Picture a high, hard ground overlooking a swampy lowland. This landscape represents your practice. As audiologists, we are most frequently found working on what reflective practice theorist Donald Schön (1987) referred to as the high, hard ground of professional practice. On this high ground, practitioners aim to apply research-generated evidence and technical rationality to best practice(s). Technical rationality is defined by Schön (1987) as the dominant epistemology of practice in which professional activity consists of instrumental problem solving through the application of scientific theory and technique. This is certainly necessary for good practice, and aligns with the current dominant professional discourse in audiology: Evidence-Based Practice (EBP) (Cox, 2000; Moodie, Johnson, & Scollie, 2008). However, audiologists must also attend to the swampy lowland of our practice, which contains the messier issues that may elude purely technical solutions (Schön, 1987). Here, the field of audiology could benefit from a solid theoretical foundation in alternative epistemologies of practice.
Reflective practice is thus offered as an alternative, or better still, a complementary, epistemology of practice (Schön, 1983). Many health and social care professions have found reflective practice to be most helpful in navigating the complexities of practice situations (e.g. Bartlett, Lucy, Bisbee, & Conti-Becker, 2007; 2009; Benner, 1984; Kinsella, 2001). This article presents reflective practice as a professional development tool for audiologists, complementary to EBP, yet drawing primarily from a different source of knowledge: the audiologist's practice experience.
What is Reflective Practice?
Kolb (1984) suggested that learners require four types of ability to effectively learn: concrete experience abilities, reflective observation abilities, abstract conceptualization abilities, and active experimentation abilities (Figure 1). Experience is necessary for learning, and reflection in and on experience can help us develop new knowledge (Dewey, 1910; 1938; Moon, 2004; Schön, 1983).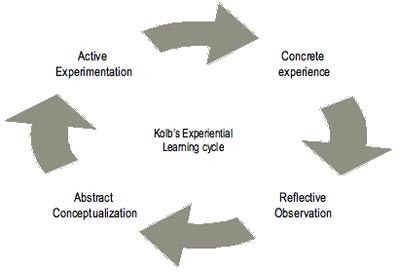
Figure 1. Kolb's Experiential Learning cycle.
We all reflect in our daily lives, albeit to varying degrees; thus, we all have a common-sense idea of what it means to reflect. Formally defined, reflection is "...active, persistent and careful consideration of any belief or supposed form of knowledge in light of the grounds that support it and further conclusions to which it tends" (Dewey, 1910, p. 9). Reflection makes action intelligent and meaningful, as opposed to blind and impulsive (Dewey, 1910). Reflection has been taken up by many disciplines, in various forms [e.g. business (Cunliffe, 2002), education (Boud & Walker, 1998; Schön, 1983; 1987), nursing (Benner, 1984), occupational therapy (Kinsella, 2001), physical therapy (Abrandt Dahlgren, Richardson, & Kalman, 2004) and social work (Plath, 2006)]. Schön (1983; 1987) focused on reflection as used by professional practitioners, or reflective practice.
Potential outcomes of becoming a reflective practitioner, outlined by Kinsella (2001) include: 1) valuing knowledge aside from the important skills and evidence that make up audiology practice, such as practical, social, political, economic, and personal knowledge, 2) consideration of the context of our practice and the lives of our patient/clients (which may ensure appropriate patient/client-centered counseling, for example), 3) exploring the assumptions that underpin our practices (have you ever assumed that a patient/client would act a certain way based on her diagnosis, level of education, socio-economic status?), 4) acknowledging and understanding our espoused or conscious theories of practice in comparison to our actual theories of practice (consider a supposedly collaborative multi-disciplinary team that lacks respect and communication amongst its members). Further, critical reflection may lead us to think differently about professionals in public policy and society (Brookfield, 1998) and will be discussed near the end of this article. Reflective practice emphasizes reflection-on-action and reflection-in-action, which is related to tacit knowledge, knowing-in-action, and professional artistry (Schön, 1983). These key elements of reflective practice are demonstrated through the following examples.
