Editor's Note:This text-based course is a transcript of the live seminar, "Modernizing Your Practice in Uncertain Times, Part 2: The Testing & Recommendation Phase of the Patient Journey," presented by Brian Taylor, Au.D. Please download supplemental course materials.
Thank you for joining me today. I hope there are a few tools or tactics that you will take away and apply to your practice that we discuss today. As some of you may have experienced first-hand, there are a lot of changes occurring in both the hearing healthcare industry and in the American & global economy today. I talk with people in practice around the country and hear a mixed bag as far as the economy and how their businesses are performing. I think uncertainty is a good way to summarize how the market is performing. As you can see, this is the title of the presentation, "Modernizing Your Practice in Uncertain Times". Today we are going to talk about a specific phase of the patient journey, which is the testing and recommendation process. We will discuss what we need to do to captivate and energize more of our patients when they come in the door, while also trying to stick to a data-driven, evidence-based clinical approach. Over the next hour, there are three ideas that I will focus on. I will talk about the fundamental drivers of any practices. These are things on a big picture level that we need to be focusing on in our practices. I will talk about some core behaviors that drive results. I am a big believer that we form habits early in our career. It is very difficult sometimes to reduce or eliminate those bad habits and change our behaviors in our interactions with patients. Finally, we will talk about some practical tools that we can use to differentiate our practices in these uncertain and turbulent economic times.
Why is it Important to Modernize?
I would first like to set the stage for why modernization of our practices is so paramount. I think there are two main reasons both of which don't have anything to do with audiology. The first reason is the concept of disruptive innovations or technology and how these disruptors might affect the evolution of hearing aids. Disruptive innovations have been around for a long time in society. They actually date back to the industry revolution, so you know this is certainly not a new concept. It has only been in the last few years that they have been surfacing in audiology and hearing care offices. I think it will only continue to be more of an issue as digital technology becomes cheaper to produce and more widely distributed. I think disruptive innovations really have the potential to transform our industry like they have transformed many other industries. Disruptive innovations target an underserved segment of the market by offering them a lower cost or "stripped down" version of a product that is currently available. Over time, disruptive innovations can overtake market leaders and may even drive them out of business. A quick example of a disruptive innovation would be MP3 recordings. Record stores are nearly nonexistent today because people download songs, rather than buy CDs at the local record store. Personal sound amplification products (PSAPs) and other direct-to-consumer amplification devices would certainly be considered a disruptive innovation that we need to combat. If you are looking for more information on the concept of disruptive innovations and how they have transformed various industries over the last 75 years, you can look at the work of Clayton Christensen. He has probably published a dozen books and articles on the topic of disruptive innovations. In the May 14, 2012 edition of the New Yorker magazine, there was a profile of him with a great summary of his work and his stature in the business community.
The second reason why it is important to modernize is that the so-called baby boomer market is much more diverse than we once thought. It is this combination of large diverse group of our population combined with the fact that our economy going through so much turmoil in the last five years that we need to rethink how we approach this group of so-called "healthy agers." I think a different, maybe more appropriate term, rather than baby-boomer, would be the healthy aging movement in an era of mindful spending. There has been some great work done in this area on an international scope by Bennett and O'Reilly (2010) in a book called Consumed: Rethinking Business in the Era of Mindful Spending. This book takes a very data-driven approach to how this very diverse group of people over the age of 60 is approaching the market. To sort of summarize there findings: People over the age of 60 expect to live longer & healthier; many expect to work well into their 70s; they are concerned about not having enough money for retirement; and, many want to have an emotional connection with their favorite businesses. The main point I want to make here is that modernizing your office in the midst of this disruptive technology and in the midst of the healthy aging movement falls on us to differentiate our practice. We have to be daring enough to find unique and interesting ways to personalize the services that we offer. Many of things we will discuss today are related to how we can make this a more personalized or customized interaction with every patient we see. Hearing aid technology is quickly becoming a commodity and we have to find other ways to differentiate our practices.
Retail/Productivity vs. Medical/Quality
Let's step back for a moment and examine the medical and retail aspects of Audiology. Our profession is somewhat unique in the sense that we world in both realms. If you put your business or retail hat on, what you really need to focus on is productivity. The three drivers of productivity, or how we generate more revenue in our practice, are a maniacal view of office traffic, number of units that we dispense every month, and our average selling price per unit. When you have a plan and process around those three components, I have found in my work over the last 5 years that this is often times the path to double-digit revenue growth in any business.
At the same time, we have to embrace the medical side of things. We are fitting a medical device. We are fitting a patient with a medical disorder, and we have to be cognizant of that fact as well. When we put our medical hat on, our focus needs to be on quality. There are three E's of quality. They are having a process and plan with maniacal focus on effectiveness (how we use evidence-based practice in our offices to make decisions), efficiency (work flow) in how the patient goes from point A to point B and so forth through their journey, and then finally an emphasis on results which is our ability to measure quality of care and outcomes. When you have a plan and process around the three E's, you are on the path to being the provider of choice in your marketplace. There are some real by-products of enjoying that status as provider of choice such as people flock to your door and you can charge a higher because people are willing to pay more for quality.
