Most audiologists have been trained to diagnose hearing disorders and treat hearing loss with non-surgical intervention. No one would argue that audiologists are the best-equipped professionals for executing these important tasks. There are other intangible skills, however, such as asking patients to do business with us, which many audiologists have not been equipped to address. Sadly, the best academically trained audiologist can struggle in a clinical situation without some appropriate training in the commercial aspects of the business. The aim of this paper is to assist the audiologist, who may be working in a commercially oriented practice for the first time, to not only survive, but also thrive.
Before reviewing some actionable closing strategies, let's first try to gain a better understanding of what "closing" really is. Although the term "closing" has many negative connotations, it aptly describes the final stages of any consultative appointment involving a financial commitment from the patient. For the audiologist, "closing" boils down to gaining an agreement from the patient to do business with you. This usually, but not always, means that the patient has decided to make an investment in hearing aids. Although this financial transaction is important, from a behavioral perspective, an effective close or summary means that you have taken the time to build a personal relationship and establish your expertise with the patient. If you think about it, the essence of professionalism is your ability to establish a trusting relationship and rapport with all your patients. Gaining an agreement is just one small step in the journey you take with every patient you see.
Gaining an agreement from the patient does not happen without managing a series of "next steps." These next steps are all components of an evidence-based clinical protocol. The foundation of any clinical protocol is something we refer to as the Discovery-Fulfillment process. Closing can occur during the very final stages of the Fulfillment process, however, effective hearing care professionals know that you need to be trial closing or pre-closing throughout the prefitting appointment. For example, we know that today's consumer cannot be pressured or cajoled into purchasing products or services (Katzenback Partners, 2007). We know that when you do not take the time to learn the individual communication needs of each patient and educate him or her about the consequences of untreated hearing loss, they are less likely to want to form a relationship or do business with you. Managing the appointment as a series of next steps is a patient-centered way to work together with consumers by addressing questions that arise during the appointment.
Trial closing or "bridging" is an essential tool
Trial closing or pre-closing is simply gaining the agreement of the patient to move to the next step. Another word often used for trial closing is "bridging" which simply means you are linking the various phases of the appointment into a logical sequence of events for the patient. Linking the phases of the appointment helps the reluctant patient have a clearer understanding of how you will be able to help them.
When trial closing or "bridging" is done well, it feels almost as natural as breathing. For example, after you have finished the communication needs assessment using the COSI, simply explain to the patient, "Now that we have finished this part of the assessment, the next step is to get more information about your understanding abilities. Would you please following me this way so I can evaluate your communication concerns?" If the patient follows you to the evaluation area, you have successfully completed a trial close. If the patient hesitates, you have the opportunity to address an objection. The bottom line is that pre-closing transparently moves the patient from step to step with their full support. This full support is the essence of consultative selling, and I have observed that the best "closers" are actually great at pre-closing throughout the appointment. They may trial close five to ten times during the pre-fitting appointment.
The ten phrases in Table 1 are intended to give the inexperienced audiologist some examples of how one step of the appointment is linked to the next by gaining an agreement with the patient. Although it might be tempting to memorize these examples and cite them verbatim at the appropriate time during the appointment, these examples are just that. The statements need to be expressed in your own words. The take home message is that the audiologist, no matter how technically proficient, needs to be able to clearly communicate with the patient and move the appointment along to the next phase with full agreement from the patient. The use of trial closing or "bridging" statements might be obvious, and even simple-minded to some, but it is an essential communication tactic that is underutilized by many audiologists. 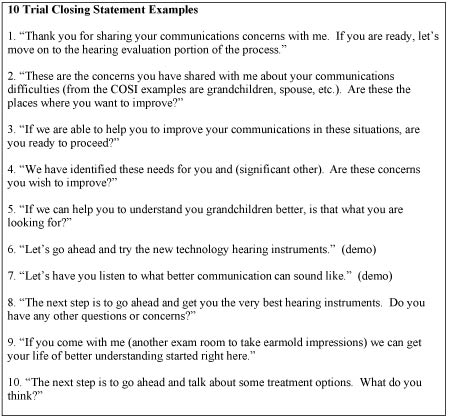
Table 1. Ten examples of how the audiologist can bridge various phases of the appointment by gaining agreement from the patient to move to the next step.
