Editor's note: This article is an edited transcript of the live expert webinar presented on November 3, 2010.
Robert Battista: Today I'll talk about bilateral cochlear implantation and the benefits of having two implants in terms of speech perception in quiet and in noise, localization ability and implications on language development in children. I'll review the auditory perceptual disadvantages caused by unilateral hearing loss, and the advantages of bilateral hearing, which is the rationale for bilateral cochlear implantation. I'll also contrast simultaneous and sequential implantation, talk about pros and cons of each, and review some published literature. My associate, Dr. Kathleen Highhouse, will review clinical case studies of three adults who use bilateral cochlear implants (CI), two of whom were implanted simultaneously.
Disadvantages of unilateral hearing
We know that children who are deaf in one ear often have speech perception and language acquisition difficulties (Bess & Tharpe, 1984; Culbertson & Gilbert, 1986; Ruscetta, Arjmand, & Pratt, 2005), and that those with unilateral hearing loss have difficulty hearing in the presence of noise, and are also unable to localize sound.
Advantages of bilateral hearing
Having good hearing in each ear gives us optimal access to sound arriving at either ear. Speech comprehension in quiet and in noise is improved in a binaural listening condition for three reasons: 1) binaural redundancy effects due to summation, 2) the squelch effect, and 3) most importantly - the head shadow effect (Litovsky, Parkinson, Arcaroli & Sammeth, 2006; Dunn, Tyler, Oakley & Gantz, 2008). Summation contributes to better speech recognition in noise because the brain receives some redundant info from each ear, and can draw more meaningful acoustic information from those two sources than it could from a single ear's input. The head shadow effect is the most important thing about binaural hearing in terms of the ability to help localize sound and also to eliminate background noise. In the context of bilateral cochlear implants, we note better speech comprehension in noise, better sound localization, and improved ease of listening.
Before I continue, I should review some terms that are important in discussing the topic of bilateral cochlear implantation. These terms are: bilateral, bimodal, and binaural hearing, as well as simultaneous and sequential bilateral implantation. The term bilateral is used to describe sound being presented to both ears at once. Bimodal refers to sound being presented to each ear using a different modality: a cochlear implant on one ear (electrical stimulation) and a hearing aid on the other ear (acoustical stimulation). Binaural hearing refers to the integration of bilateral sound input as it travels up the auditory pathway. Simultaneous cochlear implantation involves the implantation of a cochlear implant into each ear during the same surgery. Sequential implantation involves two surgeries, and these may be weeks, months or many years apart. I'll talk about the pros and cons of simultaneous versus sequential implantation a little later.
Findings: Bilateral cochlear implants
Let's review some of the literature to see what kind of results we're getting with bilateral cochlear implants.
Speech recognition in the presence of noise
In a study of 34 simultaneously-implanted bilateral cochlear implant users, Litovsky et al. (2006) found that they were able to sustain a 50% correct score on the BKB-SIN test at a lower signal-to-noise (SNR) ratio using their bilateral implants than when using only one of their implants. When only one implant was used, the SNR had to be increased to more favorable levels in order for the subjects to sustain that same performance level. In each of the three test conditions (noise from the left, noise from in front, noise from the right), these results were statistically significant after 3-months of bilateral implant use, with scores increasing further at the 6 month test. The bilateral fitting condition was superior regardless of the location of the noise. This confirms the superiority of bilateral cochlear implant use in recognizing speech in the presence of noise.
Sound localization ability using bilateral cochlear implants
Dunn et al. (2008) conducted a study of sound localization in sequentially-implanted cochlear implant users who had been using their bilateral implants for an average of 59 months. They found that sound location ability was 25° more accurate using both implants rather than using just one implant.
Clinical Questionnaire: APHAB
Patients with bilateral cochlear implants tell us it is much easier to hear with two implants than one, and we are seeing improvements in language acquisition in children with bilateral implants. Using the APHAB questionnaire, Litovsky et al. (2006) found statistically significant improvements in adult cochlear implant users' ratings on 3 of the 4 subscales in the APHAB: the ease of communication, background noise, and reverberant listening scales.
