Why do so many pediatric audiologists seemed stressed? There are many reasons. One thing is undeniable: it is not an easy job. One specific reason is that it is often difficult for information to be obtained from and presented to the parents of infants or toddlers while assuring comprehension of the information. Language barriers, language comprehension, and learning styles all influence overall comprehension. Parental stress further adds to these issues.
The pediatric audiological evaluation process is occasionally wrought with emotion. Parental stress is evident before, during, and after the completion of the evaluation. Families do not always show up for their appointments when they are supposed to arrive. When the evaluation takes place, the child may not fully participate or may demonstrate abnormal findings which the parent can see instantaneously. It takes time to get valid and reliable information from very young children. Parental stress further complicates adequate comprehension of the results and implications during counseling.
Children are complicated. So are their parents. Their evaluation process is just one snap shot of the day. What occurred before and what will occur after all may influence what happens during that snap shot during the evaluation. Yet, it is not something the audiologist can influence or control.
Ultimately, the audiologist is responsible for helping the parents understand what they need to know to follow-up appropriately. To accomplish this, they have to do a high-quality job in communicating with families to become efficacious in their work and ultimately reduce stress, burnout, and possible professional attrition.
Objectives
To achieve the goal of reduced work stress, burnout, and professional attrition, modifications can be made to the pediatric audiologist's role. This article presents several objectives that will assist the pediatric audiologist in becoming a better communicator and more efficient worker:
- Define professional burnout and determine its impact on various aspects of daily and long-term clinical practice.
- Know the inherent problems in obtaining and providing information during the pediatric audiological diagnostic process.
- Define various learning styles.
- Determine if a professional's current methods of obtaining and providing information in the diagnostic setting are efficient, effective, and valuable.
- Identify sources and resources to assist in evolving the professional's practice into a more efficient one.
Stress is defined in two ways - from a generic perspective and from a physiologic perspective (Dictionary.com, 2008). The general definition describes stress as physical, mental, or emotional strain or tension. The physiologic definition describes stress as a specific response by the body to a stimulus, as fear or pain that disturbs or interferes with the normal physiological equilibrium of an organism. Stress is often part of daily life as a pediatric audiologist. However, being aware of its presence can allow the audiologist to find ways to alleviate its effects. If the audiologist is not aware of the stress or can not facilitate changes to reduce stress, burnout occurs.
Burnout is a job-related condition involving feelings of emotional exhaustion, depersonalization, and reduced personal accomplishment (Maslach, 2003;1996;1981). It is a dynamic process, often caused by excessive work demands, resulting in avoidance and withdrawal (Kulik, 2006;Schaufeli & Buunk, 2003). Stress is at the core of burnout. Burnout can also cause stress. The short and long-term consequences of burnout can be extensive. Pediatric audiologists often feel that they are not championed by their administrators. They often do not have peer mentors to help them with ideas to resolve stress and find ways to reduce burnout. Having a few hectic and stressful days at work usually can be handled if the audiologist understands that the stress is temporary and can be reduced quickly. However, when there are no avenues to reduce the burnout, a pediatric audiologist may end up experiencing avoidance and withdrawal from work. The audiologist may feel their efforts are not sufficiently acknowledged by their peers, supervisors, administrators, and insurance companies that reimburse them for their services. Work efficiency reduces and others in the workplace, as well as the audiologist, experience the effects of the burnout condition. If this problem continues, professional attrition may occur.
The Bureau of Labor and Statistics (BLS), part of the U.S. Department of Labor, publishes information on the numbers of jobs available and the demand for those jobs in the future. For audiologists, more than 3,000 additional audiologists will be needed to fill the demand between 2002 and 2012—a 29% increase in job openings (U.S. Department of Labor, 2004).