Reflection-in-Action
Reflection-in-action refers to reflective processes that occur in the midst of action without interruption; our thinking reshapes what we are doing as we are doing it (Schön, 1987). An example of reflection-in-action in audiology occurs when a proficient, experienced audiologist is performing Visual Reinforcement Audiometry (VRA). This operant conditioning procedure requires the audiologist to present appropriate auditory test signals at various levels as required, present a visual reinforcer when the baby correctly turns her head after hearing the auditory stimuli, center the baby's gaze back to midline, and record all correct head turns, lack of head turns, false positives and control trials. This involves operating several pieces of equipment at once and must be done in a seamless fashion, because infants have such short attention spans and are relatively unpredictable in terms of how they will react and respond to the procedure. The audiologist must be able to assess if the child is developmentally ready to perform the VRA tasks, and must efficiently and effectively monitor and make adjustments to her own performance, based on the baby's individual needs. I use the word performance here because it is both an art and a science to obtain accurate hearing thresholds from the infant, while also ensuring that the experience is enjoyable, rather than traumatic. A bad experience in the sound booth may make it difficult to regain the child's trust for undergoing future assessment and habilitation. Further, the audiologist must make "on the fly" decisions when the assessment is not going as planned, whether the baby will not condition to the task, is frightened by the environment, stimuli or reinforcers, or simply feels irritable that day.
The above example of reflection-in-action demonstrates our use of tacit knowledge. Tacit knowledge is defined as the often unspoken knowing that guides us in intelligent action. It is the notion that it is difficult to put into words how we know how to do certain things (Polanyi, 1958; Schön, 1983). In the example of VRA, tacit knowledge exists in recognizing when a baby's head-turn responses are about to extinguish. It is often challenging to describe to someone (a student, for example), exactly how we know this. When we put our tacit knowledge to use, we demonstrate knowing-in-action. For example, when the audiologist recognizes that the baby's responses are about to extinguish, she may change her otherwise seemingly automatic procedures and present a different stimulus type or change the ear being tested so that the baby's attention to the task is maximized.
Reflection-in-action, tacit knowledge, and knowing-in-action combined make up our professional artistry. Professional artistry is a high-powered, esoteric type of competence exhibited in everyday acts of recognition, judgment and skillful performance (Schön, 1987). Many audiologists will say that the profession is both an art and a science. Professional artistry is the competence used by practitioners to handle indeterminate zones of practice (in which there is not necessarily one "right" solution), and is rigorous in its own right (Schön, 1987). Reflective practice offers us an avenue through which we may value, and thus actively develop, the artistic components of our practice. However, in traditional forms of education and professional development, we focus primarily on learning the science, perhaps assuming that the art will develop independently and naturally, with experience. Perhaps this is because it is difficult to make reflection-in-action, tacit knowledge, knowing-in-action and professional artistry explicit, or to engage in them purposely. Consider that perhaps the art and science of practice need not be separated, just as theory, research and practice should ideally be connected. This is where reflection-on-action may prove useful.
Reflection-on-Action
Reflection-on-action is intentional reflection on experiences of the past- to make sense of the actions taken, consider their consequences, and actively learn from the experience. Reflection-on-action thus extends one's knowledge base and potentially influences future action (Schön, 1983; 1987). Here is an example: Research demonstrates the value of using insert earphones to conduct VRA (Bagatto et al., 2005). However, a practitioner who has conducted VRA for decades without using insert earphones may not even consider the potential need for change, despite hearing or reading about evidence that demonstrates the benefits of insert earphones. Although the research evidence alone may not compel this practitioner to consider a change to her practice, reflection may help the practitioner uncover her reasons for resistance and the consequences of not being open to the change, and may help give the practitioner the motivation she needs to make the change. Reflection has the power to expose our assumptions, and lead us to question and re-think our values (Brookfield, 1998; Habermas, 1971). When we consider our patient/client's outcomes and satisfaction a priority, making time to explicitly engage in reflection may be worthwhile.
Reflective Writing as a Form of Professional Development
One way to make reflection a practical professional development tool is through writing. Through writing, practitioners can become enquirers of their own actions, feelings, beliefs, values, and identity in professional, cultural and political contexts. Further, writing can be an enjoyable way to engage in reflection. However, it is important to distinguish between traditional academic writing and reflective writing. Moon (2004) provides side-by-side comparisons of traditional academic or descriptive writing versus reflective writing and offers handouts to be used for learners new to reflective writing. This and other references for reflective practice resources are also provided at the end of this article.
