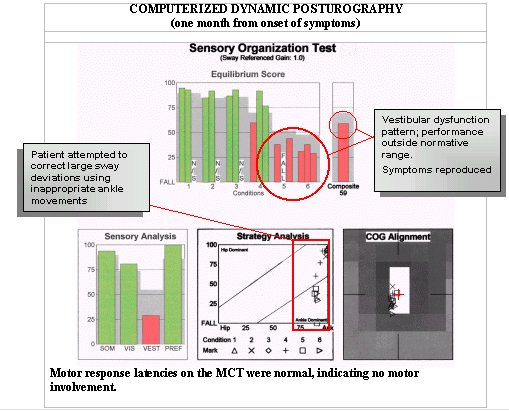
Although site-of-lesion testing indicated normal auditory and vestibular function in this case, the CDP data are consistent with vestibular impairment suggesting that the patient is either not receiving information from the peripheral vestibular system or is not effectively using the information to maintain postural stability, and that ankle movements are being used inappropriately to recover balance. Normal video nystagmography results tend to rule out peripheral vestibular system dysfunction. On the basis of CDP data, the patient was referred to physical therapy (PT) and a plan targeted toward challenging the vestibular system function on demand and making more effective use of ankle and hip movement patterns with exercises of increasing difficulty was implemented. The PT goal was to achieve more stable balance and alleviate subjective symptoms.
After several PT sessions supplemented by an individualized home exercise program, the patient was re-evaluated with CDP, with the results shown below. At the time of this evaluation, the patient reported no return of dizziness or lightheadedness symptoms, and the CDP results indicated functional control of balance to be within normal limits.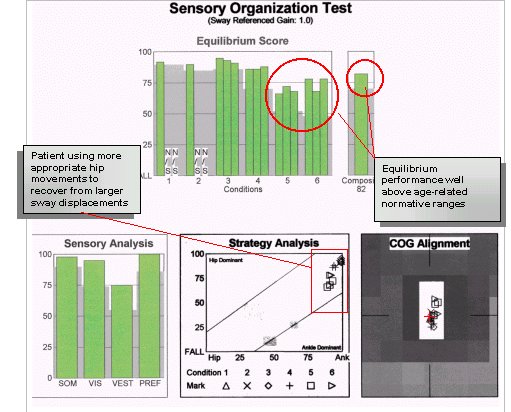
CASE TWO:
This 75-year-old male with complaints of occasional dizziness and unsteadiness is an example of an older individual in whom other clinical findings do not suggest a pathway to treat the patient's symptoms and complaints. The patient denied symptoms of true vertigo, and was most concerned with a progressive unsteadiness that hampered his snow skiing. The pure tone audiogram indicated a symmetrical mild high frequency sensorineural hearing loss with good speech discrimination bilaterally. ENG results were within normal limits for caloric, oculomotor, positional and positioning tests. CDP results indicated the following: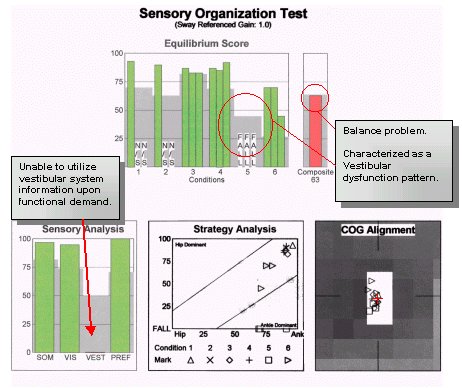
In this case, traditional auditory and vestibular testing indicated peripheral system function within the expected range for the patient's age. While the conventional site-of-lesion testing served to rule out major auditory pathway problems, it did not provide any insight about the nature of the patient's complaint, nor did it suggest a treatment program to increase function and reduce impairment. The patient is a 'high performer' who placed high demand on his balance function. Although this may be unusual for a patient his age, it is not an unusual situation for other patients. The CDP results revealed a balance problem present under activities placing a high demand on the vestibular system. Aside from qualitative measures used during the physical exam, CDP was the only objective measure of the patient's use of visual and proprioceptive inputs, and it was the only test that suggested a plan of treatment. After serious peripheral auditory and vestibular system abnormalities could be effectively ruled out, a treatment plan was designed for the patient to force the use of vestibular system input upon demand.