So, we have seen statistically-significant improvements in sound localization and in speech recognition in background noise, and, subjective ratings on three of the four subtests on the APHAB by bilateral cochlear implant users. The benefits of binaural cochlear implant use become apparent in as little as one to two months (Tyler, Dunn, Witt & Noble, 2007). In addition to these benefits, there are some other benefits to bilateral implantation. There is definite merit in providing bilateral neurological stimulation of the auditory pathways - especially for temporal lobe stimulation in the developing child's brain, and this stimulation is important now and in the future should new developments arise. In addition, with bilateral implantation, if one device fails, the user has a 'back up' unit. It is sometimes difficult to predict which ear will be the better implant candidate so bilateral implantation also removes the chance of selecting the ear with less potential. Now let's consider the arguments against bilateral cochlear implants.
Arguments against simultaneous bilateral cochlear implantation
Some of these arguments include increased operative time/surgical risk (due to prolonged anaesthesia, or fear of prolonged/permanent post-surgical dizziness), the large cost for two devices, loss of residual hearing, and the inability to use improved technologies/stem cell treatments or hair cell regeneration treatments in the future.
Operative time/risk of anaesthesia
For unilateral implants operative time used to be about 3 hours. Now we doing bilateral simultaneous implants in 2½ to 2¾ hours, so operative time is not an issue. Of course, we do pay close attention to anaesthesia, especially for young children. If they're too light, we will wait until they are bigger so that it is safe to anaesthetize them.
Increased surgical risk
The risks are minimal with cochlear implantation and the most common side effect we see is dizziness. Although we were initially concerned that bilateral cochlear implant patients were going to have significant dizziness - perhaps forever, our experience is that this does not happen. Patients who get bilateral simultaneous implants do not have any more problems with their balance than unilateral implant patients.
Damage to residual hearing
The concern about destroying residual hearing is a valid one. We do not recommend implanting people who have residual hearing. We're going to talk about some of those indications for implementation with or without residual hearing later on in the presentation.
Financial expense
If you are planning to get two implants eventually, then getting a bilateral simultaneous implantation saves you the cost of two hospital stays, two recovery times, and twice the anaesthesia.
Ability to utilize future technological advancements
Cochlear implant technology has improved tremendously over the years. As for exploiting future implant technology, there is a lot of potential for improvement. Advancements in circuitry and sound processing are likely, and can be delivered to the patient via changing or replacing the external sound processor device.
Ability to utilize future medical treatments - hair cell regeneration/stem cell treatments
This issue is one that concerns parents who are considering implanting two ears for their children who have a profound bilateral sensory hearing loss at birth. They debate on whether they should perhaps wait for newer technology, hair cell regeneration and/or stem cell research. In terms of hair cell regeneration and stem cell research, there is a lot of exciting research going on now, but it is still at least 10 years away from being utilized for hearing improvement. That is a long way off. Especially for children the question is: should the second ear be 'saved', for future cochlear implant technology or other therapies? And B. Robert Peters, M.D., of the Dallas Otolaryngology Cochlear Implant Program, has summarized this nicely: "Given that binaural hearing depends on bilateral input during a critical development period, if the second ear does not receive auditory input during the critical period of cortical development, later technology, no matter how advanced, will only provide input to a cortex incapable of receiving it."
Sequential bilateral cochlear implantation
What are the advantages of choosing sequential bilateral cochlear implantation, and how long can it be between the procedures? The clinical question is, should we wait?
The case for sequential Implantation
Zeitler et al. (2008) and other researchers have found that speech perception ability improves with bilateral implant use regardless of how many years have elapsed since the first implant was done, however there is slightly greater improvement when there is a shorter time span between the first and second implant procedures. Furthermore, children showed better speech perception in noise when implantation occurred at a younger age.
