Discussions among audiologists on how to best work with adults with hearing loss usually revolve around pathological or technical issues;for example, how to better understand the physiological aspects of hearing, how to make an accurate diagnosis, or how to optimize the benefits of technology to maximize residual hearing. Although these aspects of audiologic rehabilitation are vitally important, it is additionally helpful to evaluate the impact of interpersonal communication behavior upon communication function and social integration. Communication behavior refers to individual communicative actions that may vary from time to time. Communication function refers to the overall purpose of the collective communication behaviors - namely, social integration.
The simple reason for this additional focus is that communication behavior, whether we hear well or not, has a much more decisive influence upon success or failure in social integration than the simple ability to hear. After all, how we respond to what we hear or perceive is usually the only criteria our communication partners can use to determine how to interact with us. Therefore, an examination of the impact of communication behavior on communication function may be more enlightening as a framework for developing an audiological rehabilitation program than a clinical perspective that considers only pathological or psychological causes of the disabling impact of hearing loss on social integration.
Hearing loss is common, and regardless of the causative factors involved, there are communication behaviors that typically result from it. The inability to hear a conversation clearly as a result of a hearing loss is not much different from being able to hear a conversation but not understand it as a result of a language barrier, as in the case of a non-English speaking immigrant. Neither should be regarded as a psychological or psychosocial disorder. It is helpful to the task of rebuilding a client's communicative confidence to investigate whether the client is using any communication behaviors that could create barriers to successful social integration within his or her culture. This additional clinical focus does not mean that a clinician should deny psychosocial issues caused by hearing loss. It simply suggests that the best foundation for hearing rehabilitation planning is to focus on helping clients restore balance to their communication function.
Two Components of Communication Function
Normal acts of communication involve two components, reception and expression. We receive information about environmental sounds and interpersonal communication through our ears and eyes, and we respond to these stimuli. These responses express our feelings and thoughts and convey messages to others. The resulting interactions determine our effectiveness in interpersonal engagement and social survival. Any impedance to the frequency, quantity, or quality of communication can have a significant impact on the quality and stability of social integration and, if left untreated long enough, a negative impact on mental health. It does not matter whether the impedance is a hearing loss, speech impediment, language barrier, anti-social behavior, or a destructive communication tactic, the result will be the same—a negative impact on the ability to engage productively and in healthful ways with other people.
Communication behaviors are culturally derived;they are learned from family and social environments. Hearing is a key determinate of communication behavior as information must first be received accurately in order to learn to respond accurately. Impaired hearing, especially if it is severe and affects the formative years, may impede the ability to adopt expressive communication behavior norms. This interference can be better understood by considering fundamental *attributes of normal communication behavior and how hearing loss can affect those attributes.
The Communication Diet Model
Communication is often called "food for the mind" and is just as necessary to mental health as food is to physical health, so taking a closer look at what happens to the human body when it is deprived of food, can help us to understand what happens to the mind when it is deprived of some of the essential "nutrients" of normal, unhindered communication.
If we neglect to eat an adequate quantity of nutritious food regularly, our bodies become sick unless a correct balance of the essential elements is restored. This is an absolute rule that cannot be ignored without an eventual impact on physical survival. For example, if a person eats regularly, but eats too little or too much, even if their meals are nutritionally well balanced, excessive weight loss or weight gain will result. If a person eats regular, good-sized meals, but eats only junk food devoid of nutritional value, illness will occur. Likewise, a negative effect will happen if a person eats well-balanced, good-sized meals, but skews the frequency by eating too often or too infrequently. Logically then, it should be a reasonable hypothesis that failure to "feed" the mind with an adequate amount of "nutritious" communication at regular intervals, or merely skewing any of the three elements, (regularity, quantity or quality) to one extreme or the other, could trigger the various psychosocial symptoms associated with hearing loss such as loneliness, depression, anxiety, and withdrawal. 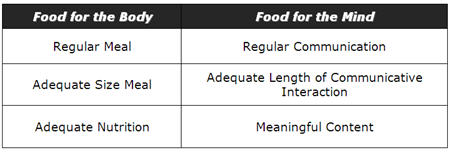
Table 1. Comparisons of three essential elements common to a food diet and to a
communication diet
A communication diet can be just as easily unbalanced as a food diet. Fleeting, irregular communication without meaningful content will upset and likely destroy a relationship if it goes on too long. (As will be discussed later in this article, the likelihood of this occurring for someone with a severe hearing loss is much higher than for someone with normal hearing.) We can expect that symptoms of an impoverished communication diet within a relationship will begin to emerge even if just one of the three essential elements (frequency, quantity, or quality) are depleted for an unacceptable length of time. Consider the example shown in Table 2.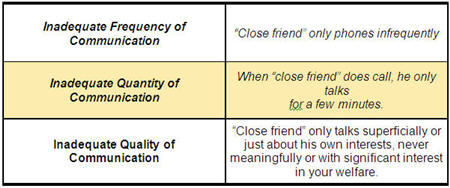
Click Here to View Larger Version of Table 2 (PDF)
Table 2. Example of an undernourished communication diet between two friends.