A practical way to approach reflective writing is to do so with a specific purpose and guidance (Johns, 1984; 2002). Benner (1984) encouraged nurses to consider experiences that were critical to their practice, including those that were especially ordinary, particularly demanding, or that went unusually well. This aligns with Dewey's (1910) first step in reflective thinking: identifying an uncertainty. Next, these critical incidents should be reflected upon in terms of context, why the incident was critical, what the practitioner's concerns were at the time and how one might be affected for future practice (Benner, 1984). This aligns with Dewey's second stage of reflective thinking, with the nurse or practitioner investigating the reasons for their previous uncertainty. Benner (1984) saw this critical incident analysis as a way to facilitate study of expert practice, and to move novice practitioners toward expert levels of practice.
Critiques of Reflective Practice
A common critique of reflective practice is that we do not have time for it (Eraut, 1995). However, the benefits of engaging in reflection in and on practice may include improved job satisfaction and practice outcomes (Benner, 1984; King et al., 2007). In fact, studies have shown that, surprisingly, more than years of experience, a practitioner's capacity for engaging in reflection is linked to the development of expert levels of practice (Benner, 1984; King et al., 2007). Thus, the critique of a lack of time can be resolved by raising the value of reflection as a crucial element of good practice.
Another critique of reflective practice is that it may lead us to rely too heavily on an inward focus, thus creating a danger of missing out on our own weaknesses and inflating our professional esteem. Johns (1984; 2002) proposes that we acquire a mentor to support our reflective practices, or a critical companion. In the example of the audiologist reluctant to use insert earphones, open dialogue with a critical companion may have helped. Further still, we may bring reflection to a team level or to share the reflective process with our patient/client, but these are topics for another article. The problems of poor self-awareness and capacity for self-assessment are indeed issues related to reflection, but may be overcome by practitioners recognizing that they need to engage in dialogue with peers and mentors and potentially the public they serve (Cunliffe, 2002; Flyvbjerg, 2001; Freire, 2007; Johns, 1984; 2002).
Finally, reflective practice as proposed by Schön does not deeply address structural, societal and systemic issues that may constrain our actions and practices. To address this, a number of theorists have taken up reflective practice through a critical lens.
Critical Reflective Practice
Critical reflection is neatly distinguished from reflection by Mezirow (1990). Mezirow (1990) stated that reflection is the "process of critically assessing the content, process, or premise(s) of our efforts to interpret and give meaning to an experience," whereas critical reflection considers the "critique of assumptions about the content or process of problem solving...making a taken-for-granted situation problematic, raising questions regarding its validity" (p. 104-5). Critical reflection focuses more on systemic and societal conditions and more explicitly seeks change and emancipation (Habermas, 1971). Brookfield states that to become critically reflective, we need to find "lenses" that reflect back to us a stark and different picture of who we are and what we do (Brookfield, 1998). Some of these lenses are our colleagues' experiences, theoretical literature, our patient/clients' eyes, and our own experiences (Brookfield, 1998). The following is a personal example of critical reflection that uses both theoretical literature and my own practice experiences as reflective lenses.
Critical Reflection in Audiology
A very common ethical challenge in the current audiology climate is hearing instrument dispensing. In fact, this issue was raised by participants in a recent focus group to adapt a professional behaviors development log (Bartlett, Lucy, & Bisbee, 2006) for use in audiology (Ng, Bartlett, & Lucy, 2008). In dispensing clinics, audiologists assess hearing sensitivity, determine if hearing aids may be of benefit, and if so, prescribe, potentially dispense and fit these hearing aids for the patient/client. Audiologists may accrue financial gain from the sale of hearing aids. Moreover, manufacturers of hearing instruments may provide incentives to audiologists for the sale of a particular type of hearing aid. As a new clinical audiologist I encountered the dilemma of putting the patient/client first, despite conscious or even sub-conscious knowledge of the financial incentives of hearing aid sales.
Essentially, I found myself in the midst of a system-imposed ethical struggle, and perhaps as a new practitioner lacked experience to draw from in negotiating this situation. My employer's incentive program was mandatory, and while many of my colleagues were able to practice with integrity in this setting, I personally struggled to reconcile the "fit" of my actual practice within my espoused theory of patient/client-centered practice. Unable to resolve the tensions I was feeling, I eventually left this position and returned to school to study Health Professional Education. I continue to practice as an educational audiologist, and I continue to find myself immersed in "swampy" practice situations, but I now have a language and theory with which to discuss and mediate these challenges.
