Editor’s Note: This text course is an edited transcript of a live seminar. Download supplemental course materials.
Today’s course is being offered because we have been listening to you and wanted to answer your questions. The questions we are asked most frequently are, “How do you take what you learned from graduate courses and apply it in a real way?” and, “How can you make tinnitus treatment a successful aspect of your business?” I hope that we are able to answer those questions for you today.
Our goals today are, first, to talk about what patients need from us. Next, we will discuss how Neuromonics can help you take care of your tinnitus patients. We are also going to discuss how you can get reimbursed for these services. With that information, I hope to arm you with what you need to make confident, practical treatment recommendations and give your patients hope, because that is often what they are seeking most. Tinnitus can be a hopeless condition. These individuals have not been afforded many great opportunities for improvement in the past, and your role in this process is extremely important.
Lastly, I hope to help you empower your patients to overcome their individual tinnitus challenges. These patients present all over the board, and their needs can be very specific and individualized. I hope that we can better understand our patients and, as a result, best meet their needs for tinnitus treatment.
What do Tinnitus Patients Need from Us?
Let’s first discuss what these patients experience. I think this is the best way to start this conversation about the emotions that these patients experience as a result of their tinnitus perception. If you are currently seeing tinnitus patients, you know they have a lot of fear associated with their tinnitus. Where does it come from? Many times it comes, seemingly, out of nowhere. They do not understand why they are having to contend with this sound that is often very loud and difficult to escape. Anxiety is another common experience. Is something more serious wrong? We need to help them to navigate those issues with an appropriate medical workup. I cannot emphasize enough the feeling of hopelessness these patients experience. They feel it is never going to get better. They may have already seen several medical professionals and have been given, sometimes, very little information and not many options of what to do about it. This piece of the puzzle is incredibly important for them.
Anger is another strong emotion many experience. Why did this happen to me? They can be bitterly focused on that. What did I do? They may spend a lot of time thinking about what concert they went to or what antibiotics they ever took. They analyze specific events that may have triggered all of this. It is important for us to understand that and to have empathy. They feel a loss of control and think, “Nothing I do makes this any better.” Many of these patients spend much of their time trying to escape the sound. They have tried lots of different things before coming into your office and can be quite skeptical. It is our role to be confident in the information we are giving them, as well as the treatment options.
Information
I can say the most important thing that we can give our patients is good information. I say that because there is a lot of inaccurate information out there, especially on the Internet. We want to make sure that they have a good understanding of the condition and have an overview of the tinnitus neurophysiological model. We also want to reassure them of the prevalence - the commonality - of this condition. The American Tinnitus Association (ATA) reports that more than 50 million Americans have tinnitus, but we also need to discuss what makes them specifically different from all the other millions of people who have tinnitus. Ultimately, we need to remove the mystery and weaken the fear and anxiety that they are experiencing. You can do that by giving them an understanding of where their tinnitus comes from and also giving them clear and concise treatment options. Importantly, you need to reassure them that you are going to figure it out together; this is a collaborative process. We need to better understand them and how their tinnitus impacts them so that we can come up with the best treatment solution.
Figure 1 is an illustration of the neurophysiological model of tinnitus. If you are already a tinnitus practitioner, I am sure you are familiar with it. I think it is a great slide for you to give to patients so they have more of a concrete sense of the elements involved in tinnitus. I first start out by telling the patient that there are three elements involved in tinnitus. One has to do with the auditory system, where there is damage, and the brain is working to fix that or compensate for it. In so doing, the tinnitus signal is generated. It is the brain trying to help you, and this sound is perceived.
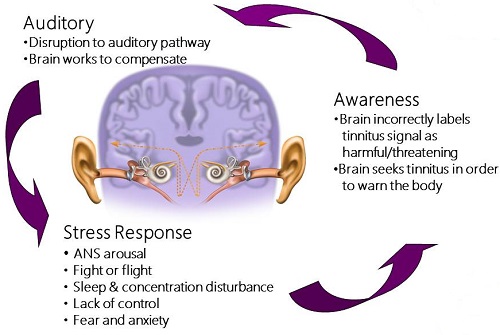
Figure 1. Illustration of the neurophysiological model of tinnitus.
