In many respects, communication skills may be the most important asset of an effective audiologist. In fact, one of the hallmarks of a successful audiologist is the ability to be a great listener and communicator. Even the most technically proficient audiologist is doomed to fail if he has poor bedside manner or feels uncomfortable talking about price with patients. Many audiologists enter the workforce ill-prepared to meet the common challenges of clinical practice in the real world, such as relating hearing aid features to expected benefits or addressing objections to their recommendations.
The purpose of this paper is to outline a specific system for taking care of hearing impaired patients in a busy commercial environment. The motivation for writing it comes from working with audiologists who graduated from institutions and, in many cases, lack the necessary skills to thrive in a commercial work environment. Fortunately, highly trained audiologists can succeed in commercial environments when they apply the simple system introduced here. The tools and tactics described below are designed to add structure to the audiologist's already strong academic and technical background.
In the commercial hearing aid business, value is largely based on the interaction between the professional and the patient. The more effectively you can build relationships and solve your patient's communication problems, the more likely you are to succeed both professionally and financially. Before reviewing the various tools and tactics needed to be an effective consultative selling professional, it is important to clearly define the term consultative selling. This is important because in many audiology clinics, the word "selling" has a rather negative connotation - even though most audiologists engage in the practice every day. In fact, to some individuals the very term "selling" conjures up fast talking men in checkered sports coats and white belts trying to pressure you into buying something you may not even want. After reading about consultative selling, most will agree that audiologists constantly engage in selling, and by honing their underlying communication skills, it can be improved.
What is Consultative Selling?
Consultative selling is a way to systematically discover the needs of each patient and to fulfill their needs for a better quality of life through counseling and treatment recommendations. Consultative selling is not about manipulating or pressuring the patient into doing something. It is a system in which the highly trained audiologist can apply both their technical and interpersonal skills in order to be successful in a commercial environment.
The core of the consultative selling system is discovering the needs of each patient by executing a series of next steps. The goal is to allow the patient to make an informed decision to buy, in an atmosphere in which the audiologist can practice in a professional manner.
Why a Consultative Sales System?
Systems provide clarity and consistency. In simple terms, a system is a step-by-step way of executing a task. Effective systems do not arise out of thin air; rather, they are typically based on what many others have done successfully for several years. Systems, like the ones outlined here, can help define your practice. When you have been taught, and then faithfully execute, a specific system your work is likely to be more focused. Moreover, when you encounter challenging situations, you will have a system to fall back on, and executing a system allows you to more effectively analyze skill areas needing improvement. For example, when you fail to complete a transaction with a patient for new hearing instruments, you can go back and review each part of the process within your system to see where you could have done better.
The majority of audiologists are not natural salespeople. This means that they have some discomfort with transacting a sale. For example, they might have difficulty asking people for money or spend too much time talking about the technical nature of the patient's hearing loss. The execution of a selling system is perhaps the most effective way in which professionals with some uneasiness with the sales process can perform admirably. In fact, many professionals that use a proven selling system flourish with a small amount of practice.
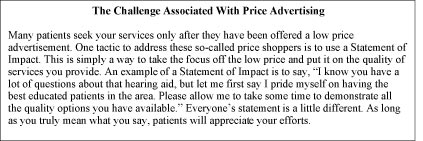
An effective consultative sales system has two core components: Discovery and Fulfillment. Within each core component is a series of tactics you need in order to move from point A (the patient has walked in the door for a pre-fitting appointment) to point B (the patient has agreed to purchase hearing instruments from you). Figure 1 outlines the essential tactics and tools you need to fulfill the discovery and fulfillment phases of the appointment.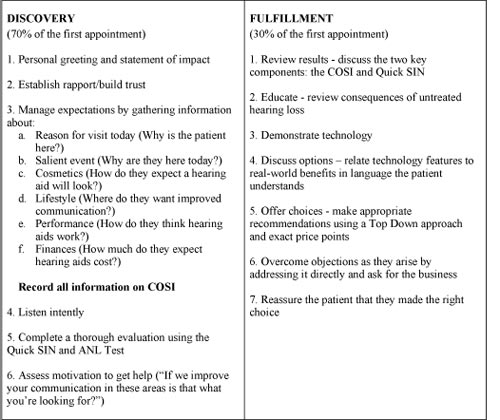
Click Here to View Larger Version of Figure 1 (PDF)
Figure 1. The essential tools and tactics needed for the discovery-fulfillment process
Phase 1: Discovery
The discovery phase of the appointment takes between 30 and 60 minutes to complete and its singular goal is to build a personal relationship between you and the patient. Although not referred to as the "discovery process," audiologists engage in it many times per day. Any time you are learning about the patient, asking good questions, and finding out all you can about a patient's communication needs, you are in the discovery phase. There are three essential steps of the discovery phase of the consultative selling model.
