&Abstract
The assessment of (central) auditory processing disorders, (C)APDS, is an aspect of audiology with which many clinicians seem to struggle, especially when working with children. Surveys indicate that audiologists' knowledge and skills in this area are lacking. Additionally, it is difficult for audiologists to start this testing in their clinics, because no single test battery has been identified as being the gold standard. In 1996, the American Speech-Language Hearing Association (ASHA) wrote a consensus statement on central auditory processing, or (C)AP (ASHA, 1996). Nearly a decade later, ASHA updated that statement with a working group document that contains recommendations to guide audiologists in assessing children for (C)APD. This article will discuss information from that document, as well as provide clinical examples to elaborate upon it.
In 2005, the American Speech-Language Hearing Association (ASHA) approved its working group document on (C)AP (ASHA, 2005). The purpose of this document was to update and augment the 1996 ASHA position statement and to help guide audiologists in the diagnosis (i.e., selecting the necessary tools to accurately perform (C)AP evaluations) and intervention (i.e., selecting the type of therapy) of (C)APD. This is valuable information because audiologists seem to have some trepidation when considering and performing (C)AP evaluations. Emanuel (2002) found that none of the 192 responding audiologists followed the recommended minimum (C)AP test battery outlined in a Bruton conference in 2000 (Jerger & Musiek, 2000). Emanuel indicated that this may be due to the lack of supporting literature for the tests (most audiologists used the SCAN-C, which comes with a manual). She also speculated that most work sites did not have electrophysiologic test equipment and therefore, were unable to perform any of those tests (e.g., middle latency response (MLR) testing). Chermak et al. (1998) queried audiologists about their graduate school education and found that 78% of audiologists were less than 50% satisfied with their school's coursework in the area of (C)AP. In addition, most audiologists reported fewer than five clinical hours performing (C)AP evaluations during their education.
Most recently, a webinar on AudiologyOnline (Erickson, 2008), asked participants to rate their level of readiness (or ability) in performing (C)AP evaluations. Of the 86 audiologists who responded, 22 said they were not ready, 10 said they were ready because they had to do the testing, 33 said they were ready but needed assistance, 12 said they were firmly ready and able to do the testing, and 9 said they were confident in their ability to test. The majority (65 audiologists) of those who responded did not feel they had a sound knowledge base for (C)AP testing, which was reflective of them taking the "101" seminar. Taken together, these reports provide documentation and insight as to why audiologists experience apprehension regarding (C)AP testing.
These inadequacies are addressed in ASHA's 2005 technical paper on (C)APD. The document augments the original document by more clearly defining the role of the audiologist in (C)AP assessment. The position paper and technical paper, focus on audiologists' knowledge base of (C)AP. These papers state that education, training, and experience are all necessary for the audiologist performing (C)AP evaluations. Pursuing additional education and/or training is recommended in the 2005 document.
(C)AP Case History
The 2005 technical paper also refines the definition of (C)AP by being the first to place the word "central" in parentheses. In 2000, it was recommended that "central" be removed from "central auditory processing" to emphasize interactions at peripheral and central sites (Jerger & Musiek, 2000). In contrast, the ASHA technical paper states that "central auditory processing" and "auditory processing" are synonymous for the purposes of the technical report;therefore, "central" was made parenthetical.
In the 2005 technical paper, ASHA outlines the basic necessities in (C)AP evaluations. Once an audiologist begins doing (C)AP evaluations, the intake of a thorough case history is recommended. The paper recommends that the following categories should be included when obtaining the history on an individual:
- family/genetic history
- pre-, peri-, and post-natal course
- health status
- communication
- listening and auditory behavior
- psychological factors
- educational achievement
- social development
- cultural and linguistic background
- prior related therapy
- current therapy (ASHA, 2005)
Hearing Evaluation
A full peripheral hearing evaluation is the next step in obtaining necessary information from an individual. At the minimum, this should include hearing thresholds, tympanograms, acoustic reflexes, and otoacoustic emissions (OAEs) (ASHA, 2005). The auditory periphery's state of health must be fully examined prior to the central auditory processing evaluation to rule out possible conductive or sensorineural hearing loss. In addition, Berlin (personal communication, April 8, 2008) strongly recommends performing acoustic reflexes in conjunction with OAE's to determine if AN/AD may be present. In addition, Hall reported that approximately 30% of children with (C)APD have abnormal OAEs (Hall, 2006).
