For many years, audiologists have relied on the results of pre-fitting hearing tests to predict patient benefit from amplification in everyday listening situations. For the typical clinician, this usually involves looking at the results of the pure-tone audiogram, word recognition scores, and other tests gathered at the pre-fitting appointment to forecast success with amplification. In today's era of evidence-based practice, audiologists must question the practice of using test results obtained during the routine pre-fitting evaluation to make predictions about real-world benefit with amplification. The purpose of this paper is to review why predicting potential benefits obtained from hearing aids is important for consumers, and what current pre-fitting tests are available to help make these predictions.
There are three reasons why audiologists might be interested in predicting how patients will perform in the real world with hearing aids. First, predicting benefit allows patients to leave the pre-fitting appointment with a more precise and individualized idea as to how much benefit they are going to be receiving before they actually start using hearing aids. Recent research indicates that consumers are better educated than ever before. Largely due to the Internet and search engines like Google, the average consumer knows they have a wide range of choices for products and price points. Due to this increasing consumer power, audiologists must be better equipped to make clinical decisions that predict real-world benefit after the patient's acquisition of new hearing aids.
Second, being able to predict benefit allows the audiologist to position herself as the expert. Experts certainly do not have all the answers, but they are able to take meaningful information, organize it, and accurately inform the patient about what should be expected following treatment. This concept is not unlike what surgeons do prior to an operation. They are able to provide the patient with a prognosis of expected outcome in their everyday living situations, using available test results.
Finally, all of us feel a little more at ease with our big-ticket purchases when we are offered some reassurance that it will indeed work in the places we need it most. If audiologists can rely on certain pre-fitting tests to more accurately predict real-world outcomes with hearing aids, there is an increased chance patients will feel more confident in their decision to purchase hearing aids.
Evidence-Based Review of Current Tests
In order to determine hearing aid candidacy, a battery of audiological tests are conducted during the pre-fitting appointment. According to numerous surveys conducted over the past several years, nearly every audiologist conducts pure-tone and speech audiometry during the pre-fitting hearing aid evaluation. Although other tests, (e.g., speech audiometry using noise) are slowly becoming part of the essential pre-fitting hearing aid selection battery, they are not routinely conducted by the majority of audiologists.
The traditional test battery used during the hearing aid selection process has a long history rooted in diagnostic audiology. Both pure-tone threshold testing and speech audiometry were originally used to identify retrocochlear pathology, and are an integral part of the pre-fitting hearing aid selection test battery today. Although there are many valid reasons for conducting the traditional pre-fitting test battery, such as finding the site of auditory disorder and assisting in the alignment of patient expectations with real-world hearing aid performance, the purpose of this article is to evaluate the predictive value of pre-fitting audiological tests, and offer alternatives if the traditional tests have little or no predictive power. If it is determined through a thorough evidence-based review of current tests that popular pre-fitting tests do not predict hearing aid outcome, then the results of these traditional tests should not be used to make important hearing aid selection and fitting decisions.
Using the five steps of audiological test Evidence Based Practice (EBP) and six levels of evidence outlined by Cox (2005), this article presents a review of the evidence published in peer reviewed journals over the past 25 years in an attempt to answer the following clinically relevant question: "Are there real-world outcome measures from adult patients to support the use of pure-tone audiometry as a pre-fitting selection tool?" In order for the evaluation of the evidence to be considered clinically effective, studies were included for review only if they met the following criteria:
- Published in a peer-reviewed journal between 1980 and 2008;
- Research designs used only randomized controlled studies and meta-analyses of high quality studies (Level 1 and Level 2 evidence), and non-randomized intervention studies (Level 3 evidence);
- Used adult subjects with hearing impairment;
- A self-report measure of real-world hearing aid outcome was conducted during the post-fitting follow-up process;
- Testing protocols were confined to pure-tone audiometry because previous evidence-based (EB) review articles have already addressed the predictive relationship of speech audiometry (Killion & Gudmundsen, 2005;Taylor, 2007), and determined that there is not a predictive relationship between pre-fitting speech audiometry scores and real-world hearing aid benefit.
