Editor’s Note: This text course is an edited transcript of a live seminar. Download supplemental course materials.
Casie Keaton: Today’s course is entitled Your Role in Treating the Tinnitus Patient: What’s Your Professional Responsibility? We will begin by talking about the prevalence of tinnitus and the absolute need for trained clinicians. I think some of the numbers will surprise you. We will also discuss advanced evaluation and treatment considerations and what to do with these patients when they are in the office. We will look at the importance of evidence-based treatment options and key counseling concepts, and then finish up with some case studies that were shared by our certified Neuromonics providers.
Why Should we Treat Tinnitus Patients?
Why, as audiologists, should we treat these patients? Let’s look at the prevalence of tinnitus. This data is from the American Tinnitus Association (2014). Tinnitus affects one in six people; that translates to about 50 million Americans. Of that number, 15 million will seek medical treatment each year from their primary care physician, ear, nose and throat physician (ENT), or audiology practices. Of those, two million are deemed to be disturbed by their tinnitus enough to where it affects their work or livelihood, their sleep and their social interaction. Another shocking number is that 800,000 new cases are diagnosed each year. This is not a problem that is going away. It is growing. We need to arm ourselves with the information and the tools to be able to help these patients as they come into our office.
Tinnitus is the number one service-connected disability of our returning veterans from the conflicts in Iraq and Afghanistan. Data from the U.S. Army Center for Health Promotion and Preventive Medicine reports that between 30% and 49% of all returning soldiers have tinnitus. We need to be prepared to start seeing more and more of these patients.
In my work with tinnitus patients each week, here are the common themes that I hear repeatedly:
- “I have suffered in silence for many years. I didn’t know there was anything I could do for my tinnitus.”
- “I’ve just always been told to learn to live with it.”
- “I can’t find anyone who understands what I’m going through or can tell me what to do about it!”
This is a personal struggle for them and something in which they have invested a lot of time, effort, and sometimes expense, with very little positive outcome. In 2013, patients are still being told that they have to learn to live with their tinnitus when there are effective, viable treatment options available. These patients are seeking advice from other medical professionals and not finding much evidence-based information, nor any ideas or referral sources as far as where to get treatment for tinnitus. We need to do a better job at getting the word out that there are solutions for patients with tinnitus.
It always helps to understand, as much as you can, where the patient is coming from and what their experiences have been. Fear is a major underlying part of this condition. Is the tinnitus indicative of something more serious? Where is the sound coming from? They need an appropriate medical work-up to assure them that there are no other factors behind their tinnitus.
These patients also experience a lot of anxiety. They feel hopeless, like it is never going to get any better or that there is something more serious going on. They may have anger and sometimes grief. Why did this happen to me? What did I do to have this happen in my life? They may feel a loss of control. Nothing they do makes it any better. That can lead to some catastrophic thinking, and we need to help patients sort through these emotions and educate them that this is not necessarily the reality. We do have options for them.
Specifically, patients’ tinnitus causes sleep interferences, where they are either not getting very much sleep at night or their sleep is frequently interrupted. There is a lack of quality sleep. If I do not get sleep, I have problems the next day in terms of my work and my interactions with other people. I can be short with people or more irritated by small things. The tinnitus can trickle into all these different areas and have a huge impact on quality of life. It is not just the tinnitus. In many cases, it encompasses several aspects of their life.
Why are we, as audiologists, best-suited to treat these patients? It is within our scope of practice. The guidelines from the American Academy of Audiology (AAA, 2000) state that, “Audiologists assess and provide audiologic treatment for persons with tinnitus using techniques that include, but are not limited to, biofeedback, masking, hearing aids, education, and counseling.” The guidelines from the American Speech-Language-Hearing Association (ASHA, 2003) state that, “Assessment and non-medical management of tinnitus using biofeedback, behavioral management, masking, hearing aids, education, and counseling.” But more than that, I think we are the best professionals because of our training and what we already do every day for our patients with hearing loss.
