Editor's Note: This is a transcript of the live seminar presented on October 11, 2011. To view the course recording, register here.
A pdf of Dr. Bankaitis' slide presentation from the live seminar is available for download here (PDF). The next course in this 2-part series, Infection Control Part II: What Audiologists Need to Do, is available as a recorded course and as a text course on AudiologyOnline.
Today we are talking about why audiologists need to practice infection control. If you do not appreciate and clearly understand why infection control is a necessary component of audiology best practices, the chances of implementing an infection control plan are very low. The goal of today's presentation is to review necessary information that will enable you to answer the following three basic questions: what is infection control; why should we, as audiologists care about infection control; and, how do you initially prepare for creating and implementing infection control in your clinical practice? There will be an Infection Control Part II course to follow today's presentation that will focus on what audiologists need to do. That information will be most meaningful only when audiologists first understand why we need to do it.
Infection Control
First and foremost, what do we mean by the term infection control? Infection control, as defined by Bankaitis and Kemp (2003; 2004), refers to the conscious management of the clinical environment for the specific purposes of minimizing or eliminating the potential spread of disease, regardless of how remote that possibility may seem. This definition is very straightforward. As a result, clinicians quickly jump to the conclusion that integrating an infection control plan will be equally as straightforward. While creating and implementing an infection control plan is not rocket science, particularly with all the recent availability of practical resources with direct applications to audiology, it is a process that does require conscious management of the clinical environment. Infection control is a cognizant, premeditated process that requires thinking through clinical procedures and assessing how those procedures may need to be modified in order to minimize the potential spread of disease.
It is usually at this point, however, where audiologists become very frustrated. It is annoying and frustrating to now suddenly be forced to think through clinical procedures that have become automatic. Furthermore, there is a tendency to overthink the entire infection control process to the point where you conclude that the only way you are going to be able to achieve the goals of an infection control plan is to basically come to work wearing a hazmat suit. Once we reach this point, the path of least resistance naturally leads us to abandon infection control efforts altogether and erroneously interpret them as unnecessary. The good news is that this sort of infection control rollercoaster is a natural progression in the learning process. Hopefully with the information covered in this presentation, as well as in Part II, you will have the necessary information and tools to create and implement an effective infection plan into your current practice with minimum frustration.
Now that we know what we mean by infection control, the next logical question you should be asking yourself is, "Why should I care?" In order to fully appreciate why we, as audiologists, must be aggressive and committed to the infection control process, we need to have a basic understanding of how the immune system works. We also need to understand the Human Immunodeficiency Virus (HIV) and how it actually affects the immune system. We need to take a few steps back and reflect on some of the big lessons that we actually learned from HIV, because it changes everything about infection control. Finally, I want to share with you how all of this information actually does apply to the audiology setting.
The Human Immune System
Human beings are continually challenged by micro organisms that are readily found throughout the environment as different bacteria, viruses and parasites that vigorously pursue a resource for growth and reproduction. Unfortunately, our bodies serve as perfect incubators for these potentially infectious micro organisms. Virtually all cells of the human body remain susceptible and vulnerable to these micro organisms. As such, it is the job of our immune system to defend and protect us from these micro organisms and associated infections. Just like your nervous system, the immune system is not comprised of a single organ. Rather, it is an extremely complex and sophisticated network of organs and cells that work in an orchestrated manner to protect us from infection.
Natural Immune System and Adaptive Immune System
At this point you may be curious how the immune system actually accomplishes this task. The immune system may be thought of as two major sub systems, the natural immune system and the adaptive immune system. The natural immune system provides us with the first line of defense against any type of micro organism. It is represented by a variety of physical barriers, cells and other soluble factors that are designed to react to all infectious agents in the same way each and every time, without any regard to the structural or chemical property of that agent. For example, your skin serves as a preliminary barrier to any type of micro organism, regardless of whether that micro organism is an innocuous bacterium, infectious virus, some sort of parasite or fungus. Because the natural immune system responds in such a nondiscriminatory fashion, it defers to what are called nonspecific immune responses. Although relatively effective, the nonspecific immune responses that are generated by the natural immune system are not foolproof. Nearly all micro organisms have evolved, revisionary systems such that the natural immune system can only effectively provide protection from disease for a few days. As a result, the human body relies significantly on the adaptive immune system to defend and protect us from infection.