Anyone who has ever been on the receiving end of this kind of communication behavior knows it usually spells disaster for that relationship and if practiced widely, will probably result in poor social integration for the person doing it. This is true with or without hearing loss. It is a major point of this article that someone with a severe hearing loss is much more likely to be on the receiving end of such destructive communicative behavior simply because it can be too difficult for others to communicate meaningfully without the need for repetition and increased loudness levels. To avoid such stressors when communicating with someone with a severe hearing loss, many people will revert to basic information sharing. The resulting communication deprivation for the person with the hearing loss becomes particularly evident when we consider the element of "nutrition" in the communication diet.
Reviewing our food analogy, a nutritional disorder may result from an imbalance of three basic elements in a diet - frequency of meals, quantity of food, and nutrition. (regularity, quantity and quality) In the case of a nutrition deficiency, remedial action must be taken to restore these three elements back into proper balance. To remedy the situation a dietician may perform two tasks: (1) Do an analysis of the client's food and nutrition intake over time and (2) Make a recommendation for changes in eating habits that will restore nutritional balance to the diet.
This level of detailed analysis and remediation if applied to communication behavior, would be of enormous value to hearing rehabilitation science. Especially if we could numerically define the "nutritional values" of various common words and phrases used in normal relationship development and maintenance among non-hearing-impaired people and contrast this with those used by people with severe hearing impairment, who have identified themselves as experiencing social integration and relationship maintenance difficulties. The resulting research based information could be useful for the construction of analytical and remedial tools to identify and help repair any expressive communication behaviors that might be hindering a client's social integration.
Table 3 attempts to describe three possible levels of communicative nutrition. 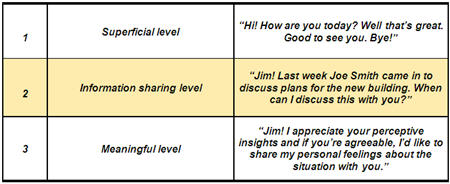
Click Here to View Larger Version of Table 3 (PDF)
Table 3. Three possible levels of communicative "nutrition"
The third level contains the most communicative nutrition. Only on this level is it possible to express the deepest emotions and obtain the reinforcement and motivation necessary to determine attitudes and feelings in relationships. Indeed, relationships cannot proceed to develop beyond a superficial or information sharing level into long-term, closely bonded partnerships unless all parties regularly engage in significant quantities of meaningful ("nutritious") communication. Jill Lindley (2009), whose husband has a profound hearing loss, reports that feeling a lack of intimacy and spontaneity in relationships are commonly experienced by the significant others of people with profound hearing loss due to difficulties with communication. Failure to continuously feed a relationship with meaningful communication may ultimately result in failure of that relationship. This will be preceded, as in the case of an impoverished food diet, by symptoms of communication starvation. The partner who feels starved or neglected may seek meaningful, nutritious communication in other relationships.
For a relationship to develop from the superficial level to the meaningful level, all parties must continuously demonstrate appropriate listening and responding skills. Typically, a relationship will start at the first level and proceed smoothly to the third level before matters of deep personal importance and sensitivity are openly discussed. If either party makes an unacceptable number of inappropriate responses at any level, the communicative relationship will stagnate or start to break down. Inappropriate responses can take many forms;they can be verbal or non-verbal, and conscious or unconscious. Examples of responses that impede communication may include failure to display interest by not paying attention;bluffing;making comments unrelated to the speakers' statements;interjecting out-of-turn;and defensive, rude or violent language.