(C)AP Test Principles
The ASHA 2005 technical paper lists 13 (C)AP test principles:
- audiologists should have the knowledge, training, and skills necessary to perform the testing
- the test battery should be driven by referring complaint
- audiologists should use "good tests" (i.e., established validity, reliability, and efficiency)
- audiologists should use tests that tax different auditory processes
- audiologists should use tests with verbal and nonverbal stimuli
- testing should be sensitive to attributes of the individual
- normative data should be available
- the audiologist should be aware of influences of age, especially on electrophysiologic tests
- test methods should be like those in the manual/literature
- the patient should be monitored and an appropriate duration of test session should be selected
- other professionals should collaborate with the audiologist
- if another deficit is suspected, the audiologist should refer on
- the (C)AP evaluation should be one part of a multifaceted evaluation and the audiologist should relate the findings to the referring complaint
Clinical Test Tips
ASHA does not explicitly describe how to relate to parents of children undergoing a (C)AP evaluation or how to relate to children in a manner that elicits the best and most reliable results. In order to implement ASHA guidelines, it is important for audiologists to listen to the parents to better understand the referring complaint. In doing so, it would seem to establish a trusting, professional relationship. In addition, setting children at ease (e.g., incorporate children in the testing by having them push a button on the immittance bridge) and encouraging them has seemed to also build trust. Giving children breaks during the approximate hour and a half test session is worthwhile (and implied in the paper). Watching body language, instead of a clock, is a good method to determine when refreshment is needed (e.g., if a child begins moving around in their seat frequently, and looking around the booth, it's probably time for a break).
An important testing tip for audiologists is to be ready to move as fast as the child during the "easy tests" (e.g., ones to which the child responds quickly and correctly). As with other types of audiological procedures, audiologists should be prepared to make decisions quickly (e.g.,alter their testing protocol;choose a different test than originally intended) and to make the time to be accurate in their scoring and interpreting the results.
(C)AP Screeners
The technical paper briefly describes that (C)AP screeners can be used to help identify those individuals at risk for (C)APD. The Differential Screening Test for Processing (DSTP) (Richard & Ferre, 2006) and the SCAN-C Revised (Keith, 2000) are screeners. In addition, the Staggered Spondaic Word (SSW) test, though not a screener per se, has norms for children as young as five years old. There are also checklists, such as the Children's Auditory Performance Scale (CHAPS), that allow an observer (e.g., teacher or parent) to rate children's listening ability compared to their same-aged peers in a variety of settings. Because not every child undergoes screening prior to a (C)AP evaluation, characteristics of "ideal" test candidates have been provided: 1) children aged 7 years, 7 months and older, 2) children with normal cognitive function, 3) children with normal hearing sensitivity, and 4) children with adequate speech and language skills.
Time and Cost Factors
It is also important that clinics realize the large amount of time that the audiologist will need for testing, counseling, report writing, and communicating with other professionals. It would not seem unreasonable for an appointment and the report writing time to exceed four hours. Audiologists should be well aware that (C)AP evaluations are not quick and easy "squeeze-in" procedures. In addition, reimbursement from insurance is variable and might not cover the cost of the testing (ASHA, 2005). Per the working group document, there is little to no third party reimbursement, and enormous amounts of time and energy are needed to establish CAP-specific codes.
The ASHA technical paper categorizes (C)AP tests into seven categories:
auditory discrimination;auditory temporal processing and patterning;
dichotic speech tests;monaural low redundancy speech tests;binaural interaction tests;electroacoustic measures, and electrophysiologic measures. In addition, the technical paper provides examples of tests in each category. These are listed and described in Tables 1, 2 and 3.
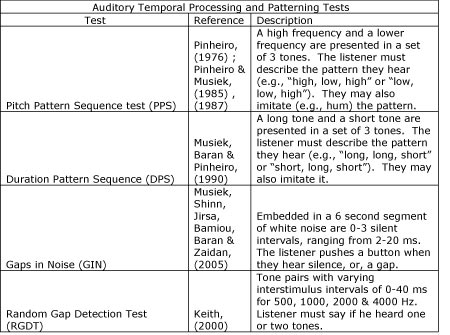
Table 1. Description of Auditory Temporal Processing and Patterning tests included in ASHA (2005).