We know in our work that there are seven dimensions of quality. This is everything from the initial greeting and contact with your office all the way through quality of the product to benefit and satisfaction. There are also seven tools you can use to measure that quality. These can be both direct, objective ways to measure like real-ear measures and data logging, and there are also more indirect, proxy measures like checklists, tracking forms, and surveys.
Today I wanted to make the point that productivity and quality are equally important in any audiology/hearing aid dispensing practice.
Another foundational component of my talk is the six interaction stations of the patient journey. Most of us think of the patient journey as three distinct components: testing, fitting and follow-up. I think we need to rethink this paradigm and look at the patient journey along six distinct interactions These are the six points which I say every patient comes in direct contact with your clinic. The first "touch point" is promotion or awareness. Promotion is the way they find out about you. Phone scheduling, arrival, testing and recommendation, fitting and purchase, and follow-up make up the other five distinct "touch points." I think it is up to all of us to define what our vision is for the patient journey, how we want to deliver services, and then put together a plan for how that these unfold in your office. For the rest of the presentation we will almost exclusively talk about interaction station number 4, which is testing and recommendation. What are some things that we can do to make that a memorable event for our patients, while at the same time relying on good solid evidence to make clinical decisions?
One last foundational aspect before getting into the testing and recommendation phase of the patient journey is in the pre-fitting appointment where the testing and recommendation occurs. It is important to view this as a series of "next-step" behaviors. There is one chapter in the book that Gus Mueller and I wrote, the last chapter of Fitting and Dispensing Hearing Aids (2011), which gets into this. I also recently published a second book called Consultative Selling Skills for Audiologists (2011) which goes into much more detail. In the book, we really focus on this discovery and commitment concept. The discovery process has all the things you do to learn about the patient as a series of steps to gather information, everything from case history to the audiological assessment. The second phase is the commitment process where you are systematically reviewing the results, maybe conducting a demonstration, discussing options, overcoming objections, and then offering a specific choice at a specific price point to the patient. It is a series of next steps done in a very assumptive, methodical fashion. Today we will be talking about a few parts of that. Now that we've covered some background concepts, let's look more carefully at the testing and recommendation phase of the patient journey.
The Pre-Fitting Stage of the Appointment - Testing/Recommendation Phase of the Patient Journey
Let's begin by looking at what we need to do to understand the patient/buyer. Again it is important to recognize that we work in both the medical and the retail arena, and the more that we respect both sides of that equation, the more successful we can be. Much of this comes down to remembering that people have a choice in how they spend their money and their time. Not only is this a choice in who they get their hearing care from, but also a choice in how they spend their $2,000 to $5,000 for the purchase of technology that will improve their quality of life.
I have a fun way to talk about how we can better understand the buying behaviors of our patients or their buying preferences. This is by looking back 18 years or so. If we turn back the clock, you might recognize a few memorable events such as the year the baseball strike occurred and the World Series was cancelled, the first hearing-impaired Miss America was crowned, George Foreman won his last heavy-weight championship at the age of 44 or so, and the famous white Bronco chase with O.J. Simpson which millions of people viewed live on TV. If you were fitting hearing aids back in this year, 1994, you may remember back to the simplicity of the times. There were very few choices relative to today that we could offer our patients. Perhaps our most favorite instrument to program and fine tune hearing aids back then was the good ol' trusty miniature screwdriver. Most of us do not even have one anymore. This is what we used to use to fine tune a lot of our hearing aids back then, and also a lot less options to offer our patients. We did have custom products. CICs were a hot topic at the time in 1994. This is interesting as they may be re-emerging in popularity in certain pockets of the country again. BTEs did not take up quite as much of the market as they do today because they were relatively large in size. We also know that there were really no digital hearing aids on the market back in the early to mid-90s, and stylish, receiver-in the canal, open-fit products were non-existent
If we move the clock ahead 18 years, we know that there are a lot more choices that we offer our patients. I think most of us would agree that it is a good thing to offer our patients many choices. We can fit hearing loss more successfully. We can be more precise in our programming. We can offer choices for how the hearing aid connects with their cell phone. We can have the hearing aid connect with the TV. There are all sorts of interesting things with trainability, remotes, multiple adaptive features, etc. I think there is also a down side to have all these choices. We can literally flood our patients with too much information during the buying process, which generally happens during our initial pre-fitting evaluation. We know from research that when we offer a customer too many choices, their brain can literally become paralyzed and they cannot make a decision. I think this happens fairly routinely in the hearing aid world as we give our patients too many choices; they shut down, and cannot make a decision that day.
Buying Preferences Matrix
One way to avoid that issue of offering our patients too much information is to think about what I call a "buying habits" or "buying preference" matrix. When a patient comes in your door and you are conducting your initial evaluation with them, you want to try to fit the patient's buying preferences into one of four buckets. They are primarily going to make their decision around one of four things. One is cosmetics or something that looks attractive and is cosmetically appealing. Another is performance. For us, this is usually a solution that works very well in background noise. Third, they will make their decision around something that is simple and easy to use. Finally they will make a decision based primarily on price . What I like about this matrix approach is that it forces you to realize, and this is backed up by some good research outside the industry, that price is only the primary factor in about ¼ of all the patient's we see. The teaching point I want to make is that it is important to understand your patient is primarily going to make their decision based on one of those four items listed on the matrix, and it is our job to figure out which of these four items resonates the strongest with the patient. Once we make that determination, we can tailor our recommendation around it.