Next is the awareness piece. For whatever reason, your brain has incorrectly labeled the tinnitus signal as something harmful or threatening. Because of that, it is searching for it much of the time. That is the reason they hear it so much, because of the negative categorization the brain has placed on it. I think a great example is a fire alarm. We all know what that means when we hear it. It means, “Get out of here. There is a problem.” That is pretty much what these patients are experiencing with tinnitus, but they have no way to turn it off. Many times they have very little control over it.
The last piece is the stress response. This is where the autonomic nervous system is activated and goes into fight-or-flight mode. It has a functional impact of the patient. It is not a choice to feel this way. This is a true physiological response; the heart rate and respiration quickens. This is where you get sleep and concentration issues, the sense of lack of control, fear, and anxiety.
These three elements serve to feed on each other, and this is what can progressively make tinnitus more of an issue for our patients. Some of them are so afraid that it is because their hearing is getting worse or they are causing more damage to their hearing, and really it is the stress response that is growing and having more of a functional impact on them.
Listen
One of the most important things we can do for our patients is to listen. We need to listen to how their tinnitus is affecting them daily so that we can determine how we can best help them. There are a number of wonderful tinnitus questionnaires and inventories, such as the Tinnitus Reaction Questionnaire (TRQ), the Tinnitus Handicap Inventory (THI), the Tinnitus Functional Index (TFI), and I am seeing more and more clinicians starting to use some depression and anxiety scales to better understand the full impact of tinnitus. All these questionnaires can be helpful, but they are still questionnaires with numbered rating scales. In order to have a more comprehensive understanding of your patients, I suggest giving some open-ended questions as well. This can be done during your interview with the patient, during the initial tinnitus assessment, or in a handout that is provided prior to the appointment so the patient has ample time to fill it out.
Following are some of questions that can be most helpful at getting to the heart of what is happening with your patient. First, “If you did not have your tinnitus, how would life be different?” You are not qualifying good or bad, just how it would be different. They will describe to you what specific areas are affected. “How does it affect you?” “How often does it affect you?” This helps you learn about their tinnitus awareness and how much of the time they hear it. “How does it affect your family?” I think that issue is overlooked sometimes. We know how hearing loss can affect other family members, but tinnitus can as well. These patients tend to be tense and more easily agitated because they are so disturbed by their tinnitus. I also recommend that family members come to the initial tinnitus assessment or evaluation appointments so that you can have that full discussion.
You can also ask, “Do you feel your tinnitus interferes with your ability to understand conversation?” I think many patients confuse their hearing loss with their tinnitus. They say, “If I didn’t have this ringing in my ears, I would be able to understand better.” Hearing is a separate issue. We want to separate those two problems and make sure that we are recommending options appropriately. Next, “Are there any places or activities that you avoid because the situation is too loud?” We are getting at hyperacusis or decreased sound tolerance here. That is another issue that can go under the radar. Patients often have control over their environment, the places they go and the activities that they do, but they cannot control the tinnitus as much. “We don’t go to restaurants after 5 pm. We don’t go to concerts anymore.” Lots of red flags can come up that way. This is a great question to ask all of your tinnitus evaluation patients.
Then simply ask, “What are your goals for treatment? What do you want out of this? What can I do for you?” This way you can better understand why they are there and whether they have realistic expectations for the process. If they immediately say, “I want a cure. I want it to go away,” you know they are not realistic yet. Most people, if it is quiet enough, can perceive their tinnitus. But knowing what they want and expect is the best way to understand where your patient is, emotionally and physically, and how you can begin to help them.
Focused Treatment Plan
Obtaining treatment is ultimately why patients are in your office in the first place. With this treatment plan, we are going to provide them with a road map for success. I try to make it as concrete and black-and-white as possible. That way you can track your recommendations, what has worked, what has not worked, and you can troubleshoot and change things along the way. Sometimes that includes lifestyle changes. If they have a particularly harsh lifestyle, we will need to ask them to do things that will mitigate that. Sometimes that has to do with their work or taking time to do things that are enjoyable. I am guilty of this myself, where we get so caught up in the day-to-day of work, family, kids and their activities, and we do not take time for ourselves. That is hugely important when you are trying to affect changes in tinnitus. Patients need to give their body a chance to regenerate and relax. I will also talk about any referrals we need to make (i.e., psychologist, ENT, or dentist to address TMJ), so we can be sure we are approaching tinnitus management in a comprehensive way.