For those of you who may be new to tinnitus treatment, this is what you do every day for patients with hearing disorders. We are helping patients by developing treatment plans and strategies to manage the impact of their hearing loss. We can do the exact same thing for patients with tinnitus. I think we can be the tinnitus patient’s No. 1 ally, and it can be one of the most rewarding aspects of practice for those of you who are not already doing so.
What is our Professional Responsibility?
What is our professional responsibility? What should we be doing for our tinnitus patients? The first thing is the evaluation. Providing comprehensive audiometric testing as well as tinnitus testing is important so that patients may have a firm picture of the extent of their tinnitus impact. We also need to provide them with education, so that we can better alleviate the fear and anxiety behind their tinnitus, allowing them to understand that they do not have to just learn to live with it. We do have viable treatment options. They need a basic understanding of the mechanisms at work behind their tinnitus. I believe a brief, straight-forward explanation for patients is the best way to go about it, telling them that there are usually three elements involved in bothersome tinnitus.
One has to do with your auditory system. If there is auditory damage, the brain is trying to correct that, which is where the tinnitus signal is generated. Next is attention. There are sounds to which our brain chooses to attend and sounds that our brain chooses to filter out into our subconscious. With disturbing tinnitus, our brain has incorrectly labeled the tinnitus signal as something harmful or threatening, and it is seeking it out much of the time. That is the reason tinnitus is heard most of the time. The last piece, and probably the most important, has to do with the stress response, or our limbic system involvement, where the heart rate quickens, respiration quickens, and the autonomic nervous system is activated. It is important to give patients a foundation of the condition, and then we can start to talk about how it specifically impacts them and devise strategies for management. This is where those evidence-based treatment options come from.
Advanced Evaluation and Treatment Considerations
There are tests that we recommend you perform during the initial tinnitus evaluation appointment. Our professionals' website, www.neuromonicsprofessional.com, has a variety of clinical resources for registered users. One such resource is a tinnitus appointment guide that you can print out and keep right next to the audiometer, detailing the specific tests as far as instructions for you as the clinician, and there are also instructions there for you to give the patient. This is very user-friendly. I recommend that each of you download that for your clinic.
We recommend tympanometry and otoacoustic emissions (OAEs). Some of these patients will present with normal hearing. We want to do comprehensive audiometry and then the assessment of tinnitus, which includes pitch-matching, loudness match, minimal masking level, and residual inhibition. The code for that assessment of tinnitus is 92625, and you must complete each of those tests in order to bill that code. We also recommend completing loudness discomfort level (LDL) testing, because many of these patients will present with decreased sound tolerance or hyperacusis concurrently. That can affect your treatment recommendations and strategies for management.
Reactive Tinnitus
Reactive tinnitus is a smaller subset of the overall tinnitus population. It is a type of tinnitus that is worsened after exposure to mild to moderate levels of sound. Typical tinnitus, if there is such a thing, is made worse by loud music, loud yard tools, loud traffic, street noise, et cetera. However, a patient with reactive tinnitus will tell you that their tinnitus is worse after they get out of the car or the shower. Most tinnitus patients find a lot of refuge in the shower; they like that constant sound. These patients do not. This increase in sensitivity tends to last for more than one day. It is a subset of the overall tinnitus patient, but one of which you need to be aware and know how to identify.
The best test for identifying reactive tinnitus is the Residual Inhibition test that you will do as a part of your overall tinnitus evaluation. The procedure for that test is presenting narrowband noise at the tinnitus frequency for about one minute at a sensation level of about 15 dB over the threshold at that pitch. You will then turn the noise off and ask the patient if their tinnitus has changed any. Some will say it is the same. There are those that will say that it has increased or it is worse. That can be a red flag of the presence of reactive tinnitus.
Also on the patient history, you will find a report of overuse of hearing protection when not indicated. These people are wearing hearing protection to the grocery store or at the gas station, or during times when they otherwise would not need to be protecting their hearing. They have also found that nothing will reduce their awareness of their tinnitus, and they may have had other trials with acoustic-based treatments that have aggravated their tinnitus. They may have tried hearing aids unsuccessfully and needed another option instead.