- For this EB review, all studies were obtained by searching Pub Med using key words. A study was excluded if any one of the characteristics listed above were not met. Exclusion decisions were based on a thorough reading of the abstract. Where insufficient information was available in the abstract to make a decision on exclusion or inclusion, the full paper was read. A total of 31 abstracts meeting a key word search criteria were read. A total of seven articles, two of which were meta-analyses, met all of the criteria listed above and were included in the systematic evidence-based review. A summary of the results of these seven articles are shown in Table 1 below.
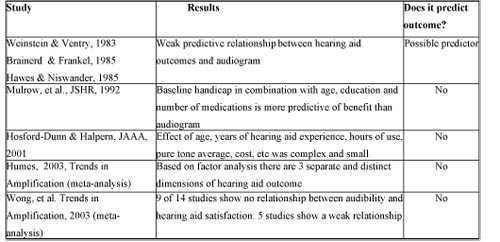
Click Here to View Larger Version of Table 1 (PDF)
Table 1. A summary of the studies meeting the criteria for inclusion in the evidence-based review of predictive value of pure-tone audiometry.
Based on the results of this systematic review of the evidence, there is not a predictive relationship between the pure-tone audiogram thresholds and real-world hearing aid benefit. Although a valuable part of the diagnostic test battery, this finding calls into question the use of pure-tone threshold audiometry results to make predictive statements about hearing aid benefit in everyday listening situations.
Given these findings, as well as those of Killon & Gudmundsen (2005) and Taylor (2007), neither pure-tone nor speech audiometry scores should be used to make predictive statements about real-world hearing aid outcomes. If making predictive statements during the pre-fitting hearing aid evaluation appointment is considered a worthwhile investment in the clinician's time, alternative tests that effectively predict real-world results must be considered. Fortunately, over the past few years, two tests have emerged as effective predictors of real-world hearing aid benefit. These pre-fitting procedures, the Acceptable Noise Level (ANL) test and the Performance Perceptual Discrepancy (PPDIS), have some clinical evidence supporting their use as predictors of real-world benefit. Both procedures are reviewed in the next section.
The Acceptable Noise Level Test
Recently, the Acceptable Noise Level (ANL) test has emerged as a commercially available pre-fitting test. The ANL test, developed some 15 years ago by Anna Nabelek and colleagues at the University of Tennessee, measures the listener's reaction to background noise, while listening to speech. Research has proven the unaided ANL to be a good predictor of hearing aid use. Nabelek, Freyaldenhoven, Tampas, Burchfield, and Meunchen (2006) suggest that full-time hearing aid users have significantly lower unaided ANL scores than do part-time users or nonusers.
To establish the Acceptable Noise Level (ANL), the audiologist finds the patient's most comfortable listening level (MCL). Once the MCL is established, a multi-talker babble is added to the speech. The provider adjusts the babble to the maximum level that is acceptable for the patient. This determines the Background Noise Level (BNL). The acceptable noise level is then calculated as the difference between MCL for speech and the BNL. In other words, ANL=MCL-BNL (in dB HL). For example, if the patient's MCL is 60 and the BNL is 50, the ANL in this case would be 10. The lower the ANL value, the more noise the listener is willing to accept, and vice versa.
As previously mentioned, Nabelek, et al. (2006) indicated that unaided ANL scores were predictive of hearing aid usage. In their study, 191 participants, consisting only of experienced hearing aid users, were placed into three categories based on their use time with amplification. Group 1 (n = 69) were classified as full-time users, Group 2 (n = 69) were classified as part-time users, and Group 3 (n = 53) were categorized as nonusers. Results indicated that full-time users were able to accept greater amounts of background noise compared to the other two groups. A prediction of hearing aid use was able to be made by comparing part-time and nonusers with full-time users. Full-time or successful hearing aid users consistently had lower ANL scores. Stated differently, full-time hearing aid users were able to accept greater amounts of background noise when compared to part-time and nonusers.
Nabelek, et al. (2006) demonstrated that patients with very low (score of 7 or less) or very high (score of 13 or higher) ANL scores could be classified as either unsuccessful or successful users. Their study, however, used participants who had been wearing hearing aids, and then were asked to classify their use time by completing a questionnaire at some time during their first year of hearing aid use. In other words, the unaided ANL was not used as part of the routine pre-fitting assessment test battery.
