From a historical perspective, parents of children with hearing loss as well as adult patients with hearing loss have both reported their hearing healthcare professional to be insensitive and indifferent or seemed to lack compassion and adequate counseling skills (Glass & Elliot, 1992;Martin, George, O'Neal & Daly, 1987;Sjoblad, Harrison, Roush, & McWilliam, 2000). When compared to the other two groups of hearing care professionals (hearing instrument specialists and otolaryngologists), audiologists seem to fare slightly better in this unfortunate rating, but are still far from being perceived as consistently strong in these areas.
Clearly, hearing care providers do not share this view of professional insensitivity and indifference. Audiologists' training heightens their awareness of the personal and psychosocial impacts of diminished hearing, and we view ourselves as uniquely positioned to address the concerns and challenges of those with hearing loss. So how can it be that such a dichotomy of views exists between the patients served and the professionals dedicated to their care? Clark and Brueggeman (in press) have posited that this dichotomy is largely related to the manner in which we deliver needed information to patients. While information delivery style is critically important to patients' perceptions of care, it can also be argued that the manner in which we listen to our patients will have an equal impact on the development of successful clinical interactions.
Listening is a Skill to be Honed
Listening is a process in which we hear another person speak, we attend to that person's message, and we attempt to comprehend the full meaning of the statements expressed that may often be masked by the very words chosen. While we frequently think of listening as a process that develops naturally, good listening is not a passive enterprise and requires attended practice (Table 1).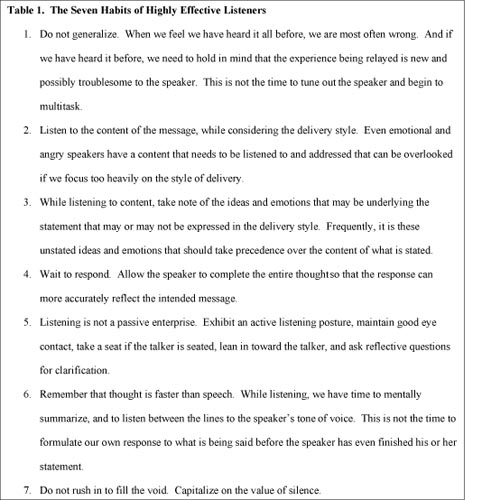
Click Here to View a Larger Version of Table 1 (PDF)
If we are to combat patients' perceptions that we are insensitive and indifferent to their plight, we can take no better first step than to hone our listening skills. Hearing loss management is a complex process, the success of which hinges directly upon the willingness of the patient to take ownership of the hearing loss itself and to accept the treatment recommendations we offer. We are grossly underestimating the complexities of this process if we do not recognize how very difficult it can be for many to accept the concept of handicap and all that that entails within the human psyche (Clark & English, 2004). It can be emotionally wrenching for parents to let go of the dreams they held for their child, dreams that formed even before conception. For adults to alter their view of the "self" they have known for years and the "self" they wanted to carry forward through life is no easy task, either.
Key Attributes to Successful Clinicians and Successful Listening
Successful clinicians are successful listeners, and these successes cannot be separated. Rogers (1961) professes three attributes that are primary to the success of any clinician. One of these key attributes is the clinician's developed sense of self-congruence. Self- congruent audiologists allow themselves to be who they are naturally without donning the persona of the appointed expert ready to bestow clear solutions and authoritarian guidance. The congruent audiologist allows for the greatest opportunities for positive and constructive development of the patient so that patients can more easily find their own inner resources for growth. When clinicians are fully congruent, they are in a state that allows true listening from the heart.
The second attribute that audiologists must cultivate within themselves is an unconditional acceptance of their patients. Rogers (1961) referred to this as an unconditional positive regard that is paramount in audiologists' ability to listen fully to their patients. Only when we can truly accept our patients for who they are, for the beliefs and limitations they bring to the table and the attitudes they may portray - both positive and negative - will our patients feel fully listened to. Full acceptance of patients' attitudes and statements does not imply our agreement. We can acknowledge that we understand why patients may feel what they feel or express what they express, yet not inwardly agree. However, it is through our nonjudgmental acceptance of patients' behaviors and attitudes that patients begin to recognize their own assets and not their disabilities as the greater reality. When we fail to acknowledge and accept, patients begin to feel uncomfortable continuing the dialogue. When we pass judgment on our patients' feelings, actions, or concerns, or when we project to our patients how we believe they should feel or act, we place barriers to the relationship for which we are striving and decrease the effectiveness of our services, thus fostering perceptions of indifference and insensitivity.