Brookfield (1998) wrote: "Theory helps us 'name' our practice by illuminating the general elements of what we think are idiosyncratic experiences...theory can help us realize that what we thought were signs of our personal failings as practitioners can actually be interpreted as the inevitable consequence of certain economic, social, and political processes" (p. 200). Before I "found" the literature surrounding reflective practice, I held within me many unspoken tensions about professional practice issues in audiology. I did not possess the language of reflection and reflective practice discourses, so I doubted that what I was experiencing could be valid enough to be voiced in a scholarly way. I felt disheartened. Then I began to read Schön's The Reflective Practitioner, and felt inspired. I was given the gift of a language with which to voice my concerns, and with this I could begin to address some of the issues in which I was immersed. Despite my appreciation for this new ability to "name" my practice, I must state that one certainly could not be a good audiologist without a well-equipped technical and scientific toolkit. The valuing of reflective practice does not mean the devaluing of research evidence as a key source of knowledge to inform practice. Both are necessary, and both need a scholarly and practical space for discussion.
There is no denying that we need to keep abreast of new developments in research and technology in order to deliver optimal services to our patient/clients. Yet, we also need to value other forms of knowledge that inform practice, such as those described in this article. Reflective practice requires openness to an alternative way of thinking about knowledge, and perhaps an adjustment in our value system. This can be a challenging task. "Reflective thinking...involves overcoming the inertia that inclines one to accept suggestions at face value; it involves willingness to endure a condition of mental unrest and disturbance...[it] means judgment suspended during further inquiry; and suspense is likely to be somewhat painful" (Dewey, 1910, p. 13).
Audiology can learn from other professions, which have made steps toward improving education and practice through reflective practices. Four very practical resources for professionals are provided below.
- Professional Development and Reflective Practice: Strategies for Learning through Professional Experience, A Workbook for Practitioners (Kinsella, 2000). Available through the Canadian Association of Occupational Therapists.
- Preceptor Education Program www.preceptor.ca/index.html (Kinsella, 2007; Kinsella & Jenkins, 2007).
- A Handbook of Reflective and Experiential Learning: Theory and Practice (Moon, 2004).
- Reflective Practice: An Approach for Expanding Your Learning Frontiers https://ocw.mit.edu/index.htm (MIT OpenCourseWare).
References
Abrandt Dahlgren, M., Richardson, B., & Kalman, H. (2004). Redefining the reflective practitioner. In J. Higgs, B. Richardson & M. Abrandt Dahlgren (Eds.), Developing practice knowledge for health professionals (pp. 15-33). London, UK: Elsevier Science.
Bagatto, M., Moodie, S., Scollie, S., Seewald, R., Moodie, S., Pumford, J., et al. (2005). Clinical protocols for hearing instrument fitting in the Desired Sensation Level method. Trends in Amplification, 9(4), 199-226.
Bartlett, D. J., Lucy, D. S., & Bisbee, L. (2006). Item generation and pilot testing of the Comprehensive Professional Behaviours Development Log. Journal of Allied Health, 35(2), 89-93.
Bartlett, D. J., Lucy, S. D., Bisbee, L., & Conti-Becker, A. (2007, June). Understanding early professional socialization of physical therapy students: A critical step in facilitating professional development. Paper presented at the World Congress of Physical Therapy, Vancouver, Canada.
Bartlett, D. J., Lucy, S. D., Bisbee, L., & Conti-Becker, A. (2009). Understanding professional socialization of Canadian Physical Therapy students: A qualitative investigation. Physiotherapy Canada, 61(1), 15-25.
Benner, P. (1984). From Novice to Expert: Excellence and Power in Clinical Nursing Practice. Menlo Park, CA: Addison-Wesley.
Boud, D., & Walker, D. (1998). Promoting reflection in professional courses: the challenge of context. Studies in Higher Education, 23(2), 191-206.
Brookfield, S. (1998). Critically Reflective Practice. Journal of Continuing Education in the Health Professions, 18(4), 197-205.
Cox, R. M. (2000). Evidence-based practice in audiology. Journal of the American Academy of Audiology, 16(7), Special Issue.