In a recently published study in a non-peer reviewed journal, Taylor (2008) investigated the relationship between unaided ANL scores measured at pre-fitting appointments and real-world outcomes as measured on the International Outcome Inventory for Hearing Aids (IOI-HA). Results of this study suggest that for intrinsic dimensions of hearing aid outcome ("me and my hearing aids") the unaided ANL score is a very strong predictor of final outcome as measured by Factor 1 of the IOI-HA. This finding suggests that intrinsic factors related to hearing aid outcome, such as how patients feel about their hearing aids, can be predicted by the unaided ANL score.
Although the sample size was small for two of the three ANL groups in the Taylor (2008) study, there is a statistically significant trend suggesting that the unaided ANL score contributes to the final outcome as measured by the IOI-HA, with 16% of the overall IOI-HA score accounted for in the unaided ANL. More specifically, there is a significant finding that Factor 1 variables on the IOI-HA can be predicted from the unaided ANL score. Given the predictive relationship between Factor 1 ("me and my hearing aid") IOI-HA scores and the unaided ANL, knowing the unaided ANL scores at the pre-fitting provides quantifiable insights into how patient's perceive their handicap prior to using hearing aids.
Past research regarding the ANL has shown it to be good predictor of hearing aid usage (Nabelek, 2005). Although this is a positive finding, hearing aid use does not necessarily equate to overall hearing aid satisfaction and benefit. Results from this study are some of the first data to show that it may be possible to predict hearing aid benefit from the unaided ANL score. Given this finding, it is prudent for audiologists to begin conducting the ANL as a routine part of the pre-fitting hearing aid evaluation.
Performance-Perceptual Discrepancy (PPDIS)
In an attempt to reconcile the possible differences between objective measures obtained with speech audiometry and perceived difficulties in speech understanding, Saunders and colleagues (2004) developed the Performance-Perceptual Test (PPT). The PPT allows the audiologists to first test the patient's ability to understand speech in noise, using the Hearing in Noise Test (HINT) or other sentence-length speech-in-noise test, and compare it to subjective reports from the patient using the same test. The difference between the objective speech audiometry score and the patient's subjective perception of their ability to understand speech in noise is called the Performance Perceptual Discrepancy (PPDIS).
For the objective part of the test, the patient repeats the words that are heard, which determines the signal-to-noise ratio (SNR) at which the patient can understand 50% of the material. For the subjective part of the test, the audiologist adjusts the SNR based on whether the patient reports that they can "just barely understand everything that was said." The PPDIS is a measure of the extent to which listeners "misjudge" their ability to communicate in noise. Saunders et al. (2004) found that when the objective score is lower (a conversation can be followed in a more adverse SNR) than their subjective score, patients are underestimating their ability to understand speech in noise. While an objective score that is higher (a less adverse SNR is required to follow a conversation) than their subjective score, patients are overestimating their ability to understand speech in noise.
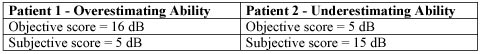
Table 2. A difference between the objective speech-in-noise audiometry score and the subjective score on the same test is the PPDIS.
The PPDIS has been reported to account for almost 15% of the variance of the score obtained on the Hearing Handicap Inventory for the Elderly/Adult (HHIE/A), with an additional 14% of the variance in the HHIE/A explained by the objective speech-in-noise score. In other words, the reported unaided hearing handicap is affected as much by the patient's perception of the ability to understand speech in noise as it is by the actual ability to hear (Saunders & Forsline, 2006a).
In another study investigating aided listening;patients were classified into three groups according to their HHIE/A score predicted from their pure-tone audiogram. It was determined that patients reporting more handicap than expected, based on their pure-tone audiogram, had a negative PPDIS (that is, they had a tendency to underestimate their hearing ability in noise). Based on their work in this area, Saunders and Forsline (2006b) have created PPT-Based Counseling. Their PPT-Based Counseling method allows the audiologist and patient to engage in a meaningful discussion about communication difficulties in challenging listening situations. The content of this discussion is determined by the PPDIS in the following manner:
- Underestimators: PPDIS value is in the bottom third of normative scores.
- Accurate assessment: PPDIS value is between 33rd and 66th percentage of normative scores.
- Overestimators: PPDIS value is in the top third of normative scores.