A total of 6,000 job openings for audiologists are projected between 2002 and 2012 due to growth and net replacements. Therefore, a loss of 3,000 audiologists to burnout, retirement, and other issues will occur in a 10-year period (U.S. Department of Labor, 2004). Neither one of the two major national professional audiology organizations have data to pinpoint how much of the professional attrition is due to burnout, retirement, elimination of positions, changing from full-time to part-time status, or anything else. Neither do they have information on the amount of experience in pediatric fields these audiologists possess. Therefore, it is entirely unclear if we are losing our best and most experienced pediatric diagnosticians or whether there is a good rate of exchange through mentoring occurring. Regardless, one can expect that burnout is one of the issues that results in professional attrition.
Figure 1 below is yet another way of describing this enveloping issue that may result in job attrition or positive change in the workplace.
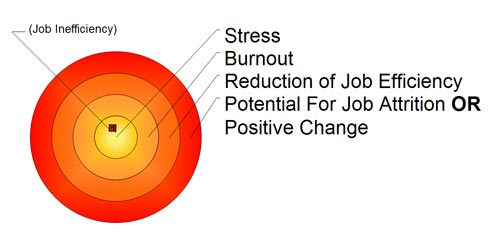
Figure 1. Relationship between Stress, Burnout, Job Efficiency, and Job Attrition.
Obtaining and Providing Information in the Pediatric Diagnostic Process
Inherent problems exist in obtaining and providing information in the pediatric diagnostic process in the field of audiology. These problems are present in other diagnostic fields, yet professional discussion of this important issue tends to be focused in realm of occupational therapy, not audiology or other pediatric diagnostic fields. Up to this time, solutions to these inherent problems have not been adequately addressed. Obviously stress, burnout, job efficiency, and professional attrition will result without the presentation of sound solutions to the daily issues impacting the pediatric audiologist.
Three fundamental facts presented here are not part of most formal education programs, but are critical to the efficiency and effectiveness of communicating during daily work experiences.
- Preferred learning styles that the parent possesses can have a significant impact on what a parent understands from the diagnostic session.
- Reading ease and/or reading grade level can significantly impact what a parent learns from you.
- The audiologist's own language and vocabulary may or may not be remotely related to the parent's own native language and vocabulary.
In order to communicate effectively, learning styles, reading ease and reading grade level, and language will be discussed in detail here. These three fundamental issues are at the heart of assisting the audiologist to become a more efficient and effective communicator.
Learning Styles
Dictionary.com (n.d.) defines learning style as an individual's mode of gaining knowledge, especially a preferred or best method. By understanding your own preferred learning styles, you can facilitate how efficient you can be in learning new information and skills. By understanding the parent's learning styles, the audiologist can differentiate how to disseminate information to become more efficient, less stressed, and ensure good comprehension.
There are several ways to determine one's learning style. The Index of Learning Styles Questionnaire (available at www.engr.ncsu.edu/learningstyles/ilsweb.html) is a good way to assess preferred learning styles. The 44-item questionnaire is designed to hone in on a person's four pairs of learning styles. Though people may have learning style tendencies toward one component of each pair, they usually benefit from all the styles. The four pairs will be presented below with explanations provided from the Web site. Additionally, more comprehensive explanations of the learning pairs and the analysis of the results are available on the Web site.
Learning Pair One:
ACTIVE AND REFLECTIVE LEARNERS
Active learners tend to retain and understand information best by doing something active with it-discussing or applying it or explaining it to others. Reflective learners prefer to think about it quietly first.
Learning Pair Two:
SENSING AND INTUITIVE LEARNERS
Sensing learners tend to like learning facts;intuitive learners often prefer discovering possibilities and relationships.
Learning Pair Three:
VISUAL AND VERBAL LEARNERS
Visual learners remember best what they see: pictures, diagrams, flow charts, time lines, films, and demonstrations. Verbal learners get more out of words: written and spoken explanations. Everyone learns more when information is presented both visually and verbally.