Click Here to View Larger Image of Table 1 (PDF)
Buying is emotional, not logical
Human beings make buying decisions based on emotion rather than logic. For the audiologist, this means that you need to appeal to the patient on an emotional level. This is particularly challenging in our business because much of the communicative assessment is based on science and logic rather than emotion. Audiologists who excel in commercially driven practices are like good actors. Think about a Broadway production that has been running for several months. The actor is likely somewhat bored with playing the same role night after night;however, if you are sitting in the audience watching the six-hundred and forty-second production of Hamlet for the first time, the professional actor will seem fresh and authentic. Over the years, I have observed great audiologists to be much the same way. They are genuinely engaged in the process of delivering high-quality care. Even though they are absolute experts in their profession, their presentation to the patient appeals to the emotions of the patient. The take home message is that the content of your message (what you say) is not as important as the process (how you say it) when working knee-to-knee with patients.
The left side of Table 2 below describes some common logical components of the patient-provider interaction. On the right side of the table, the emotional equivalent is listed. The intent of the table is to give the reader concrete examples of how gestures and vocal inflection, which are the more emotionally-laden aspects of communication, can be used to build trust and rapport with the patient.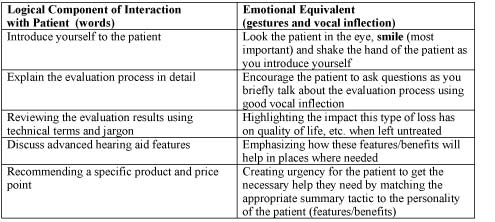
Table 2. A summary of the various logical components of the patient-provider interaction, along with examples of how emotions can be brought into this interaction.
Click Here to View Larger Image of Table 2 (PDF)
One important tool that helps to bridge the logical components of our job with the emotional aspect is our ability to focus on educating the patient about the consequences of untreated hearing loss in a dramatic fashion. Of course, this doesn't mean that you need to be theatrical in your approach. That would be melodrama. By "dramatic" we mean that the audiologist has to be emotionally invested in the appointment. As the old adage goes, "Patients don't care how much you know until they know how much you care." When patients realize that waiting to get help may affect their well being and quality of life, they are more likely to do business with you. Being authentic and appealing to the patient's emotions will create an urgency to receive help from you that day.
Match the closing technique to the patient's behavior
There is a tool that is beneficial to use that comes from basic psychology called the DISC Profile (for more information, visit the publisher's Web site at www.inscapepublishing.com) DISC is a four-quadrant behavioral profile model based on the work of William Marston (1931). DISC profiling is relatively common in business management courses and is thought to be an effective tool for assessing the behavior and interaction of people in specific workplace situations. It can help us determine a patient's general behaviors and match our response to their behavior. Figure 1 below shows the two main axes. On the vertical continuum we have assertiveness and passivity. On the horizontal continuum we have control and openness. Audiologists can rate their patients along both these axes after several minutes of rapport building conversation during the Discovery phase on the appointment. 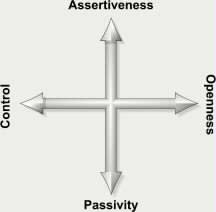
Figure 1. The DISC Profile's two axes of behavioral continuum.
Once we have rated a patient on these two axes, we place them in one of the four DISC quadrants. Each quadrant is labeled in Figure 2. According to the DISC Profile, the quadrant to which the patient corresponds describes their main trait that drives their behavior. Of course, the real challenge for the hearing care professional is using this profiling method as a tool for making a generalization about the motive behind each patient's behavior. This can be especially helpful during the Fulfillment stage of the appointment because you want to be able to address the patient on an emotional level as efficiently as possible. The DISC Profile helps you pick a closing strategy that is more likely to resonate with the patient and appeal to them on an emotional level.