These types of responses send out contradictory or negative messages that if repeatedly exhibited, will prevent development to a higher or more personal level where the greatest communication nutrition and resultant relationship bonding occurs. Because communication skill and tolerance varies with each individual, impoverished communication has a different effect on each person. Some people may tolerate an impoverished communicative relationship for years without complaint, whereas others may separate when a relationship does not move beyond the superficial or information exchange levels. Indeed, experts indicate that poor communication is most often the catalyst for all other marital problems, and the main reason for divorce (American Academy of Matrimonial Lawyers, 2009).
Implications for People With Severe Hearing Loss
People with hearing loss are equally responsible for these principles of communication as anyone else. Fortunately, for most clients, current technology is good at providing amplification so that many hindrances to communicative reception are removed. Even with latest and most effectively fitted amplification technology, the restoration of hearing reception does not guarantee the restoration of expressive communication skills. Technological solutions to hearing loss focus only on the reception element of the communication paradigm. This one-sided focus completely ignores the impact on the expression element. In cases when the loss is so severe that a residual hearing disorder still remains even with appropriately-fitted technology, the communication deprivation is only partially alleviated by amplification, and the client will be more likely to repeatedly make inappropriate responses.
For people with severe and profound hearing loss, problems with expressive communication may result from hearing difficulty, or because they have not learned to develop effective compensatory expressive communication skills. Consequently, it can be much more difficult to maintain a healthy communication diet with their workmates, peers and families. This is particularly true if their communication partners exhibit a low tolerance for the hearing loss or do not practice effective communication strategies (e.g., speaks from another room or at a distance, speaks with their head turned away from listener, failure to repeat/rephrase when a breakdown occurs, etc). Our clients face the need to take responsibility, not only to obtain and use the best amplification technology they can afford, but also to learn how to develop optimal expressive communication strategies that will improve their chances of successful integration into their individual communicative environments. Failure to achieve these two critical goals may result in workplace and family relationships inevitably becoming strained, sometimes to a breaking point with painful consequences for everyone involved. This is where the inadequacies of our current audiological toolkits become most painfully evident.
It therefore remains vital to include as part of the initial pre-fitting hearing assessment, an evaluation of the expressive communicative behaviors the client may be using. Then measure these again during post fitting follow-up to determine if amplification affected any changes. If there are no measurable improvements in communication involvement / social integration, then this should trigger a remedial plan aimed at restoring a healthy balance to the client's communication diet. In developing this plan, because the focus will be on expressive rather than receptive communication, remedial strategies will more likely focus on speaking tactics rather than hearing tactics. Of course, this does not ignore the need to optimize effective listening skills. Expressive communication behavior training will simply be an addition to the rehabilitation plan that has largely been overlooked until now in hearing rehabilitation.
Teaching Strategies
Teaching expressive communication strategies is similar to teaching receptive communication strategies, with the focus shifted from listening skills to speaking skills. Unfortunately, professional tools for teaching expressive communication strategies are scarce, and professionals may thus need to create their own resources in this area. The teaching method can be as simple as suggesting and demonstrating alternative approaches during individual counseling sessions, as a clinician normally does when teaching auditory training or listening skills.
There are many texts and resources on aural rehabilitation, but only a select few contain tools and strategies for dealing with the impact of hearing loss on expressive communication skills. Table 4 contains a list of resources in this area. These are tools that I have found helpful in my experience;this is by no means an exhaustive list. Further resources from Dr. Norman Erber, who is well published in this area, can be found at his Web site, www.hearingvision.com.
Practical tools and games designed to help people without hearing impairment to hone their speaking and communication skills are already available on the Internet (e.g., www.conversationmatters.com) and may be useful as a starting point for designing appropriate intervention tools and techniques for helping people with hearing impairment. However, the concept offers a ripe field for research and development of new resources.
The expressive communication skills aspect of the human side of hearing loss in adults has not been studied extensively, and may inspire audiology students, researchers and other professionals interested in rehabilitation to develop new resources and information for use in clinical audiology settings. Other professional fields dealing with human interaction, such as didactic analysis, may also offer potential for the development of new clinical tools that help clients with hearing impairment improve their communication diet.