Learning Pair Four:
SEQUENTIAL AND GLOBAL LEARNERS
Sequential learners tend to gain understanding in linear steps, with each step following logically from the previous one. Global learners tend to learn in large jumps, absorbing material almost randomly without seeing connections, and then suddenly "getting it."
By reviewing this article, you may see that it is presented using the following primary learning styles: active, sensing, verbal, and sequential. If the reader learns best using these styles, the information presented should be comprehended with more ease. However, if the reader is more of an intuitive, visual, and global learner, the expectation for good and quick comprehension would be poorer.
As learning styles are now defined, it would seem beneficial to know what learning styles parents use. However, it is not reasonable or efficient to ask parents to take this assessment. There are easier ways to do this when the daily schedule is filled with new patients. At the start of each session, it will help to observe the parents and the family interactions. It may even begin during the time the family is waiting in the lobby to register or fill out forms. At various times during the pediatric evaluation, simple questions can be presented to help identify parental learning styles. Some questions may include:
- Do you want me to go into detail or give you the overall picture?
- Would you like to have handouts and graphs that explain what we will talk about?
- Do you want to see some pictures that show us what is going on?
- Do you want me to discuss this in detail now or would you like to set up a meeting to talk about this later?
- Do you want me to tell you how your concerns are connected to your child's hearing problems?
- Do you want to watch a video that explains this?
- Do you want names of other parents who have children with similar hearing problems?
Another major issue arises in providing information in an appropriate and comprehendible manner. The following statistics are disconcerting, yet pertinent, to the goal of improving communication.
About 20% of the US population is functionally illiterate;the percentage may be higher in certain subsets of the population. When questioned about medical care, 41.6% of the population could not comprehend directions to take medicine while they had an empty stomach;26% could not understand information regarding when their next appointment was scheduled. Close to 50% of Americans could not read well enough to comprehend a single message in a short written publication. The average reading level of Americans with young children is equivalent to the 7th or 8th grade. However, professional materials written for parents are typically presented at the 10th grade reading level or above (Association of Medical Directors of Information Systems, n.d.).
The second fundamental fact in attempting to improve communication is by understanding the importance of reading ease and reading grade levels. There are several published programs that can assist the audiologist in determining whether the information presented is in accordance with the parental level of reading ease and reading grade level. Providing information using high-level language structures may not be appropriate for the parent. Presenting information in any form should account for the parental reading level.
It is not necessary to "dumb down" information. The key is to write and talk clearly in an approachable fashion for the audience. Comprehension is greatest with materials that are written at least two grade levels lower than the education level of the audience. For complex information, and for information that can be expected to cause an emotional response, writing at more easily comprehended reading levels is more effective.
Flesch Reading Ease
The Flesch Reading Ease formula is a good source to determine reading ease, and is available on most word processing programs in use today. It has a good reputation for providing valid results. The output of the Flesch Reading Ease formula is a number from 0 to 100, with a higher score indicating easier reading. The average document has a Flesch Reading Ease score between 6 and 70. Audiologists can adjust their written documents to obtain a high reading ease score.
Flesch-Kincaid Grade Level
The Flesch-Kincaid Grade Level formula converts the Reading Ease Score to a U.S. grade-school level. Most parents have a general understanding of the meaning of grade-school level performance. By formulating a reading grade level, the audiologist can determine if the material presented is too difficult or easy. Again, this formula is available on most word processing programs today.
It is easy to review and evaluate reading ease and reading grade level of professionally prepared documents designed for parents. Many documents reviewed from very reputable sources within the profession were at the 8.1 or higher reading grade level. As noted above, the average reading level of parents with young children is in the 7th to 8th grade range. Therefore, material should be presented at the 5th to 6th grade reading level or even lower if the information is likely to cause an emotional response. Based upon this information, the audiology profession is doing a disservice to the parents they are trying to reach. An adjustment in the presentation of written material is in order to allow for more appropriate reading levels.