The Neuromonics Oasis product has a two-stage protocol. We have a reactive tinnitus protocol for these patients where you would begin the patient in Phase 2 and complete their treatment using just that phase of the therapy. That protocol is available to registered users on our professionals’ website (www.neuromonicsprofessional.com). I invite you to check that out and contact me if you have any questions. This can be a tricky patient, and you may need help to navigate their issues.
Hyperacusis
Another difficult tinnitus patient can be one who has decreased sound tolerance or hyperacusis in conjunction with their tinnitus. Decreased sound tolerance is discomfort from sounds at a level which most people would not find uncomfortable. The guideline is loudness discomfort levels below 90 dB. Hyperacusis is when the patient experiences sounds that would normally be considered loud, but easy tolerated by other patients. This patient would perceive sound to be painful or very loud. There is some physical discomfort that many of these patients experience. As a guideline, LDLs are typically below 70 dB across all frequencies. We recommend testing 500, 1000, and 4000 Hz in the tinnitus frequency to give you a good basis for their discomfort levels.
How does decreased sound tolerance or hyperacusis affect treatment? The literature reports that anywhere from 8% to 50% of these tinnitus patients will report decreased sound tolerance or hyperacusis. If you do not address this issue first, it will be very difficult to achieve any headway in managing their tinnitus. For example, let’s say you are providing sound therapy as a tinnitus therapy for decreased sound tolerance and the idea there is to give them relief, relaxation, and sense of control. If they are not able to tolerate that sound therapy at a volume loud enough to get relief from the tinnitus, you will not be able to effectively treat the tinnitus. You need to effectively address the hyperacusis first, and then you can begin to address the tinnitus goals.
In terms of expectation management, you need to lay out realities for the patient; they must be on board with those and understand the process of treatment. Then they can follow recommendations, and you will be on the same page. That can be a frustrating exercise if you begin what you think is treatment for their tinnitus, and then you run into brick walls when it comes to their decreased sound tolerance. These are my favorite patients to treat, because many times they have become withdrawn and disconnected from a lot of things they enjoy and love. To give them the ability to go back and experience those things again is very powerful and rewarding.
Neuromonics Products
For those of you not familiar with the Neuromonics product line, I would like to give you a brief introduction to our two products, the Oasis and the Sanctuary.
(Editor’s note: Since the presentation date of the live seminar on which this article is based, Neuromonics has introduced a third product. The Haven, with the ability to program and individualize hearing profiles, is a management tool offering situational relief for tinnitus symptoms.)
Oasis
The Oasis it is a two-phase formal treatment protocol for tinnitus. The goal is to not only address a patient’s tinnitus disturbance, but to also facilitate habituation from the tinnitus. The Oasis provides an individualized ear-specific stimulus; music is the carrier for the treatment. It accounts for any asymmetry in hearing. The music is spectrally modified based on the user’s audiogram in order to provide maximum stimulation to the patient, especially in the ultra-high frequencies out to 12,500 Hz. The device also provides data logging, which is helpful in patient management and troubleshooting.
There are the four musical programs. The meter of the music mimics the resting heart rate at 60 beats per minute, providing that profound relaxation response. Music is a perfect tool to use in treating tinnitus because it directly taps into that limbic system response where we process our emotions. We all know music that can make us happy, and there is music that makes us relax. There is nothing that comes close to the effect that music can have on the limbic system and the stress response associated with tinnitus. The Oasis is designed for patients with moderate to severe tinnitus disturbance. As a guideline, we use a Tinnitus Reaction Questionnaire (TRQ) score of greater than 35. This has been our gold-standard product in the United States since 2007. It is clinically proven, tried and tested; we get great results with the Oasis.
Sanctuary
The Sanctuary is our newest product, released in 2014 at AudiologyNOW!. We have been seeing great outcomes thus far. It is designed for patients who need more situational tinnitus relief. In real-world terms, these are patients who do not have as high of tinnitus awareness. The Oasis is for those patients who hear their tinnitus much of the time and are impacted by it much of the time. Sanctuary patients may not be as aware of their tinnitus. They have tinnitus awareness of less than 50%, but their disturbance is fairly high. When they do hear their tinnitus, they need something to help them. We are utilizing what we know works from the Oasis product, but paring it down in a format that is extremely user-friendly for both the clinician and the patient.