The patient was instructed in a home program targeting the vestibular system. On completion, the patient was retested with CDP, with the following results.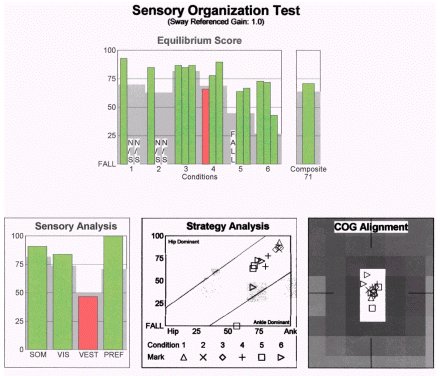
Note that the vestibular pattern on the SOT was considerably improved after physical therapy intervention, although a subtle deficit remained. This suggests that the vestibular mechanism was providing information to the central nervous system, but the information was not being used effectively. The absence of significant abnormalities in the ENG would support this impression. The patient was able to improve his function, once the impairment was measured and better understood. If SOT data were not available, the clinician would have lacked the data to formulate a treatment plan.
In consideration of this gentleman's active lifestyle, normal vestibular function was the goal and the home program was adjusted accordingly by increasing the intensity of the balance challenges.
CASE THREE:
A 69-year-old librarian initially presented with acute BPPV and was treated with canalith repositioning. The positional symptoms were resolved, but the patient continued to complain of dizziness and imbalance.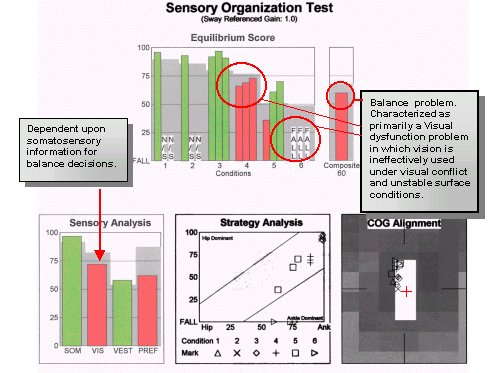
Test results revealed an underlying visual/vestibular functional deficit along with the positional symptoms of BPPV. A recent population study has shown that problems using vision for balance were common following treatment of BPPV patients with positioning maneuvers.
For this patient, treatment was designed to challenge the visual and vestibular systems to respond under conditions of altered somatosensory, or support surface, and visual conflict conditions. Through this focused intervention, the following results were achieved in thirty days.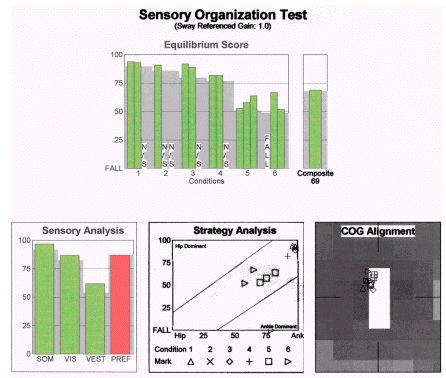
Note that in this case, conventional assessment and treatment would probably have led to treatment being stopped after the canalith repositioning procedure. The SOT, however, indicated that there were residual impairments in use of visual information for balance that were not addressed with the repositioning maneuvers. Once the impairment was demonstrated and better understood, the treatment plan was redesigned to be more effective and comprehensive.
SUMMARY
Clinical evaluation of dizzy or balance-disordered patients should include both conventional site-of-lesion tests and objective measures of balance. In the first two cases reviewed above, it is important to note that the patients were self-referred. Presumably, these patients were seeking more than a diagnosis; these patients were looking for professional assessment and a treatment plan to reduce the impact of their balance impairment.
The clinician's task is to investigate and rule out problems related to specific auditory/vestibular pathways and structures and to investigate possible means of effective treatment. With a comprehensive evaluation, the clinician can also establish a baseline for evaluating the outcome of the treatment plan. Although balance and vestibular rehabilitation can be effective solutions to increase function and reduce impairment, the program must be based on an objective functional assessment.
References:
1.Black F, Angel C, Pesznecker S, Gianna C. Outcome analysis of individualized vestibular rehabilitation protocols. The American Journal of Otology. 2000;21:543-551.
2.Black F. Clinical Status of Computerized Dynamic Posturography in Neurotology. Current Opinion in Otolaryngology and Head and Neck Surgery. 2001;9:314-318.
3.Stewart M, Chen A, Wyatt R, et al. Cost-effectiveness of the diagnostic evaluation of vertigo. Laryngoscope. 1999;108:600-605.
4.Shepard N, Telian S. Practical Management of the Balance Disorder Patient. San Diego, CA: Singular Publishing Group, Inc; 1996.
5.Fife T, Baloh, RW. Disequilibrium of unknown cause in older people. Ann Neurol. 1993 1994;34:694-702.