Several forms at Resurrection Medical Center in Chicago were revised based on the above information. Forms and information presented in a written format were easily reduced from a 12th grade level to a 3rd to 5th grade level. Forms continue to be modified to meet the needs of the parents. Forms directed toward physicians have higher reading levels but are still reasonable if the parent decides to fill out the forms. Examples of these forms, which can be used only with permission from Resurrection Medical Center, are provided below.
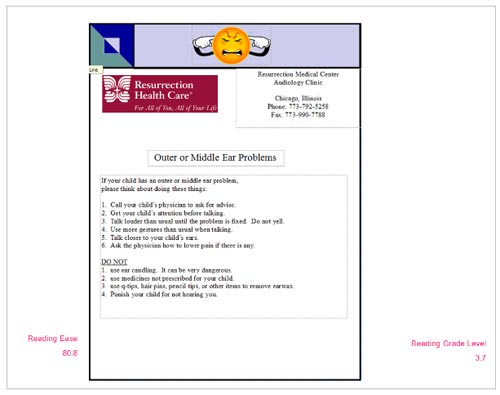
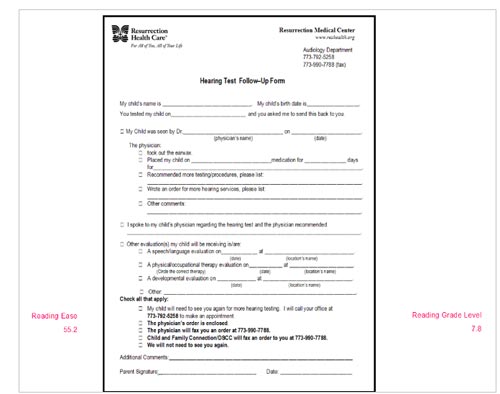
Click Here to View a Larger Version of Figure 2 (PDF)
Figure 2. Examples of adjusted reading-level material, Resurrection Medical Center, Chicago.
The Hearing Test Follow-Up Form (Figure 2) was originally presented in a format that was at a 10th grade level. After rewording to a 7.8 reading level, most of the parents were adequately completing and returning the form or they were asking their physicians or ENTs to do it. This form has been highly successful in relaying information and reducing the number of follow-up phone calls.
Native Language and Vocabulary
The third fundamental skill in becoming a better and more effective communicator is to understand that the audiologist's own native language and vocabulary may or may not be remotely related to the parent's own native language and vocabulary. Our society is composed of many people who do not speak English as their native language. Unless we are fluent in the parent's language, poor comprehension is almost a guarantee for both the audiologist and parent.
Consider the parent who uses English as a second or even third language. In a comprehensive study, adult literacy students often lacked literacy skills in their own native language as well in general English communication skills (Condelli & Wrigley, 2003). These learners faced the challenge of developing basic skills for decoding, comprehending, and producing print, in addition to learning English. The average reading comprehension and reading vocabulary after 9 months of formal instruction was at the 1.3 grade level for about 500 ESL adult students (Condelli and Wrigley, 2003). These statistics pose even greater problems for the audiologist and the parents. Further reducing reading grade level and increasing reading ease is critical, even when the information is presented in the native language of the parent.
Both amusing and unfortunate tales can be told of situations where the audiologist and the parent speak different languages. Even language interpreters get caught in the web of misunderstanding. In order to do our best to obtain accurate information and to assure that the parents understand the results, implications, and recommendations, it is critical to use a variety of techniques.
Presenting case history questions in the parent's native language is critical. If the parent can not read, a language interpreter is needed to present the questions orally. The interpreter should also detail how much time will be taken for the appointment and what will go on during the evaluation. Of course, the audiologist must present this information in a simple manner and with attention to vocabulary and grammar in order to reduce confusion and stress. Follow-up forms should also be in the native language of the parents.
The following is an example of a case history provided to parents. English, Spanish, and Polish forms were all prepared so that each number reflected the same statement no matter which language was used. Professional translators were utilized to transfer the following English case history into Spanish and Polish. Please do not use the form without written consent from Resurrection Medical Center, Chicago, Illinois.
