Learning Outcomes
After this course, participants will be able to:
- Describe the interwoven factors impacting language, communication, social-emotional, and educational outcomes for students using CI technology.
- Discuss the characteristics of effective educational placements and supports for students with CIs.
- Explain what can be found in various resources to support educational planning for students with CIs.
Introduction
The focus of this course will be on the students who use cochlear implant (CI) technology and not on the technology itself. I have had considerable experience working with children throughout the United States along with their families, educators, and audiologists regarding what occurs after a child receives a CI. I want to help you think about how we can collaboratively work together to plan for the children who use this technology. I have been in the field since 1977, at the Laurent Clerc National Deaf Education Center on Gallaudet University's Campus. We have national demonstration programs that serve children from birth through high school age; the Kendall Demonstration Elementary School and the Model Secondary School for the Deaf. We serve the country and are federally funded. You will hear about some of our other resources throughout this course.
Prevalence of Children with CIs
The most recent information I could locate was back from 2012, stating that 325,000 devices had been implanted worldwide. Of those implants, 58,000 had been implanted in adults and 38,000 in children. However, if you visit the website of one of the manufacturers, they state between 2012 and 2013 alone, approximately 50,000 implants were fit and roughly 30,000 of those were to children. This is to say that the prevalence of children who have implants is inconsistent. We do not know the exact number. As a provider you might see these children in your schools and practices and need to know which resources to utilize and with whom to collaborate. It is important to think about how to plan and share with the families as well.
Changing candidacy requirements. Children are receiving implants at a younger age. The FDA currently recommends the implantation of some devices for children as young as 12 months of age. With the first CIs, children had to have a profound hearing loss to be considered a candidate. Candidacy requirements are expanding, and now we are seeing children receiving CIs who have some functional hearing at the time of implantation. The technology itself and the characteristics of the child are just one part of the journey. I am now going to talk briefly about the other factors that might affect a child with a CI.
Factors Effecting Children with CIs
It is important to think about the many factors that impact language, communication, social, emotional, and educational outcomes for the students using CIs. The key is to identify the characteristics of an effective educational placement and support system. The majority of early evidence focuses on the speech perception and production of the child. Until recently, discussions often overlook the children's educational, learning, thinking, social, and emotional outcomes. Thus, we need to examine all areas of development and not focus on listening and spoken language alone.
Individual Needs
In my experience, "If you've met one student with a CI, then you've met one student with a CI". The overall theme of this course highlights the importance of planning for each student with regard to their individual needs. During the planning process, it is critical not to assume every student with a CI can understand what is being taught in the classroom. Consider who are the students that you might be serving. It is not a one size fits all approach because you will need to factor in the child's individual needs as shown in Figure 1.
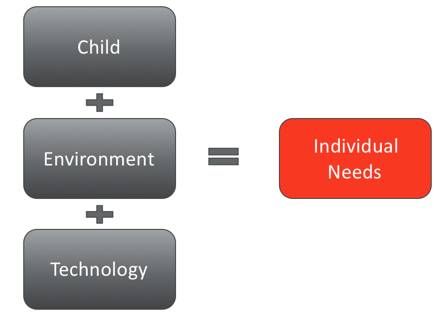
Figure 1. Individual Needs.
Child
When planning for a child with a CI you should consider the child's age at implantation. You might have a young child who received their CI at the youngest FDA recommendation (i.e., 12 months of age) or even younger. Maybe you have a student who received their CI when they were older and already had developed spoken language. Perhaps you are going to be serving a student who received their CI when they have additional learning challenges. Another scenario might be a student who obtained their CI young and developed a learning disability that you might not have been aware of. We need to be cognizant of all possible scenarios when we meet a child with a CI. Also, we need to recognize the various hearing loss configurations prior to receiving an implant and varied types of CIs now used with children (i.e., hybrid CIs). The outcomes for these children will be different.
Environment
Some children have been placed in programs where they are solely using spoken language. Perhaps some have been using sign language prior to receiving an implant and as they transition, some may continue to use sign language. There will be children using both American Sign Language and spoken language from the start and continue to use both post-implantation. The audiologist should consider the educational and linguistic environment the child is in. If a child has a secondary language in the home, what are the recommendations and expected outcomes?