A secondary advantage of using the DISC profiling system is that audiologists who use it have a tendency to be less frustrated in their interaction with so-called demanding patients. The DISC assessment profile, as well as other similar tools, provides the audiologist with an instrument that can help him take conflict less personally. When it is understood that disagreement or conflict largely arises from mismatched social styles between the audiologist and the patient, the audiologist can take the necessary steps to modify his behavior so that the professional relationship can develop.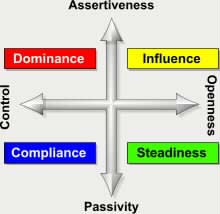
Figure 2. DISC Profile's Four Quadrants.
Figure 3 outlines some of the most important behaviors you are likely to encounter with each of the four DISC profiles. Your job, once you have placed a patient into one of the four quadrants, is to choose the closing or summary strategy that is most likely to have the most emotional appeal to each patient. Of course, there are never any hard and fast rules when it comes to human behavior. The take home message is that the professional needs to adapt their closing strategy to the DISC profile of the patient. 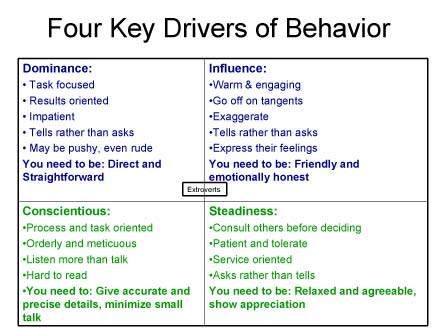
Figure 3. Example of behaviors for each of the four quadrants and what behavior is needed from the consultant to appeal emotionally to the patient. From the DISC Profile.
Click Here to View Larger Image of Figure 3 (PDF)
Figure 4 takes the DISC Profile to a more practical level. Once you have identified the quadrant into which each patient falls, the next step is to match it with the appropriate closing technique. Figure 4 summarizes one example of a closing technique that is likely to resonate with each of the four DISC profiles. Once you become familiar with all of them, take the time to match the closing technique to the appropriate profile.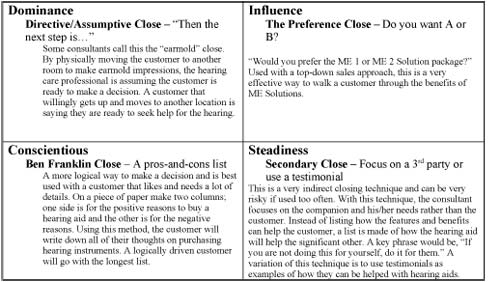
Figure 4. Example of tactics to gain agreement at the end of a hearing aid evaluation appointment for each of the four DISC quadrants.
Click Here to View Larger Image of Figure 4 (PDF)
Don't forget to ask
I have observed that the best "closers" among us ask their patients more than once to do business with them. I have also observed that the professionals who struggle the most with closing simply forget to ask the patient. In other words, they often talk so much that the patient shuts down, and the appointment has no logical conclusion. 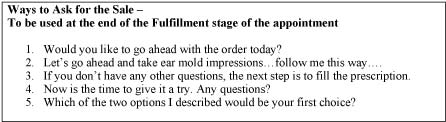
Table 3. Examples of ways to ask for the sale.
Click Here to View Larger Image of Table 3 (PDF)
The Focus of Effective Managers: Behavior = Performance = Results
Business owners and managers of audiology and/or hearing aid dispensing practices often focus on performance and results and forget that behavior (what a person actually does!) is what impacts bottom-line results. Aggregated behavior is performance. It is the manager's obligation to identify behaviors that could be improved, thus resulting in improved business performance. It is a manager's job to encourage this type of thinking and provide coaching and guidance when needed. If you are a practice owner or manager working with a newly graduated audiologist, the following information will be helpful in putting the tactics described in this article into daily practice. If you are an audiologist, these strategies can help you in your role of effectively moving patients step-by-step through the rehabilitation process, and also help you work effectively with your manager in achieving this goal.