The case against sequential implantation
Sequential implantation might be more stressful for a child/family or for an adult patient, having to go through everything (surgery, recovery, repeat visits for mapping) again. And, of course, if enough time has passed, the equipment may be new so the user would have to adjust to using different technology than he is accustomed to using. The second implant need not be the same model or manufacturer as the first implant however. Some parents still in denial of their child's deafness may decline a second implant later, may not want to give up using the hearing aid, or may be concerned about the appearance of two implants on their child.
Is there a 'critical age' for implanting the second implant?
A natural question is: Is there a critical age (timeframe) during which to implant the second side? The answer is maybe. Numerous studies have addressed this, with conflicting results. Early studies indicated that a delay exceeding 3 to 3.5 years could slow or compromise binaural processing (Beijen, Snik & Mylanus, 2007; Gordon, Valero & Papsin, 2007; Mok, Galvin, Dowell & McKay, 2007; Papsin & Gordon, 2008). Presently, there is no known 'acceptable' time delay for sequential implantation (Zeitler et al. 2008). Some researchers have concluded that long delays between implants may not give the full benefits of bilateral implants (Tyler et al., 2007; Laske et al. 2009). One study by Graham et al. (2009) found that in teens/young adults who had had their first implant 16-18 years earlier, speech perception was poor with the second implant.
Candidacy for bilateral cochlear implants
While each patient is evaluated individually, there are some guidelines. Patients who have residual hearing that responds well to acoustic amplification (a hearing aid) wouldn't be implanted on that side. With people who have an ear that is anatomically atypical, we simply might be unable to insert the implant into that ear. Some patients are not emotionally ready to use a second implant, or they cannot pay for a second implant. However, more and more insurance companies are covering bilateral implants, sequentially or simultaneously. Medicare will cover a unilateral implant if a candidate scores less than 40% on the HINT in quiet, while some private insurers have less stringent criteria for implant coverage.
Robert Battista - Concluding remarks
We've reviewed the benefits of bilateral cochlear implantation, addressed some concerns, and compared sequential and simultaneous implantation issues. We've seen that sound localization, speech recognition in noise, and ease of listening are improved through the use of bilateral implants or bimodal listening as compared to monaural listening. We consider it best practices to provide binaural stimulation, either through hearing aids, implants or one of each. Now my associate, Dr. Kathleen Highhouse, will review several interesting case studies with you.
Case Studies
Kathleen Highhouse: I'm going to review three case studies with you. Two of them are for simultaneous implant recipients and one is for sequential. In each case, note that sound detection has improved, and that word recognition in quiet and in noise is also improved with bilateral cochlear implants.
Bilateral case study 1, RV
Male, age 69. History of progressive hearing loss through adulthood, and bilateral hearing aid use. First CI in left ear at age 67; second CI in right ear at age 69.
Pre-op testing of RV's speech recognition in quiet resulted in scores of 7% correct in his left ear, and 31% correct in his right ear on the HINT in quiet. His left ear was implanted, followed two years later by the right ear. His aided thresholds were considerably poorer than his CI thresholds, which is normal for CI users. What is important to note is his performance with his CI. At 2.5 years post-op in his left ear, he scored 92% correct on the HINT in quiet at 55 dBHL. At 1 year post-op in his right ear, he scored 92% correct on the HINT in quiet at 45dBHL. His binaural scores were 96% correct on the HINT in quiet, 80% correct on the HINT in noise at a SNR of +10, and on the CNC single word test, he correctly identified 70% of the words and 88% of the phonemes.
Figure 1 shows results for the left ear.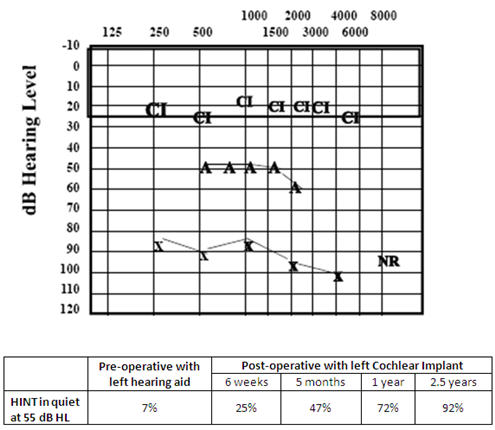
Figure 1. Audiogram and HINT scores for RV, left ear. X = unaided air conduction thresholds. A = aided thresholds with left hearing aid. CI = thresholds using left cochlear implant.