There are four musical programs. There are three fitting ranges, providing a semi-customization of the music. There is a quick patient delivery model. There is no software required. You can literally fit a patient in about a minute and a half. Another great advantage is the entry-level price point. This increases access to tinnitus treatment for a lot of patients. It is designed for the lower to moderate tinnitus disturbance, with a guideline of a TRQ score of less than 35.
Both of these products are now available, and we are working on developments as a company with a new version of the Oasis and another product as well. Be on the lookout for more information to come.
Evidence-Based Treatment Options
Let’s move into the importance of providing patients with evidence-based treatment options. Why is that so important? By the time these patients reach your door, they have sought information from many different medical professionals. In a lot of cases, they have been given very little information and presented with few to no options for their tinnitus. They are frustrated. In addition to that, they have tried several over-the-counter treatments to no avail. They may have spent a lot of money, time, and effort to try to do something about this problem. They are also skeptical. Sometimes they are convinced that there is nothing that can be done because they have been told that for so long. It is our job to give them confident treatment recommendations and tell them why we feel it is a good option for their particular case.
Neuromonics has the only tinnitus product on the market with more than 11 years of documented success. No one else currently comes close. We have published peer-reviewed clinical studies in diverse settings (e.g., U.S. Department of Veterans Affairs – Veterans Administration – private practice, and Department of Defense) with a wide range of patients. We have consistently delivered ranges of success between 72% and 96% with in-house clinical trials as well as 10 independently replicated studies that, in some cases, achieved even better results than our in-house studies. There is a lot of confidence you can place in that type of data. We have studied more than 900 patients; this gives a patient the sense of security that this product has worked for a lot of people.
Figure 1 is a summary of all of the data that has been published up to this point. The first four studies listed in the figure were conducted in-house at Neuromonics. The sheer volume of patients and the different etiologies that were studied allowed us to gather a lot of information, and you can apply it clinically to your patients.
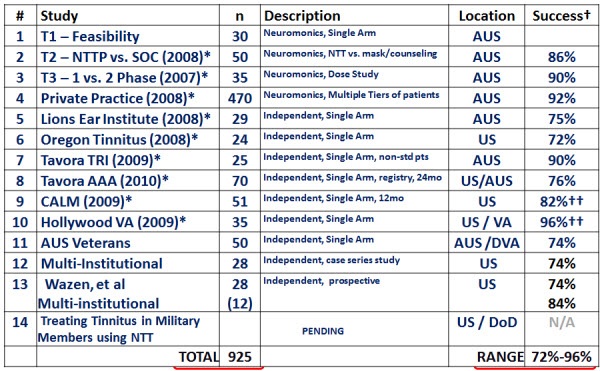
Figure 1. Summary of studies conducted with Neuromonics’ devices, including results.
The private practice trial (Hanley, Davis, Paki, Quinn, & Bellekom, 2008) included seven clinics with nine different audiologists. The patients had a variety of etiologies, referral paths, and socioeconomic and demographic profiles. Of all the participants, 72% were male. The mean age was 56 years, with an age range of 19 to 88, and tinnitus duration of 11 years. Nearly half of all the participants had tried other treatments previously. Going back to the level of skepticism, that is huge. They had tried something else and it had not worked, and they needed further intervention. A standardized treatment protocol was used, namely the Oasis device. The TRQ was used as the primary pre- and post-treatment measure, as well as tinnitus awareness, minimum masking levels. LDLs were also tracked. Of 470 patients, 85% progressed with treatment. These patients were divided into three patient suitability tiers based on specific characteristics (Figure 2).