The COAT
There is a tool or questionnaire that we can use to help in this evaluation process which is the COAT, the Characteristics of Amplification Tool. This was created by Sandridge and Newman at Cleveland Clinic. in 2006. You can go to the Audiology Online website and enter the key word COAT. You will be able to download a copy of the COAT. The authors and the article that goes along with the COAT actually encourage you to modify it to your liking. There are some important questions that get at not only the motivation or the buying preferences of the patient, but also expectations and other important aspects of the patient's point of view regarding their hearing ability. Figure 1 is a modified version of the COAT that could be used clinically to gather buying preference as well some of these other important bits of patient information.
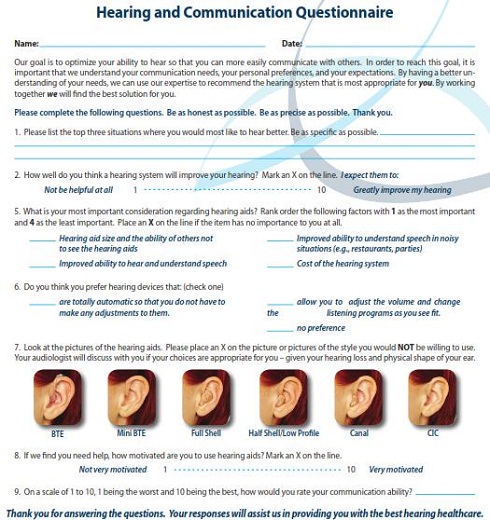
Figure 1. Modified version of the COAT that can be used to gather buying preference and other patient information. Click Here to View Larger View of Figure 1 (PDF)
Essential Patient Information
Once that information is gathered, there are three additional essential pieces of information that we have to get from the patient. These are communication needs of the patient, the extent of the problem (Audiological Evaluation), and the motivation/self-perception of the problem. If you are looking for a written source for what I will talk about next, in the most current issue of Audiology Today which was published about two weeks ago, I wrote an article that goes into more detail about the three pieces of information that need to be gathered. None of those things are a surprise as we were taught in graduate school to gather this information. An important point I would like to make is that it is not only what information you gather, but how you gather it. When you are differentiating your office, especially trying to differentiate from low-end retailers, direct to consumer and over the counter types of products, how you do things is paramount in the whole interaction process. It has to be captivating and interesting for the patient. There is nothing more mundane than a routine hearing test, if you put yourself in the patient's shoes. The more we can bring these things to life and make them interesting for the patient, the more valuable it becomes and the more we can differentiate our practice from direct-to-consumer products.
Communication Needs of the Patient
Here is some data from Kochkin. MELU stands for multiple-environment listening utility and it is a very intuitive concept. In Figure 2, you can see on the X-axis the number of listening situations satisfied and on the vertical or Y-axis, you have overall satisfaction expressed as a percentage. All of us who have been fitting hearing aids know intuitively that the more listening situations that we can improve with amplification, the more likely patients are to express overall satisfaction. Satisfaction is around 20% when patients are satisfied in one or two discrete listening situations. However, when we move up to 10 and 15 listening situations satisfied, overall patient satisfaction goes up to 80-90%. The message here is during the pre-fitting appointment it is important to get out on the table, evaluate, and have the patient self-rate 10 to 15 discrete individual listening situations that they encounter on a daily basis.
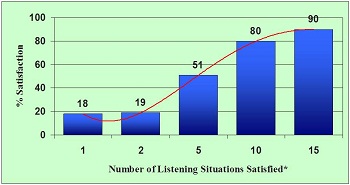
Figure 2. Chart demonstrating the impact of multiple-environment listening utility (MELU) on hearing aid satisfaction. As consumers are satisfied with their hearing aids in more listening situations, overall satisfaction increases. Modified from Kochkin et al., 2005.
Client Oriented Scale of Improvement (COSI)
One tool many people have used in the past and still use today is the Client Oriented Scale of Improvement (COSI). It is an open-ended measure that comes from the National Acoustic Laboratories in Australia (Dillon, James, & Ginis, 1997). You can specify up to 5 situations in order of significance, and use the tool to track the degree of change or improvement in those situations with the use of hearing aids. This is a nice tool that serves as a measure of outcome, both relative and absolute outcome with degree of change and final ability. It is open-ended and it only allows you to write in on one form 5 specific needs that can be prioritized. It is a good start, but remember, according to the MELU data that Kochkin collected, when we can help someone and satisfy their ability to hear in 10 to 15 situations that is when overall satisfaction gets over 80%.