Step 1: Establishing Rapport and Building Trust
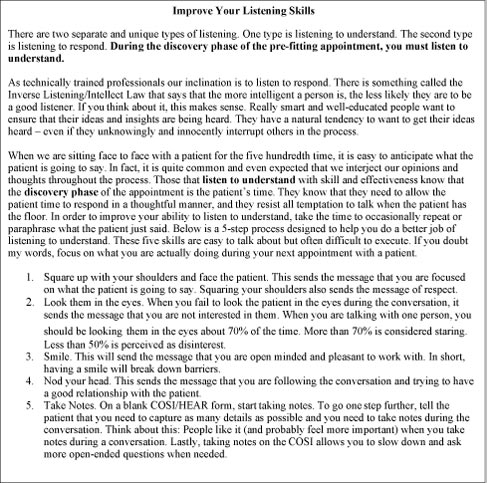
In order to effectively undertake the discovery phase of the consultation appointment you need to focus on two fundamental skills: 1) asking good questions to the patient and 2) being an effective listener. If you can master these two fundamentals, you will be more comfortable in a commercial environment.
Asking good questions and taking the time to listen is truly an art. Both of these skills can take a lifetime to master for some people. Below is a list of seven essential questions you should ask all patients during the initial evaluation. Please note this is not intended to be a script that is mindlessly read to the patient. That would be insincere and manipulative. Patients notice that right away.
Establishing Ownership of Visit (case history):
- What brings you to the office today?
- How may I help you?
- How long have you noticed this (communication difficulty)?
- I'm curious about____, please tell me more about that...
(Do not forget to involve third party)
Assessing Motivations/Establishing Need to Help:- What situations cause you the most difficulty with your communication?
- On a scale of 1 to 10, 10 being perfect hearing and 1 being a complete hearing loss; how would you rate your hearing?
- How ready are you for hearing aids? If 1 is "No way I'm ready for hearing aids" and 10 is "I wish I had hearing aids yesterday," how would you rate yourself?
Step 2: Assessing Communication Need; How to Complete a Detailed COSI
The COSI (Client Oriented Scale of Improvement) is the ideal tool for completing a pre-fitting assessment of communication need (Dillon, James, & Ginis, 1997). It takes things that most providers already do quite well, which is emotionally connect with the patient, and adds some structure to it.
The COSI allows the patient to target five or six specific listening situations for improvement; therefore, it is called an "open-ended" pre-fitting assessment. Because it is open-ended it allows the hearing care professional, patient, and significant other to work together during the hearing consultation to build a hearing aid treatment plan.
Below are four practical tips for completing a detailed COSI with all your patients.
A. List and target.
The first step when completing the COSI is to obtain patient-specific needs. The goal is to find at least five of the most important environments your client struggles to communicate effectively in and would like to improve with the use of hearing aids. These individualized needs can be as diverse as your clientele.
During the initial interview process you should sit down and engage the patient in conversation as you normally would. The only difference when using the COSI is you need to record the patient's goals and needs on the form. Notice on the blank COSI form that there are five spaces to record goals.
After collecting the individual's five specific needs it is important to rank each area in order of importance to the patient. The 5 specific needs can then be directly targeted as areas of improvement for the hearing aid user. The COSI allows hearing care professionals to build a patient-specific counseling agenda, as well as to pinpoint specific areas that are essential when talking about expectations. Figure 2 shows an example COSI for a patient, Henry O. His five specific needs are described in detail then ranked in order of importance to him.