Our active listening leads to what Rogers (1961) labels as empathic understanding, the third of his primary counselor attributes. Our participation within clinical exchanges through active listening enhances our comprehension and reduces misunderstandings. It is through our active listening that we become more in tune with our patients' needs and concerns as they experience them, rather than as we might anticipate them because of our past experiences with others of similar ages, backgrounds, and hearing losses. It is only through our active listening that we can better translate a person's feelings into needs and begin to share in a partnership with them to address those needs.
Active listening is demonstrated through the audiologist's ability to reflect the expressed feeling of the patient in order to understand the patient's viewpoint and communicate that understanding. Reflections of feelings, while simple in principle, are often difficult in practice, as they differ greatly from our long and more familiar experience of responding to content. When attempting to develop an empathic response through reflection of feelings, the audiologist might try to select the one word that best describes the patient's feelings underlying a given statement. These reflections allow patients to examine their feelings or beliefs from another perspective, thus allowing for a continued, and perhaps broader, consideration of a topic. For example, the father who questions our test findings is not necessarily passing judgment on our clinical skills. A reflective response that acknowledges the root of the parent's comment and our acceptance of the situation in which the parent finds himself might be, "I would think it would be quite frightening to consider that these results might be accurate."
Active listening is a key to successful communication, a key to the development of strong interpersonal relationships, and a key to the bond of trust that must be attained if our adult patients or the parents of our pediatric patients are going to take action on the treatment recommendations we propose. Equally important, the clinician's active listening to a patient's or parent's sometimes poorly expressed needs and concerns is a primary key to that individual's own self-esteem. If we are to engage the parents of our pediatric patients and the adult patients we see in a team approach to hearing loss management, the only approach with far-reaching and lasting success, we need to empower them to take a lead role in their own care. By demonstrating our clear desire to fully understand what lies beneath a patient's statements, it becomes less likely that we will be judged as insensitive or indifferent.
What We See when We Listen from the Heart
Audiologists' reflective listening helps ensure that they have clearly heard one's intended meaning rather than as filtered by their own past experiences. But when listeners work toward a heightened comprehension of the content of the patient's message, they must also remain tuned to the style in which the words are conveyed that may belie something that the patient failed to verbalize. The vigilant listener will consciously make note of a patient's posture, forthcoming or reluctant eye contact, facial expressions, gestures and tone of voice. The audiologist may wish to bring observed nonverbal behaviors to a patient's attention, allowing the patient to draw his or her own conclusions about their meaning. While the patient may deny the validity of the audiologist's observations, once pointed out, these observations will frequently permit unexpressed feelings to surface for a more open discussion.
What Patients See When We Listen from the Heart
There are many things in life that we know to do, yet sometimes fall short in the doing. Just as audiologists need to remain cognizant of the nonverbal cues their patients may present during a clinic appointment, so must they be aware of the positive and negative nonverbal behaviors they may present within clinical interactions. These behaviors begin with the warm handshake, smile and direct eye contact that accompany our first greeting of the patient and continue through the attentive posturing we provide as our patients tell their own stories of what it means to live with hearing loss (Table 1). The negative listening behaviors that become painfully apparent when we fail to practice more positive actions stifle the sometimes allusive rapport we are trying to develop with the patient, impede meaningful dialogue necessary for progress, and increase perceptions of indifference and insensitivity.
What Blocks Our Effective Listening?