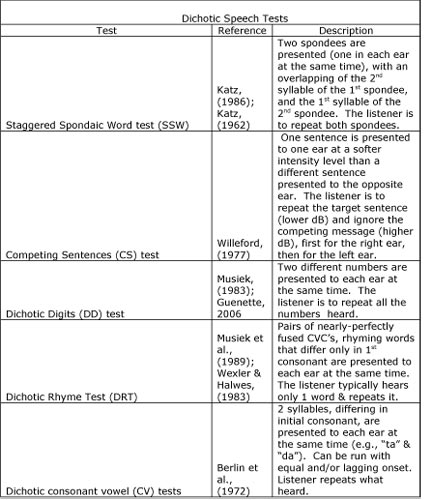
Table 2. Description of Dichotic Speech Tests included in ASHA (2005).
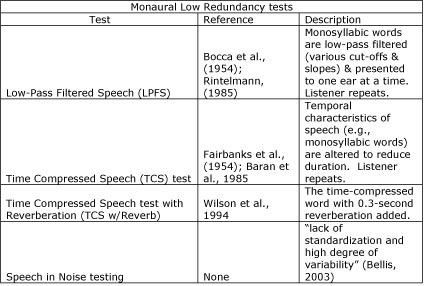
Table 3. Description of Monaural Low Redundancy tests included in ASHA (2005).
Most of the auditory discrimination tests, described by the technical paper as "difference limens", are not performed in an audiologist's test battery;in fact, word recognition scores are not considered true tests of auditory discrimination. An example of a test of binaural interaction is the Masking Level Difference test.
Clinical Test Tips
It may be helpful for audiologists who are first doing behavioral testing, to plan more time initially to physically set up the tests in the CD player and on the audiometer. In addition, the audiologist needs to be listening to the child's responses (and noting them) just as closely as the child is listening to the test items. Having the child face the audiologist can make it easier for the audiologist to hear and see responses and to monitor other behaviors during the test session. Other clinical reminders are to use headphones versus insert earphones to do all the testing, as the (C)AP tests were normed through headphones. In addition, not every single test needs to be performed from each of the test categories (e.g., a clinician may use only two dichotic tests). In addition, when doing the PPS test, reducing the number of items to 15 or 20 is acceptable (Musiek, 2002). Also, initially asking the child to verbalize responses on the PPS test will cut the length of the test in half if the score is within normal limits for the age. There would then be no need to perform the imitative version of the test if the child has already demonstrated the ability to discriminate the patterns in order and with labeling. (Musiek, 2002)
Electroacoustic and Electrophysiologic Tests
Electroacoustic measures include acoustic reflexes, acoustic decay, and OAEs. For electrophysiologic tests, auditory brainstem response (ABR), MLR, frequency following response and cortical potentials such as the P-300 are named. Electrophysiologic tests are important because they provide evidence of CANS function, which is especially useful if no behavioral testing can be performed (e.g., a young child), and they can confirm or clarify behavioral findings (ASHA, 2005). If a neurologic lesion is suspected, electrophysiologic tests are critical. They are also necessary in diagnosing AN/AD (in conjunction with OAE testing). Electrophysiologic testing is further discussed in ASHA's technical paper as a means to obtain data from a child apart from the possible confounding variables of attention and language. In addition, these tests can serve as objective post-therapy data. Jirsa (1992) evaluated a group of children with and without (C)APD on several measures, including P-300s. The children with (C)APD had delayed latencies and reduced P-300 amplitudes. A group of these children underwent therapy, and post-test results of these children revealed improvements in the latency and amplitude of their P-300s. BioMAP is a speech evoked ABR that was developed at Northwestern University (Kraus et al., 2005). The benefits of this test include objective measures to a speech stimulus, ease of administration, and ease of interpretation. BioMAP has been shown to identify neural encoding deficits in children 5-12 years of age, and research has shown that at least 30% of children with language-based learning problems have abnormal BioMAP scores (Kraus et al., 2005). In the future, normative data should be available for children younger than age 5, as well as those over the age of 12 (Kraus, personal communication, April 9, 2008).