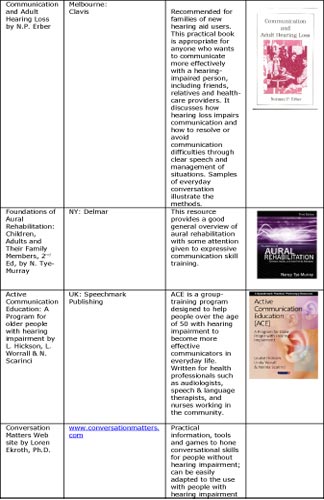
Click Here to View Larger Version of Table 4 (PDF)
Table 4. Expressive communication skills resources
Learning by Example - The Power of Real-Life Experiences
Case Study 1 - Youth Group
Group practical experiences in real-life situations outside the classroom can corroborate classroom learning. Sometimes the best way to address sensitive issues such as expressive communication behaviors is by creating experiential situations that teach by example. Peers learn by observing and emulating others from their group;therefore, the effectiveness of behavioral modeling approaches towards teaching effective expressive communication skills is evident.
As an anecdotal example, some years ago I was a leader in a social group for young people with severe hearing impairment. We had regular meetings mainly focused on organizing a social agenda and how we could best find and help other young, hearing-impaired people. Like other clubs or common interest groups, the chance to communicate with peers was highly valued and our meetings were usually well attended.
During an outing on a hot day, several members of the group decided to buy some take-out food for lunch. On entering the store, all except one girl lined up in the queue to order. This girl did not want to order for herself;rather, she tried to get other members of the group to place her lunch order. The others, aware of the need to help one another develop social confidence, gently encouraged her to watch carefully and copy how the others placed their orders. Encouraged by this, she finally made an effort and succeeded in getting her food without fumbling her order or embarrassing herself with what she felt were faulty expressive communication skills. After several similar experiences during a number of group outings, her expressive communication skills gradually improved to the point where she could deal with many difficult listening situations comfortably in spite of her profound loss. The catalyst for change for this young woman's expressive communication skills was the understanding and encouragement she received from her severely hearing-impaired peers in real-life, difficult listening situations.
These group experiences, amazingly, never included a formal training agenda or qualified instructors. Although there was an acknowledgement of hearing loss and its problems, this was not the main focus as we were simply trying to have a good time among supportive friends. We all wanted acceptance and involvement in a normal social life in spite of our hearing difficulties and sometimes inept expressive communication skills. Group members often exhibited extreme verbal or non-verbal reactions, such as loud, hysterical laughter to statements or events where a more subdued reaction would be deemed appropriate. If this happened at a social outing, it would inevitably draw stares, amused looks, or frowns from bystanders. Some in the group were unaware about the impact of their behavior;however, others keenly felt a sense of social rejection and thereafter tended to avoid outings unless they knew that the more socially inept members would not be there. At the time, the inept social behaviors from the more severely-impaired members of our group puzzled me. Many years later , after completing my master's degree at Gallaudet, I realized that the group experience provided an environment where we could feel uninhibited and unhindered by communicative barriers. This allowed us to fully participate in third level conversations with minimal fear of social rejection. In such an unrestricted environment, behavioral extremes were more evident.
Looking back on those enjoyable experiences, the expressive communication behaviors were fascinating to watch. One notable observation was that barriers that are frequently cited as hindrances to communication with normal hearing people, such as high levels of background noise, ceased to be barriers in our often noisy social gatherings. Those who found it difficult to communicate among normal hearing peers in similar situations suddenly seemed to have little difficulty expressing themselves with one another in noise. We were not users of sign language, so what was happening to demolish those typically insurmountable barriers to communication? I believe that our ability to communicate in these situations was a reflection of the impact of the group activities on our communication diets.
