Learning Outcomes
After this course, participants will be able to:
- List the benefits offered by Signia TeleCare.
- Describe new features in TeleCare 3.0.
- Explain results from a clinical study conducted with TeleCare 3.0
Introduction
In many cases, especially with new hearing aid users, success with hearing instruments depends on the patient’s experiences during the first few weeks following the fitting. This is when important questions need to be answered, when program changes may be necessary, or when the patient simply needs some hand-holding during this initial adjustment and acclimatization period. In the past, for most of these issues, the patient needed to schedule one or more repeat office visits to have the problem addressed. This was burdensome for both the patient and the dispensing audiologist. In some cases, the patient simply “gave up” and decided against the use of hearing aids.
Fortunately, today, the majority of these issues can be handled through telemedicine, which is the umbrella term to describe the provision of healthcare services from a distance by using modern telecommunication systems including wireless communication. First in the hearing aid industry to take up this idea and launch remote hearing care, Signia’s TeleCare system not only reduces barriers for hearing impaired individuals living in underserved areas, or for people who are not able to drive or take public transport, it also reduces traveling and waiting time for all patients. Marketing research has shown that the new generation of hearing aid users appreciates the convenience of using modern communication tools to obtain prompt support whenever it fits best into their daily schedule and routine. Handling personal issues through emails, texting and the Internet is now common in most all medical disciplines.
In addition to convenience, TeleCare provides hearing aid wearers with the opportunity to become more involved in the fitting process. This strengthens their commitment and therefore not only increases the initial acceptance of hearing aids, but also increases overall patient satisfaction. As reviewed by Kochkin, Dennison and Jackson (2014), patient loyalty is vitally important for all practitioners. These authors point out that MarkeTrak data show that over 60% of individuals purchasing hearing aids are repeat patients. Current patients in hearing healthcare are a precious commodity. In fact, they are the key driver of growth and profitability. Given the difficulty in attracting new hearing aid users, ways must be found to enhance consumer loyalty of current hearing aid users. TeleCare is an excellent way to do this.
TeleCare also benefits the professional in that they can reach more patients and deliver extra patient-centered care. This special service is a good means to recommend him/herself not only as a competent service provider but as an attentive companion and partner throughout the entire fitting process. Beyond that, TeleCare can diminish professional isolation in rural areas. In busy practices, it can help to better structure working hours by using time slots with fewer or no patients in the practice to remotely solve issues which do not require on-site appointments.
Overall, both the patient and the professional will save time and gain efficiency. And even more importantly: TeleCare is an effective method to strengthen the “doctor/patient” relationship, helping to turn patients with hearing loss into satisfied hearing aid users by keeping the fitting process on track.
The Latest Signia TeleCare
Signia TeleCare 3.0 offers complete live remote tuning so that audiologists can fine-tune patients’ hearing aids in the real-life situations for which they are intended. After the initial fitting, follow-up appointments can be held online via video call—in essence, a virtual home visit. This allows professionals to adjust the hearing aids to achieve the most natural individual sound quality in real time and at the patient’s convenience, to keep the necessary adjustment to amplification on track.
Specific features of TeleCare 3.0, designed to increase patient acceptance, benefit and satisfaction with their new instruments include:
- The ability to remotely monitor indicators such as wearing time, program use, and situation classification to determine when intervention might be necessary.
- Ability to track the patient’s satisfaction for different real-world listening conditions to determine if programming changes or additional counseling is warranted.
- The option to deliver at-home patient care by solving issues after the initial fitting through remote programming changes to the gain, output, frequency response, noise reduction and other algorithms.
- Real-time video calls as well as text and voice CareChat capabilities enable easy and direct communication between the audiologist and the patient.
Although the benefits of TeleCare seem obvious, other than anecdotal reports there are little data to support the usefulness of this technology. To determine the impact on hearing aid benefit and satisfaction, a field study therefore was conducted using the Signia TeleCare 3.0 at the University of Western Ontario.
Clinical Study
The participants were 15 individuals age 56-79 (mean age 68 years); six females and nine males. All had bilateral downward sloping hearing losses, with the mean audiogram showing hearing loss ranging from 20-25 dB in the low frequencies (250, 500 Hz) dropping to 60-65 dB in the high frequencies (6000, 8000 Hz). Hearing aid experience was varied, with four individuals using hearing aids for the first time, and others with several years of hearing aid use; for the eleven experienced users, the median duration of hearing aid experience was six years.