The 2005 ASHA technical paper states that there is no gold standard for test interpretation;however, norm-based interpretation (absolute) and patient-based interpretation (relative) can be used to evaluate test results. A combination of these two approaches is intended to assist audiologists in differentially diagnosing (C)APD. Absolute interpretation judges an individual's test scores compared to normal control group scores. Relative interpretation uses intra-test, inter-test, and cross-discipline analysis to judge the individual's performance. In addition, there are at least two models from which an audiologist can draw upon to assist in "profiling the individual" (i.e., relate central auditory function to behavioral symptoms). For example, the Bellis-Ferre model (Bellis & Ferre, 1999) is popular in guiding interpretation and providing deficit specific recommendations. The Bellis-Ferre model uses a combination of absolute and relative interpretation to examine patterns across CAP tests to differentially diagnose the auditory component of suspected processing deficit. It then uses results to discuss/clarify listeners' behaviors. The Buffalo model is also used by many audiologists. Further information about the Buffalo model can be found in "Central Auditory Processing - A Transdisciplinary View" by Katz, Stecker and Henderson (1992).
The following tables depict clinical examples of the three primary (C)APD profiles of the Bellis-Ferre model (Bellis, 2003). The first profile (Table 4) is a 14 year old female with an auditory decoding deficit, which is essentially defined as having difficulties in discriminating speech sounds. She had a history of middle ear problems (no tubes). Her mother thought that she had difficulty hearing and clearly (correctly) hearing what was said, especially when in noise. According to the Bellis-Ferre model, hallmark (C)AP test findings in those with an auditory decoding deficit include poor scores on monaural low-redundancy speech tests. Table 1 shows the below normal scores on the LPFS and borderline scores on the TCS with Reverberation tests. Her low scores on binaural separation/integration tests (CS and SSW) can also be found in those with auditory decoding deficits.
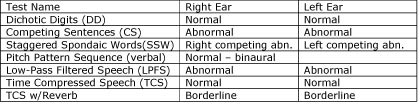
Table 4. Results of a 14-year-old female diagnosed with an auditory decoding deficit.
The second profile (Table 5) is of an integration deficit, which is defined as a deficit in interhemispheric communication. A 12-year-old male presented with a history of problems learning letters and their corresponding sounds and current reading difficulties. Psychoeducational testing indicated auditory weakness. It was also reported that he had difficulty listening in noise and following multi-step directions. The finding of an individual being able to imitate (e.g., hum) a response on patterning tests, but not being able to verbalize the response (e.g., say "high" or "low") is hallmark. In addition, left ear deficits are expected on dichotic tests.
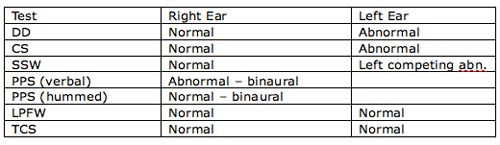
Table 5. Results of a 12-year-old boy diagnosed with an integration deficit.
The last of the three primary (C)APD profiles is the prosodic deficit (Table 6), which is a right hemisphere disorder that greatly impacts a listener's understanding of the intent of the message. Classic (C)AP test findings for a prosodic deficit include poor performance on the imitative and verbal portions of patterning tests and left ear deficits on dichotic tests. The scores of a 13-year-old girl with a history of middle ear, speech-language, and learning problems are listed in Table 3. She had been diagnosed with ADHD and had tried several prescription medications. Psychoeducational testing was performed three times (over six years), with her Perceptual (Performance) IQ score being lower each time. Her Verbal IQ was consistently significantly higher.
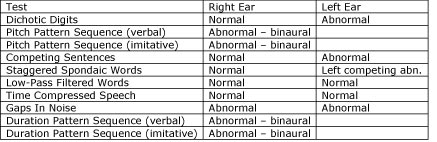
Table 6. Results of a 13-year-old female diagnosed with a prosodic deficit.
There can be some degree of variation in test scores and still fall into one of the previously mentioned categories (auditory decoding, integration and prosodic deficits). Interpretation should be guided by outlined principles, such as those by Bellis and Ferre, or Katz.
Summary
The ASHA Working Group Technical Report on (C)APD provides a considerable amount of information to guide audiologists in what areas further study may be needed, in what comprises an appropriate/ecological test(s), and in what constitutes a CAPD. The audiologist performing CAP evaluations will see children with many different presenting problems and histories. It is important that the audiologist is aware of limitations (e.g., a child with a unilateral hearing loss), as well as possible obstacles (e.g., attention and fatigue), prior to performing the test battery in order to obtain accurate results. Interpretation of results should be guided by references listed in the Technical Report, as well as those found in this paper. In addition, the audiologist should contact other audiologists if they have questions about doing the testing or test results on a certain child, as well as contact those members of a child's multidisciplinary team. Lastly, although not a part of this paper, the Technical Report lists many specific interventions for CAPD. Every audiologist should determine whether or not (C)AP testing is something that can be realistically implemented and maintained at their work setting.