One of the biggest attractions to involvement in the social group was the abundance of third level, meaningful communication that took place. For many of us, a significant portion of our communication with normal hearing family and work colleagues was often first or second level communication, with very little opportunity to engage in meaningful third level conversation on a regular basis. One member of our group worked as a medical orderly in a large repatriation hospital. This profoundly hearing impaired man was constantly under a great deal of stress caused by his hearing difficulties and a largely unsympathetic attitude from his work colleagues. In the unfriendly workplace, his communication diet was superficial at best, and by his own admission, the chain reaction of stress negatively impacted his social and family relationships for many years. Most other members of the group also suffered from similar communication deprivation. Therefore, when we were together, the hunger for third level communication was so great that typically impenetrable barriers to (e.g. high levels of background noise) had no affect on us. From personal experience, I can best describe this as a reaction to communicative starvation, and starving people can be expected to do desperate things for nourishment.
Case Study 2 - Rocky Stone
Another example of the effectiveness of unconscious modeling of expressive communicative behavior by a severely hearing impaired person is illustrated in a story about Rocky Stone, the founder of S.H.H.H. (Self Help For Hard of Hearing People). A few years ago, I attended an anniversary gathering of S.H.H.H. where Rocky Stone was the keynote speaker. After Rocky delivered his speech, I observed him as he worked his way around the large and noisy group of attendees. Knowing just how severely hearing impaired Rocky was, and how little information he received from his hearing aids, I was amazed at how successfully he managed to integrate into each group, then extricate himself smoothly so he could move on to the next group. His chief strategy seemed to be the art of what I call "confirmatory questioning." He would open with a question related to his speech or a few words he thought he had picked up as he entered the discussion. This piece of guesswork would provide a degree of predictability in the responses he would likely receive and some control of the conversation flow. He would then make a concluding remark and move to the next group where he would repeat the same procedure. In the light of the Communication Diet theory, I concluded that Rocky learned how to make the best use of superficial information in this instance to not only survive in a group, but to thrive. No one could exist for long on such a superficial communication diet;however, his example illustrates that it is possible to utilize even superficial information to maintain social integration in difficult listening environments.
Rocky's adaptive skills are an excellent example of how modified expressive communication strategies can be powerful tools in hearing rehabilitation, in spite of severe auditory impairment. Rocky has always been a role model for me as I develop a set of coping strategies for my own profound hearing loss and was the inspiration for an earlier statement in this article, "Communication function is a much more important determinate of success in social integration than simple ability to hear." In other words, how we respond to what we hear or perceive has a far more significant impact on our success or failure in social integration than how much auditory information we actually hear.
Identifying Destructive Communication Behaviors
Fortunately, for many mild to moderate losses, technology solutions alone do a good job of providing adequate levels of receptive capacity for communication, and the negative impact on expressive communication behaviors may be minimal. With post-lingual severe or profound hearing losses, technology solutions usually leave a residual level of impairment and hence difficulty with expressive communication is common. However, regardless of the loss, objective verification of communication behaviors is necessary and cannot be assumed from an audiological evaluation. The presence of an impoverished communication diet will not always be evident without targeted questioning. Learning to live with communication problems is not an option for most clients, especially if they are given no direction or advice on exactly how to live with them.
Table 5 lists five typical questions and a follow-up ranking scale that can be administered pre- and post-fitting in order to identify a client's potentially destructive expressive communication behaviors as part of an effective hearing rehabilitation plan. Targeted questions like these can be easily incorporated into an initial assessment questionnaire and completed by the client in the waiting room. The clinician can then review the answers at follow up appointments to monitor targeted communication behaviors. Little or no change in negative behaviors identifies a need to train expressive communication skills in these areas. Such a carefully targeted, measurable, and individualized approach will likely be more effective than involving the client in broadly-focused (individual or group) counselling sessions on hearing strategies that may provide generic information without meeting the client's specific needs. However, if specialized professional assistance is not available, a self-help group such as S.H.H.H. may be the best resource. Often, even if they do not conduct individual or group courses in effective communication, members of these organizations can serve as role models of appropriate communicative behaviors, helping clients develop effective adaptive strategies. Learning can occur in a social, non-threatening environment, with peers who understand and accommodate the client's communicative needs. Association with effective and understanding role models can sometimes be all that is needed to achieve a satisfactory transfer of skills. 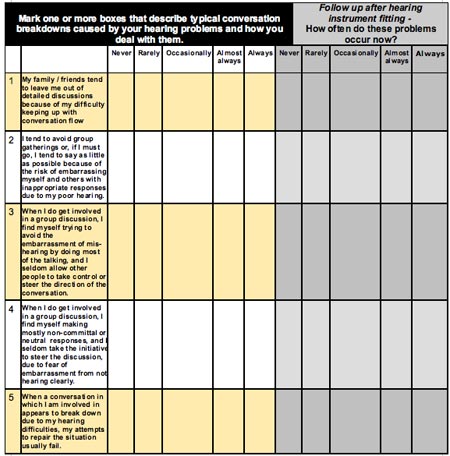
Click Here to View Larger Version of Table 5 (PDF)
Table 5. Suggested questionnaire design for identifying potentially destructive, expressive communication behaviors. Question 1 targets the degree of social isolation experienced;Question 2 targets the extent of passive communicative behaviors;Question 3 targets the extent of aggressive communicative behaviors;Question 4 targets the extent of neutral or non-committal behaviors and Question 5 targets the degree of success with present conversational repair strategies. Monitoring a change in response (improvement or worsening) for each of the five scenarios identifies the specific type of unhelpful communication behavior to be targeted by communication skills training.