All participants were fitted bilaterally with the Signia Pure Nx using click sleeve coupling appropriate for their hearing loss. The hearing aids were programmed using the Signia Connexx 8.4 software to the DSL v5.0 adult prescriptive targets, verified with probe-microphone measures. Minor adjustments were made regarding listening preference. Additional programs for noise, music, television, and tinnitus were added based on the participants’ needs. All directional and noise reduction features were activated. Frequency compression was activated if necessary on a case-by-case basis, and the settings optimized using the maximum audible frequency range (MAOF) technique (Gista, Hawkins & Scollie, 2016), with the /s/ stimulus included with the Audioscan VF2 probe-microphone equipment.
The Client was enabled in Signia TeleCare 3.0 via the Connexx software. The myHearing app was downloaded from GooglePlay or the Apple App Store and paired to the hearing aids prior to leaving the fitting appointment. Research staff had access to TeleCare at the Signia Internet portal (https://telecare.signiausa.com/#/login). The portal was checked throughout the work week for messages from participants and to assess their daily use and satisfaction ratings. If two consecutive daily ratings indicated that the participant was unsatisfied, the study staff reached out to the participant through the app. Counseling through “Messages” and remote fine tuning adjustments through “Remote Tuning” were completed.
At the time of the fitting, using the COSI format (Dillon, James & Ginis, 1997), each individual was asked to nominate listening situations that were important for them, and where they would want to see improvement using hearing aids. Once the situations were determined for each participant, they rated their current ability for each setting on a 0-100% scale in 5% increments. They also then rated their satisfaction with their performance for these situations on a 7-Point scale ranging from 1=Extremely Dissatisfied to 7=Extremely Satisfied. A minimum of three listening situations were required for each participant. The majority selected four different situations and some chose five. In total, the 15 participants selected 60 personal situations. At the conclusion of the home trial, each individual again rated their personally selected situations for ability on the 0-100 scale, and on the seven-point satisfaction scale. For the four new users, the comparison was unaided versus aided. For the eleven experienced users, the comparison was the Signia Nx instruments to their personal hearing aids.
A second self-assessment scale also was conducted at the conclusion of the study—the International Outcome Inventory for Hearing Aids (IOI-HA; see Figure 1). The IOI-HA consists of seven items that focus on different domains of hearing aid outcomes (Cox and Alexander, 2002). The domains that are assessed are benefit, daily use, satisfaction, impact on significant others, residual activity limitation, residual participation restriction and quality of life. Each of the IOI-HA items has five answers that range from the worst outcome on the left (value=1) and the best outcome on the right (value=5). Norms for the English version of the IOI-HA have been provided by Cox, Alexander & Beyer (2003).
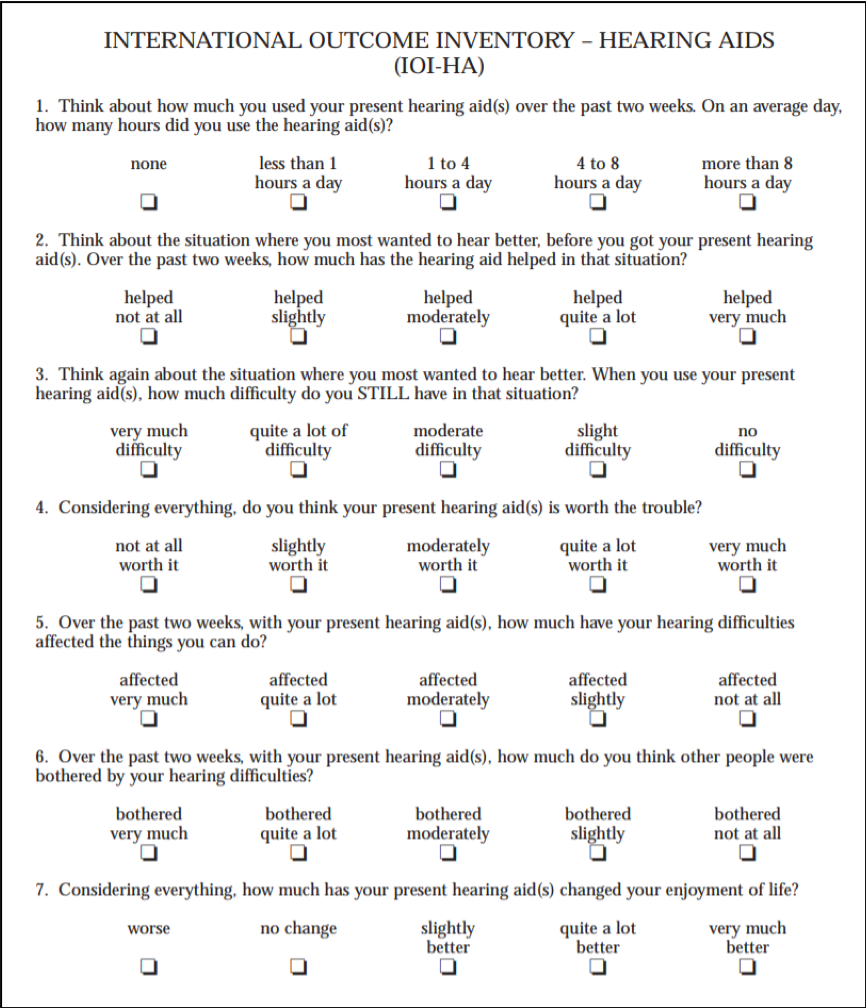