Notice his improvement in post implantation speech perception performance over time: his scores were 26% at 6 weeks post implantation, 47% at 5 months, 72% at 1 year, and 92% at 2.5 years. As you can see by these results, it can take some time to see the progress.
Figure 2 shows results for the right ear.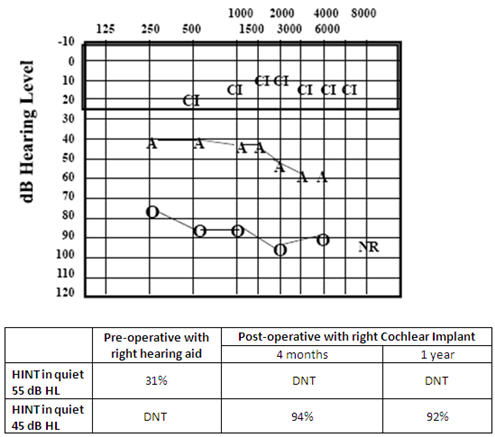
Figure 2. Audiogram and HINT scores for RV, right ear. 0 = unaided air conduction thresholds. A = aided thresholds with right hearing aid. CI = thresholds using right cochlear implant.
Using the right ear, RV scored very well (92%) at just 4 months, and this may be because it was the better ear. It seems that we see sequentially-implanted users improve more rapidly on the second implant, just as RV did. Bilaterally with cochlear implants, RV scored 96% for the HINT in quiet. As for his binaural performance, many times we find patients report that they do very well with their second implant in noise in restaurants, and in other real life situations, but when you put them in the sound booth the scores do not reflect the subjective reports of the users. However, RV did well on the HINT in noise (80% at SNR of +10).
Bilateral case study 2, WK
Female, age 44. Bilateral simultaneous implants. Progressive loss since childhood. Prior to implantation, right ear aided for 29 years, left ear aided for 15 years. Received bilateral simultaneous implants after sudden worsening of left ear, making it no longer aidable.
As you can see from the audiograms in Figures 3 and 4, WK had a severe-to-profound loss bilaterally and she received no benefit from hearing aids. Her better ear (the left) had taken a sudden sharp decline that steroids did not reverse. She decided that simultaneous implants were the best route for her.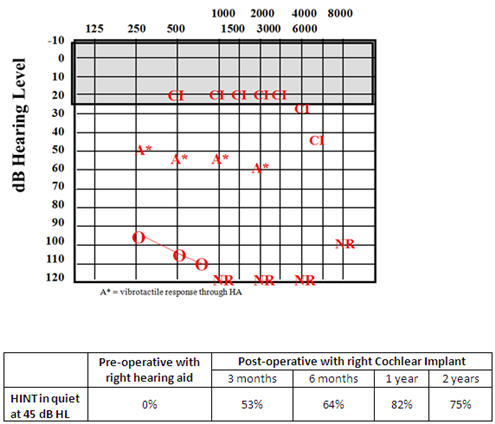
Figure 3. Audiogram and HINT scores for WK, right ear. 0 = unaided air conduction thresholds. A* = vibrotactile response through right hearing aid. NR = No response. CI = thresholds using right cochlear implant.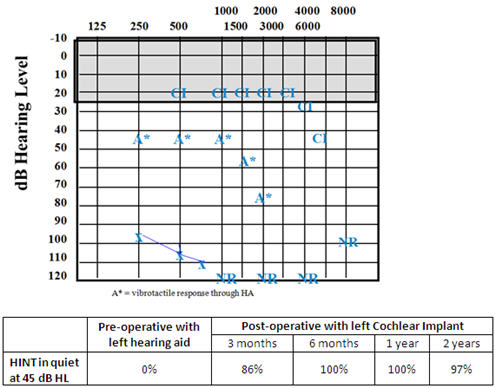
Figure 4. Audiogram and HINT scores for WK, left ear. X = unaided air conduction thresholds. A* = vibrotactile response through left hearing aid. NR = No response. CI = thresholds using left cochlear implant.