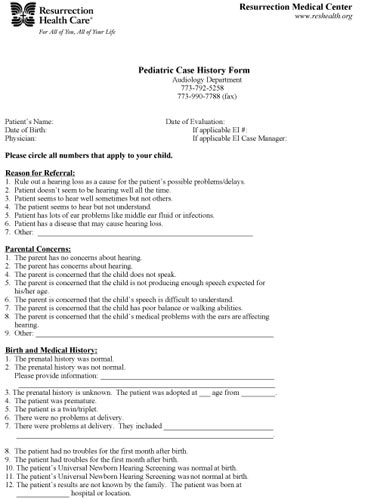
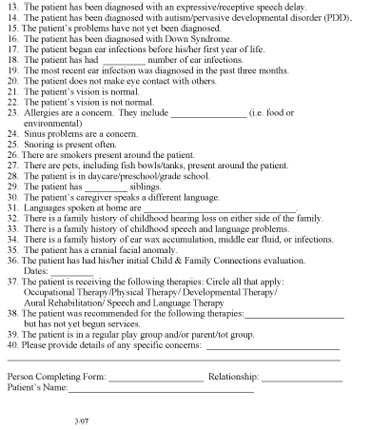
Click Here to View a Larger Version of Case History Form (PDF)
General Guidelines to Improve Communication During Pediatric Audiologic Evaluations
Now that the three fundamental communication issues have been detailed, it is important to pull this information into valuable suggestions that can help the audiologist individually alter communication strategies to meet the needs of each family. The following sections offer such suggestions.
- Present information in the parent's primary language.
- Utilize professional interpreters when needed and whenever possible.
- Provide clear information on how the parents can get to your office and what they should bring to the appointment.
- Use a language level at least two reading levels below the parent's language level.
- Keep sentences short. Sentence length is the single greatest factor affecting comprehension.
- Use terminology that is familiar to your audience.
- Avoid jargon.
- Avoid overuse of modifiers.
- Use terms that have single meanings in the parent's native language. Multiple meanings lead to confusion.
- Provide as much pertinent information to the caregivers in their own best learning style to reduce follow-up phone calls.
- Utilize appropriate professional organization handouts or your own handouts to provide information.
- Use a patient Follow-Up Form when needed.
- Paperless software options can facilitate report writing, generate informational handouts, store data, schedule patients, bill for services, generate registration forms, etc.:
- Nuance PDF Converter
- Dragon Naturally Speaking Medical Edition
- Trigram Med Temps also stores case history and other data
- MACspeech Dictate
- E-speaking.com (free) for Windows
- Microsoft XP Office Speech Recognition engine
- Nuance PDF Converter
- Reading level and reading ease software
- Appropriate professional organization Web sites
- Action plans
- Obtain orders and/or prior authorizations as well as insurance information and case histories before the day of the evaluation.
- Get as much paperwork done ahead of time.
- Adequately train staff to disseminate pre-appointment information and written material.
- Format a case history so that statements need only to be circled instead of answered.
- Use software programs to generate simple forms.
- Format the case history with the same statements in the same order no matter what language is being used.
- Format specific reports to exactly meet the authorizing facility's requirements.
- Prepare multiple facsimile cover sheets for those whom you often send information.
- Have someone make appointment reminder calls the day before the appointment. You can also use telephone software programs to make automated calls, though you cannot account for non-English language listeners or parental questions.
- Use e-mail if possible and acceptable to the parents. Be careful to use disclosure statements just like you use on a fax cover sheet.
- Use self-addressed stamped envelopes for follow-up forms.
- Utilize professional translation services for forms, informational handouts, and Web site development.
- Back-up your data.
- Obtain orders and/or prior authorizations as well as insurance information and case histories before the day of the evaluation.
