Learning Objectives
- Participants will be able to describe some of the key needs and challenges of parents of children fitted with cochlear implants.
- Participants will be able to list concrete steps to make the journey of children fitted with cochlear implants and their families more family centered.
- Participants will be able to describe how to apply the My Turn to Talk tool with parents and use their input to ensure that important needs are met.
Introduction and Overview
Today I will discuss journey that the Ida Institute undertook about a year ago to explore the successes, gaps, and challenges in the rehabilitation of children fitted with cochlear implants (CIs). We wanted to understand this journey better and to find out how it is experienced by parents, children, and professionals.
This topic aligned very well with the Ida Institute's mission, which is to foster a better understanding of the human aspects of hearing loss. If you're not familiar with the Ida Institute, we are a non-profit organization established in 2007 with a grant from the Oticon Foundation, and we have been funded by the foundation ever since. We work with a network of over 10,000 hearing care professionals worldwide to achieve our mission, and we do this by developing tools and assets that can help foster person-centered practices in audiology, and improve the outcomes for patients every day.
Some of the topics we've looked at in the recent past include patient motivation, living well with hearing loss, how to include communication partners in rehabilitation, and how to use telehealth effectively in audiological practice. I invite you to visit our website to explore the tools and other resources available. Everything we develop with our network is created in collaboration with hearing care professionals around the world and it is available free of charge. All you need to do is register on the website and you have access to everything.
Today's topic is cochlear implantation and rehabilitation. This is one area we've recently begun to address, to explore how we can foster patient-centered practices in relation to the treatment of patients with cochlear implants.
As you may already know, cochlear implants have been rated the most successful medical prosthesis within medicine to date, based on the fact that there is less than a 0.2% rejection rate. Worldwide, there have been 250,000 cochlear implants fitted, and this trend is projected to increase. We also know from research that many children fitted with cochlear implants are able to be mainstreamed, and that many have quite remarkable outcomes in terms of speech and language, although results can be variable.
However, being fitted with a cochlear implant is only the beginning of a journey that lasts a lifetime. For families of children diagnosed with hearing loss, the journey that begins with a newborn hearing screening carries through years of rehabilitation, speech and language therapy, and decision-making on education options, hearing technologies, and much more.
Today, I will share with you what we've learned about this journey in a seminar that was hosted by the Ida Institute in 2015. The reason the Ida Institute is interested in this topic is that even though there are well-established clinical pathways and protocols for the CI patient journey in many countries, we as a person-centered institute were curious to explore what could be done to further improve the experience of children and families in dealing with cochlear implants.
The Seminar
Make the Normal Happen
The focus of the seminar was first, to explore the needs, successes, and challenges in cochlear implant rehabilitation today. We wanted to understand the critical gaps in the CI patient journey. Above all, we wanted to identify what is needed to “make the normal happen.” “Make the normal happen” is a phrase we've become quite fond of here at the Ida Institute. It was coined by Margret Tate at the Ear Foundation in 1987. We think it expresses our mission quite well: to help children with hearing loss have the same choices and the same opportunities in life as all other children.
With 21 seminar participants from 14 countries, we set out to explore these topics. Our participants all worked at different capacities within the cochlear implant area. There were audiologists, speech and language therapists, ENTs, surgeons and even psychologists. With them, we addressed these important questions over two days in a highly interactive and very creative innovation process. We listened to their experiences with the CI journey in their respective countries, and we facilitated sessions in which they were asked to collaborate with each other to identify what is needed to create the ideal patient journey for children with CIs and their families. The process we used is a typical Ida Institute innovation process, comprised of three parts: understand, explore, and create.
Understand
Using a broad approach, we first set out to begin to understand the challenges that are faced during the CI process. These include both challenges faced by professionals when they work with children who are being fitted with cochlear implants and with their families, and also challenges faced by these children and their families. It was a two-pronged approach to begin to understand the broader consequences and the broader nature of the journey. We were looking to obtain a global perspective, to collaborate with professionals from around the world, and to benefit from the different perspectives that they were able to bring to the process.
Explore
Secondly, we set out to explore the journey and the way it looks in all of these different countries today. We quickly learned that that there are some differences, because we were talking to people from very different parts of the world. However, we soon realized that there were more commonalities than differences, and that there were many similarities in the way that the journey is carried out in their respective countries.
Create
We also set out to build on success and take an appreciative approach to our process to see what works well now, rather than focus on what is not working. Next, our goal was co-create ideas for how we can address the needs that were uncovered and identified in our discussions. Based on everything we had seen, heard and discussed over the two days, seminar participants generated concrete ideas for tools that we could develop to help fill some of the gaps that we identified.
Understanding Family Needs
One of the things we set out to do was to understand the needs of each family. What was the family's experience like? We don't always hear that when they come to the clinics because we have a set process. We have clinical procedures we need them to complete. Lots of things are happening in the patient journey, and we didn't always feel we'd heard enough about it directly from the parents and the families.
Insights into Family Experiences
One way we set out to learn about these needs and experiences was through interviews conducted by the Ida Institute in-house anthropologist. At the Ida Institute, we work extensively with ethnographic videos that document various aspects of living with hearing loss and the interaction between patients and professionals. The purpose of these videos is to increase our understanding of patients’ and professionals’ challenges, and to learn what we can do to foster more person-centered practices in daily interactions.