Summary
Hearing rehabilitation is more than the restoration of hearing. It is about the restoration of communication function. Communication function involves both receiving information as well as expressing information. In addition to providing an awareness of our environment, hearing enables us to obtain the information needed to express ourselves with a reasonable degree of confidence and relevance. Anything that impedes communication - whether it is a speech disorder, the inability to speak the language of one's community, or a hearing loss - will affect our ability to feel integrated within our community. Nowhere is the damage to communication function more evident than in clients with post-lingual (beyond the formative years) severe to profound hearing loss. Their needs can painfully emphasize the limitations of our professional tools and skill sets.
The majority of audiology research and rehabilitation product development addresses only the first part of the communication paradigm, reception. Much more research and product development can and should be done on helping our clients repair the damage defective hearing has done to their expressive communication abilities. The traditional view of approaching the problem of hearing loss from a pathological or technological perspective needs to be supplemented with an examination of the culturally-learned communicative behaviors that may hinder social integration.
A person's ability or inability to communicate is the most critical aspect of a hearing loss, and it is communication function, rather than ability to hear, that determines successful integration into family and social life.
References
American Academy of Matrimonial Lawyers (2009). Making Marriage Last. Retrieved April 13, 2009 from www.aaml.org/go/library/publications/making-marriage-last/
Lindley, J. (2009). The significant other: A consumer perspective. Unpublished manuscript.
Communication Diet Theory: An Extended Foundation for Hearing Rehabilitation
August 31, 2009
Related Courses
1
https://www.audiologyonline.com/audiology-ceus/course/patient-perspective-what-your-clients-39939
The Patient Perspective: What Your Clients Need from You
To live well with hearing loss clients must employ non-technical dynamics that are often underrepresented or overlooked in standard clinical practice, such as the reframing of attitudes towards hearing loss, and embracing a range of non-technical behavioral game-changers. This course introduces client-centered concepts to help them become stronger self-advocates, better builders of relationships and equipped to improve almost any listening situation.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
The Patient Perspective: What Your Clients Need from You
To live well with hearing loss clients must employ non-technical dynamics that are often underrepresented or overlooked in standard clinical practice, such as the reframing of attitudes towards hearing loss, and embracing a range of non-technical behavioral game-changers. This course introduces client-centered concepts to help them become stronger self-advocates, better builders of relationships and equipped to improve almost any listening situation.
39939
Online
PT60M
The Patient Perspective: What Your Clients Need from You
Presented by Shari Eberts, Gael Hannan
Course: #39939Level: Introductory1 Hour
AAA/0.1 Introductory; ACAud inc HAASA/1.0; AHIP/1.0; ASHA/0.1 Introductory, Professional; BAA/1.0; CAA/1.0; Calif. SLPAB/1.0; IACET/0.1; IHS/1.0; Kansas, LTS-S0035/1.0; NZAS/1.0; SAC/1.0; TX TDLR, #142/1.0 Non-manufacturer, X
To live well with hearing loss clients must employ non-technical dynamics that are often underrepresented or overlooked in standard clinical practice, such as the reframing of attitudes towards hearing loss, and embracing a range of non-technical behavioral game-changers. This course introduces client-centered concepts to help them become stronger self-advocates, better builders of relationships and equipped to improve almost any listening situation.