Technology and Equipment
Lastly, we need to consider what type of CI was implanted and under what circumstances. One might ask, were there any surgical complications? We need to look at the history to see if the electrodes were inserted completely. Most importantly for audiologists, we want to ensure that the CIs are maintained after the surgery so the child may be successful post-implantation. Many families are not given clear information regarding the process, and it is important that we discuss what is involved after the CI surgery (i.e., frequency of follow-up visits, the proximity of programming centers). Additionally, we need to identify support in the child's school system. We need to determine if there is someone in the school that is checking the student's equipment and has extra parts on hand in the event the educational audiologist is not available.
Spoken Language Abilities
Listening and spoken language skills require time to develop. Certain students who are receiving CIs have excellent social language. They can communicate with you and have a social banter, but often struggle when it comes to academic learning. As language becomes more complex, they are not always able to communicate and use their listening skills at the same level as other students to learn. Looking at the language outcomes for children with CIs is critical to their development.
American Sign Language
We have been exploring the role of American Sign Language (ASL) and using other visual supports for children using CI technology. These children are still deaf or hard of hearing when they are not wearing their equipment. In certain cases, children might not use listening as their primary method for learning. A common myth is if the child continues to sign, that the child will not learn spoken language. The evidence does not support this. If you are using ASL or sign as support to spoken English, you must also have the supports in place to develop listening and spoken language. If the child uses sign exclusively, the spoken language will not have the opportunity to develop.
Difference between sign and ASL. In your work, it is important to understand the difference between sign and ASL. When you are discussing signing, be careful to distinguish sign to support spoken English or ASL. ASL is a full visual language with its own grammar and syntax. ASL cannot be coupled with spoken English. When working with families it is critical they understand the difference as well. Evidence shows that whether it is sign as support to spoken English, or ASL early in a child's development, children can transition to spoken language when the appropriate supports are in place (Nussbaum, Waddy-Smith & Doyle, 2012). In fact, the symbolic use of sign can aid in the development of spoken language. A great example is when culturally deaf families chose a CI for their child. The child has a strong language based in ASL, but once given the supports in spoken English they transition and develop spoken skills. It is important to keep in mind that not all children will or have the capability to transition to spoken language, which is why individual planning is important for these children.
Communication Continuums
Receptive communication continuum. If you have a child who is a visual learner or mostly visual with the auditory understanding they will fall on the receptive end of the continuum. These children learn best through audition with some visual support (i.e., sign language, cued speech). Understanding how students function on this receptive communication continuum allows everyone involved to have a common understanding of the child's communication style. This continuum is helpful when describing the students’ abilities and future goal planning. Goals need to be aligned with the capabilities of the child and individualized.
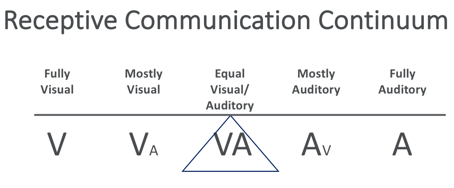
Figure 2. Receptive Communication Continuum.
Expressive communication continuum. It is also important to evaluate the child’s functioning on an expressive continuum. This continuum examines how a child is communicating (i.e., sign, oral, the combination of sign and oral).
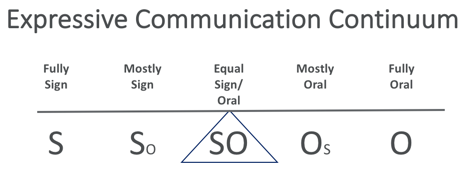
Figure 3. Expressive Communication Continuum
Importance of pragmatic language. With the use of CI technology, a child can develop listening and spoken language. However, social language development is equally important (i.e., understanding idioms, social vocabulary, figurative language, turn-taking). We need to focus as much on pragmatic language skills as we do on receptive and expressive spoken language development once the child is implanted.
Language Plateau
Language abilities of children may plateau over time. When children are young they can test at an age-appropriate level because language is simple and not complex. As students advance in school, the language becomes more complex and abstract. We need to plan for this plateau and realize that some of the language structures that are more complex might not be picked up incidentally. The school program should focus on training the child in these skills that will aid in their academic and social interactions. "Beyond Early Intervention: Supporting Children with CIs Through Elementary School" highlights the concept of language abilities plateauing in the middle of elementary years. Much of the early research and attention has been focused on initial phases post-CI implantation, but we really need to think about the child and their social and emotional development.
Collaborative Planning
Students With Cochlear Implants: Guidelines For Educational Program Planning is a resource developed by Boston Children's Hospital and the Clerc Center by approximately 40 professionals from various disciplines, educational backgrounds, and philosophies related to working with children wearing CIs. These guidelines are universal because they can be utilized by any professional and can be implemented in any setting (e.g., general education, school for the deaf, early intervention program). Coordination is key. A guidelines coordinator should be tasked at collecting all of the information from various professionals and family members, so a collaborative discussion can occur regarding each child.