Several literary resources are available for audiologists to increase their knowledge base about (C)APD. The following resources are recommended to not only "bring an audiologist up to speed" on what may, or may not, have been learned in school, but have proven to be invaluable to this author for interpreting test results and providing clear and practical intervention strategies:
- Processing Power (ISBN: 076-1615-80-6) by Jeanane Ferre, Ph.D.
- Assessment of Central Auditory Processing in the Educational Setting - From Science to Practice (ISBN: 0-7693-0130-4) by Teri Bellis, Ph.D.
- volumes I and II of Musiek's and Chermak's Handbook of (Central) Auditory Processing Disorders (ISBN:1-59756-056-1)
- The Pathways column in The Hearing Journal, edited by Frank Musiek, Ph.D
- Texts on electrophysiologic tests are also beneficial. A few recommended titles include either of Hall's books, the most recent being New Handbook of Auditory Evoked Responses, as well as Auditory Evoked Potentials: Basic Principles and Clinical Application (ISBN: 0781757568-9780781757560) by Don, Eggermont & Burkard.
American Speech-Language-Hearing Association. (2005). Technical report: (Central) auditory processing disorders - Working group on auditory processing disorders. Rockville, MD: ASHA.
American Speech-Language-Hearing Association. (1996). Central auditory processing: Current status of research and implications for clinical practice. American Journal of Audiology, 5, 41-54.
Baran, J. A., Verkest, S., Gollegly, K., Kibbe-Michal, K., Rintelmann, W. F., & Musiek, F. E. (1985). Use of compressed speech in the assessment of central nervous system disorder. Journal of the Acoustical Society of America, 78 (Suppl. 1), S41.
Bellis, T. J. (2003). Assessment and management of central auditory processing disorders in the educational setting: From science to practice (2nd Ed.). Canada: Delmar Learning.
Bellis, T. J. & Ferre, J. M. (1999). Multidimensional approach to the differential diagnosis of central auditory processing disorders in children. Journal of the American Academy of Audiology, 10, 319-328.
Berlin, C. I., Lowe-Bell, S. S., Jannetta, P. J. & Kline, D. G. (1972). Central auditory deficits after temporal lobectomy. Archives of Otolaryngology, 96, 4-10.
Bocca, E., Calearo, C. & Cassinari, V. (1954). A new method for testing hearing in temporal lobe tumors. Acta Otolaryngologica (Stockholm), 44, 219-221.
Chermak, G. D., Traynham, W. A., Seikel, J.A., & Musiek, F. E. (1998). Professional education and assessment practices in central auditory processing. Journal of the American Academy of Audiology, 9, 452-465.
Don, M., Eggermont, J. & Burkard, R. (2007). Auditory evoked potentials: Basic principles and clinical application. Philadelphia, PA: Lippincott, Williams & Wilkins.
Emanuel, D. C. (2002). The auditory processing battery: Survey of common practices. Journal of the American Academy of Audiology, 13, 93-117.
Erickson, K. (2008, May 8). CAP testing 101: Recommendations for testing and interpreting, Presented in partnership with ILAA. AudiologyOnline, Recorded Course 11108. Retrieved May 8, 2008 from the e-Learning section on www.audiologyonline.com.
Fairbanks, G., Everitt, W., & Jaeger, R. (1954). Methods for time or frequency compression-expansion of speech. Trans IRE-PGA, AU-2, 7-12.
Ferre, J.M. (1997). Processing power - A guide to (C)APD assessment and management. San Antonio, TX: Communication Skill Builders.
Guenette, L.A. (2006). How to administer the Dichotic Digit Test. The Hearing Journal, 59, 50.
Hall, J. (2006). Electroacoustic and Electrophysiologic Auditory Measures in the Assessment of (Central) Auditory Processing Disorder. In F. Musiek & G. Chermak (Eds.), Handbook of (central) auditory processing disorders, Volume I: Auditory neuroscience and diagnosis (pp. 287-315). San Diego, CA: Plural Publishing.
Hall, J. (2007). New handbook for auditory evoked responses. Allyn & Bacon, Inc.