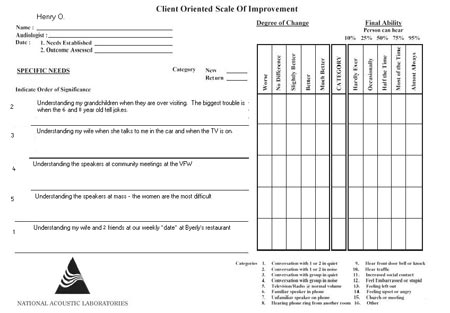
Click Here to View Larger Version of Figure 2 (PDF)
Figure 2. Example COSI for a sample patient
B. Get the details.
When obtaining the five specific needs from your patient it is important to obtain as much information as possible. For example if the patient states, "I want to hear better in noise," it is important to find out where, when, and with whom. Try to have your patient be as specific as possible.
Below is a list of questions to help delve further. It is important to make sure the questions are open ended rather than simple yes/no questions.
- What are specific situations you have trouble in?
- When was the last time you had trouble in noise and where was this?
- How frequently are you in noisy situations?
- Who are you trying to communicate with in noisy situations?
- What kind of room are you in when you have difficulty hearing in noise?
- How many people are typically in this environment?
C. Pick Two.
After the five specific areas are written down and ranked, choose two of the five most important areas to specifically focus on. Circle the two areas on the COSI form and number them #1 and #2 (see Figure 3). The reason for choosing only two is because most patients will only consistently pick two of the five original situations targeted for improvement.
For patient Henry O., we chose a situation that involves listening in noise, which is a fairly difficult environment, and a situation that involves soft voices in a quiet environment, which is an easier environment. It is important to pick both an easy and difficult environment to focus on and then develop realistic expectations around these areas.
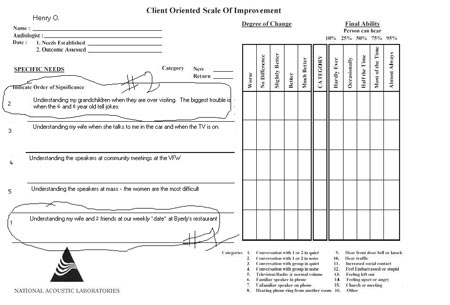
Click Here to View Larger Version of Figure 3 (PDF)
Figure 3. Circle and number two needs to initially focus on with the patient
D. A Tactic for Establishing Realistic Expectations.
After choosing the two situations to focus on, ask the patient how much benefit he or she expects to receive from their hearing aids in each environment. This is done to discover the patient's expectations before the hearing aids are even fit. The clinician can do this on a scale from 0 to 100 by asking the patient "From 0 to 100, how much do you expect a hearing aid to improve this area?"
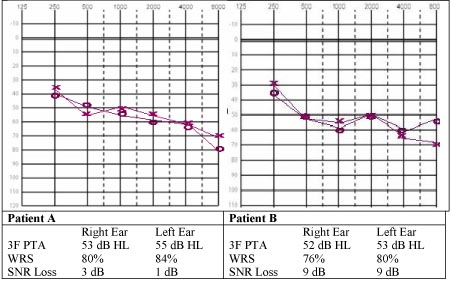
Take the following audiograms and QuickSIN scores for patient A and patient B. Both patients have relatively similar audiograms but vastly different SNR loss scores (please see QuickSIN on-line class for further explanation). Patient A is able to understand speech in noise at near normal levels and Patient B has significant difficulty understanding speech in noise. Depending on their expectations to hear better in noise, there may be vastly different counseling approaches taken for both patients.
Click Here to View Larger Version of Figure 4 (PDF)
Figure 4. Audiogram and QuickSIN scores for two patients
If both patient A and patient B said that they expected hearing aids to improve their ability to understand in noise by 70% you know there will be a need to counsel each patient differently.