6.Tinetti M, Doucette J, Claus E, Marottoli R. Risk Factors for Serious Injury During Falls by Older Persons in the Community. Journal of American Geriatrics Society. 1995;43:1214-1221.
7.Di Girolamo S, Paludetti G, Briglia G, Cosenza A, Santarelli R, Di Nardo W. Postural control in benign paroxysmal positional vertigo before and after recovery. Acta Otolaryngol (Stockh). 1998;118:289-293.
8.Blatt P, Georgakakis G, Herdman S, Clendaniel R, Tusa R. The effects of the Canalith Repositioning Maneuver on resolving postural instability in patients with Benign Paroxysmal Positional Vertigo. The American Journal of Otology. 2000;21:356-363.
Computerized Dynamic Posturography: Clinical Application & Contribution in Three Cases
November 5, 2001
Related Courses
1
https://www.audiologyonline.com/audiology-ceus/course/addressing-fall-risk-pt-ot-38144
Addressing Fall Risk: PT, OT, and Audiology Assessment and Intervention, presented in partnership with Salus University
Multidisciplinary assessment and intervention of individuals at risk of falls is crucial in identifying functional and diagnostic factors as well as effective rehabilitation and prevention of future falls. This series identifies areas of collaboration and supportive information-sharing strategies between professions who commonly see individuals who fall and are likely to be injured due to a fall.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
Addressing Fall Risk: PT, OT, and Audiology Assessment and Intervention, presented in partnership with Salus University
Multidisciplinary assessment and intervention of individuals at risk of falls is crucial in identifying functional and diagnostic factors as well as effective rehabilitation and prevention of future falls. This series identifies areas of collaboration and supportive information-sharing strategies between professions who commonly see individuals who fall and are likely to be injured due to a fall.
38144
Online
PT180M
Addressing Fall Risk: PT, OT, and Audiology Assessment and Intervention, presented in partnership with Salus University
Presented by Bre Myers, AuD, PhD, Helena Esmonde, PT, DPT, NCS, Anna Grasso, OTD
Course: #38144Level: Intermediate3 Hours
AAA/0.3 Intermediate; ACAud inc HAASA/3.0; AHIP/3.0; ASHA/0.3 Intermediate, Professional; BAA/3.0; CAA/3.0; Calif. SLPAB/3.0; IACET/0.3; IHS/3.0; Kansas, LTS-S0035/3.0; NZAS/3.0; SAC/3.0; Tier 1 (ABA Certificants)/0.3
Multidisciplinary assessment and intervention of individuals at risk of falls is crucial in identifying functional and diagnostic factors as well as effective rehabilitation and prevention of future falls. This series identifies areas of collaboration and supportive information-sharing strategies between professions who commonly see individuals who fall and are likely to be injured due to a fall.
2
https://www.audiologyonline.com/audiology-ceus/course/contemporary-concepts-in-pediatric-vestibular-35586
Contemporary Concepts in Pediatric Vestibular Assessment and Management, presented in partnership with Seminars in Hearing
This 5-part webinar series is focused on the growing evidence of the need for pediatric vestibular evaluation, as well as the availability of successful treatment options for children. Guest editors, Dr. Devin McCaslin and Dr. Jennifer Christy along with a team of leading experts will present on select articles from a recent issue of the journal Seminars in Hearing (Issue 03 · Volume 39 · 2018).
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
Contemporary Concepts in Pediatric Vestibular Assessment and Management, presented in partnership with Seminars in Hearing
This 5-part webinar series is focused on the growing evidence of the need for pediatric vestibular evaluation, as well as the availability of successful treatment options for children. Guest editors, Dr. Devin McCaslin and Dr. Jennifer Christy along with a team of leading experts will present on select articles from a recent issue of the journal Seminars in Hearing (Issue 03 · Volume 39 · 2018).
35586
Online
PT300M
Contemporary Concepts in Pediatric Vestibular Assessment and Management, presented in partnership with Seminars in Hearing
Presented by Sharon Cushing, MD, FRCSC, Katheryn Bachmann, PhD, Violette Lavender, AuD, Jennifer B. Christy, PhD, PT, Steven M. Doettl, AuD, PhD, Devin L. McCaslin, PhD, Kristen L. Janky, PhD, Amanda I. Rodriguez, PhD, AuD
Course: #35586Level: Intermediate5 Hours
AAA/0.5 Intermediate; ACAud inc HAASA/5.0; BAA/5.0; CAA/5.0; Calif. SLPAB/5.0; IACET/0.5; IHS/5.0; Kansas, LTS-S0035/5.0; NZAS/3.0; SAC/5.0
This 5-part webinar series is focused on the growing evidence of the need for pediatric vestibular evaluation, as well as the availability of successful treatment options for children. Guest editors, Dr. Devin McCaslin and Dr. Jennifer Christy along with a team of leading experts will present on select articles from a recent issue of the journal Seminars in Hearing (Issue 03 · Volume 39 · 2018).