WK's pre-op right aided HINT score was 0%, but at 3 months post-activation of her CI, her score was 53%, then continued to improve to 82% at 1 year. Her pre-op left aided HINT score was also 0%, but at 3 months post CI activation she scored 86% correct, and achieved 100% at 6 months. Her bilateral score on the HINT in quiet at a 45 dBHL presentation level was 100% correct, and she scored 58% correct on the HINT in noise at a +10 SNR. WK was very happy with her decision to go ahead and do both implants at the same time and in fact she is trying to convince her husband who has hearing loss to go ahead and get one as well. She is definitely a strong advocate for bilateral implantation. Despite the 58% score when listening in noise, she reports that she does very well in noise. Because of her history of poor hearing, WK has always avoided using the phone and as of her last appointment had still been avoiding the telephone. Her goal for our next follow-up is to practice with the phone and get more comfortable with it. She should do very well with the telephone considering her scores.
Bilateral case study 3, NC
Female, age 44. Bilateral simultaneous implants. Progressive sensorineural loss for previous 9 years; wore bilateral hearing aids.
NC had normal hearing for most of her life and then had a progressive sensorineural hearing loss over the course of 9 years. She then lost a significant amount of her residual hearing a few months before she received her implants. Steroid treatment initially helped recover some of her hearing, but the second round only stabilized her hearing and there was no further improvement. NC's audiological results for the left ear are shown in Figures 5 and the right ear results are shown in Figure 6.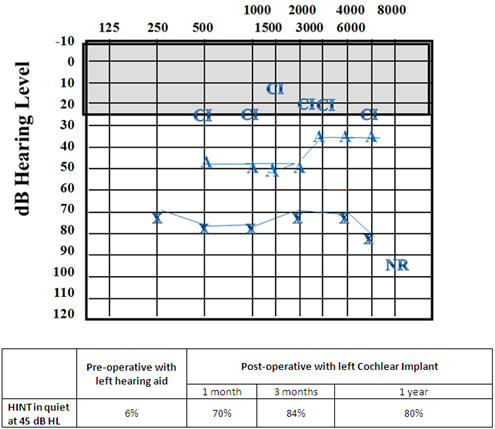
Figure 5. Audiogram and HINT scores for NC, left ear. X = unaided air conduction thresholds. A = aided thresholds with left hearing aid. NR = No response. CI = thresholds using left cochlear implant.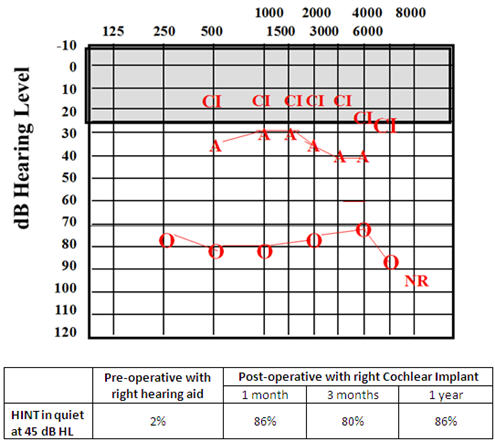
Figure 6. Audiogram and HINT scores for NC, right ear. 0 = unaided air conduction thresholds. A = aided thresholds with right hearing aid. NR = No response. CI = thresholds using right cochlear implant.
You can see from NC's unaided results in Figure 5 and Figure 6 that she had more pre-operative residual hearing than WK, but she did very poorly on the aided HINT sentence test in quiet at 45 dB HL presentation level: 6% on the left and 2% on the right. She enjoyed great benefit from her CIs right from the start, as you can see by her scores on this same test at one month post activation: 86% on the right and 70% on the left. At one year post CI her scores were 86% right and 80% left. Combined, her bilateral score on the HINT in quiet at 45 dB HL was 91%. NC reports that she does pretty well in restaurants and group settings but she only scored 12% when we tested her with the HINT sentence test in the soundfield with + 10 dB SNR. I think this test was done when she just had been using her CIs for six months, and she is due for follow-up where we will repeat the testing. It is possible she may do better.