Due to Patient A's near normal ability to understand speech in noise we may counsel him that it is very possible to obtain or to do even better than 70%. However, patient B will need to be counseled that due to his difficulty to understand speech in noise he may perform a little worse than 70%, maybe even lower than 50% in some situations, especially without directional microphones. It is important to give realistic expectations in the beginning, even before the first fit. This establishes more real-world expectations and provides for more successful outcomes.
Knowing this information allows the clinician to continue to encourage Henry to wear his hearing aids to obtain maximum results. Also, the clinician can continue to counsel on the use of hearing aids in noise. From Henry's COSI, you can see that he is only getting a slight amount of improvement in this area. This may be due to directional microphone misuse, unrealistic expectations, or improper positioning in a noisy environment. With further questioning, the clinician is able to continue to counsel Henry on understanding speech in noise.
Click Here to View Larger Version (PDF)
Step 3: Audiological Assessment
The final stage of the discovery process is the comprehensive audiological assessment. The obvious purpose of these tests is to ensure that you have accurately identified the patient's residual dynamic range and ruled out a medical problem. From a consultative selling perspective, however, these tests are used to gather information about the patient's communication ability in order to help them make an informed decision later in the appointment. The essential components of a complete audiological assessment are:
- Air Conduction Thresholds
- Bone Conduction Thresholds
- Immittance Audiometry (tymps and reflexes)
- Speech Audiometry (Quick SIN and ANL test)
- Threshold of Discomfort (LDL) Testing
Once you have completed all of your discovery work, you cannot abruptly move to the fulfillment stage of the appointment. It is helpful to transition from discovery to fulfillment with permission from the patient to move ahead. An effective way to do this is to simply ask the patient if they are ready to learn about the test results and possible treatment options. Once the patient has granted you permission, you may move to the second phase of the consultative sales model, which is fulfillment.
Phase 2: Fulfillment
The single goal of the fulfillment stage is gaining an agreement from the patient to do business with you. Gaining agreement does not necessarily mean that the patient is agreeing to purchase hearing aids from you. It could mean that the patient has agreed to see another professional you are recommending. It might even mean the patient is agreeing to come back and see you for a follow-up appointment in six months. Many times, however, you are asking the patient to complete a hearing aid transaction.
In most cases the fulfillment stage is much shorter than the discovery stage. If you have executed the discovery phase effectively, the fulfillment phase should be a natural conclusion to the appointment that often results in a transaction. The fulfillment stage of the appointment is a 7-step process that should culminate in the patient's decision to do business with you. In order to make the essential steps of the fulfillment stage easy to remember, use the acronym RED DOOR.
Step 1: Review results
Start by asking the patient if they would like a relatively brief review of the results, or if they would like to go into the details. By asking the patient how to proceed the patient will be more receptive to your explanation of the results.
It is important that you use language that the patient understands and relate the test results to the communication difficulties the patient is experiencing on a daily basis. It is up to you as the professional to create urgency to get help, and the way in which you communicate the results can build the necessary urgency in order for the patient to move to the next step. When reviewing results always use visual aids so that the patient clearly understands what you are saying.
Step 2: Educate (Discuss Consequences of Untreated Hearing Loss)
All of us would agree that there is a strong stigma associated with hearing loss and the use of hearing aids. In simple terms, most patients do not want to wear hearing aids because they make them feel old. It is relatively easy for many patients to simply delay their decision to purchase hearing aids because acquired and gradual hearing loss is not a life threatening condition. Educating the patient on the ill-effects of untreated hearing loss helps create urgency to accept your recommendation for new hearing aids (assuming the patient is a candidate for them) in an evidence-based manner.
After you review the test results, ask the patient for permission to move to the next step, which is to educate them about the consequences of untreated hearing loss and getting help today from hearing aids. This is an extremely important step because you need to overcome the reluctance on the part of many patients to overcome the easy decision to not get help from you. The most effective professionals take the time to build a strong case for getting help today, rather than waiting. Their effectiveness is directly related to their ability to explain the consequences of untreated hearing loss.