Figure 1. Shown is the U.S. English version of the International Outcome Inventory for Hearing Aids (IOI-HA; Cox and Alexander, 2002). Each question represents an outcome domain. The domains (in order of listing) include: Daily Use, Benefit, Handicap, Satisfaction, Disability, Impact on Others, and Quality of Life.
Results Following Home Trial
The results during and following the home trial included the TeleCare actions that occurred during the home trial period, the participant’s ratings of benefit and satisfaction for the different listening situations, and the scores obtained for the seven items of the IOI-HA.
TeleCare Services. As reviewed earlier, Signia TeleCare includes a wide range of services ranging from monitoring patient satisfaction to messaging regarding patient concerns to remote programming of the instruments themselves. Table 1 provides a summary of the remote programming that was conducted. A total of 6 of the 15 participants requested programming changes, and for some, several changes were made. The most common changes were regarding loudness and reducing high frequency gain.
Participant | Complaint(s) | Troubleshooting – Fine Tuning |
S1 | Sounds are too sharp or noisy, trouble with TV connection, feedback | Remote tuning sent to adjust frequency response, Review connectivity with TV |
S2 | Sound quality distorted with musical instrument, too sharp | Remote tuning sent to adjust frequency response |
S3 | Acoustic Feedback | Remote tuning to reduce feedback after patient declined to return to the office for physical fit adjustment |
S4 | Sounds are loud or noisy | Remote tuning to decrease gain. Counseled on hearing aid cleaning & maintenance procedures |
S5 | Acoustic Feedback | Remote tuning to reduce high frequency gain |
Table 1. Summary of the remote programming.
Table 2 summarizes some of the other communication via the myHearing app. Note that in some cases, the communication was initiated by the researchers, in other instances, by the patients. For those participants who used the message feature, the number of messages ranged from 1-38, with an average of twelve (12) messages per participant.
Participant | Reason(s) for Contact | Messaging |
S6 | Low satisfaction ratings | Staff initiated communication after receiving low satisfaction ratings. After follow-up appointment, staff followed up via app to ensure everything was better. |
S7 | Participant asked about connecting hearing aids to phone. | Staff recommended troubleshooting tips. After the study, the participant messaged again to report high satisfaction with the aids. |
S8 | Low satisfaction ratings | Staff initiated communication but received no response from patient. |
S9 | Staff messaged instructions on how to rate situations. Patient also initiated communication on a separate occasion. | Patient messaged staff to report that low rating was due to illness and not hearing aid. |
S10 | Staff initiated communication. | Staff reminded patient to send ratings. |
S11 | Patient asked about problem with app. | Staff provided re-installation instructions. |
S12 | Staff provided usage instructions. Participant also messaged questions to staff on a separate occasion. | Staff provided instructions on hearing aid and app usage. Participant used the app to ask questions about hearing aid usage. |
Table 2. Communication via the myHearing app.