We did conduct the CNC word test with NC although we tested each side individually. Her scores were good, with 80% on the right and 84% in the left ear but it should be noted that it was done using monitored live voice. All other testing was conducted using recorded stimuli.
Dr. Highhouse - Closing remarks
We have been excited to see our patients with bilateral CIs progress and to note improvements in performance in each ear. In our practice, patients with bilateral implants have done well and overall are very satisfied. We have also had patients who have done better with their second implant than their first, and we never would have known that had they not gotten the second implant. Of course, the decision to implant one ear or both, and in the case of bilateral implants to do them simultaneously or sequentially, needs to be made on an individual basis taking into consideration many factors, as we have discussed today.
References
Beijen, J.W., Snik, A.F. & Mylanus, E.A. (2007). Sound localization ability of young children with bilateral cochlear implants. Otol Neurotol,28,479-485.
Bess, F.H. & Tharpe, A.M. (1984). Unilateral hearing impairment in children. Pediatrics. 74(2), 206-216.
Culbertson J.L. & Gilbert, L.E. (1986). Children with unilateral sensorineural hearing loss: cognitive, academic, and social development. Ear Hear, 7(1), 38-42.
Dunn, C.C., Tyler, R.S., Oakley, S. & Gantz, B.J. (2008). Comparison of speech recognition and localization performance in bilateral and unilateral cochlear implant users matched on duration of deafness and age at implantations. Ear Hear, 29(3), 352-359.
Gordon, K.A., Valero, J. & Papsin, B.C. (2007). Auditory brainstem activity in children with 9 to 30 months of bilateral cochlear implant use. Hear Res, 233(1-2),97-107.
Graham, J., Vickers, D., Eyles, J., Brinton, J., Al Malky, G., Alesky, W. et al. (2009). Bilateral sequential cochlear implantation in the congenitally deaf child: evidence to support the concept of a 'critical age' after which the second ear is less likely to provide an adequate level of speech perception on its own. Cochlear Implants Int, 10(3),119-141.
Laske, R.D., Veraguth, D., Dillier, N., Binkert, A., Holzmann, D. & Huber, A.M. (2009). Subjective and objective results after bilateral cochlear implantation in adults. Otol Neurotol, 30(3), 313-318.
Litovsky, R, Parkinson, A., Arcaroli, J. & Sammeth, C. (2006). Simultaneous bilateral cochlear implantation in adults: A multicenter clinical study. Ear Hear, 27(6), 714-731.
Mok, M., Galvin, K.L., Dowell, R.C. & McKay, C.M. (2007). Spatial unmasking and binaural advantage for children with normal hearing, a cochlear implant and a hearing aid, and bilateral implants. Audiol Neurootol,12, 295-306.
Papsin, B. & Gordon, K.A. (2008). Bilateral cochlear implants should be the standard for children with bilateral sensorineural deafness. Curr Opin Otolaryngol Head Neck Surg, 16(1), 69-74.
Peters, B.R. (2006). Rationale for bilateral cochlear implantation in children and adults. White paper available from Cochlear Americas.
Ruscetta, M.N., Arjmand, E.M. & Pratt, S.R. (2005). Speech recognition abilities in noise for children with severe-to-profound unilateral hearing impairment. Int J Pediatr Otorhinolaryngol, 69(6), 771-9.
Tyler, R.S., Dunn, C.C., Witt, S.A. & Noble, W.G. (2007). Speech perception and localization with adults with bilateral sequential cochlear implants. Ear Hear, 28(2 Suppl), 86S-90S.
Zeitler, D.M., Kessler, M.A., Terushkin, V., Roland, T.J. Jr, Svirsky, M.A., Lalwani ,A.D. & Waltzman, S.B. (2008). Speech perception benefits of sequential bilateral cochlear implantation in children and adults: a retrospective analysis. Otol Neurotol., 29(3), 314-325.