The content of your message will vary slightly depending on the test results and needs of the individual, however, you need to focus on the consequences of not getting the necessary help today. One way to convey this message is to simply say, "There are a few consequences of untreated hearing loss that all my patients need to know about...." All patients need a brief explanation of the following:
- The Effects of Auditory Deprivation. Auditory deprivation is the term used to describe a decrease in speech understanding resulting from a hearing loss. All levels of hearing loss starve the auditory centers in the brain of acoustic information. When it comes to fitting hearing aids, there is considerable evidence suggesting that patients with sensorineural hearing loss lose their ability to understand speech more rapidly than people with normal or near normal hearing (i.e. Silman, Gelfand & Silverman, 1984). You can express this to patients by saying, "Using hearing aids now will prevent your ability to understand speech from getting worse, and possibly, if you wait too long to get help, hearing aids would have very limited benefit."
- The Binaural Advantage. The discussion of auditory deprivation leads directly into a discussion of the advantage of binaural hearing provided from two hearing aids. You can also talk about auditory deprivation effects with those that want to wear only one hearing aid when they really need two. We know, moreover, that when a hearing aid is fitted to the unaided ear after two or three years of non-use, there is often a significant recovery in speech understanding ability in the newly aided ear. These recovery effects can be measured within a year of fitting the second hearing aid. It is also worth noting that a patient with normal hearing in one ear and an aidable loss in the other ear also experiences auditory deprivation and recovery upon amplification. Regardless of the hearing loss, overcoming the effects of auditory deprivation is possible through bilateral amplification.
- Social and Emotional Impact of Untreated Hearing Loss. There is also considerable evidence, much of it archived on the Better Hearing Institute (BHI) website (www.betterhearing.org/research/), suggesting that patients with untreated hearing loss suffer more from depression and social isolation compared to those of similar age who wear hearing aids. You can even site the recently published JAAA meta-analysis finding that those that decide to wear hearing aids have a higher quality of life when compared to people with hearing loss not using amplification (Chisolm et al., 2007).
- Financial Impact of Untreated Hearing Loss. The last piece of evidence to share with reluctant patients during this phase of the appointment is the fact that working-age people with untreated hearing loss typically earn less than those individuals with hearing loss that wear hearing instruments, which can be supported by resources at www.betterhearing.org.
This discussion should be part of the education phase of the pre-fitting appointment. When you communicate the consequences in a compelling way, you are very likely to create urgency within the patient to get help now. An added benefit is that it takes the focus off product and price and puts the focus on the needs of the patient.
During this specific phase of the appointment, this technique requires that you only discuss the consequences of not taking action to get help now and avoid any discussions of product or price. Once you have built a case for taking action today, you can move to the next step, which is to demonstrate technology and discuss model and price options in a top-down manner.
A second point is that when you are discussing consequences of untreated hearing loss with the patient, you need to focus on the evidence. This means you are citing findings from relevant studies and communicating them to the patient in language they understand, rather than relying on your opinions. Your clinical experience and opinions are important, but when you include evidence-based thinking into your process, it markedly improves your credibility and professionalism to the patient.
Step 3: Demonstrate Technology
After you take the time to educate the patient, emphasizing the consequences of untreated hearing loss, the next step is to demonstrate to the patient how hearing aids can work. Using a pair of programmable hearing aids, take the time to briefly show the patient how modern hearing aids are programmed with computer software and are customized to the individual's hearing loss. Be sure to use a pair of devices that are cosmetically appealing, such as open canal products.
During the demonstration process, it is a good idea to show the effectiveness of directional microphone technology and binaural hearing. You will need to prepare for the demo ahead of time by having two hearing aids ready to program and a listening situation available that has some background noise. In general terms, the demo step is there to build value and to educate the patient.
Click Here to View Larger Version (PDF)
Step 4: Discuss Options
The two major points of the discussion step are style (form factors) and technology. Make a clear recommendation regarding the style that is best for the patient by assessing the results of the audiogram and their lifestyle and communication needs. Depending on the social style of the patient, you can either inform them what their best option is or give them a couple of possibilities and allow them to make an informed decision.