I have provided a guideline for that treatment plan in Figure 2. I like to come up with three or four tinnitus objectives so that we know what we are going to be working on together, and then we outline steps to achieve those objectives. This gives them some real-life suggestions. This may have to do with whatever product you choose or whatever lifestyle changes that need to be made, but you have it written in black and white. The patient understands what we need to do to make the changes we are looking for.
Figure 2. Guideline for tinnitus treatment plan.
Next is product implementation. I think it is important for patients to understand why one product is their best option. Why did we recommend this for them? That has to do with their particular needs and characteristics as far as hearing, stress, sound tolerance, individual tinnitus impact, how it is affecting them, and the clinical evidence. Why is this going to be the most effective solution for you? We do this so patients can have confidence in the process. You are also building their confidence in you, as the expert. They are coming to you for that solution and we need to be clear about how we are going to help them so they understand point of all this and the end result.
Neuromonics
Let’s talk about Neuromonics and how it can help you in treating your tinnitus patients. Neuromonics focuses on four key elements of sound therapy. First, we need to reduce the attention drawn to tinnitus. Next, we need to reduce loudness of the tinnitus, and substitute a less disruptive noise for an unpleasant one, being the perception of tinnitus. Lastly, we also need to give the patient a sense of control. Neuromonics uses music as the vehicle to accomplish these objectives.
In our mind, there are two types of patients. There are patients who can benefit from complete masking, which renders the tinnitus inaudible. That gives them situational relief while they are listening to the device. These would be patients with low tinnitus awareness and disturbance. Our Sanctuary product would be most appropriate for this. We launched this new product at the American Academy of Audiology’s (AAA) expo this year for patients who are on the lower end of the tinnitus disturbance scale. I, myself, have had tinnitus for a long time. There are only specific situations where my tinnitus impacts me. I am able to use the Sanctuary device, get the relief I am looking for at those times, and get on with my day. I am not aware of it a lot of the time, but during those specific situations, I am looking for the relief. That is what these patients are looking for.
Next we have patients who are better-suited for partial masking, which results in a perceptual change in tinnitus as the tinnitus is reduced in prominence. This end goal is habituation. These are patients who have a high tinnitus awareness and are more impacted by their tinnitus. More of their everyday activities are affected by the tinnitus, and they need more of a formal treatment approach. That is where the Oasis comes in. Of course, not everyone falls into these neat categories. That is where our open-ended questions come and tinnitus inventories come into play, but I think it is helpful to break them up into these two categories so that you can understand candidacy and when to use each product.
Our clinical data for Neuromonics can be found in Figure 3. I think it is important to share this with patients because it is substantial. We have data on over 900 patients with success rates from 72% to 96%. We have more data than any other product or therapy out there. This goes a long way for patients so they can understand that this has been clinically tested and proven as an effective treatment for tinnitus. Sharing this data can help patients understand why you are recommending it as a potential treatment option for them.
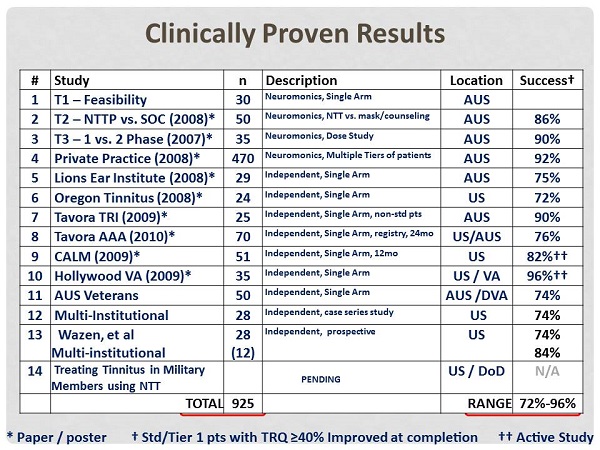
Figure 3. Summary of 14 clinical trials with Neuromonics and the success rate.