TELEGRAM
Another tool that helps us get information about MELU, which I believe is better than the COSI, is the TELEGRAM (Thibodeau, 2004). TELEGRAM is an acronym. It stands for telephone, employment, legislation, entertainment, groups, recreation, alarms, and members of the family. For each of these categories, there are several subcategories. For example, under telephone, there are cell phone and land line subcategories. For employment, you have school or job, depending upon the person. It could also be both, if the person is working and going to school. Entertainment has the subcategories of TV and movies. Under groups, you have church, parties, and meetings. Under recreation, there are blank lines for you to fill in with anything that might be a recreational activity for the patient. Under alarms, you have smoke, doorbell and clock. Then under members of the family on the right side, you can choose from several situations where the patient is spending most of their time, what their living situation might be, and who they are communicating with on a daily basis.
The TELEGRAM uses a rating scale from 1 to 5, with 1 being no difficulty and 5 being great difficulty. It, like the COSI, has an open-ended spot to write in the three main problems that the patient is experiencing, and is a great way to prioritize them. It also goes one step further with a spot where you can write in some recommendations for assistive technology, telecoils, and maybe for managing the listening situations. This is a tool once completed for which you can send to the school or the referring physician, or send home with the family to provide them with more regimented information. The TELEGRAM enables you to sit down and have a conversation with the patient about some very ordinary occurrences, which could be very easy to gloss over during the initial evaluation. Imagine sitting down face-to-face with the patient before you have even put the ear phones and done a test and talking about situations where they are having difficulty across this whole spectrum of situations. You and the patient are working together to self-rate on a 1 to 5 scale how much difficulty they may be having in the unaided condition.
A good example is the telephone. Everyone talks on the telephone. More and more people talk on both a land line and a cell phone, regardless of their age or background. It is good to have a rating for both of those in the unaided condition. Also in older patients who want to live at home independently, you can discuss some various alarms that could be helpful. The TELEGRAM is a great way to assess communication need, not just need for a traditional hearing aid. It is a comprehensive approach that gets at trying to help someone in 10 to 15 unique listening situations.
Figure 3 shows a completed TELEGRAM with the three individually prioritized situations being at church, meetings at work, and the phone at work. The self-rating was also completed across the spectrum, with most scores being around 4 to 5 which is not very good. As you might guess, the results of this unaided TELEGRAM suggest there is a lot of potential to help this person.
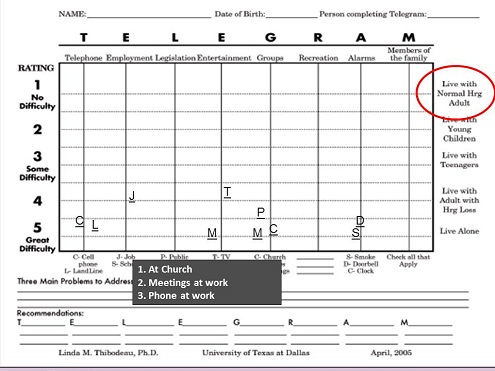
Figure 3. Completed TELEGRAM with the three individually prioritized situations being at church, meetings at work, and the phone at work, and most ratings in the 4 - 5 range, indicating the person is having difficulty in these situations.
Based on my experience I think it is important to complete the TELEGRAM before hearing is assessed. It is a natural conversational style and it gets at the fact that your primary goal is to help the patient communicate better, not just to evaluate their hearing. When it is done in a comprehensive manner, it takes no more than 10 to 20 minutes at the most to complete. You should try to get the patient to point out 10 to 15 individual situations. It is also important to involve the patient in the scoring. Most patients, based on my observation and my experience, understand and grasp the 1 to 5 concept. While you are doing this, you should be reminding the patient that you are going into a lot more detail than was expected about where they are having difficulty.
The TELEGRAM also serves as an outcome measure. By completing the TELEGRAM before and after a hearing aid fitting, you can measure the relative benefit across those different listening situations. As a rule of thumb, you would consider having the patient complete a TELEGRAM maybe 30, 45, or 60 days after the fitting to rescore those situations with their amplification. For example, if a patient's score for cell phone moved from a 4.5 pre-fitting to a 2 post-fitting, and for the land line they moved from a 4.5 to a 1, you would see there is quite a bit of improvement. Another rule of thumb is you should be getting about two and a half categories of improvement on average for all of those situations that you have rated. Kochkin last year (2011) published an article that indicated custom hearing aid solutions offer about 55% relative benefit. This equates to two and a half categories of improvement on a 1 to 5 scale. It is important to have a benchmark for judging the success of the fitting when you are using the TELEGRAM, or COSI which also employs a 1 to 5 scale. This data from Kochkin could serve as your benchmark.
Finding the Extent of the Problem
Finding the extent of the communication problem is another important component of the testing and recommendation phase of the patient journey. Of course, there are a number of tests you need to conduct when quantifying the extent of the problem. The one I want to focus on today is speech-in-noise tests. This is because speech-in-tests, I think, have the ability capture critical information in a memorable way for patients.