When discussing technology it is easy to overwhelm patients on the technical details. Remember to keep things simple and talk about what needs to go inside the hearing aid to maximize their ability to communicate. The emphasis needs to be on what level of technology is needed for their individual needs. As a general rule, you need to discuss technology and advanced features using an evidence-based approach. Relating the results of the COSI to levels of technology is another effective tactic for this step of the fulfillment stage.
Step 5: Offer Choices
During this phase you recommend between two and four models for the patient to choose from. It is very important to write the options down, so that the patient can clearly see them.
Recommendations should be communicated in a top down fashion. This means that you begin with the highest technology and work down from there. Be sure to write down the price with each level of technology you are presenting.
Price points are important. You need to make sure that you are presenting your recommendations at two to four specific price points, corresponding to the level of technology. Price points should be separated by between $500 and $1000.
Even though you are discussing technology options, you are still educating the patient about how technology will improve their ability to communicate in everyday situations. Relate the features at each price point to the expected benefit they should receive. Use the information you wrote on the COSI as a guide.
Be sure you show them the non-discount value at all price points. This will help the patient see how much money they may be saving with certain discounts you are currently offering. Also, to avoid the perception of haggling, ask the patient if they have any other coupons or offers that will help them save some money.
Once you have finished educating the patient, make a recommendation in writing, including the price. Simply wait for the patient to respond once you have made the recommendation. Talking too much during this step can lead to confusion and apprehension on the part of the patient.
Step 6: Overcome Objections and Ask for the Business
Chances are great that you will encounter at least one objection, usually involving price. Think of price objections as issues related to value. Perhaps you have not built enough value into the products or services.
Just like everything else, objections can be overcome with a step-by-step process. First, acknowledge the objection. "Yes, Mr. Smith, I understand your concern." Second, respond to the objection in an unflappable and honest manner. "Mr. Smith, the hearing aids are that price because they have the most sophisticated technology on the market." Third, offer the patient something that is agreeable to them. "If we stepped down in price and gave up some features, would that be suitable to you?" Finally, move to the next step. Many inexperienced providers get defensive and actually explain more than necessary. This often results in a lost sale because the patient loses confidence in you.
Objections are as natural as the smell of fresh cut hay. They are simply requests for more information. Your job is to acknowledge them when they come up and work to move the patient to the next step. Objections are expected and really no big deal. In fact, objections can be positive because it means the patient is interested.
Step 7: Reassurance
Once the patient has made a decision on a product and price, you need to take the time to offer some reassurance. Basic psychology tells us that buyers want to feel good about their purchases. During the ear mold impression phase of the appointment, remind the patient what you want your business to be known for. For example, you could say, "I pride myself on having the most satisfied patients, I expect you to leave this office feeling good about your decision to do business with us." Offer them something tangible as proof that their decision was the best thing they could have done.
Click Here to View Larger Version (PDF)
Summary
Although most audiologists have all the essential technical and interpersonal skills to excel in clinical practice, there is a need for a consultative sales system to improve face-to-face communication with patients in a competitive commercial environment. When the two-step discovery-fulfillment consultative selling model outlined here is implemented, audiologists will become more proficient at building relationships with patients and asking for the business at the end of the communication assessment appointment. In a competitive business situation, executing many of the tactics described here can help more patients embrace your mission of providing improved communication through amplification and counseling.
References
Chisolm, T.H, Johnson, C.E., Danhauer, J.L, Portz, L.J.P., Abrams, H.B., et al. (2007). A systematic review of health-related quality of life and hearing aids: Final report of the American Academy of Audiology task force on the health-related quality of life benefits of amplification in adults. Journal of the American Academy of Audiology, 18(2), 151-183.
Dillon, H., James, A., Ginis, J. (1997). Client Oriented Scale of Improvement (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids. JAAA 8(1):27-43.
Publications, Better Hearing Institute. Retrieved September 26, 2008, from www.betterhearing.org/research/
Silman, S., Gelfand, S.A., & Silverman, C.A. (1984). Late-onset auditory deprivation: Effects of monaural versus binaural hearing aids. Journal of the Acoustical Society of America, 76, 1357-1362.