Neuromonics uses music as the vehicle for the therapy. Music has been shown to be extremely effective in treating anxiety as well as in managing chronic pain disorders. It is a perfect carryover to tinnitus. Anxiety is a big part of what these patients experience. Music also has a direct path to our limbic system, which is where we process our emotions. That is a big part of the neurophysiological model. Those of you who have used Neuromonics have seen the profound relaxation response the stimulus has on patients. These are patients who have been able to achieve very little relief from their tinnitus. They have been searching for something and have tried so many different things. You give them the Neuromonics stimulus and let them listen to it. I love to see it. Their eyes close. They sit back in their chair. They relax, and that relaxation response is extremely powerful. I feel like that is a big part of why we are able to be so effective with treatment.
Music also activates our sympathetic nervous system. Tinnitus activates the autonomic nervous system fight-or-flight stress response. The sympathetic nervous system slows the heart rate and respiration so that you can counteract that stress response. We all know music that helps us to do this. Music has also been found to be equivalent to progressive muscle relaxation training, which is a common therapy technique used in managing anxiety disorders. It has a perfect application here. These patients tend to be anxious.
Further, music has been found to be preferable for tinnitus treatment instead of noise. There tends to be greater acceptability to music. They like it because it is pleasant to listen to. It is helpful in that respect. Also, music has complex temporal qualities that provide a greater distraction from tinnitus than noise. This makes sense. What is going to distract you from your tinnitus more: white noise, which is straightforward, or music, which requires more brain processing, at a higher interest level? Music can provide a greater distraction from the tinnitus.
Many patients ask, “How is the Neuromonics stimulus different?” It is important for you to be able to explain this to your patients. First is the spectral modification. We are shaping the music based on the patient’s audiogram. That allows us to do some important things for the brain. To start with, you are feeding the auditory system exactly what it is looking for. The pink rectangles in Figure 4 show the frequency response of a typical piece of music. Music typically has a low-frequency bias and very little energy in the high frequencies. Most of these patients have hearing loss as well as a tinnitus perception in the high frequencies. If they use an iPod, they turn it up and up, trying to get relief from the tinnitus. It is typically too loud before they are able to get the relief they are looking for, especially when you consider that most of these patients have some sound tolerance issues.
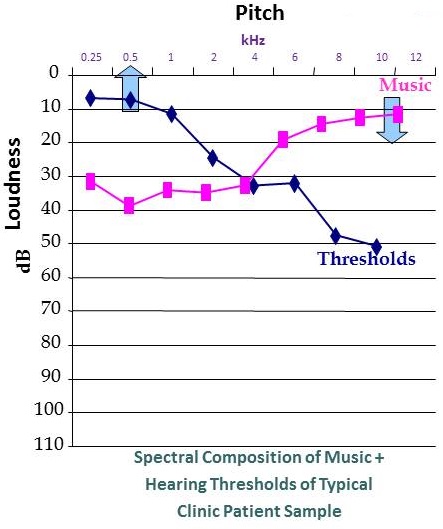
Figure 4. Spectral composition of music (pink) compared to a typical sensorineural hearing loss.
We are also providing a wide frequency stimulus out to 12.5 kHz. That is very important in this process. We do that because research shows that if you feed the auditory system the sound it is searching for, you can facilitate neurological changes in the tinnitus. You can actually turn it down. We are able to see that through the minimum masking level measurement we do during the tinnitus evaluation. That number should wind down over the course of the therapy if the treatment is effective for the patient. That is just another objective measure that we look for in this process as a benchmark for success.
We are also providing maximum stimulation of the auditory pathways. With Neuromonics, we are not only treating the reaction to the tinnitus, but we make them feel better. We give them the relaxation and relief from the tinnitus that they are looking for. We are also treating the tinnitus directly by stimulating those areas of the auditory system; we do that because of the supporting research.