The adaptive immune system involves the meticulous recognition of antigen. Antigen simply refers to any substance or molecule that the adaptive immune system interprets as being foreign. When the adaptive immune system detects the presence of antigen, it calls upon different groups of immune cells to help neutralize and kill that antigen. Each specific group of immune cells is designed to accomplish very different, yet very specific, functions. As such, the adaptive immune system generates specific immune responses. We are going to dissect some of the specific immune responses that are generated by the adaptive immune system, but before we do that we need to have a better appreciation of the general anatomy of the adaptive immune system.
The organs of the adaptive immune system are positioned throughout the body, and they include: bone marrow, the thymus, lymph nodes, spleen, tonsils, adenoids, appendix and clumps of lymphoid tissue located in the small intestine that are referred to as peyer's patches. Bone marrow refers to the soft material that is found within the hollow shafts of bone. In contrast, the thymus is a small butterfly-shaped organ that is located slightly above the heart. Both the bone marrow and the thymus are locations where these specialized immune cells of the adaptive immune system develop and mature. Once these immune cells develop and fully mature, they assemble in the lymph nodes, which are located in the armpit, the neck, the abdomen and the groin regions. While the immune cells of the adaptive immune system mainly congregate in the lymph nodes, they do continually mobilize throughout the body via two interconnected systems, the lymphatic system and the bloodstream. I want to talk about both of these systems briefly.
Lymphatic system and bloodstream.
Let's talk first about the lymphatic system. The lymphatic system is a network of vessels that is responsible for channeling the clear tissue bathing lymph fluid to the lymph nodes. Keep in mind the lymph fluid is saturated with adaptive immune cells, so as the lymph fluid is channeled to the lymph nodes, the lymph nodes work as little filters designed to detect the presence of antigen. Sometimes when you are getting sick you can actually feel your lymph nodes swell up. This is a very good indicator that our adaptive immune system is preparing to fight off a potential infection by generating some of the specific immune responses. From the lymph nodes, the lymph fluid is directed to flow towards the chest where it is going to empty into the bloodstream by way of the thoracic and lymphatic ducts. Once liberated in the bloodstream, the lymph fluid is eventually reabsorbed by the body, organs and tissues, and the lymph fluid is once again redirected to flow throughout the lymphatic system. In other words, immune cells of the adaptive immune system are designed to continually flow throughout the body. As a result of these brilliant connections, immune responses that were generated at one specific area of the body will ultimately be dispersed throughout its entirety. It is a wonderfully efficient and effective system designed to protect us from infection. However, these systems actually serve as a double-edged sword.
Because of these very same connections, what we do at the level of a patient's ear cannot only affect the health of the ear locally, but given the right conditions, it can affect the health of our patients systemically. This is a critical concept to appreciate and recognize, because it drives home the point that what you, as an audiologist, do or do not do from an infection control perspective in your clinical practice can certainly impact the overall health of your patient. In addition to the lymphatic system, as previously mentioned, the immune cells of the adaptive immune system continually mobilize via the bloodstream.
Erythrocytes and leukocytes.
Our blood is comprised of two very distinct cell populations, erythrocytes and leukocytes. Erythrocytes are equipped with hemoglobin, which is a red-colored protein that gives blood its traditional red color, so as a result these cells are more commonly referred to as red blood cells. In contrast, leukocytes lack hemoglobin, so they are colorless as compared to their red blood-cell counterparts. Leukocytes are more commonly referred to as white blood cells. There are several different categories of white blood cells; however, for purposes of our discussion today, we are going to be focusing on a category of white blood cells referred to as lymphocytes.