Pediatric diagnostic audiology services are essential to our society. In an age when universal newborn hearing screening has been mandated nationally and implemented in various degrees in most states, prevention, early detection, thorough evaluation, and follow-up are all necessary. In addition, hearing loss in infants, toddlers, and older children has a well-documented, long-term impact on many aspects of society.
Unfortunately, factors out of the control of the audiologist lead to stress. On the other hand, pediatric audiologists can reduce stress by making a variety of adjustments in their daily lives. Applying aspects of the information presented can make a profound impression on an audiologist's skills to improve effective and efficient communication and counseling, thus reducing stress, burnout, and professional attrition.
Some fundamental ways to improve communication and counseling are by using appropriate language, reading levels, and a variety of media to obtain and explain information. Parents absorb information and recommendations in many ways. These ways may or may not be congruent with the audiologist's preferred methods. Therefore, it is important to establish how the parents take in information and understand recommendations by using their learning styles and reading levels to present the information. Developing or using appropriate pre-made forms can significantly reduce miscommunication and improve counseling. Alteration in the audiologist's communication and presentation of information can have a significant impact on the time investment and efficiency of daily work efforts.
Finally, it is helpful to establish office procedures that reduce paperwork and follow-up phone calls. The overall improvement in communication and reduction in inefficient office procedures results in a more cost-effective and streamlined pediatric practice. By combining more efficient communication formats and improving office procedures, professional and parental stress can be reduced. As a result, the pediatric audiologic evaluation process becomes a less stressful and more manageable experience for everyone involved.
Acknowledgements
This paper was adapted from a presentation presented on AudiologyOnline on October 3, 2008. Thanks to Paul Dybala and Carolyn Smaka for their enthusiasm and encouragement in allowing me to bring this topic to the AudiologyOnline audience.
References
Association of Medical Directors of Information Systems (n.d.). Comprehension and reading level. The Informatics Review. Retrieved September 2, 2008 from the Frequently Asked Questions section on www.informatics-review.com/.
Condelli, L. & Wrigley, H.S. (2003). Instruction, language, and literacy: What works for adult ESL literacy students. Washington, D.C: U.S. Department of Education's Office of Vocational and Adult Education and the Planning and Evaluation Service.
Felder, R.M. & Henriques, E.R. (1995). Learning and teaching styles in foreign and second language education. Foreign Language Annals, 28, 21-31.
Index of Learning Styles Questionnaire. Retrieved September 7, 2008, from www.engr.ncsu.edu/learningstyles/ilsweb.html
Kulik, L. (2006). Burnout among volunteers in the social services: The impact of gender and employment status. Journal of Community Psychology, 34, 541-562.
learning style. (n.d.). Webster's New Millennium™ Dictionary of English, Preview Edition (v 0.9.7). Retrieved September 06, 2008, from dictionary.reference.com/browse/learning style
Maslach, C. (2003). Job burnout: New directions in research and intervention. Current Directions in Psychological Science, 12, 189-192.
Maslach, C., Jackson, S. E., & Leiter, M. P. (1996). The Maslach burnout inventory (3rd ed.). Palo Alto, CA: Consulting Psychologists Press.
Maslach, C. & Jackson, S.E. (1981). The measurement of experienced burnout. Journal of Occupational Behaviour, 2, 99-113.
Resurrection Medical Center. Various forms and handouts. Chicago.
Schaufeli, W.B. & Buunk, B.P. (2003). Burnout: An overview of 25 years of research and theorizing. In M.J. Schabracq, J.A.M. Winnubst, & C.L. Cooper (Eds.) The Handbook of Work and Health Psychology (2nd ed.) (pp. 383-425). Denmark: John Wiley & Sons, Ltd.
stress. (n.d.). Dictionary.com Unabridged (v 1.1). Retrieved July 24, 2008, from dictionary.reference.com/browse/stress
U.S. Department of Labor. (2004). Occupational employment projections to 2012. Monthly Labor Review. Washington, DC: Author.