I also want to talk about the impact of customizing the music for the patients’ audiograms. Once that process is complete, patients were able to get tinnitus interaction at a much more comfortable listening volume; on average, it was 16 dB less. Think about it - you are trying to help a patient sleep, relax or concentrate. That is not going to happen with a loud signal blaring in their ears. Being able to provide affective tinnitus coverage at a much lower listening volume is critical to meet those patients’ needs.
We have also found that speech intelligibility was preserved by customizing the music. The low frequencies are not being blurred out and most patients are able to carry on a conversation with the Neuromonics devices on. Of course, with asymmetrical losses, that is much more difficult, but most patients are able to use the device seamlessly and fit it into their day-to-day activities.
How does Neuromonics work in treating tinnitus? Remember the three aspects of the neurophysiological model: the auditory, the attentional, and the stress response. For the auditory portion, we have talked about wide frequency stimulation and the customization for the patient’s hearing. We are treating the tinnitus, stimulating the brain, and giving it what it is looking for. We are also treating the emotional reaction, or the stress response. The music has been chosen for its relaxation properties. It mimics the resting heart rate. For those of you who have not seen it, I would encourage you to demo the device on your next tinnitus patient to see what they think. My experience has been extremely positive.
Last is the attention portion, or the awareness in helping patients to habituate. That is a feature primarily available in the Oasis product. Nonetheless, we are working to re-train the brain. It is still going to perceive the tinnitus, but it will work to ignore it and filter it out into the subconscious, like all the millions of patients who have tinnitus and do not notice. That is what we are working to do with Neuromonics treatment.
Oasis and Sanctuary
Here is a quick detail of the two products. The Oasis has been our gold-standard product to date; we have been in the United States since 2007. Oasis is a two-phase formal treatment protocol working to facilitate habituation to the tinnitus. We are not only treating the disturbance by helping them to manage the impact and how their tinnitus affects them, but also working to facilitate habituation where tinnitus is not in the forefront of their attention. It is an individualized, ear-specific stimulus to account for asymmetries in hearing. These patients can even have a dead ear, and we can treat them with our contralateral prescription. The Oasis provides data logging, as well as four musical programs. That music has been chosen for its relaxation properties, mimicking the resting heart rate to give these patients a profound relaxation response and relief from their tinnitus. The Oasis has been designed more for the moderate-to-severe tinnitus patient who has daily tinnitus impact and needs a more formal treatment protocol.
Next, let’s talk about the Sanctuary. The Sanctuary is a single-phase device. We have pared down what we know works with the Oasis into the Sanctuary, and provide it for those patients who are on the lower end of the disturbance scale. The reason we created the Sanctuary is because we realized there was an entire subset of patients who do not need hearing aids, or maybe they are not getting the relief that they are seeking from hearing aids. They still need an effective product to help them to manage their tinnitus. The Sanctuary is a semi-customized device that provides three fitting ranges. It also follows a quick patient delivery model. There is no software required. It has an entry-level price point, which our providers and patients love. We have been fitting it on patients since March 2013, and the results have been fantastic. If you would like more information on those specific results, I would be glad to share that with you. Our clinicians have been very kind in sharing their personal experiences, and I would love to pass that along to you.
Case Studies
I thought it would be helpful to discuss a couple of patient cases so that we can determine candidacy and think about treatment plans.
Case #1
This patient scored a 20 on the TRQ and reported a tinnitus awareness of 75% and disturbance of 50%. Here are some of their answers to the open-ended assessment. The patient is having trouble falling asleep. He wakes up several times during the night and finds it very difficult to go back to sleep. He is extremely tense at work. He has difficulty accomplishing deadlines and meeting objectives at their job. He avoids restaurants after 6:00 pm because they are too noisy and unpleasant. Both the spouse and the patient admitted to being very tense at home. The spouse reported feeling like they are walking on eggshells to not make too much noise because the patient was so tense. The patient found the tinnitus to be very distracting, making it very difficult to focus on conversation and interact with the family. This is significant. It is affecting him at home, work and social activities.
The audiogram from the left ear was normal. The audiogram from the right ear had a mild precipitous loss. The loudness discomfort levels (LDLs) were all below 90 dB, which is evidence of some decreased sound tolerance, consistent with what he reports about avoiding the restaurants.