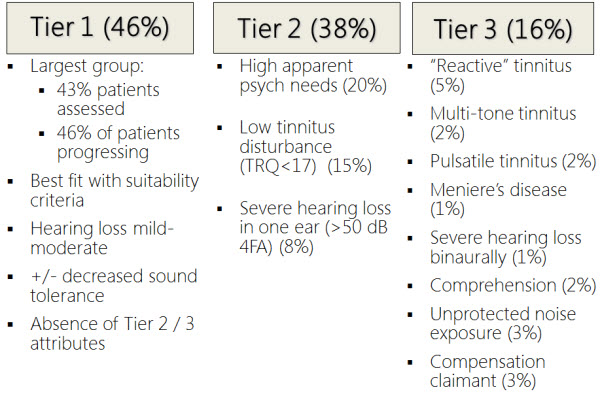
Figure 2. Three tiers of patient suitability criteria.
The largest group was Tier 1, and these were the most suitable patients, accounting for about 46% of the total group. They had mild to moderate hearing loss or better. They may or may not have had decreased sound tolerance, and they had the absence of any Tier 2 or Tier 3 attributes.
Tier 2 patients had high apparent psych needs and additional issues with anxiety and depression. They may have also had a low tinnitus disturbance or a TRQ less than 17, as well as more severe hearing loss. Patients with a completely dead ear were included in this study.
Tier 3 patients encompassed the smallest percentage, and they had more of what we call non-standard factors, such as reactive tinnitus, multi-tonal pulsatile tinnitus, and Meniere’s disease, which is tricky with treatment. There was also more severe hearing loss. Some patients had comprehension issues, perhaps with some early-onset dementia. They had unprotected noise exposure, which is another inhibitor in progress. Then a few of them were compensation claimants, which added another layer to their treatment.
The private practice outcomes were as follows (Figure 3). Tier 1 patients did better than Tier 2 and Tier 3, which makes sense. However, Tier 1 patients had a 71% mean improvement in their TRQ score, which is quite large. Tier 2 patients had a 44% improvement, and Tier 3 increased 24%.
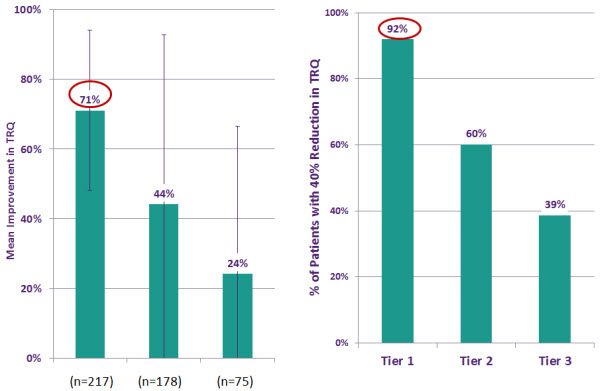
Figure 3. Outcomes of the private practice study. Mean improvement in TRQ scores (left) and Percentage of patient with 40% reduction in TRQ (right).
The data on the right panel (Figure 3) shows the percent of patients with at least a 40% reduction in their TRQ. In Tier 1, 92% of patients had at least a 40% reduction in their TRQ. We used 40% as a benchmark for success, because some studies show up to 30% can be placebo. We wanted to go beyond that and step it up to 40% as a success outcome. Even those patients with more complicated, nonstandard factors in Tier 2 and Tier 3 still had measurable success with treatment. Tier 2 had 60% of patients with a 40% reduction and Tier 3 had 39%. This goes along with expectation management. Did Tier 3 patients with reactive tinnitus get outcomes as good as the Tier 1 patients? No, but there is still a measurable improvement. We have to talk with our patients about whether or not this is enough. Is this still something with which they want to proceed and work on with that measurable amount of improvement available?
Hyperacusis Benefit
Hyperacusis benefit is often overlooked. I would like for you to understand the improvement that can be expected in patients with decreased sound tolerance and have that as part of your treatment goals. In Tier 1 patients, 67% had at least a 5 dB improvement in their LDLs with a mean improvement of 11 dB. Anecdotally, I see these LDLs improve sometimes 15 to 20 dB in a very short period of time, like 6 to 8 weeks. I certainly want you to consider these patients and show them this data. This is something with which we can help.