In our fast-paced society, we are rapidly becoming "human-doings" rather than "human-beings." It has become easier for us to be actively engaged in completing a task than it is for us to simply be with someone: listening to the story of their hearing loss, sharing their emotions, sharing their pain. Our frequent state of "human-doing" has emerged from our rapid-paced society's demand that we all become masters at multitasking. When we succumb to the temptations of multitasking, we fuel patients' perceptions that we are insensitive and indifferent. How can they feel otherwise that we are "listening" while we leaf through our charts, fill in the day's date and the patient's date of birth on the form in front of us, or jot ourselves a note so we don't later forget something that just popped into our wandering minds? It is unfortunate that good listening is frequently not modeled in our personal lives, during our academic careers, or within our professional encounters. But this is little excuse for us not to combat our distractions and more actively attend to our patients.
How do we perceive our patients? From our patient's perspective, each has a unique experience. Frustrations with hearing loss are frequently creating short fuses within families. Tempers flare when simple requests to modify one's speaking style are forgotten because the modification is not required consistently;questions answered inappropriately sometimes engender hurtful mirth;self-worth is too frequently eroded as hearing loss goes unaddressed. As Kennedy and Charles (2001) have stated, our attempts to fully appreciate the experiences of our patients "should be an exercise in treating people with dignity and respect for their individuality" (p. 131). One might question how effective we are in this exercise.
Are we clearly acknowledging each patient's individuality when we look at the audiogram and generalize the experiences the patient in front of us will have to those experiences that so many of our other patients of a similar age who have similar hearing loss configurations have expressed before? Have we ever said to ourselves, "This patient is just like my 11:00 patient this morning." Have we ever feigned listening while thinking, "Haven't I heard all of this before?" If we are truly listening to the experiences our patients are telling us, if we are truly working to draw out the unexpressed concerns through our reflective listening so that we know what to address, if we are truly dignifying and respecting each patient's individuality, we will be able to better serve each person's needs. When we do this, we will be perceived by our patients as the caring professionals we believe we are. It is when our treatment recommendations are based on a true understanding of and appreciation for the difficulties our patients are experiencing that we are perceived as caring and supportive.
The Strength of Silence
The sense of having been understood is increased when one feels time has been given to fully state concerns and thoughts. Silent reflection on the words one has spoken and receptive waiting on the words yet to be expressed are valuable for patients who may be confronting bad news or grappling with issues foreign to past experiences. In social contexts, there is a natural tendency to fill silent voids within a dialogue. However, when we rush in to fill silent pauses within clinical exchanges, we reinforce the patient's perception that the audiologist is responsible for initiating and maintaining discussion.
When we fill the void too quickly with our own comments or further questioning in our effort to maintain discussion, we can disrupt the patient's thoughts or sidetrack an issue that may not have been fully explored. By allowing some temporal space for reflection, we can help our patients assume responsibility for their own progress and foster their sense of empowerment required for rehabilitative success. Our primary clinical goal is to foster our patient's strength of self-direction.
Hearing the Words / Missing the Point
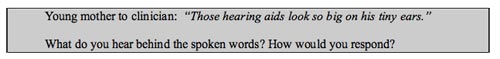
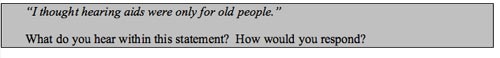
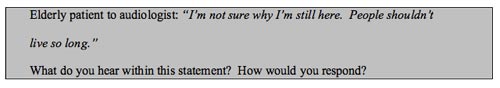
Frequently we respond to the content of our patient's statements while we fail to hear the true concern. How do we respond to the mother who expresses concern about the size of the new and unwanted hearing aids relative to the size of her child's ears? How do we respond to the adult patient who reflects on his perception that hearing aids are for people significantly older than he is? How do we respond to the elderly woman who questions the futility of her existence at this late stage in her life?
Reassurances and platitudes are not what these patients are seeking. We can be quite certain that the mother knows that hearing aids have become smaller over the years and addressing this fact, or the fact that her child's ears will indeed grow, speaks only to her words. Pointing out to our adult patient that we have a number of hearing aid users in our practice who are considerably younger is not a reassuring revelation. Responding to the elderly patient who is questioning why she is still on this earth by reassuring her that things will seem much brighter once she hears better is not the comfort she is seeking.