Speech-In-Noise tests. There is good research to support the fact that speech-in-noise tests should be done routinely during the pre-fitting evaluation. Speech-in-noise tests address the most common complaint of most of our patients, which is an inability to hear in background noise. It helps provide some realistic insight into what the most appropriate amplification strategies can be, and it also can help us counsel our patients throughout the process. As you may know or may learn, when someone's signal-to-noise ratio loss is quite high, we would counsel that patient far differently than someone who had near normal or normal signal-to-noise ratio loss. There are several tests these days that you can use to evaluate someone's ability to hear in noise. There are variable and adaptive type tests. There are single word tests, sentence length tests, tests that have broadband noise like the HINT (Nilsson, Soli, & Sullivan, 1994) and tests that have speech shaped noise like the QuickSIN (Killion, Niquette, Gudmundsen, Revit & Banerjee, 2004). I am a big proponent of the QuickSIN. I think it is very user-friendly. It takes about 5 minutes to do this test in the clinic. It is easy to score and it's reliable. Figure 4 is an example of the score sheet from the QuickSIN.
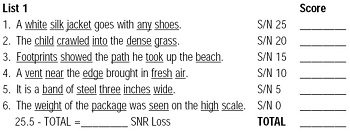
Figure 4. A sample scoring of a list of six sentences from the QuickSIN test.
You will test at 6 different signal-to-noise ratio levels, from +25, which is easy, to 0, which is very difficult. This test is administered in each ear under headphones at about 70 dB HL at a loud, but okay level. Then you count the number of words that the patient correctly repeats. You put those in the columns listed on the score sheet, add them up, and you get a score by taking the number of words repeated correctly and subtracting it from 25.5. The general guidelines are:
- SNR Loss = 0-2 dB (Normal Hearing)
Once audibility is restored, should do pretty well in most background noise situations
- SNR Loss = 3-6 dB (Mild SNR Loss)
With good directional hearing aids, should be okay for most situations with SNRs +5 dB or better
- SNR Loss = 7-12 dB (Moderate SNR Loss)
Even with good technology, will have problems in many noisy listening situations
- SNR Loss =>12 dB (Severe SNR Loss)
Strongly encourage use of FM system if listening in noise is important to patient Speech-in-noise tests are something that you want to gather on every patient to measure their intelligibility.
Acceptable noise level test. Another important component is to look at is annoyance. There is a test on the market now that looks at annoyance. This is the Acceptable Noise Level test. It has been around now for a while. Anna Nabelek, and her colleagues at the University of Tennessee developed this test (Nabelek, Tucker, & Letwoski, 1991). You can think of the ANL test as the MCL test with some background noise. We know from their research that the score on the Acceptable Noise Level (ANL) test is not related to age, gender, or hearing loss. We also know from their research that if someone has a low score, this tends to show the patient can accept greater amounts of background noise. If they have a high score on the ANL, their research suggests that patients are not likely going to wear their hearing aids on a full time basis. Accordingly to Nabelek et al. research, they can predict success as defined by use time with something like 83% accuracy. This is useful and interesting information. . You first obtain the MCL done on CD with a two-channel audiometer. You then introduce background noise. The biggest challenge with doing this test, which leads to the greatest amount of variability, is that instructions are a little challenging to give.. You are more or less telling the patient to tell you to stop turning up the background noise when they become so annoyed that they can no longer put up with it. Once you get the MCL and the BNL, you will subtract the BNL from the MCL and this gives you the Acceptable Noise Level score. If the score is less than 7 to 10, this is a sign that annoyance is not much of an issue. I do have to say that in the last year or so, there has been a couple of studies out that have been done independent of the University of Tennessee group that show there is more variability with re-test of the ANL than was first suggested by their research. I still think this is a good test because it involves the patient. It also tries to evaluate annoyance, which is an issue for many patients. I would be very cautious in the interpretation of the results however. We do not want to over-interpret the results, but if we see an ANL score of greater than 12 or 13, this would be a red flag for an annoyance issue we need to pay attention to. The test is distributed by Frye Electronics.
Red flag matrix. Next, I would like to discuss the Red Flag Matrix that I developed with Jill Bernstein, (2011) who is an audiologist in Buffalo, NY. It was developed to help precisely identify patients who might be considered at-risk for struggling with speech intelligibility in noise or annoyance from sound prior to receiving hearing aids., Using this tool, you take the results of two tests that we should be routinely conducting during the pre-fit, the QuickSIN and the ANL, and plot their results as a single point on a matrix. Using the normative data from these tests, the matrix is divided into four quadrants. Depending upon which quadrant the patient's data point is in will indicate if there are red flags or the patient may be at risk for issues that could impact hearing aid success.
Figure 5 shows the Red Flag Matrix. On the X-axis (horizontal), from 0 to beyond 15 is the QuickSIN score. It will be plotted on a 0 to 15 or beyond horizontal axis. On the Y-axis (vertical), we have the ANL score. You can have a negative score on the ANL, but typically it will be around 0 to 7. You will notice that the scale vertically for ANL goes from -5 to around 15. These two lines, the QuickSIN horizontally and the ANL vertically, intersect at about 7. This is done deliberately. On the QuickSIN, if the score or SNR is greater than 7, this is a moderate SNR loss. These are the people who may need a little more help or more counseling on the use of noise reduction technology in every day listening than what convention directional microphone technology can provide If you also look at the ANL score, if the score is less than 7, in the research that Nabelek's group performed, this was a pretty strong indicator that they would be full-time hearing aid users. For these reasons we put the intersection line at 7.