Furthermore, after 6 months, 95% of patients were able to achieve at least a 40% reduction in their tinnitus disturbance (Davis, Paki, & Hanley, 2007). That is measured by the TRQ. Eighty-four percent were able to achieve at least a 40% reduction in their awareness, or the amount of time that they actually heard their tinnitus; 78% got at least a 5 dB reduction in their minimum masking level, which means that their perception of the tinnitus was softer. Lastly, 69% were able to get at least a 5 dB improvement in their overall LDLs. These are big numbers and ones on which you can stand when recommending Neuromonics to your patients.
This is what means the most to the patient who has come into the office looking for an effective treatment option. They want to know if they are going to get relief from their tinnitus. Will they be able to sleep better? Can they gain a sense of control and get the ability to relax? The answer is yes. They can achieve those things.
Some of the advantages of Neuromonics are rapid relief and sense of control, improved relaxation and sleep, and reduced awareness and disturbance. Another benefit we found in our clinical trials was the improved tolerance of loud sounds. There are a lot of patients who could benefit from that. The long-term benefit is that this is not something they have to do for the rest of their lives. The typical treatment time is six to eight months, and then they move into a maintenance phase, using it occasionally. As we know, stress is a trigger for tinnitus. They have the device available to them to use when those stressful situations arise. Then there is the proven efficacy with more than 900 subjects studied.
Counseling
Let’s go into key counseling concepts. The No. 1 key to success is being confident in your recommendations. Why are you recommending this treatment for the patient? What results and characteristics are you using to indicate that a treatment option will be good for them? Remember that some of these patients are skeptics; many of them have been through the ringer already. They need to know why your recommendation is a good option. Certainly, you should reference clinical data and your own experience. For those who are new to tinnitus treatment, you may not have a whole lot of your own experience yet. That clinical data is going to be very useful to you in helping patients to understand why this is the option you have chosen for them.
Insisting on a positive prognosis is a counseling concept I cannot stress enough. These patients can sometimes be “glass-half empty” people. There is a level of pessimism there, and rightly so. Tinnitus is a daily struggle and they need help. Insist on the positive prognosis. Let them know that you are recommending these treatment options because of specific reasons and that they will do well if they work with you, together.
Another key is to acknowledge their desire for a quick solution. Everyone wants the silver bullet, but that is just not how it works. We need to acknowledge that it is reasonable for them to want that, but that is not the reality, and you need to educate them as to why. I use a physical therapy analogy. If you have an issue with your knee or your shoulder, there is no quick fix for it. Over time with consistent therapy, you can make improvements to those specific areas. That is the same thing you will do with tinnitus. It is not a one-pronged approach. You have to look at tinnitus comprehensively. What are the different elements involved? Tease them apart and get to the bottom of each one. That may be outside of what we feel comfortable in doing in the office with patients.
We want to facilitate a discussion of tinnitus emotions. This is typically not too difficult. Patients usually want to talk about this, and while we want to have a collaborative type of counseling style, I do find that directive counseling is helpful. They can get lost in their tinnitus. It can become this big, gray, nebulous entity. They do not know where it begins or where it ends. We are there to guide them through and help them to realize what parts of their lifestyle are affected by their tinnitus, and then explain what we can do about it. While we want to work together with the patient, we also need to provide them that directive type of counseling with focus, a purpose, and a plan.
We also need to identify and challenge any cognitive distortions they have. Examples of that would be, “I could hear well if I did not have my tinnitus.” That is not the reality. The tinnitus is not what is keeping them from hearing well. Sometimes it can translate into a processing problem, but by and large, patients with tinnitus do have some hearing loss. They need to address that in addition to their tinnitus treatment.
Another example of a cognitive distortion would be, “If my son would make better grades in school, I wouldn’t have my tinnitus.” Maybe the stress around his poor academic performance is making the tinnitus worse, but it is not the specific issue. Those are the things that we have to help our patients learn. We have to clear up misconceptions and provide them with the facts. Give them a clear and directed plan for success.
We also need to reinforce incremental changes. This is a marathon, not a sprint. We will use the TRQ and our test battery to measure the tinnitus impact as well as any improvements that they make. Gradual changes are not always apparent. I think about my hearing aid patients who were not able to hear much conversation prior to being fit. We fit them with hearing aids and now they want to hear conversation from four rooms away with the sink running. That is not a realistic expectation. The way to safeguard against those types of issues is to develop a list of goals at the treatment outset. Ask what they want out of this process and what you can realistically do together to help manage the impact of their tinnitus. This way we understand how we are going to change specific issues with treatment, and we can give them periodic report cards showing the progress of the treatment intervention.