Lymphocytes are a special group of white blood cells that are responsible for executing and managing all the activities of the adaptive immune system. These are very important cells. There are several different types of lymphocytes but the two specific categories that we need to focus on are the B cell lymphocyte and the T cell lymphocyte.
The B cell lymphocyte develops and fully matures in the bone marrow. An easy way to remember this is that the bone marrow starts with the letter B, which is probably why they are referred to as B cells. The job of the B cell is simply to identify the presence of antigen. As you recall, antigen refers to any substance or molecule recognized as foreign. Once the B cell establishes the presence of the antigen, it is triggered to mass-produce antigen-specific antibodies and send those antibodies throughout the body's fluids so that the antibody can neutralize and kill the antigen.
So the big bad B cell comes in and detects the presence of antigen. Despite the fact that it detects the presence of antigen, it will just sit there. The B cell needs to be triggered in order to start producing antibodies. Once it receives the activation signal, it will then start mass producing the antibody. Then it will send the antibody throughout the body's fluids, or humor, so the antibody can attach itself to the antigen, neutralize and kill the antigen. Another term for bodily fluid is humor. This entire process whereby the B cell mass-produces antibody and allows the antibody to proliferate throughout the body's fluids is referred to as humeral immunity.
Now let's talk about the T cell. All T cells initiate their development in the bone marrow; however, in order for a T cell to become a T cell, it has to pass through the thymus where it fully matures. An easy way to remember this is that thymus starts with the letter T, probably why they are referred to as T cells. There are several different categories of T cells, and for today's discussion we are going to focus on one specific category referred to as the CD4 T cell.
CD4 simply stands for cluster designation 4. It refers to the unique suction-cup-like receptors that are found in the outer envelope on the surface of the actual cell. When you look under a microscope, it is easy to determine that the cell is a T cell because of this unique outer envelope. Like the B cell, the T cell is also designed to recognize the presence of antigen; however, in contrast, unlike the B cell which basically relies on antibodies to do the work, the T cell itself will neutralize and kill the antigen. The CD4 T cell comes in, recognizes the presence of antigen and then, because of its unique outer receptors, actually attaches itself to the antigen and kills it. This process whereby the actual T cell attaches itself to the antigen is called cell-mediated immunity. Recall that the B cell is simply going to be dormant until it receives an activation signal. Once the CD4 T cell attaches itself to the antigen, it sends the B cell the message to start mass producing antibody. The B cell will mass-produce the antibody, proliferate it throughout the body fluids and attach it to the antigen. Because the CD4 T cell is responsible for providing this activation signal, it sometimes is referred to as the T helper cell because it helps the B cell do its job.
Human Immunodeficiency Virus (HIV)
Now that we understand how the healthy adaptive immune system works, let's introduce HIV. HIV is a virus that causes Acquired Immune Deficiency Syndrome, or AIDS. The main cells that HIV targets are the CD4 T cells. You probably already have a good idea of what happens to HIV infected individuals, in terms of their overall immunity. To make sure that we are on the same page, understand that the HIV is the antigen or foreign body. The healthy B cell comes in and it recognizes the presence of HIV. However, since the virus attacks the CD4 T cells, whether it is because there are not enough or they are too weak to generate any kind of activation signals, the virus ultimately leads to the demise of both cell-alleviated and humeral immunities. This patient population is very susceptible to infections, including those caused by ubiquitous or ever present micro organisms that we tend to take for granted on a daily basis.
Now that we understand how HIV affects our immune system, let's reflect on some important lessons learned from HIV. I think the three most important lessons for audiologists to learn from HIV are as follows. Lesson number one, we learned early on during the 1980s that HIV was the catalytic change when it came to infection control. With the discovery of HIV, the concern for cross contamination resulted in the Occupational Safety and Health Administration (OSHA) and other regulatory bodies enacting regulations that provided healthcare workers with guidelines on how to reduce or eliminate exposure to these agents. HIV transformed how healthcare and medical professionals approached infection control. The risk of transmitting HIV in the audiology clinic is extremely rare and remote, however.