Student Background Summary
Summarizing a student's background is the first step in educational planning for the child. The summary is a place to document the student's background (i.e., age of implantation, manufacturer, consistent use of device). The guidelines also provide three different competency checklists which document the child's language skills; one for receptive, expressive, and pragmatic language skills. Once all of the information is collected it is recommended that a guidelines coordinator create a summary of the student.
School-Based Language Competency Checklists
The checklists are useful because they give you an opportunity to look at a child's language competencies. The checklist is a place to document how the child is using ASL, spoken English or spoken English with sign as a support. If there is another support that the child might be using such as, cued speech or other augmentative communication you can list those in the checklist as well. Make note of what environment (e.g., home, cafeteria, classroom) the child is in. Thus, you can summarize how they are using their communication skills in various environments.
Team Discussion Tool and Team Summary Sheet
Here, each professional's perception and perspective are included and collective recommendations are made. Secondly, if the program is not supporting the student, what modifications can be made to this educational environment to provide the supports that are recommended? Third, If the recommended accommodations cannot be achieved should another placement be considered? The tool lists four areas to consider:
- Language and communication
- Staff and Training
- Equipment and Technology
- Other Integral Considerations
Language and Communication
Guidelines look at such things as:
- Does the educational setting provide accessible language for the development of academic achievement?
- Does the program provide direct instruction to the student?
- Does the program provide habilitation services to facilitate listening and spoken language skill development as recommended on a student’s IFSP/IEP/504 Plan?
- Does the program provide other recommended support to facilitate a student's access to the curriculum as determined by the IFSP/IEP/504 plan?
This guideline examines whether the educational setting provides accessible language for the development of academic achievement. Can the student learn through spoken language? In general education settings, the assumption is that if the child has their CI on then they should be understanding. Teachers who are not familiar with CIs may assume that the classroom is accessible since the child is wearing their equipment. This section of the guidelines also encourages discussion about what accommodations should be made to support language and communication (e.g., interpreter, cued speech translator). Without planning, the assumption may be made that when a child is not understanding spoken language that it is time to add a sign language interpreter into the classroom. However, we have unfortunately seen this recommendation when the child did not even know sign language. That is why planning is so important. Also, this is a time to discuss additional services needed to facilitate listening and spoken language skills as recommended in a child’s FSP/IEP/504 Plan. It is also a time to discuss if the program does or could provide other supports to language access such as real-time captioning. Oftentimes, general education teachers do not know where to obtain these services. As an audiologist, you may be the individual to coordinate services to support the student to abide by their IEP Plan.
Staff Training
The section on Staff Training addresses such questions as:
- Are the services of an educational audiologist available to oversee and monitor a student’s cochlear implant?
- Are supports from other specialists experienced in working with students who use cochlear implants available as recommended in a student’s IFSP/IEP/504 plan?
- When listening and spoken language skill development services are recommended, does the service provider have training and experience working with students who have CIs?
- Are teachers and staff members trained in understanding the needs of students with cochlear implants and implementing recommended accommodations and strategies?
- Is there consistent collaboration among professionals involved with the student?
This leads to the discussion on the importance of making sure the staff working with the students have the knowledge and skills to support them. For students who are in the general education setting, you may be the person called in to assist, monitor, and train other professionals regarding the CI. If you are working in a hospital or clinic, identify if an educational audiologist is in their school so that they can ensure the CI is functioning and has the parts in place every day. Perhaps as a related service provider, you could be working with the schools in planning an orientation. It is crucial to work with the family to help the teachers and staff understand the educational needs of a student with a CI. If there are multiple providers, ensure there is consistent collaboration so that you can make sure that you are collaboratively planning.
Equipment and Technology
Address questions such as:
- Is the acoustic environment appropriate for a student with a cochlear implant? (Refer to accommodations appendix)
- Are there appropriate hearing assistive technology systems (HATS) available and supported?
- Are there staff members identified, trained, and responsible for daily troubleshooting of the cochlear implant and associated HATS to confirm their proper functioning?
- Is there a mechanism for ongoing home-school collaboration related to the cochlear implant?
Other Integral Considerations
Lastly, there are other considerations related to social-emotional development that are provided. Questions such as the following are addressed:
- Does the program provide an appropriate peer group and opportunities for social interactions?