Once the PPDIS value is determined, the information reprinted from Saunders and Forsline (2006b) in the table below can be used to systematically counsel the patient on how to cope in everyday listening situations.
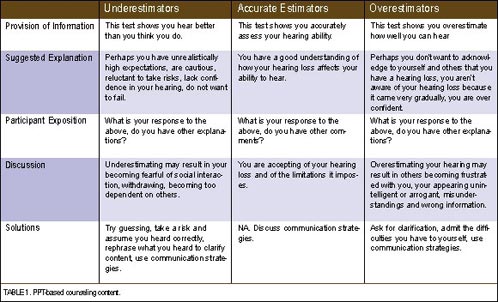
Click Here to View Larger Version of Table 3 (PDF)
Table 3. A review of how to use the PPDIS in the counseling of patients during the pre-fitting hearing aid selection process. Reprinted with permission from The Hearing Review.
There is very little evidence supporting the use of pure-tone and speech audiometry as predictors of real-world hearing aid benefit. Fortunately, two procedures, which are currently conducted by very few audiologists, have been shown to have some predictive ability. Based on this emerging evidence both the ANL and the PPT can be used during the pre-fitting appointment to make accurate predictions about hearing aid outcomes.
References
Brainerd, S. & Frankel, B. (1985). The relationship between audiometric and self-report measures of hearing handicap. Ear and Hearing, 6(2), 89-92.
Cox, R. (2005). Evidence-based practice as a provision of amplification. Journal of the American Academy of Audiology, 16 (7), 419-438.
Hawes, N. & Niswander, P. (1985). Comparison of the revised Hearing Performance Inventory with audiometric measures. Ear and Hearing, 6(2), 93-97.
Hosford-Dunn, H. & Halpern, J. (2001). Clinical application of the SADL scale practice II: Predictive validity of fitting variables. Journal of the American Academy of Audiology, 12(1), 15-36.
Humes, L. (2003). Modeling and predicting hearing aid outcome. Trends in Amplification, 7(2), 41-75.
Killion, M.C., & Gudmundsen, G.I. (2005). Fitting Hearing Aids Using Clinical Prefitting Speech Measures: An Evidence-Based Review. Journal of the American Academy of Audiology, 16(7), 439-447.
Mulrow, C., Tuley, M., & Aguilar, C. (1992). Sustained benefits of hearing aids. Journal of Speech and Hearing Research, 35(6), 1402-1405.
Nabelek, A. (2005). Acceptance of background noise may be key to successful fittings. The Hearing Journal, 58, 10-15.
Nabelek. A., Freyaldenhoven, M., Tampas, J., Burchfield, S., & Meunchen, R. (2006). Acceptable Noise Level as a predictor of hearing aid use. Journal of the American Academy of Audiology, 17(9), 626-639.
Saunders, G., Forsline, A., & Fausti, S. (2004). The Performance-Perceptual Test (PPT) and its relationship to unaided reported handicap. Ear and Hearing, 25, 117-126.
Saunders, G., & Forsline, A. (2006a). The performance-Perceptual Test (PPT) and its relationship to aided reported handicap and hearing aid satisfaction. Ear and Hearing, 27(3), 229-242.
Saunders, G. & Forsline, A. (December 2006b). The Performance-Perceptual Test (PPT) and its application to hearing aid counseling. The Hearing Review. Retrieved July 8, 2008, from www.hearingreview.com/issues/articles/2006-12_08.asp
Taylor, B. (2007, May 7). Predicting real world hearing aid benefit with speech audiometry: An evidence-based review. Audiology Online, Article 1802. Direct URL: www.audiologyonline.com/articles/article_detail.asp?article_id=1802 Retrieved July 8, 2008, from the Articles Archive on www.audiologyonline.com
Taylor, B. (2008). The Acceptable Noise Level test as a predictor of real-world hearing aid benefit. The Hearing Journal (in press).
Weinstein, B, & Ventry, I. (1983). Audiologic correlates of hearing handicap in the elderly. Journal of Speech and Hearing Research, 26(1), 148-151.
Wong, L. Hickson, L., & McPherson, B. (2003). Hearing aid satisfaction: What does research from the past 20 years say? Trends in Amplification, 7(4), 117-161.