The Art of Deliberate Practice
Deliberate Practice is a concept that comes from years of research conducted by Anders Ericsson, first in Germany and now the United States. The central question prompting his research is, "What separates truly outstanding performance from very good performance?" What his research uncovered is a little surprising and has the potential to change the way you think about your own skills and those in your practice (Ericsson, 2007). According to the deliberate practice model, it is not intellect or talent that separates the outstanding from the very good. Instead, outstanding performers practice more effectively. Yes, practice! One of the things managers and staff audiologists can do to truly improve their business is take the time to apply this model.
This can help to bridge one step to the next and make the appointment flow more naturally. It will also give the patient the appearance that you are not being pushy or too aggressive in trying to sell them something. Some people have natural talent;others have to work hard to excel in what they do. Deliberate Practice is something both these individuals need. An example for this is Michael Jordan. Some say he has natural talent. Natural talent helps, but what makes Michael Jordan so great is the hours and hours he spent practicing on the court. Another example is Tiger Woods. He has become a student of the game, analyzing all the aspects of the tournament in which he is he is participating, hole by hole. This is what makes him better than anyone else in the game. We need to look at that same Deliberate Practice in our business.
Outstanding performers have the ability to set specific goals, obtain immediate feedback on their performance, and concentrate on technique. In short, Deliberate Practice is not just for Olympic athletes. It has been shown to be an effective technique for improving the skills of all types of professionals, including health care providers. Here is how it works:
Step 1: Foster a Culture of Self-Improvement
If you are a manager or owner, the first thing you need to do to improve the behavior of your staff. As an audiologist or hearing instrument specialist, you need to examine your behaviors with patients and be open to changing them, if needed. Of course, we are not referring to behavior as manners, but behavior as the observable actions of professionals with their patients. Improving these behaviors leads to better performance. This process starts with a culture where employees are free to make mistakes and are open to discussing the consequences of them. In short, managers and owners need to create an environment that nurtures professional growth and development through self-improvement, and professionals need to be willing to examine and change their behaviors when those changes enable them to grow professionally.
Step 2: Define Ideal Behaviors Needed to Succeed
This step requires that the most attention be paid to detail. Audiologists, like most professionals, have to make important decisions based on less-than-perfect information. One way to reduce the margin for error is for a practice to document all the necessary behaviors in which audiologists engage with patients. Once these behaviors are precisely documented, managers and professionals should discuss and record the ideal behaviors that are needed in order to achieve success. This ensures that expectations are clearly defined, and mutually agreed upon by managers and staff.
Step 3: Set Specific Goals
After clearly defining the ideal behaviors needed to succeed, managers and staff need to identify the gaps between the actual behavior of the professionals, and the ideal behavior that is required to be successful. This is done through observation and self-analysis (by setting specific goals). Once the gaps are identified, measurable and time-bound goals should be established.
Step 4: Focus on Technique as much as Repetition
This statement means that employees need to demonstrate the ideal way to interact with patients. For example, the closing tactics described in this article can be demonstrated to new audiologists by role-playing specific case studies. Managers and employees can do this using a simple 3-step process:
- Describe the ideal behavior. Talk about why and how a certain behavior or skill needs to be conducted in the practice.
- Demonstrate it. Using role-play, managers can demonstrate how the behaviors should be conducted.
- Do it. Allow new audiologists to play the role of service provider.
Mangers need to provide new employees with both positive and constructive feedback. This dialog should be a two-way process, with new employees communicating their feedback openly to managers and business owners. In doing so, both managers and employees are clear on areas that need improvement and on how to go about making changes that enable them to achieve mutually-defined behaviors and goals. Effective feedback is not about focusing on mistakes;rather, it is about how to go about improving them.
References
Katzenbach Partners. (2007). The Empathy Engine: Turning customer service into a sustainable advantage. Retrieved April 15, 2008, from www.katzenbach.com
Marston, W.M., C.King, C.D., & Marston, E.H. (1931). Integrative Psychology: A Study of Unit Response. London, England: The International Library of Psychology.
Ericsson, K. A. (2007). Deliberate practice and the modifiability of body and mind: Toward a science of the structure and acquisition of expert and elite performance. International Journal of Sport Psychology, 38, 4-34.