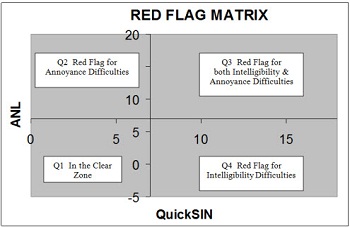
Figure 5. The Four Quadrants of the Red Flag Matrix
You can see from the Figure, that quadrant 1 in the lower left is the "in the clear" zone. The "in the clear" zone is someone who has a normal or near normal score for both tests. For example, a patient who has a QuickSIN of 4, which is a mild SNR loss, and an ANL of 2, which indicates that this person is not annoyed by sounds, falls in the "in the clear" zone. A patient with a high ANL score of 13, but a low QuickSIN of 2 would fall in quadrant 2, the zone for a red flag for annoyance. The Red Flag indicates that this person may be annoyed more than the average hearing aid user by background noise. The important point is that it is good to know who those patients are before you fit them with hearing aids. They are certainly still candidates for amplification and for our services, but we are sharing the information that they are at-risk for having an annoyance problem before we fit them. They may not have an annoyance problem, but you now have one data point that shows they are at-risk, and can approach the fitting and management of this patient accordingly.
A patient whose data point falls in quadrant 4 indicates they are at risk or there is a red flag for problems with intelligibility in background noise. Such a person has no difficulty with annoyance in the pre-fitting test, but they have a significant red flag for intelligibility and noise problems. You will want to share your finding with them and let them know they are at-risk for struggling in background noise even with amplification. You may have to do some things differently in order to make them a successful user.
Quadrant 3 in the upper right indicates a red flag for both annoyance and intelligibility problems. Jill and I published an article on AudiologyOnline (Taylor & Bernstein, 2011) showing the Red Flag Matrix results of 24 hearing aid users. We showed a fairly wide distribution of the data. We put together the Red Flag Matrix as a counseling tool. If someone falls into quadrant 1, they have a tendency to be very accepting of amplification. There are no red flags. However, whenever you get into these other quadrants, or the higher the scores, you get into where acceptance might become more of an issue. The Red Flag Matrix is designed to help clinicians more precisely counsel patients on some potential challenges prior to the actual fitting.
Motivation and Self-Perception of the Problem
Let's look at one final piece of information we should be gathering at this stage of the patient journey. It is quantifying the patient's perception of a hearing problem. I found an interesting article that show how the answer to one question can provide powerful, data-driven insights into how the pre-fitting appointment may unfold. It was published by Palmer, Solodar, Hurley, Byrne, and Williams in 2009 in the Journal of the American Academy of Audiology. This article has a few factors that make it very clinically useful. It has a very high sample size of 800 subjects. Also most of the data was collected in an actual commercial environment. It was not a university clinic or government hospital. If I am not mistaken their data was collected in a place where people were paying out of pocket for the majority of their services. The question they asked to evaluate self-perception of the problem was, "On a scale of 1 to 10, 1 being the worst and 10 being the best, how would you rate your overall hearing ability?" This question was asked to everyone during the pre-fitting process and then the results were charted as a function of the pure-tone average and the individuals that received hearing aids
There is a lot of data available in Figure 6. On the horizontal axis of this graph you have self-rating from worst which was 1 all the way to a 10 which was best. On the left vertical axis, you have the percentage of individuals that purchased or did not purchase. On the right vertical axis, you have the pure-tone average. The dotted line indicates the percentage of patients across the spectrum on the 1 to 10 rating that purchased hearing aids. The solid dark line is the percentage of patients who did not purchase hearing aids. We will focus on the dotted line to keep this simple. The pure-tone averages are also shown with gray blocks with the mean and the standard deviation which is probably + or - 2 standard deviations. As you would expect, as the self-rating becomes higher or better, hearing loss becomes less severe. For example, with a rating of 10, the pure-tone average was less than 20 on average, and with a rating of 1 or 2, the pure-tone average was over 60.
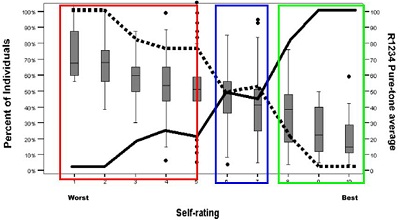
Figure 6. Data from Palmer et al. (2009) adapted into three buckets of information. The dotted line indicates the percentage of patients that received hearing aids. The solid dark line is the percentage of patients who did not receive hearing aids.
To this, I have put the data in three different colored "buckets of information." The people who scored themselves between 1 and 5 were 80% or more likely to purchase hearing aids. As you notice at 9 and 10, almost no one purchased hearing aids. About 20% of those that self-rated an 8 received hearing aids.