Lesson number two we learned in the early 1990s. As audiologists, we began to realize that we provide services, sometimes unknowingly, to the HIV infected population. The HIV and AIDS populations develop various types of hearing loss, and quantifiable audiological changes occur either as direct or indirect consequences of HIV. A direct effect of HIV is that it maintains a preferential affinity to the central nervous system with nearly 100 percent of manifestations involving the areas of the head and neck. As confirmed by histopathological study, auditory lesions have been found throughout the cortical and subcortical nervous system. Because the nervous system is extensive throughout these regions, auditory manifestations are to be expected, and they have been consistently documented throughout the literature in the form of abnormal auditory recordings.
In terms of indirect effects of HIV on the auditory system, ototoxicity and opportunistic infections are two examples of how HIV may indirectly cause hearing loss. With regard to ototoxicity, in the absence of a vaccine the medical management of HIV relies on numerous pharmacological interventions incorporating both FDA-approved as well as experimental antiviral medications. According to the Physicians' Desk Reference (2011) frequent side effects of the antiviral medications include dizziness, hearing loss and vertigo. Furthermore, HIV infected individuals are additionally prescribed medications as a prophylactic or treatment for opportunistic infections. Common medications prescribed in this domain are also associated with hearing loss, tinnitus, dizziness, and decrease in hearing. This patient population is extremely susceptible to opportunistic infections that are associated with hearing loss. Table 1 lists the most common opportunistic infections contracted by HIV infected individuals. Although this table is from 1996, the information remains relevant. The left hand column lists the 10 most common opportunistic infections, whereas the right hand column lists hearing losses associated with each opportunistic infection regardless of the HIV status of the individual.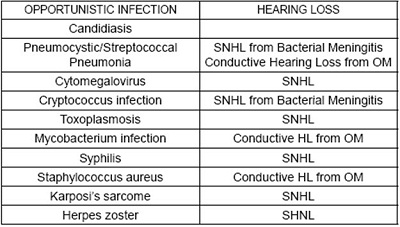
Table 1. Hearing loss types as a result of opportunistic infections in people with HIV (Bankaitis, 1996).
In short, what we learned as audiologists in the 1990s was that the HIV infected patient population was susceptible to developing hearing loss and vestibular disorders. As advances in pharmacological therapies were made, the life expectancy of this patient population increased with many individuals returning to work, seeking opportunities to improve their quality of life. The morale of the story is that audiologists will find themselves in a position where they will be providing services both knowingly and unknowingly to the HIV infected population. From this perspective, infection control arguably became a very important issue in the 1990s for audiologists.
Keeping it Healthy
We obviously no longer live in the 1990s, and the third, and probably most important, lesson we learned from HIV is the one that really needs to resonate with all of you from this point forward. Audiologists are exposed to various micro organisms and various immunocompromised individuals beyond HIV. While the first two lessons we learned from HIV were very HIV-focused, the third lesson brings home the following critical point: Infection control is not about keeping you and your patients safe from HIV. Realistically, there are bigger problems with other microbes that are readily found throughout the audiology environment that you need to be concerned about, particularly on hearing aid devices. Audiologists are routinely exposed to various micro organisms that put us at risk for potential exposures to Hepatitis B, which is a very resilient virus that can survive at least a week in dry blood at room temperature on floors or tables. Exposures occur to other microbes including, but not limited to, candidiasis, various forms of staphylococcus as well as pseudomonas. The recent outbreak of methicillin-resistant staphylococcus aureus (MRSA) reminds us of the importance of infection control in the medical environment.