First I would ask, does the TRQ score of 20 match up with the open-ended responses? I cannot tell you how many times I have been in a tinnitus evaluation where the TRQ says one thing but the patient says something totally different. We have also seen clinicians fit a patient based on the TRQ and then after the fitting, all these other issues start to come up that they never talked about during the assessment. Those open-ended questions can save the day. Do you think that there are enough quality-of-life factors to warrant formal treatment protocol in this patient’s case? I would say absolutely. When your livelihood is affected, it is a big deal. Also, do not overlook the decreased sound tolerance. That is going to affect how you treat the patient. The Oasis includes a hyperacusis protocol, which would be used as an off-label approach. Neuromonics has been shown to be extremely effective in helping patients with improving their tolerance to sound.
The other piece he reported during those open-ended questions is that he wanted a cure. Red flag! That is certainly an opportunity for counseling regarding realistic expectations, but it also tells us that he is looking for habituation. He is hearing the tinnitus much of the time, and he wants treatment. Based on that information, what product would you recommend? I would say the Oasis.
The patient’s tinnitus impact goes well beyond situational relief. He is affected much of the time in work, social situations, and at home. He needs a more formalized approach to treatment. We need to work specifically on conditioning the brain to lose the stress response, and then we need to work on his goals of habituation. With the Oasis, we have that two-phase protocol. We also have data logging, which is extremely helpful in guiding his usage, optimizing results, troubleshooting if he is not meeting the appropriate benchmarks, and addressing decreased sound tolerance. You can see from the data logging at what volume they are listening, and make recommendations accordingly. I have seen many patients with hyperacusis and looked at their data logging. All they did was turn it on; they did not even turn it up. You are never going to get anywhere near addressing the stress response because they are not getting relief, but they are not able to tolerate the sound. We definitely need to implement that hyperacusis protocol and build some extra time into treatment to address the hyperacusis effectively before we can address those tinnitus goals. The Oasis is also programmed to address asymmetrical hearing so that it can provide that truly balanced surround sound, which helps with coverage interaction with the tinnitus. That is why I think the Oasis would be the best choice for this particular patient.
I wanted to provide a sample treatment plan (Figure 5). I picked two of his goals, and then provided some suggested steps to achieve those objectives. You can print this out and give this to a patient so that you are on the same page. This also helps to keep the patient on realistic ground. The example I use over and over again is patients with hearing loss who cannot hear thunder, but now they want to hear grass grow with hearing aids. They do not remember how much their hearing was impacting them before they started their hearing aid use. The same thing goes for tinnitus. They come in. They are not sleeping. They are short with their wives every time they turn around. They are easily agitated. We have started treatment and those things start to subside. Now their goal is to never hear their tinnitus again. Remember that is not a realistic expectation. If you can put together these objectives in black and white, both you and your patient are on the same page. You can check in with the data logging to see if they are actually following your recommendations. If they are and it is still not giving the results that both you and the patient are looking for, then you need to move to plan B, and work with a different set of suggestions. This helps to navigate the treatment process.
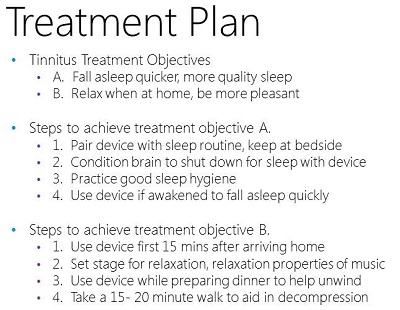
Figure 5. Sample treatment plan for Case #1.
Let’s look at Objective B (Figure 5). The patient wanted to relax when at home and be more pleasant with their family. We suggest using the device the first 15 minutes after they arrive home, setting the stage for relaxation, winding down and having some decompression time. Maybe they use it while they are preparing dinner to help unwind. Also, they may have to implement a lifestyle change, such as taking a 15- or 20-minute walk after dinner to aid in that decompression. We have to provide not only device usage suggestions, but also give lifestyle changes, real-life activities, or things they can do to make changes in their tinnitus. As we know, there is no silver bullet to anything we do. We need to look at things from a global perspective and help them to manage it as effectively as possible.