Jerger, J., & Musiek, F. (2000). Report of the consensus conference on the diagnosis of auditory processing disorders in school-aged children. Journal of the American Academy of Audiology, 11, 467-474.
Jirsa, R. E. (1992). The clinical utility of the P3 AERP in children with auditory processing disorders. Journal of Speech and Hearing Research, 35, 903-912.
Katz, J. (1986). SSW Test User's Manual. Vancouver, WA: Precision Acoustics.
Katz, J. (1962). The use of staggered spondaic words for assessing the integrity of the central auditory system. Journal of Auditory Research, 2, 327-337.
Katz, J., Stecker, N. A., & Henderson, D. (1992). Central auditory processing: A transdisciplinary view. St. Louis, MO: Mosby Year Book.
Keith, R.W. (2000). SCAN-C test for auditory processing disorders in children - revised. San Antonio, TX: Harcourt Assessment, Inc.
Keith, R.W. (2000). Random gap detection test. St. Louis, MO: Auditec.
Kraus, N., Nicol, T., Zecker, S. & Skoe, E. (2005). BioMAP: Biological marker of auditory processing. Retrieved June 1, 2008, from Northwestern University, Auditory Neuroscience Lab Web site: www.communication.northwestern.edu/brainvolts/
Musiek, F. E. (2002). The frequency pattern test: A guide. The Hearing Journal, 55, 58.
Musiek, F.E., & Chermak G.D. (Eds.) (2006). Handbook of (central) auditory processing disorders, Volume I: Auditory neuroscience and diagnosis. San Diego, CA: Plural Publishing.
Musiek, F.E., & Chermak G.D. (Eds.) (2006). Handbook of (central) auditory processing disorders, Volume II: Comprehensive intervention. San Diego, CA: Plural Publishing.
Musiek, F.E., Shinn, J.B., Jirsa, R., Bamiou, D., Baran, J.A. & Zaidan, E. (2005). GIN (Gaps-In-Noise) test performance in subjects with confirmed central auditory nervous system involvement. Ear & Hearing, 29, 608-618.
Musiek, F. E., Baran, J. A., & Pinheiro, M. L. (1990). Duration pattern recognition in normal subjects and in patients with cerebral and cochlear lesions. Audiology, 29, 304-313.
Musiek, F.E. Kurdziel-Schwan, S., Kibbe, K.S., Gollegly, K.M., Baran, J.A., Rintelmann, W. F. (1989). The dichotic rhyme task: Results in split-brain patients. Ear and Hearing, 10, 33-39.
Musiek, F. E., & Pinheiro, M. L. (1987). Frequency patterns in cochlear, brainstem, and cerebral lesions. Audiology, 26, 79-88.
Musiek, F.E. (1983). Assessment of central auditory dysfunction: The Dichotic Digits Test revisited. Ear and Hearing, 4, 79-83.
Pinheiro, M.L. (1976). Auditory pattern perception in patients with right and left hemisphere lesions. Ohio Journal of Speech and Hearing, 2, 9-20.
Pinheiro, M.L. & Musiek, F.E. (1985). Sequencing and temporal ordering in the auditory system. In M. L. Pinheiro & F. E. Musiek (Eds.), Assessment of central auditory dysfunction: Foundations and clinical correlates (pp.219-238). Baltimore: Williams & Wilkins.
Richard, G., & Ferre, J.M. (2006). Differential screening test for processing (DSTP). East Moline, IL: Linguisystems.
Rintelmann, W. F. (1985). Monaural speech tests in the detection of central auditory disorders. In M. L. Pinheiro & F. E. Musiek (Eds.), Assessment of central auditory dysfunction: Foundations and clinical correlates (pp. 173-200). Baltimore: Williams & Wilkins.
Wexler, B. & Halwes, T. (1983). Increasing the power of dichotic methods: The fused rhymed words test. Neuropsychologia, 21, 59-66.
Willeford, J. A. (1977). Assessing central auditory behavior in children: A test battery approach. In Keith, R. (Ed.), Central auditory dysfunction (pp. 43-72). New York: Grune & Stratton.
Wilson, R. H., Preece, J. P., Salamon, D. L., Sperry, J. L., & Bornstein, S. P. (1994). Effects of time compression and time compression plus reverberation on the intelligibility of the Northwestern University Auditory Test No. 6. Journal of the American Academy of Audiology, 5, 269-277.