2
https://www.audiologyonline.com/audiology-ceus/course/adult-assessments-in-hearing-healthcare-38660
Adult Assessments in Hearing Healthcare: Working Across the Continuum
This five-course series on adult assessments in hearing health is intended to stimulate collaborative approaches for hearing health professionals, regardless of what hearing technologies they typically provide. Ideally, professionals will support patients in their long-term hearing loss journey, facilitating transitions when appropriate and a comfortable sense of the range of ways hearing loss can be addressed throughout one’s hearing journey.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
Adult Assessments in Hearing Healthcare: Working Across the Continuum
This five-course series on adult assessments in hearing health is intended to stimulate collaborative approaches for hearing health professionals, regardless of what hearing technologies they typically provide. Ideally, professionals will support patients in their long-term hearing loss journey, facilitating transitions when appropriate and a comfortable sense of the range of ways hearing loss can be addressed throughout one’s hearing journey.
38660
Online
PT300M
Adult Assessments in Hearing Healthcare: Working Across the Continuum
Presented by Camille Dunn, PhD, Susan Good, AuD, MBA, Alejandra Ullauri, AuD, MPH, Ted McRackan, MD, MSCR, Donna L. Sorkin, MA, Rene Gifford, PhD
Course: #38660Level: Intermediate5 Hours
AAA/0.5 Intermediate; ACAud inc HAASA/5.0; ASHA/0.5 Intermediate, Professional; BAA/5.0; CAA/5.0; Calif. SLPAB/5.0; IACET/0.5; IHS/5.0; Kansas, LTS-S0035/5.0; NZAS/3.0; SAC/5.0; Tier 1 (ABA Certificants)/0.5
This five-course series on adult assessments in hearing health is intended to stimulate collaborative approaches for hearing health professionals, regardless of what hearing technologies they typically provide. Ideally, professionals will support patients in their long-term hearing loss journey, facilitating transitions when appropriate and a comfortable sense of the range of ways hearing loss can be addressed throughout one’s hearing journey.
3
https://www.audiologyonline.com/audiology-ceus/course/roles-audiologists-and-dispensers-working-38413
The Roles of Audiologists and Dispensers Working with Hearing Aid Users in Cochlear Implant Candidacy, in partnership with American Cochlear Implant Alliance
This course will review the multiple roles audiologists and hearing aid dispensers play in the continuity of care for hearing aid users—from screening and referring potential cochlear implant candidates to performing comprehensive cochlear implant evaluations prior to referring candidates to cochlear implant surgical teams. Adults with hearing loss live with a chronic condition that requires hearing services for life. Professionals working with them must be able to provide services and guidance to these patients throughout their lifespan. Depending on their licensure and scope of practice, hearing aid dispensers and audiologists can screen, assess, and counsel their own patients regarding cochlear implants as a treatment option.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
The Roles of Audiologists and Dispensers Working with Hearing Aid Users in Cochlear Implant Candidacy, in partnership with American Cochlear Implant Alliance
This course will review the multiple roles audiologists and hearing aid dispensers play in the continuity of care for hearing aid users—from screening and referring potential cochlear implant candidates to performing comprehensive cochlear implant evaluations prior to referring candidates to cochlear implant surgical teams. Adults with hearing loss live with a chronic condition that requires hearing services for life. Professionals working with them must be able to provide services and guidance to these patients throughout their lifespan. Depending on their licensure and scope of practice, hearing aid dispensers and audiologists can screen, assess, and counsel their own patients regarding cochlear implants as a treatment option.