Case #2
Let’s look at our next patient. There is a TRQ of 15. Their tinnitus awareness is 20%. Their tinnitus disturbance is 80%. Here are some of their answers to the open-ended questions. They have some difficulty falling asleep from the tinnitus a few times a week. They have difficulty concentrating at work. They find the tinnitus distracting, but they are okay. They are finding it hard to relax, and ultimately they would like relief from their tinnitus. Their audiogram is a mild to moderate precipitous, symmetrical loss for both ears. They wear hearing aids but still find the tinnitus bothersome. However, the tinnitus seems to be bothersome only when the hearing aids are out and they are trying to fall asleep, and also maybe in quiet where the hearing aids do not amplify much. Their Loudness Discomfort Levels (LDLs) were normal above 90 dB. We do not have to worry about sound tolerance with this patient. What would you select?
Based on this information, I think the Sanctuary would be a good product. They need effective relief to disengage the limbic system. They are having a stress response as a result of their tinnitus perception. The Sanctuary will give them the ability to relax during those specific situations at bed time and to concentrate at work. This patient has a low tinnitus awareness, so we are looking to address specific situations and activities that are impacted. He has symmetrical hearing and normal sound tolerance. The Sanctuary would be a great option for him. We did a demonstration with him in the clinic. He loved it, and has been using it during these specific times and doing great.
Figure 6 shows a sample treatment plan for the Sanctuary patient. There are the treatment objectives, and then some of the steps to achieve those treatment objectives. Let’s look at Objective B, concentration at work. The steps to achieve this objective are to use the device at work while at the desk using headphones or a speaker. The Sanctuary has an auxiliary rechargeable speaker that can be ordered as an additional accessory for $45. It can be used at a desk or even bedside. We will also suggest that the patient does not fight through their tinnitus. He should try to use the device as soon as the tinnitus becomes bothersome. He should take breaks after long meetings. That is one of the times that he was most impacted by his tinnitus - when having to concentrate. He also wears hearing aids, and I am sure he was straining to hear at times during those meetings. He should take breaks to use this device, get back on top of his tinnitus, feel better, and address the stress response so that he can go about his day. We should be as specific as possible when writing objectives for the patient.
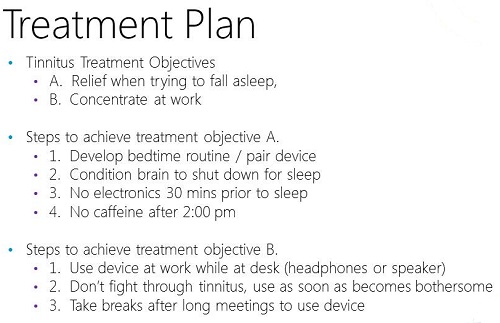
Figure 6. Sample treatment plan for Case #2.
Reimbursement
With that accomplished, let’s look at reimbursement. I am sure you would agree that this is important. We need to be able to be reimbursed, not only for the assessment and the device, but also the treatment services that we provide. That can be a gray area for a lot of tinnitus practitioners. Let’s talk about some of the ways that we can optimize reimbursement.
Assessment
We typically we have very little difficulty being reimbursed for diagnostic testing. That is one thing audiologists can count on. We have codes for that. If you do not file insurance, you need to look at what the typical reimbursement rate is for these codes, and come up with your own charges for this appointment. I would encourage you not only to look at the diagnostic piece, but also the counseling that you do above and beyond the diagnostic testing. That is a service you provide for which you can certainly request payment from the patient. There are not codes that are particularly effective for billing insurance for this, but it is certainly something that you can ask the patient to pay for out of pocket. I have seen these fees range all over the country - from $75 to $200 for the testing. You bill the insurance for the testing and then there is a $75 tinnitus assessment fee. These are suggestions. I would encourage you to look at your own practice. Look at how much you need to charge for your time, and bill the patient accordingly.