We need to encourage our patient to stop self-monitoring and stop checking in with the tinnitus. We have some patients who will keep a journal on the length and characteristics of their tinnitus. That is counterproductive to this process. Our role as their clinician is to monitor the tinnitus at those different benchmarks in their treatment and to make sure that they are meeting those milestones. It is not their job. Continuing to self-monitor and research the tinnitus causes them to be more focused and aware of it, when we are trying to help them do the exact opposite. Some counseling in that area can be beneficial.
Troubleshooting
When troubleshooting, we always need to look at lifestyle factors that may impede a patient’s progress. Let’s say we start treatment. We fit them with a device, everything is going well and we see them at their two-week check. Things are great. Then we see then again at the eight-week appointment. We read the data logging and their TRQ has jumped up 20 points. What has changed from week two to week eight? Have there been any periods of acute stress? What is going on at home or at work that may have led to this increase in perception? We need to help the patient to realize that it is normal and okay. It is part of the process, and you are going to keep doing what you are doing, because we know the benefit that we have already been able to achieve from it. We just need to work to get back to that point by building confidence in the process.
Many patients will continue to expose themselves to high levels of noise or have noisy hobbies. We have to make sure that they are protecting their hearing in those situations and that they understand the impact that can have on their treatment.
Also, anytime they are straining to hear can make an impact. I had a patient that started with the Oasis treatment. He had a mild precipitous loss, but based on his lifestyle, he did not perceive any communication difficulties. He was retired. He did some volunteer work, but it was not anything social or interactive. He came back for a follow-up appointment and his TRQ had gone up quite a bit. In speaking to him, he had changed his volunteerism to a position at the hospital as a patient liaison, and he was in crowded, noisy hallways trying to help patients and visitors find hospital rooms. It was a totally different scenario. For him, a fitting with hearing aids alongside the Oasis treatment was helpful in treating both issues.
Lack of sleep can go under the radar if you have patients who are perpetually bad sleepers. They have terrible sleep hygiene and they are not getting an adequate amount of sleep a night. They may be using electronics before they go to bed, watching TV, or browsing their phones, iPads or computers; all those things can definitely detract from being able to fall asleep in a timely manner and then stay asleep. We want to make sure that we give them information and tips on how to have good sleep hygiene and get an adequate amount of sleep. Sleep deprivation has been shown to increase patients’ tinnitus perceptions.
Tinnitus Coach
Getting into the role of the tinnitus coach. Who is the tinnitus coach? We may need to refer outside of our office to a psychologist that can help patients deal with any significant anxiety or depression issues. Sometimes there can be the presence of suicidal ideation. There can be cognitive distortions or mindset barriers. I had a patient not long ago who continued to believe he was never going to get any better, no matter what information, education, or clinical data we gave him. He had decided that. We set him up with a psychologist to help him in working on those mindset barriers.
We found that the best professional for the role of tinnitus coach is a psychologist specializing in cognitive behavioral therapy (CBT). They employ a directive style of therapy when these thoughts and feelings come up to help patients realize the truth instead of the self-talk, which is keeping them from progressing as they should. Some patients will also have a bit of grief or anger over whatever caused their tinnitus. Sometimes this can be a traumatic event, such as with a car accident or our veterans returning from theaters of war. The psychologist can be help in those instances. These are things that extend beyond our scope of practice and comfort, and we should enlist the help of someone like this to give our patients every tool accessible to them to overcome their tinnitus challenges.
Case Studies
To finish, we have some patient case studies. These were shared from a few of our certified providers.
Case #1
This is a 40-year-old college professor. Per his description, he has had ringing tinnitus for several decades. It worsened last year, and he was told that there is nothing he could do about it. He met with a Neuromonics provider, and they decided to fit him with the Oasis device. Prior to fitting, his TRQ score was 52. Some of his lifestyle impact had to do with sleep. He was waking up several nights per week and was not able to go back to sleep. It also bothered him when he awakened and tried to fall back asleep. It made him avoid both quiet and noisy environments.