The group in the middle, scores between 6 and 7, received hearing aids about 50% of the time. (See blue bucket.) This middle bucket is there we should be focusing our attention. These are patients who are not motivated enough, or do not notice enough of a problem to get help -even though they have a fairly significant hearing loss. Based on their findings of this one study, I would suggest treating this group differently than patients who fall into one of the other two buckets. These patients should be treated differently. There is very little difference in hearing thresholds between those rating themselves at 4 or 5, compared to patients who rate themselves at a 6 or 7. If they rated themselves a 4 or 5, they were 80% likely to purchase a hearing aids that day. If they rated themselves a 6, they had about the same amount of hearing loss on the audiogram, but there was only a 50% chance that they were going to purchase. This really gives us some actionable information that we can use clinically. Imagine yourself asking this question routinely during the pre-fit, and if someone gives you an answer of a 6 or a 7, you will probably treat that patient a little differently than someone who answers with a 1 to 5 Bucket 1 has patients who self-rate on that question between an 8 and 10. A response of 8 to 10 changes the entire tenor of the conversation. It will become a more educational opportunity. You are going to add this patient to your patient recall list. You will want to provide them with annual testing. . You will want them to become a promoter of your practice. If you are using Facebook and other social media, you want to make sure that they 'like' your Facebook page to get information from you rather than a competitor. However you will not spend a lot of time trying to convince these patients that they need hearing aids. Even if their audiogram would suggest it, they are not ready yet for them.
In Bucket 3, you will move right into the hearing aid selection process and get into the important details of performance, lifestyle, cosmetics, and cost. There is no reason to spend a long time trying to convince these patients as they are already motivated.
I am a big believer that this question has incredible clinic utility. I think it helps us streamline the process, identify the patients more quickly of who might be on the fence, and spend more time trying to create some urgency around them getting help today, rather than waiting. For example, you may decide that you want to conduct a hearing aid demonstration for every patient who falls in the 6-7 bucket.
My Challenge to You
Here is my challenge to you. It is important for us to modernize our clinical protocol using some of the tools and techniques I discussed today. One of the two main criteria for any new addition to your protocol needs to be some evidence or research around why this tool is important. For example, with speech-in-noise testing and why we should do this routinely, there are probably a dozen or more articles that show this test measures something different than what speech audiometry in quiet and pure-tones do. I am thinking mainly of the research that Rachel McArdle and Richard Wilson (2005) have done. At the same time, just as importantly in today's era of uncertainty and direct-to-consumer over-the-counter devices, if we want to be different, we need to create a memorable and meaningful patient experience. Pure-tones and single words have no meaning to the patient and it is up to us to bring some of these other tools to life in our practices.
Make a Recommendation
Lastly I want to discuss the importance of making a recommendation. What happens when the patient leaves our test booth and we are in process of discussing test results and making a recommendation? If you look at some of the anecdotal reports and a little bit of research in this area, quantitative research, it is important that we do not give our patients too many options.
In the article that I published with Drs. Amlani and Weinberg (Amlani, Taylor, and Weinberg, 2011), we looked at the issue of unbundling or itemizing features and benefits. . I want to share this with you because I think it will give some good information on how you might want to position products and prices to our patients. In this study, we had three different groups of 40 retired adults in each group. Half of the group was experienced with hearing aids, and the other half were new hearing aid users. The three groups were given ads, which can be seen in Figure 7.

Figure 7. Advertisements shown to respondents in Amlani, Taylor & Weinberg (2011) study.
The first ad, shown to one group only, had very little information about the product being advertised. The second group was shown an ad that was very techno-centric. The third ad showed real world potential benefits and not features to its group. Each group was informed that the average price per unit was $2,000. They were shown in an itemized and non-itemized format. Then they were asked to provide the maximum price that they would pay. In Figure 8, you can see the data collected, and in the interest of time I encourage you to read this article.
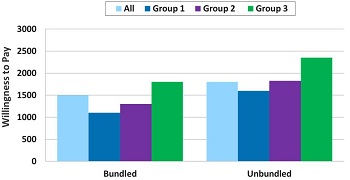
Figure 8. Willingness-to-pay results by group for the same hearing aid presented in a bundled and unbundled pricing model. Adapted from Amlani, Taylor & Weinberg, 2011.
In Figure 9, you can see the willingness-to-pay by group. The first thing you will notice is that when we itemized or unbundled the features and the benefits for all three groups, their willingness to pay increased by a few hundred dollars. This suggests that when you are positioning your recommendation and show the patient in an itemized way the different things you get as part of the price, patients are probably seeing more value and are willing to pay a little bit more. This was definitely the case with the inexperienced users.

Figure 9. Willingness-to-pay results by hearing aid experience (blue = experienced; green = inexperienced) for the same hearing aid presented in a bundled and unbundled pricing model. Adapted from Amlani, Taylor & Weinberg, 2011.
This study suggests that when you itemize or unbundle features during your presentation to the patient, it leads to a higher average selling price. This is proabably because patients can actually see what the value is for the different components of your offering. We also noticed that for new patients, who were not as familiar with technology, unbundling of services (rather than product features) was important. The data would indicate that inexperienced users were willing to pay more for the services. Examples of these services are the 2-yr warranty, X number of batteries, or unlimited office visits for a period of time. Your testing and dispensing fees can also be itemized. We also noticed that experienced patients focus more on the unbundling or itemization of technology features. When you unbundle, or itemize the features such as better hearing in background noise or feedback canceller, our data would suggest that experienced hearing aid users may understand what this means and are willing to pay more for it.