- Does the program have a mechanism in place to help the student build a positive self-image as a child who is deaf?
- Does the program facilitate student and/or family advocacy skills related to the use of a cochlear implant?
- Does the program facilitate student/family skills in an effort to build self-advocacy independence?
It is important to have discussions about topics which address whether the program provides appropriate peers for the child, which is closely tied to self-esteem. This section looks at making sure the child feels comfortable about who they are as a deaf child using a CI. What can the program do to support self-advocacy strategies? Many times, the students themselves have to learn how to develop their independence in knowing when their CI is working and telling someone when it is not working. They need to feel confident and competent in doing so.
Additional Resources
There are a few other resources I would like to bring to your attention:
- Education Planning for Students with CIs
- A Guide for Interpreters Working with Students Who Use CIs.
- Visual Language and Visual Learning (VL2).
- eBulletins: CIs: Considerations for Families (and the Professionals Who Work Alongside of Them) and CIs: Making Sure Families Are Aware of The Full Picture
- Bookmarks
Another resource that I would like to mention is a research brief developed for VL2. The Visual Language and Visual Learning center is located at Gallaudet University. They have a series of research briefs on different topics related to raising and educating deaf and hard of hearing children. This one in particular: The Implications of Bilingual Bimodal Approaches for Children with Cochlear Implants focuses on the implications of a bimodal and bilingual approach for children with CIs. I bring this up because in the field of audiology, the majority of audiologists when they hear 'bimodal,' they may think of a hearing aid in one ear and a CI in the other ear. In this instance, bimodal represents the terms of the modalities used for language (i.e., visual, auditory). Not modality of technology. It is the implications of using both listening and spoken language as well as ASL and what role each can play in education. In language acquisition and learning for children with CIs this can be crucial.
What I wanted to mention about the eBulletins is they are brief. One eBulletin ensures families are aware of the full picture. There is much to think about in terms of what their role is as a family in supporting not only their spoken language development, but their overall linguistic and social emotional development. The other e-bulletin looks at planning, similar to what we discussed here today. Again, both of those documents are on the website for Raising and Educating Deaf Children: Foundations for Policy Practice and Outcomes. The website also includes other helpful resources.
The Bookmarks mentioned are available through the Clerc Center created for educators who are new to educating deaf and hard of hearing students. They are nice to share with teachers in general education settings who are working with all deaf or hard of hearing student, including those with cochlear implants. This could be something you can give to teachers that talk about basic considerations about the IEP, individual needs of the student, and socio-emotional needs.
Summary
The areas discussed today are part of the guidelines to help any professional go through a step by step discussion of the individual child. A summary sheet provides a place to compile all that was discussed and planned for recommendations. Keep in mind that this document may drive the decision to change IEP goals or educational placements if needed. In the appendices of the guidelines is a wealth of information about accommodations that can be made to enhance the auditory environment. This section provides information about acoustics and troubleshooting the technology. Visual accommodations provide information related to areas such as the lighting in the room and seating sight lines. Accommodations for educational access, provides information about making sure you are conducting annual in-service training. The appendix on technology provides helpful information about performing a physical and functional check of the technology every day. All of these steps will ensure the children who wear CIs can maximize their potential with the technology. Again, I want to highlight that The Clerc Center is federally funded and our resources are free. We hope you find them helpful in educational planning for children with CIs.
References
Bavelier, D., Newport, E., & Supalla, T. (2012). Educational planning for students with cochlear implants. Nature Reviews Neuroscience, 5, 831-843.
Med El: cohclear implant facts (2013, September). Retrieved from https://www.medel.com/cochlear-implants-facts/
Nittrouer, S. (2016). Beyond early intervention: supporting children with CIs through elementary school. Otology & Neurotology, 37(2), e43.
Nussbaum, D., Scott, S., Waddy-Smith, B., & Koch, M. (June 2004). Spoken language and sign: Optimizing learning for children with CIs. Paper presented at Laurent Clerc National Deaf Education Center, Washington, DC.
Nussbaum, D., Waddy-Smith, B., & Doyle, J. (2012). Students who are deaf and hard of hearing and use sign language: considerations and strategies for developing spoken language and literacy skills. Seminars in Speech and Language, 33(4), 310-321.
Citation
Nussbaum, D. (2018, March). Cochlear implants: educational planning for school-age children. AudiologyOnline, Article 22411. Retrieved from https://www.audiologyonline.com