At the completion of treatment at 6 months, his TRQ score went from 52 to 27. He is no longer awakened during the night by his tinnitus. He is getting not only an appropriate amount of sleep, but also quality sleep, which has made a huge difference in his life. He now has several mornings a week without tinnitus. He wakes up and it is not there. During the day, his tinnitus has receded to the point where he has to think about it to notice it is there. If it is quiet enough and we search for it, most of us can hear some level of tinnitus. This has made a big difference in his day-to-day quality of life, and he feels that he has been successful with treatment.
Case #2
This patient had a bilateral, high-frequency sensorineural loss from 4000 to 8000 Hz. The TRQ was 71 with 90% awareness and disturbance. She described it as screaming and that her teeth hurt. She has had tinnitus for 18 years, and the treatment goals were to give the patient a sense of control of the tinnitus, improved concentration and lessen the bad tinnitus days. Together, with her provider, they decided to fit the Oasis.
At two months, the patient’s TRQ score went from 71 to 59, with 70% awareness and disturbance. The two-month mark is typically when we transition to Phase 2, but they decided that the way she was wearing it was not optimal to get the most benefit from the treatment. The Oasis works best if you focus or target your usage at the time when the tinnitus is most disturbing, not just out of convenience. They decided to keep her on Phase 1.
At the four-month follow-up, she was switched to Phase 2 because her TRQ score had gone to 35 with 70% awareness and disturbance. At the 7-month follow-up, she then had a TRQ of 22, with 50% awareness and disturbance, and she was moved to maintenance phase. She is now feeling that sense of control and her tinnitus goals have been met.
Case #3
This case has less to do with the TRQ numbers or awareness and disturbance. This is more from a patient’s perspective. This patient described the tinnitus as buzzing or static sound in his ears, and stated that he lost the freedom to relax. He felt he was not as calm of a person, he was easily irritated, and took less part in social gatherings. He started to pull away from others, especially his wife and children. He had big quality-of-life issues here.
The patient was fit with the Oasis. He has now regained that sense of control. He has regained the ability to relax, and he feels much better overall. He reported an overall increased quality of life. That is why we do this. We are working to help patients regain the things and people that they love and have lost as a result of their tinnitus. We definitely have the tools to be able to help you and your patients to do that.
Questions and Answers
What are the candidacy requirements for a patient with the Sanctuary device?
We are using the TRQ guideline of 35 and below. This is only one piece of the puzzle. You also want to look at their tinnitus awareness; how much are they aware of the tinnitus? If that is high, the Oasis is typically a better choice because they need more of a formal approach to treatment. However, if the tinnitus is more situational and they need help during those specific times, then the Sanctuary is a great choice for them. This is also available at the entry-level price point.
References
American Academy of Audiology. (October 2000). Audiologic guidelines for the diagnosis & management of tinnitus patients. Retrieved from https://www.audiology.org/resources/documentlibrary/Pages/TinnitusGuidelines.aspx
American Speech-Language-Hearing Association. (November 2003). Scope of practice in audiology. Retrieved https://www.asha.org/policy/SP2004-00192/
American Tinnitus Association. (June 2014). ATA's top 10 most frequently asked questions. Retrieved from https://www.ata.org/for-patients/faqs
Davis, P., Paki, B., & Hanley, P. (2007). Neuromonics tinnitus treatment: Third clinical trial. Ear and Hearing, 28(2), 242-257.
Hanley, P. J., Davis, P. B., Paki, B., Quinn, S. A., & Bellekom, S. R. (2008). Treatment of tinnitus with a customized, dynamic acoustic neural stimulus: Clinical outcomes in general private practice. The Annals of Otology, Rhinology and Laryngology, 117(11), 791-799.
Cite this content as:
Keaton, C. (2014, July). Your role in treating the tinnitus patient: What’s your professional responsibility? AudiologyOnline, Article 12792. Retrieved from: https://www.audiologyonline.com