MRSA is a type of bacterium that is resistant to certain antibiotics, including methicillin, penicillin and amoxicillin. In the beginning, this staphylococcus manifested as a nosocomial, or hospital-acquired, infection and has now found its way into the general population. So just like the 1980s when HIV appeared, now many of us are contemplating what we need to do differently now that MRSA is here. The answer may surprise you.
Basically, we do nothing different than what we otherwise should be doing in terms of infection control. Just as there are other microbes to be concerned about in the audiology clinic there are many other patient populations who do remain susceptible to opportunistic micro organisms. As audiologists, we provide services to a wide range of patients, many of whom exhibit varying degrees of immunocompromise that may be or may not be overtly evident. Geriatric patients are automatically considered immunocompromised, simply because the elderly immune system does not work as well. In addition, any pediatric patient under the age of two is considered immunocompromised because the young immune system does not fully develop and mature until approximately the age of two or later. Patients undergoing or who have undergone chemotherapy or radiation, diabetic patients, or any patient taking medications are all considered immunocompromised because all of those things will affect your immune system. The bottom line is that we provide services to patient populations that are vulnerable to common micro organisms residing in abundance throughout the clinical environment, making it that much more critical to implement effective infection control procedures.
Let's go back full circle and basically ask ourselves, "Why should we care about infection control?" There are a lot of reasons why we should care. First and foremost, infection control is a federal mandate. In other words, it is the law. OSHA is the federal regulatory body that is responsible for overseeing the implementation of safety procedures in the workplace. Infection control falls under the umbrella of safety in the workplace, and as such OSHA has issued specific guidelines on how to reduce the exposure to infectious agents. Audiologists are legally, as well as ethically, obligated to uphold these federally mandated infection control standards, as are audiology students.
Students are not exempt from infection control protocols. Students, whether they have graduated, have a degree or are in the clinic providing audiological services, are considered hearing healthcare professionals.
The second reason we should care is that audiologists do come in contact with bodily fluids and substances on a daily basis during routine procedures. Cerumen is bodily substance, and it is infectious when it combines with ear drainage and pus. Given the viscosity of cerumen, the audiologist is not in a position to determine with visual accuracy whether or not cerumen is contaminated with these things, and as a result cerumen needs to be treated as a potentially infectious bodily substance. Third, audiologists come in contact with numerous patients and reusable objects throughout the day. This is an issue of concern because multiple contacts inherently increase the potential for disease transmission to occur. We need to take a few steps back and have a virology one on one lesson so that we understand how disease can occur.
In order for a microbial transmission to occur, two main things need to happen at the level of the outside environment. First and foremost, a micro organism requires a mode as well as a route of transmission. We will first focus on the mode. Mode refers to how a micro organism travels from point A, the environment, to point B, the human body. There are four general modes of disease transmission and they basically include contact, vehicle, airborne and vector-borne transmission. We are going discuss contact transmission in detail, but to provide some background information, vehicle transmission refers to microbe transfer via exposure to or ingestion of contaminated food or water such as salmonella. Airborne transmission involves breathing in microbes that reside on dust particles or are suspended in the air as droplet nuclei for a long time such as with Legionnaires' disease. Finally, vector-borne transmission involves animals or insects that carry the pathogen and subsequently infect susceptible hosts. Some examples are ticks associated with Lyme disease or mosquitoes associated with malaria.
With regard to the audiology clinic, contact transmission represents the most common mode of microbial transmission. There are three subtypes: direct, indirect and droplet. Direct contact transmission occurs when the clinician comes in contact with the microbe in the environment. Removing a hearing instrument from the patient's ear with the bare hands without the necessary infection control precautions is an example of direct contact transmission. Touching somebody's draining ear with your bare hand is another example. Indirect contact transmission typically occurs when you are handling or reusing a contaminated object. For example, if you are using the same listening stethoscope to conduct a hearing aid listening check on two different hearing instruments without first cleaning and disinfecting the tip of the stethoscope valve, you can indirectly contaminate the hearing aids.