A few other things you can extrapolate from our work, and also supported by what Carol Rogin of HIA (2009), is patients like it when you offer them a single option at a single price. Offering them too many choices has a tendency to paralyze their decision-making process, which may result in someone needing to think it over and not purchase hearing aids. I think there is still a lot we need to learn about bundling and unbundling services. Perhaps the one nugget of wisdom from the study I did with Dr. Amlani is that clinicians can add value and drive average selling price when they unbundle or itemize certain key product and service benefits.
Summary
In the face of economic uncertainty, disruptive innovations and changing buying behaviors of healthy agers, we need to strive to modernize. Modernizing of clinical processes, marketing plans and patient interactions is the key to immunizing your practice from these forces. We do this by, what I call a better design of the patient experience. As I have mentioned, it is not easy to change habits that we may have learned 20 or more years ago, but this is how modernization occurs, by fundamentally changing some of our behaviors as we interact with the patient. More detail of what I have discussed can be found in my books, Fitting and Dispensing Hear Aids and Consultative Selling Skills for Audiologists.
Questions and Answers
You mentioned that the ANL was available through Frye and the COAT is on Audiology Online, what about the TELEGRAM?
The TELEGRAM was created by Linda Thibodeau who is a PhD audiologist at the University of Texas - Dallas, the Callier Center. It is not under Copyright restrictions. If you want the official version of the TELEGRAM you could reach out to Dr. Thibodeau in Texas. If you want to email me, I can find her email for you. I also have some copies of the TELEGRAM that I would be willing to share with people if they are interested.
Supplemental Links
Frye Electronics - www.frye.com
References
Amlani, A., Taylor, B., & Weinberg, T. (2011). Increasing hearing aid adoption rates through value-based advertising and price unbundling. Hearing Review, 18(13), 10, 12, 16-17.
Bennett, A. & O'Reilly, A. (2010). Consumed: Rethinking business in the era of mindful spending. New York, NY. Palgrave MacMillan.
Dillon,H., James, A., & Ginis, J. (1997). Client Oriented Scale of Improvement (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids.
Harvey, M. (2003). Audiology and motivational interviewing: A psychologist's perspective. AudiologyOnline, Article #459. Retrieved from: /articles/audiology-and-motivational-interviewing-psychologist-1119
Killion, M.C., Niquette, P.A., Gudmundsen, G.I.2G Revit, L.J., Banerjee, S. (2004). Development of a quick speech-in-noise test for measuring signal-to-noise ratio loss in normal hearing and hearing impaired listeners. Journal of the Acoustical Society of America, 116(4), 2395-2405.
Kochkin, S. (2010). MarkeTrak VIII: Consumer satisfaction with hearing aids is slowly increasing. Hearing Journal, 63(1), 19 - 20,22,24,26,28,30-32.
Kochkin, S., Beck, D.L., Christensen, L.A., Compton-Conley, C., Kricos, P.B., et al. (2010). MarkeTrak VIII: The impact of the hearing healthcare professional on hearing aid user success. Hearing Review, 17(4), 12 - 34.
MacFarquhar, L. (2012) When Giants Fail.
Nabelek, A., Tucker, F., & Letowski, T. (1991). Toleration of background noises: Relationship with patterns of hearing aid use by elderly persons. Journal of Speech and Hearing Research, 34, 679-685.
Nilsson, M., Soli, S., & Sullivan, J. (1994). Development of the hearing in noise test for the measurement of speech reception thresholds in quiet and in noise. Journal of the Acoustical Society of America, 95(2), 1085-99.
Palmer, C., Solodar, H., Hurley, W., Byrne, D., & Williams, K. (2009) Self-perception of hearing ability as a strong predictor of hearing aid purchase. Journal of the American Academy of Audiology, 20(6), 341-347(7).
Rogin, C. (2009). Top 10 reasons for hearing aid delight. AudiologyOnline Recorded Course #14615. Retrieved on April 1, 2011 from the eLearning Library on www.audiologyonline.com
Sandridge, S, & Newman, C. (2006, April 6). Improving the efficiency and accountability of the hearing aid selection process. Audiology Online, Article 1541. Retrieved August 16, 2006 from the Articles Archive on www.audiologyonline.com. Direct access URL located at: www.audiologyonline.com/articles/article_detail.asp?article_id=1541
Thibodeau, L. (2004) Maximizing communication via hearing assistance technology. Plotting beyond the audiogram to the TELEGRAM, a new assessment tool. Special Issue: Assistive Listening Devices. Hearing Journal. 57(11), 46-51.
Taylor, B. (2011). Consultative selling skills for audiologists. San Diego, CA. Plural Publishing.
Taylor, B., & Bernstein, J. (2011). The red flag matrix hearing aid counseling tool. AudiologyOnline, Article #2380. Retrieved from: /articles/red-flag-matrix-hearing-aid-816
Taylor, B. & Mueller, G. (2011). Fitting and dispensing hearing aids. San Diego, CA. Plural Publishing.
Wilson, R. & McArdle, R. (2005). Speech signals used to evaluate functional status of the auditory system. Journal of Rehabilitation Research & Development, 42(4), 79-94.