3
https://www.audiologyonline.com/audiology-ceus/course/quantitative-vestibular-function-testing-pediatrics-35334
Quantitative Vestibular Function Testing in the Pediatric Population, presented in partnership with Seminars in Hearing
The purpose of this presentation is to provide an overview of how to perform vestibular tests in children, including which tests are recommended based on the child’s age and any modifications or considerations that can be made.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
Quantitative Vestibular Function Testing in the Pediatric Population, presented in partnership with Seminars in Hearing
The purpose of this presentation is to provide an overview of how to perform vestibular tests in children, including which tests are recommended based on the child’s age and any modifications or considerations that can be made.
35334
Online
PT60M
Quantitative Vestibular Function Testing in the Pediatric Population, presented in partnership with Seminars in Hearing
Presented by Kristen L. Janky, PhD, Amanda I. Rodriguez, PhD, AuD
Course: #35334Level: Intermediate1 Hour
AAA/0.1 Intermediate; ACAud inc HAASA/1.0; BAA/1.0; CAA/1.0; IACET/0.1; IHS/1.0; Kansas, LTS-S0035/1.0; NZAS/1.0; SAC/1.0
The purpose of this presentation is to provide an overview of how to perform vestibular tests in children, including which tests are recommended based on the child’s age and any modifications or considerations that can be made.
4
https://www.audiologyonline.com/audiology-ceus/course/minimum-stimulus-strategy-in-diagnosis-39433
Minimum Stimulus Strategy in the Diagnosis of BPPV
Benign Paroxysmal Positional Vertigo (BPPV) is the most common inner ear disorder, with a cumulative lifetime incidence of 10%. This course will cover the Minimum Stimulus Strategy (MSS), a nystagmus-based approach to streamline BPPV management, reducing the need for diagnostic and therapeutic maneuvers and minimizing patient discomfort.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
Minimum Stimulus Strategy in the Diagnosis of BPPV
Benign Paroxysmal Positional Vertigo (BPPV) is the most common inner ear disorder, with a cumulative lifetime incidence of 10%. This course will cover the Minimum Stimulus Strategy (MSS), a nystagmus-based approach to streamline BPPV management, reducing the need for diagnostic and therapeutic maneuvers and minimizing patient discomfort.
39433
Online
PT120M
Minimum Stimulus Strategy in the Diagnosis of BPPV
Presented by Andrea Castellucci, MD
Course: #39433Level: Intermediate2 Hours
AAA/0.2 Intermediate; ACAud inc HAASA/2.0; AHIP/2.0; BAA/2.0; CAA/2.0; IACET/0.2; IHS/2.0; Kansas, LTS-S0035/2.0; NZAS/2.0; SAC/2.0
Benign Paroxysmal Positional Vertigo (BPPV) is the most common inner ear disorder, with a cumulative lifetime incidence of 10%. This course will cover the Minimum Stimulus Strategy (MSS), a nystagmus-based approach to streamline BPPV management, reducing the need for diagnostic and therapeutic maneuvers and minimizing patient discomfort.
5
https://www.audiologyonline.com/audiology-ceus/course/debunking-vestibular-migraine-39434
Debunking Vestibular Migraine
Vestibular migraine seems elusive yet ever-present and misunderstood. Everything from features to test results and how to better serve this population of patients is covered in this course.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
Debunking Vestibular Migraine
Vestibular migraine seems elusive yet ever-present and misunderstood. Everything from features to test results and how to better serve this population of patients is covered in this course.
39434
Online
PT60M
Debunking Vestibular Migraine
Presented by Kaitlin Ryan, AuD, CCC-A
Course: #39434Level: Advanced1 Hour
AAA/0.1 Advanced; ACAud inc HAASA/1.0; AHIP/1.0; ASHA/0.1 Advanced, Professional; BAA/1.0; CAA/1.0; Calif. SLPAB/1.0; IACET/0.1; IHS/1.0; Kansas, LTS-S0035/1.0; NZAS/1.0; SAC/1.0
Vestibular migraine seems elusive yet ever-present and misunderstood. Everything from features to test results and how to better serve this population of patients is covered in this course.