Finally, we have droplet transmission. Droplet transmission can occur when microbial droplets are expelled briefly into the air and are then quickly breathed in or they come in contact with your eyes, nose, mouth or skin. A good example is when someone coughs or sneezes directly on you. The critical point to gain from this is not so much how you differentiate direct and indirect droplet transmission, but rather recognizing what activities you, as an audiologist, perform throughout the day that potentially offer micro organisms an opportunity to travel from one location in the clinical environment to the next.
Once a micro organism has a mode, the second thing it needs is it needs a route. A route essentially refers to a portal of entry into the body. Common portals of entry include skin surfaces that may be dry such as hands, as well as natural body orifices such as the nose, eyes, mouth and ears. Once the micro organism enters the human body, a million different things need to happen in order for disease to occur. Whether or not disease manifests is a moot point. From an infection control standpoint our responsibility as audiologists is to control our external environment in the manner that eliminates potential modes and routes of microbial transmission.
Not to beat a dead horse, but another reason why we should care about infection control is the concept of opportunistic infections that I mentioned earlier. An opportunistic infection is the hallmark of immunocompromise. These infections occur as a result of micro organisms that are commonplace and are readily found throughout an environment. Opportunistic micro organisms do not cause disease in those individuals with healthy immune systems, but rather, as the name implies, these micro organisms take the opportunity to infect a body with some degree of immunocompromise. Take a moment and start thinking about the patient populations that you currently serve or have served. As audiologists, we provide services to a wide range of patients, many of whom exhibit varying degrees of immunocompromise and are potentially vulnerable to these opportunistic microorganisms in our clinical environment. It makes it that much more critical to be serious about implementing infection control procedures.
To put this concept of opportunistic infections in a more meaningful context, it is appropriate to review the findings of my study (Bankaitis, 2002) that was published in The Hearing Journal entitled "What's Growing on your Patient's Hearing Aids?" The purpose of this study was to identify the presence or absence of microbial growth on hearing instrument surfaces. If microbial growth was detected, the secondary purpose was to identify the type of bacterium or fungus that was recovered from these services. Ten custom hearing instruments were randomly selected from one ear of ten different patients, all who were binaural wearers of amplification. The hearing aid surfaces were swabbed utilizing the Baxter Culturette System which is basically a very expensive sterile Q Tip. Two Culturette Systems were used to simultaneously swab the hearing instrument surfaces. Two swabs were necessary for the purposes of microbial differentiation. One swab was used by the microbiology lab to identify bacterial growth, whereas the other swab was used to identify the presence of any fungal growth. Now, in terms of the results you are going to see several tables that are going to follow this slide and they will list any microbes that were recovered from the hearing aid surfaces. We included microbes that heavy, moderate, and light amounts on the hearing instrument. These are relative terms. Light does not mean that they had to squint to see the stuff. Light is still a lot, it just not as much as moderate or as heavy as the yellow.
Let's take a look at the results of the first five hearing instruments. Each hearing instrument was listed along with a more specific indicator to the custom device whether it was an ITE or CIC. We also indicated bacteria recovered and fungal growth recovered. Let's take a look at hearing instrument No. 2. We found moderate amounts of staphylococcus on hearing instrument number two as well as light amounts of the acinetobacter. In addition, we found moderate amounts of the fungus aspergillus. In contrast, if we examine hearing instrument No. 5 no fungal growth was recovered, but we found light amounts of staphylococcus and the bacterium lactobacillus.
Three given types of bacterium were recovered from hearing instrument No. 7: enterobacter, pseudomonas aeruginosa, and candida. On hearing instrument No. 10, no fungal growth was found; however, we did find moderate amounts of staphylococcus aureus as well as light amounts of regular run-of-the-mill staphylococcus. Recall that 9 of the 10 hearing instruments were contaminated with some type of staphylococcus. Beyond staphylococcus, seven additional bacterium were also recovered from hearing aid surfaces in various combinations. Furthermore, 4 of the 10 hearing instruments were also contaminated with some sort of fungal growth.