Benefit Ratings for Listening Situations. Participants rated their “ability” for each situation they selected before and after the home trial using TeleCare. For the majority of the participants, the pre-trial ratings reflected the ability they were experiencing with their current hearing aids. The ratings were conducted on a 0-100% scale. The mean findings for the 60 selected situations are shown in Figure 2. Observe that a substantial increase in the ability ratings occurred, with mean values going from 58% to 87% following the fitting of the new hearing aids. Moreover, at the end of the trial, 38 of the 60 situations (63%) received an ability rating of 95-100%.
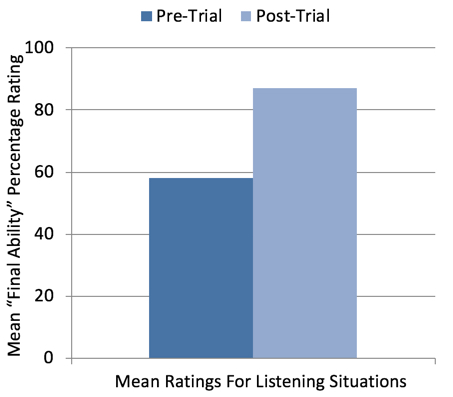
Figure 2. Shown are the mean “Final Ability” ratings for the 60 different listening situations selected by the participants. Ratings were taken Pre-Home Trial and Post Home Trial, and based on a 0-100% ability rating scale.
Satisfaction for Listening Situations. In addition to rating ability, recall that each participant also rated their satisfaction of their performance in these selected situations before and after the home trial. The mean results of these ratings (total ratings=60) are shown in Figure 3. As displayed, and in general agreement with the ratings of ability, there was nearly a two-point improvement (3.8 versus 5.7) following the home trial with TeleCare assistance. This is particularly noteworthy in that 11 of the 15 individuals were satisfied hearing aid users prior to the start of the study.
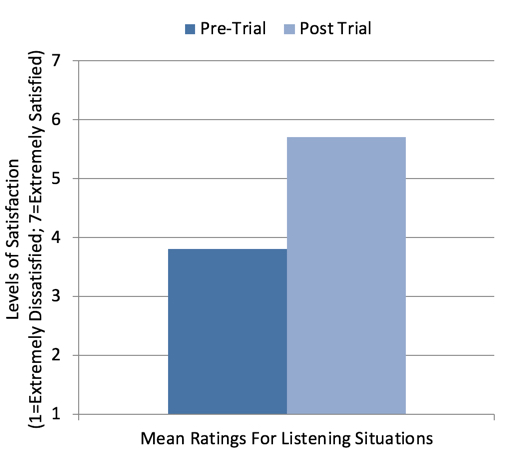
Figure 3. Shown are the mean satisfaction ratings for 60 different listening situations selected by the participants. Ratings were taken Pre-Home Trial and Post Home Trial, and based on a seven-point Satisfaction Scale (1=Extremely Dissatisfied and 7=Extremely Satisfied).
Even more significant than the improvement in the mean ratings, was the number of situations where the participant was Very Satisfied or Extremely Satisfied (i.e., a rating of #6 or #7). As shown in Figure 4, prior to the home trial, 13% of the situations received a rating of #6, and only 3% a rating of #7. Following the fitting and TeleCare intervention, 32% and 38% of situations received a rating of #6 and#7 respectively. That is, 70% of situations received a highly satisfied rating. It’s important to point out that 23 of the 60 (38%) situations nominated involved speech understanding in background noise.
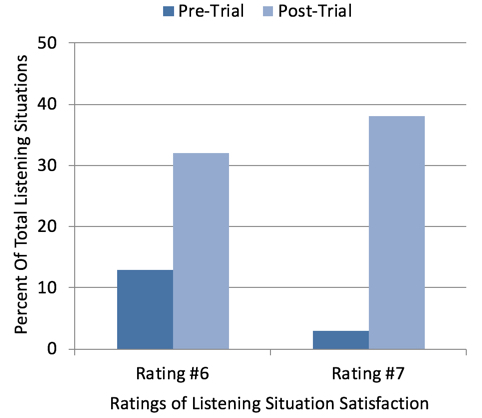
Figure 4. Satisfaction ratings for 60 different listening situations were obtained Pre-Home Trial and Post Home Trial, and based on a seven-point Satisfaction Scale (1=Extremely Dissatisfied and 7=Extremely Satisfied). Shown here are the percent of ratings that were either a #6 (Very Satisfied) or #7 (Extremely Satisfied).