Figure 7 shows the reimbursement rate for Medicare 2013 for the diagnostic codes. You can look at around $140 reimbursement if you bill insurance for the testing. You need to think about what you need to bill total, because private insurance carriers often reimburse above this. That way, you are not selling yourself short by billing any of these codes. We wanted to provide you a baseline so that you know what to expect, and we can guide you in being able to charge for these services.
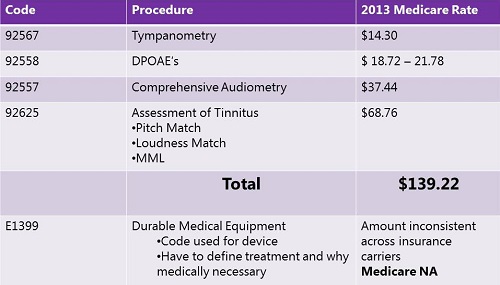
Figure 7. Medicare reimbursement rate for related audiological services in 2013.
Submitting a Claim for Neuromonics Devices
Let’s talk about submitting a claim for both the Oasis and the Sanctuary. We have found through our experience with providers that a successful claim receiving reimbursement for the device needs to include the following components. You need to include a letter of medical necessity from yourself, as the audiologist. I am an audiologist as well, and it is a point of contention, but we have found that reimbursement is also increased if you provide a letter of medical necessity from a physician. This letter should be from the person who saw and tested the patient, and then from the physician, containing their evaluation of the patient. You should have a copy of all clinic and physician chart notes, a summary of all the efforts and appointments the patient has made to get help for their tinnitus, a description of the device you are submitting the claim for, any inventories you used to assess the patient, the tinnitus history, the diagnostic assessment results including the audiogram and the tinnitus assessment test specifically, and a copy of the Neuromonics summary of clinical data. By including all of this, we have found that reimbursement for the device has been fairly consistent. This is, of course, dependent on specific policies and carriers, but we have found a lot of providers who followed this procedure are receiving reimbursement for the device.
The current procedural terminology (CPT) code for the device is E1399, which is a durable medical equipment (DME) code. It is a broad code, which encompasses many different devices. This is why the description of the device that you include in this claim is very important. The insurance company needs to know what the device does. Based on the definition, the Sanctuary should be considered DME.
The problem has been, to date, with reimbursement in the Oasis. It has had limited coverage under the DME provision, most likely due to providers exceeding the typical DME coverage cap of $2,500 to $3,500 per calendar year. This means that most providers have been bundling the device along with their diagnostic services, and that number is above the $2,500-$3,500 cap. We have been seeing more consistent insurance coverage for the Sanctuary because it falls well below that cap. If you would like more specific pricing information, feel free to reach out to me and we will certainly give you descriptions of that. The Sanctuary also falls under our current FDA 510(k) letter clearance, so you can use the same FDA clearance letter, which also that provides additional credibility to the claim. We have all these materials for you in a concise packet to help you to streamline this process and get better reimbursement for the device.
With that being said, how do you get reimbursed or receive payment for the services you provide these patients in your office? As you know, unfortunately as audiologists, there are no good CPT codes available for tinnitus treatment at all. That does not mean that we cannot provide services just because the CPT codes are not there. We are the leaders in providing these patients with solutions to their tinnitus. We suggest that you bill your patient for the counseling and treatment plan that you provide them. Bill the insurance for the device. There is nothing that says that you cannot bill the patient for these services. There are no CPT codes for it anyway. That is the patient’s responsibility. That being said, I have to provide the disclaimer that you must check individual insurance contracts and make sure that you fall within those. This is our basic understanding of how to optimize reimbursement or payment for your services.
If you take an unbundled approach, I think it is wise to tell your patient you are going to bill insurance for the device, but also give them a guideline as to how many appointments you anticipate over a certain period of time for treatment so they can understand the cost that may be involved as they begin this process. I think this is the most successful way to approach this and get paid for your tinnitus services. No one expects you to do this for free. We certainly should not have to.
Cite this content as:
Keaton, C. (2014, January). Embracing the tinnitus patient: making treatment and reimbursement a practical reality. AudiologyOnline, Article 12420. Retrieved from: https://www.audiologyonline.com