To summarize, none of the 10 hearing instruments were contaminated with the same things. The logical question at this point would be, "Are these findings surprising?" Well, the good news is if you answered yes or if you answered no, you are correct. On the one hand, these findings are not surprising. If I were to take a Baxter Culturette System and stick it in your ear and send it to the microbiology lab, they would most likely find microbial growth in many people's ears including varying degrees of staphylococcus, diphtheroids and occasional fungal growth. There is something we have to keep in mind, however. Given the fact that each of the 10 hearing instruments reflected a very unique combination of microbial contamination, the findings of this study are surprising because it possess some significance to the relevance of infection control to audiology.
The external auditory canal is more prone to infection than virtually any other skin surface. As audiologists we are all familiar with the literature that supports the antimicrobial property of cerumen, but it is important to note that the overall literature has been equivocal. For any study that says cerumen provides protection, there is a comparable study out there that argues that it does not. For our purposes, let us assume that cerumen does have the microbial properties. The efficacy of cerumen's properties will be highly challenged in the hearing aid wearer population. The ear canal is already a very warm, dark, moist place, and when you plug it up with an earmold or a custom hearing instrument or an earbud, the ear canal becomes a warmer, darker, place that retains moisture. That is going to change the overall surface pH from a neutral or alkaline level to a more normal or alkaline level, which means that your ear canal suddenly becomes much more conducive to microbial growth. It is at this point that you have to be concerned about the potential for opportunistic infections.
Thinking back, hearing aid No. 9 was contaminated with staphylococcus. This bacterium is ubiquitous. It is readily found throughout the environment; however, this very same bacterium accounts for the highest rates of nosocomial or infection. Why is something found in the environment cause so much disease in hospitals? Think about it. Who goes to hospitals? It is sick people with some degree of immunocompromise. It could be something as simple as touching a patient with your hand that you have not washed and suddenly you transmitted staphylococcus onto that patient's skin, and now they are in a position where they can actually acquire some sort of serious life-threatening pseudomonas. While pseudomonas may be found in some patients' ear flora, it is not considered a part of every patient's ear canal flora. This bacterium is actually highly virulent and causes otitis externa, and given the right set of circumstances, produces malignant otitis externa in HIV infected individuals as well as diabetic individuals.
While staphylococcus or pseudomonas are connected with ear canal flora, there are some micro organisms collected that are not considered any part of human being's normal flora. For example, hearing aid No. 5 was contaminated with lactobacillus and enterobacter. Lactobacillus is a bacterium that is isolated from urine. The specific strain of enterobacter that we recovered is found in human feces. So what is the real point here? Basically, you need to keep in mind that each hearing instrument reflects a very unique microbial composition. Just like two snowflakes, no two hearing instruments are alike. This certainly has specific implications to infection control.
For example, if you were handling one hearing instrument, and in the absence of any infection control procedures, you started handling another patient's hearing instrument, consider that anything that was on the first hearing aid is now going to cross-contaminate the other hearing aid. When you insert that now-contaminated hearing aid into the ear canal of your 80 year old patient who has diabetes, you have just provided the potential perfect storm for micro organisms to gain entry into the human body and to potentially cause disease. There was a follow up study conducted by Stacy Sturgulewski (2006) as a capstone project at Rush University Medical Center and she basically found that the same stuff is still growing on patients' hearing aids.