38413
Online
PT60M
The Roles of Audiologists and Dispensers Working with Hearing Aid Users in Cochlear Implant Candidacy, in partnership with American Cochlear Implant Alliance
Presented by Alejandra Ullauri, AuD, MPH
Course: #38413Level: Introductory1 Hour
AAA/0.1 Introductory; ACAud inc HAASA/1.0; AHIP/1.0; ASHA/0.1 Introductory, Professional; BAA/1.0; CAA/1.0; Calif. SLPAB/1.0; IACET/0.1; IHS/1.0; Kansas, LTS-S0035/1.0; NZAS/1.0; SAC/1.0
This course will review the multiple roles audiologists and hearing aid dispensers play in the continuity of care for hearing aid users—from screening and referring potential cochlear implant candidates to performing comprehensive cochlear implant evaluations prior to referring candidates to cochlear implant surgical teams. Adults with hearing loss live with a chronic condition that requires hearing services for life. Professionals working with them must be able to provide services and guidance to these patients throughout their lifespan. Depending on their licensure and scope of practice, hearing aid dispensers and audiologists can screen, assess, and counsel their own patients regarding cochlear implants as a treatment option.
4
https://www.audiologyonline.com/audiology-ceus/course/listening-effort-fatigue-and-social-31022
Listening Effort, Fatigue and Social Isolation: Consequences of Age Related Hearing Loss
A hallmark of age related hearing loss is difficulty understanding in noisy environments. The difficulty requires significant listening effort on the listener’s part which, when prolonged, is associated with fatigue. The fatigue in combination with the listening effort and cognitive load often leads people to withdraw from social situations. Social disengagement has many downstream negative outcomes which will be discussed in this course.
auditory, textual, visual
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
Listening Effort, Fatigue and Social Isolation: Consequences of Age Related Hearing Loss
A hallmark of age related hearing loss is difficulty understanding in noisy environments. The difficulty requires significant listening effort on the listener’s part which, when prolonged, is associated with fatigue. The fatigue in combination with the listening effort and cognitive load often leads people to withdraw from social situations. Social disengagement has many downstream negative outcomes which will be discussed in this course.
31022
Online
PT90M
Listening Effort, Fatigue and Social Isolation: Consequences of Age Related Hearing Loss
Presented by Barbara Weinstein, PhD
Course: #31022Level: Intermediate1.5 Hours
AAA/0.15 Intermediate; ACAud inc HAASA/1.5; AHIP/1.5; BAA/1.5; CAA/1.5; Calif. SLPAB/1.5; IACET/0.2; IHS/1.5; Kansas, LTS-S0035/1.5; NZAS/2.0; SAC/1.5
A hallmark of age related hearing loss is difficulty understanding in noisy environments. The difficulty requires significant listening effort on the listener’s part which, when prolonged, is associated with fatigue. The fatigue in combination with the listening effort and cognitive load often leads people to withdraw from social situations. Social disengagement has many downstream negative outcomes which will be discussed in this course.
5
https://www.audiologyonline.com/audiology-ceus/course/sound-bites-dr-archelle-georgiou-37427
Sound Bites: Dr. Archelle Georgiou on How Hearing is Tied to Our Overall Health
Dr. Dave Fabry talks to Starkey's Chief Health Officer, Archelle Georgiou, MD, about the importance of early identification of hearing loss, degrees of hearing loss and implications, why hearing professionals are vital to the healthcare ecosystem, and hearing loss during the holidays.
auditory
129
USD
Subscription
Unlimited COURSE Access for $129/year
OnlineOnly
AudiologyOnline
www.audiologyonline.com
Sound Bites: Dr. Archelle Georgiou on How Hearing is Tied to Our Overall Health
Dr. Dave Fabry talks to Starkey's Chief Health Officer, Archelle Georgiou, MD, about the importance of early identification of hearing loss, degrees of hearing loss and implications, why hearing professionals are vital to the healthcare ecosystem, and hearing loss during the holidays.
37427
Online
PT30M
Sound Bites: Dr. Archelle Georgiou on How Hearing is Tied to Our Overall Health
Presented by Dave Fabry, PhD, Archelle Georgiou, MD
Course: #37427Level: Introductory0.5 Hours
AAA/0.05 Introductory; ACAud inc HAASA/0.5; AHIP/0.5; ASHA/0.05 Introductory, Professional; BAA/0.5; CAA/0.5; IACET/0.1; IHS/0.5; Kansas, LTS-S0035/0.5; NZAS/1.0; SAC/0.5
Dr. Dave Fabry talks to Starkey's Chief Health Officer, Archelle Georgiou, MD, about the importance of early identification of hearing loss, degrees of hearing loss and implications, why hearing professionals are vital to the healthcare ecosystem, and hearing loss during the holidays.