IOI-HA Findings. As reviewed earlier, the IOI-HA consists of seven questions related to different domains of hearing aid outcomes. Each question is scored on a 1 (worse) to 5 (best) scale. The mean results are shown in Figure 5. To make these findings meaningful, we have included the Cox, Alexander & Beyer (2003) norms for each item (norms shown here are those for individuals with mild-to-moderate hearing loss, which corresponds to our participants). Observe that for all 7 domains, the participants’ ratings were substantially higher than normative values. The largest difference was for the item: “Considering everything, do you think your present hearing aids are worth the trouble?” The mean rating for this item was one category higher than what would be expected from the average hearing aid user. We interpret this to mean, that with TeleCare, much of the “trouble” associated with the use of hearing aids has been eliminated or at least minimized.
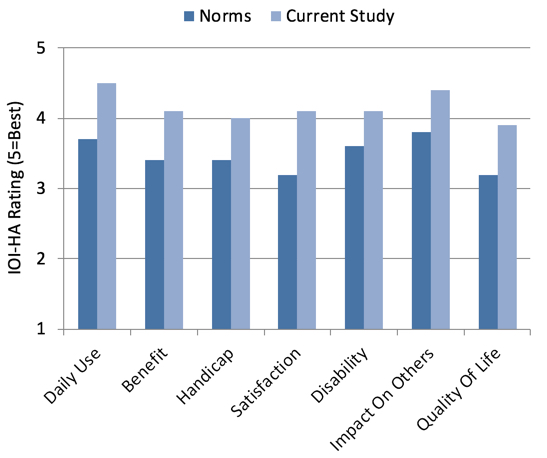
Figure 5. Shown are the mean IOI-HA findings for the seven different domains for the participants of this study. For comparison, also shown are the normative data for individuals with mild-to-moderate hearing loss (Cox, Alexander & Beyer, 2003).
Summary
Much of the long-term success with hearing aids, especially with new hearing aid users, depends on the user’s experiences during the first few weeks following the fitting of the instruments. It is during this period that fitting issues that easily could be fixed can become problems that lead to hearing aid rejection. The results of the research presented here reveal that by using Signia TeleCare, fitting issues easily can be resolved remotely. The data show that the result of this extended patient care leads to increased benefit for several different outcome domains, as clearly shown in the high final ability ratings and the findings from the IOI-HA. Also observed was high patient satisfaction for the majority of the listening experiences. Moreover, this fine tuning and counseling assistance was provided without the need for the patient to return to the clinic, an added convenience for the patient, and time saving for the audiologist.
References
Cox RM., Alexander, GC. and Beyer CM. (2003) Norms for the International Outcome Inventory for Hearing Aids. Journal of the American Academy of Audiology, 14(8): 403-413.
Cox, R.M., and Alexander, G.C. (2002) The International Outcome Inventory for Hearing Aids (IOI-HA): psychometric properties of the English version. International Journal of Aud. 41(1): 30-35.
Dillon H, James A, Ginis J. (1997) Client Oriented Scale of Improvement (COSI) and Its Relationship to Several Other Measures of Benefit and Satisfaction Provided by Hearing Aids. J Am Acad Audiol 8: 27-43 (1997)
Glista, D., Hawkins, M., & Scollie, S. (2016, April). An update on modified verification approaches for frequency lowering devices. AudiologyOnline, Article 16932. Retrieved from www.audiologyonline.com
Kochkin S, Dennison L, Jackson L. (2014) What is your customer loyalty quotient (CLQ)?: Applying Deming and Heskett’s principles to hearing healthcare practices. Hearing Review. 21(9):16-21.
Citation
Froehlich, M., Branda, E., Apel, D. (2018). Signia TeleCare facilitates improvements in hearing aid fitting outcomes. AudiologyOnline, Article 24096. Retrieved from www.audiologyonline.com