Making a Plan
With all this in mind, it brings us to the third and final objective of today's presentation which is to clarify how you can initially prepare an infection control plan. The first thing you need to do is assess the scope of services that are provided at your specific work environment. This step involves conducting an inventory of services that you and your staff provide so that you can start creating a list of audiological procedures that are performed in your clinic. For those of you who are serious about implementing an infection control plan or having an up to date infection control plan before you tune in to Part II, this is your homework assignment. You need to start making a list of procedures that your clinic provides. For example, if your clinic dispenses hearing instruments, you need to be more specific and write each step of dispensing the hearing aid on your list. Specific examples include taking earmold impressions, making hearing instrument modifications, performing listening checks, conducting electroacoustic measurements, drop-off services, and any other service that relates to dispensing hearing instruments. Next, if you do audiological assessments you need to spell out what that really means in your clinic. Examples would include otoscopy, air-conduction audiometry, bone-conduction audiometry, immittance, and perhaps otoacoustic emissions. You need to be specific. Are you removing cerumen mechanically or via suction and/or via irrigation? Do you use cerumen softening agents? Are you concerned that you will have a bleeder? You have to start writing down all the aspects of daily clinical flow in which you and your staff are involved. This list is essentially going to dictate how many work-practice controls that you are going to have to create for your clinic's infection control plan. Work-practice control is a profession-specific procedure this is designed to reduce the likelihood of contamination. In other words, you take the procedural list that you developed and you start writing a protocol that reflects how that procedure is going to be performed that is consistent with minimizing the spread of disease. We are going to cover this in more detail in Part II, but essentially this is all based on the universal precautions that were originally set by the Centers for Disease Control in 1987. It is a list of recommendations that are intended to reduce cross contamination. They are called universal precautions because they were designed to protect the healthcare worker from exposures to bloodborne pathogens, but they recently have been expanded to include all potentially infectious microbes including the ones in your audiology clinic. Now you see them referred to as standard precautions.
The whole mindset of standard precautions is that you need to treat every patient as if they were a carrier of a potentially infectious disease. This means that your infection control procedures outlined in your plan are going to be consistently followed for every single patient. These standard precautions include five guidelines that we are going to be addressing in Part II. We are going to talk about how we create work-practice controls using these standard precautions as our guide.
Conclusion
The take home message is that infection control requires consciously managing the clinical environment. It is not incomprehensible, but when you start peeling the onion and trying to put a plan in place, you can get frustrated; however, there are resources available. Infection control is a very important element in terms of best practices for audiology. It requires preparation in the form of identifying the scope of services prior to you being able to develop a written infection control plan. Again, your homework assignment is to start making a list of all the services that you provide, and from there you are going to be halfway home to developing your infection control plan. For further questions or clarification, I can be easily contacted by e mail at [email protected] or at 800 347 1960 and ask for A.U. For those of you that want more information on infection control, check out my blog at aubankaitis.wordpress.com. Thank you so much for your attention.
Question & Answer
If someone already has an infection control plan in place at their practice, how often should they be looking to updating it?
That is a very good question. Basically, it all has to do with training which we will talk about in Part II. Essentially, any time a new procedure is put in place like, you are required by OSHA to update your infection control plan to reflect the fact that you are providing a new procedure. It must be done at least annually and as needed when new procedures are implemented.
When a sterile solution is depleted is it considered to be infectious?
Probably not. It is a chemical so when you are done using the sterilant, you need to get rid of it immediately. That typically means disposing of it down the sink with running water.
References
Bankaitis, A.U. (1996). Audiological changes attributable to HIV. Audiology Today, 8(6), 7-9.
Bankaitis, A.U. (2002). What's growing on your patient's hearing aids? The Hearing Journal, 55(6), 48-56.
Bankaitis, A.U. & Kemp, R.J. (2003). Infection Control in the Hearing Aid Clinic. Boulder, CO: Auban.
Bankaitis, A.U. & Kemp, R.J. (2004). Infection Control in the Audiology Clinic. Boulder, CO: Auban.
Physicians' Desk Reference. (2011). Physicians' Desk Reference, 65th Edition. Montvale, NJ: PDR Network.
Sturgulewski, S.K., Bankaitis, A.U., Klodd, D.A., Haberkamp, T. (2006). What's still growing on your patients' hearing aids? The Hearing Journal, 59(9), 45-46, 48.