Cunliffe, A. L. (2002). Reflexive dialogical practice in management learning. Management Learning, 33(1), 35-61.
Dewey, J. (1910). How we think. Mineola, NY: Dover Publications Inc.
Dewey, J. (1938). Experience and Education. New York, NY: Touchstone.
Eraut, M. (1995), Schön shock: A case for reframing reflection-in-action? Teachers
and Teaching, 1(1), 9-22.
Flyvbjerg, B. (2001). Making Social Science Matter. New York: Cambridge University Press.
Freire, P. (2007). Pedagogy of the Oppressed, 30th Anniversary Edition (originally published in 1970) (M. Bergman Ramos, Trans.). New York, NY: Continuum.
Habermas, J. (1971). Knowledge and human interests: A general perspective. Boston, MA: Beacon Press.
Johns, C. (1984). Guided reflection. In A. Palmer, S. Burns & C. Bulman (Eds.), Reflective Practice in Nursing: The Growth of the Professional Practitioner. Oxford, UK: Blackwell Science.
Johns, C. (2002). Guided reflection: advancing practice. Oxford, UK: Blackwell Science.
King, G., Bartlett, D. J., Currie, M., Gilpin, M., Baxter, D., Willoughby, C., et al. (2007). The development of expertise in pediatric rehabilitation therapists: Changes in approach, self-knowledge, and use of enabling and customizing strategies. Developmental Neurorehabilitation, 10(3), 223-240.
Kinsella, E. A. (2000). Professional Development and Reflective Practice: Strategies for learning through professional experience, A workbook for practitioners. Ottawa, ON: Canadian Association of Occupational Therapists.
Kinsella, E. A. (2001). Reflections on reflective practice. Canadian Journal of Occupational Therapy, 68(3), 195-198.
Kinsella, E. A. (2007). Advanced topics in reflective practice. In A. Bossers, M. B. Bezzina, S. Hobson, A. Kinsella, A. MacPhail, S. Schurr, T. Mosa, L. Rolleman, K. Ferguson, S. Deluca, J. Macnab & K. Jenkins (Eds.), Advanced topics in reflective practice: University of Western Ontario, Faculty of Health Sciences & The Ontario Ministry of Health and Long Term Care.
Kinsella, E. A., & Jenkins, K. (2007). Fostering reflective practice. In A. Bossers, M. B. Bezzina, S. Hobson, A. Kinsella, A. MacPhail, S. Schurr, T. Mosa, L. Rolleman, K. Ferguson, S. Deluca, J. Macnab & K. Jenkins (Eds.), On-line preceptor education program: Preparing partners of learning in the field. www.preceptor.ca: University of Western Ontario, Faculty of Health Sciences & The Ontario Ministry of Health and Long Term Care.
Kolb, D.A. (1984). Experiential Learning: experience as the source of learning and development. New Jersey, NJ: Prentice-Hall.
Mezirow, J. (1990). Fostering critical reflection in adulthood: A guide to transformative and emancipatory learning. San Francisco, CA: Jossey Bass.
Moodie, S., Johnson, A., & Scollie, S. (2008). Evidence-Based Practice and Canadian Audiology. Canadian Hearing Report, 3(1), 12-14.
Moon, J. A. (2004). A Handbook of Reflective and Experiential Learning: Theory and Practice. New York, NY: Routledge.
Ng, S., Bartlett, D., & Lucy, D. (2008). The Comprehensive Professional Behaviours Development Log - Audiology [Adapted with permission from Bartlett, D., Lucy, D., Bisbee, L. and Beggs, C. (2004). The Comprehensive Professional Behaviours Development Log. School of Physical Therapy, Faculty of Health Sciences, The University of Western Ontario, London, Canada]. The University of Western Ontario.
Plath, D. (2006). Evidence-Based Practice: Current issues and future directions. Australian Social Work, 59(1), 56-72.
Polanyi, M. (1958). Personal Knowledge: Towards a Post-Critical Philosophy. Chicago, IL: University of Chicago Press.
Schön, D. A. (1983). The reflective practitioner: How professionals think in action. New York, NY: Basic Books.
Schön, D. A. (1987). Educating the Reflective Practitioner: Toward a New Design for Teaching and Learning in the Professions. San Francisco, CA: Jossey-Bass Inc.