When we listen only to the words, we are not listening from the heart. When we listen from the heart we hear the pain that cannot be fully expressed. Sometimes the strongest words we might choose are those that express our acknowledgement of the emotion behind the statement. A statement as simple as, "It must be difficult when life takes us in directions we weren't expecting," lets others know we have heard the unstated concerns and emotions and helps us to connect with them while lifting the perceptions of indifference and insensitivity.
Moving Closer toward Personal Adjustment Counseling
When we fail to listen from the heart, we perpetuate the perception that we are insensitive and indifferent. When we fail to listen from the heart, we contribute to the unbelievably low penetration rate within the market comprised of those growing number of people with hearing loss who have yet to take action to address their difficulties. When we fail to listen from the heart, we hurt our own profession. And most importantly, when we fail to listen from the heart, we have failed those whom we claim we want to serve.
True listening is an active engagement with another person and can be frequently draining if one does not exercise this skill regularly. To truly combat negative impressions of our services, we must first combat the impediments to listening that draw us away from our patients. When we listen from the heart we are moving away from simple content counseling or information transfer. Much of the counseling we provide our patients will be, by necessity, the delivery of information about diagnostic findings and rehabilitative recommendations. When we present our information fully cognizant of how it may be received (Clark and Brueggeman, in press) and strive to listen from the heart at all times, we will find we are moving directly into the realm of personal support counseling where we truly need to be.
To see how your listening skills fare, see the Appendix following the References of this article
References
Clark, J.G., & Brueggeman, P.M. (in press). The impact of grief on the delivery of information: increasing student effectiveness. Journal of the Academy of Rehabilitative Audiology.
Clark, J.G. & English, K. M. (2004). Counseling in Audiologic Practice: Helping Patients and Families Adjust to Hearing Loss. Boston: Allyn & Bacon.
Glass, L.E. & Elliot, H.H. (1992). The professionals told me what it was, but that's not enough. SHHH Journal, January/February, 26-28.
Kennedy, E. & Charles, S.C. (2001). On Becoming a Counselor: A Basic Guide for Nonprofessional Counselors and Other Helpers. New York: Crossword Publishing.
Martin, F., George, K., O'Neal, J., & Daly, J. (1987). Audiologists' and parents' attitudes regarding counseling of families of hearing impaired children. Asha, 29(2), 27-33.
Rogers, C. (1961). On becoming a person. Boston: Houghton Mifflin.
Sjoblad, S., Harrison, M., Roush, J., & McWilliam, R.A. (2000). Parents' reactions and recommendations after diagnosis and haring aid fitting. American Journal of Audiology, 10(1), 24-31.
Appendix
How would you rate your listening skills?
Contrary to popular belief, good listening does not develop naturally nor is it a passive enterprise. Good listening aids our comprehension, reduces misunderstandings, enhances our critical thinking, and helps determine a person's real needs and concerns so that they may be translated into actions. Poor listening skills contribute to patients' frequently reported perception that hearing health care professionals are insensitive and indifferent.
Take the listening skills test below to see how well your ranking matches with your perceptions of your listening skills. The following questions should be scored with a numerical ranking as follows:
5 = almost always____ Do you ever anticipate what people will say next as they are speaking?
4 = frequently
3 = occasionally
2 = rarely
1 = almost never
____ Do you ever find you want to jump in to fix the problem or provide a solution while the other person is still talking?
____ Do you ever feign attention while you are listening to someone?
____ Do you ever pay more attention to the speaker's mannerisms, or what words he/she is using, than to what is being said?
____ Do you ever interrupt others to speed the conversation along or to inject your opinion?
____ Does your mind tend to wander when you are listening to someone speak about something you believe you have heard before from others in similar circumstances?
____ Do you find yourself preparing a response to what the other person is saying while that person is still talking?
____ Do you ever try to multi-task while you are listening to someone?
____ Do you get so overly stimulated about what someone is saying that you have difficulty listening to what is being said?
____ Do you daydream or allow your mind to wander if you are listening to someone speak about something that is difficult for you to understand or is uninteresting?
How do you rank?
10 -15 You are a good listener
16 - 39 You are OK, but you could stand some improvement. Others would not call you a "bad" listener, but you may be judged as insensitive or indifferent.
40 - 50 You need some work on your listening skills.