In these interviews, the parents share what has been helpful and what has been difficult to them, from the early diagnosis, through surgery, and into rehabilitation. These videos, as all other ethnographic videos that Ida develops, are also freely accessed on our website in our video library, and you are welcome to view them.
I would like to share one of these videos with you. We're going to meet Kate and her parents in South Africa. Kate is six years old and she was fitted with a cochlear implant at birth. As you watch it, I encourage you to think about, "What are the needs that you can uncover on this journey? What are the needs of the parents? What are the needs of Kate, the child? What could perhaps have been the needs of the professionals who worked with this family?"
![]()
Transcript of Video: What's that? Kate my baby? Yeah. Baby girl!
Kate is six years old so she was born in 2008 and I had an absolutely normal pregnancy. There was no indication at all that she'd be born with a disability like hearing loss.
They said it out of the blue. They said, "Sorry, your daughter's got no hearing." There has to be a mistake. You can't be serious. This is a joke. Yeah, it left us it felt like we'd been hit by a train that afternoon and we just came back and we just cried for two days.
Yeah, and we were running around the kitchen just getting all the pots and pans out the cupboards and just banging them behind her in complete denial just wanting her to move to the sound of the loud noises, but that didn't happen.
It's like, "Can we get a second opinion? We'll go somewhere else. We'll go to someone who knows what they're doing. These people obviously don't know what they're doing. They were quite abrupt."
Before Kate had her cochlear implants, I was involved in cochlear implantation helping the surgeon. I'm an anesthetist. I was doing the anesthetics for the cochlear implants and it was interesting because you learned about the technical side of things. It's an expensive device and it's difficult to insert, and it takes a long time, and you've got the whole anesthetic aspect of performing a cochlear implant which is my area of expertise.
You'd take the child to theater. You would anesthetize the child. You'd make sure the child's not in pain afterwards and then you'd visit them maybe once or twice after the operation and the child would go home. That'd be it and you'd think, "This is something marvelous we've done."
That was until Kate was born deaf, which came out of the blue. At that point, I know had the other side of things and what the parents were going through. After having done this for six years. Kate's now six. I realized that medical personnel across the board everywhere. Audiologists, physiotherapists, occupational therapists have no concept of what you're changing by giving a child hearing.
You're changing not just their lives. You're changing the life of everyone they come into contact with. You don't understand the time, the effort, the expense, the stress that families go into to get to that point where they are sitting by the bedside waiting for their child's operation. It's a long passage.
It's difficult to give someone that sort of empathy unless they have been through it themselves. I was lucky because I had first the experience before Kate was implanted where I had as much empathy as I thought was necessary.
To think that she could have been trapped in her body, there that just freaks me out. Just to look at this miracle and what it's done, it's just incredible.
Kate: I used to do lots of fashion shows, but now I don't anymore. I did one last one, which was a long time ago. Not such a long time ago, but yeah. It was all fine. I had a singing part, which was at the very end and I wore a dress. Pink at the bottom. It's a pink down thing. It's almost to my feet and a white thing here. Silver belt. White and pink bows here. Straps, short-sleeved straps. Very short.
What are you talking about, darling?
The fashion show.
Oh, the fashion show.
So you sang as well?
Yeah.
Where did you sing?
I sang a song about being brave because the theme was being brave.
Oh, okay.
Being brave about telling people about your cochlear implants.
Do you want to sing it to her?
Yes.
Sing it then.
Impromptu.
Let's hear it.
Sing it.
You can just sing the one verse. Can you remember how it goes?
No.
No, of course you can. Come on, “you can be amazing…”Come on.
Oh, yeah. “You can be amazing; you can turn a phrase into a weapon or a drug. You can be the outcast, you can be the backlash of somebody's lack of love, or you can start speaking up.”
We've walked and worked a very long road to get her to this point. From there on you've got now ...
Access.
Access to sound, but that's where the hard work starts.
Vera used to sit down on the floor with the exercises from Carol du Toit every single day for six or seven hours a day going through repetition. Sounds. "What's this sound?" You lift up the cup, it's like, "Kate, I'm lifting up the cup. Look, the cup is pink. The cup is round. The cup has tea inside. We're going to take a sip of the cup. Look, Kate, I'm taking a sip."
"Listen to the sound that the tea makes when you swallow."
"The tea pouring in. Let's go and make another cup of tea. Look, I'm switching on the kettle. I take the kettle off. I fill the kettle up with water. Put the kettle back," just talking your whole day every day for years.
It paid off. Honestly, if there is one bit of advice I can give any parent out there is just to do it. You've got to sacrifice and put aside 18 months or 2 years of your life just to invest all those activities, and exercises, and time into your child because you can't go back and have it again. You can never redo that.
As parents, you feed off the feedback from the audiologists. They're the people that are able to tell you how you are doing as parents and you want to know that you are doing well in trying to raise a child with a hearing disability in the way that is best.
Has any one of your friends in your class said anything to you nasty about your ears? Never?
No, not about my ears. Never about my ears.
Okay.
Have they said anything nasty?
That's okay. That's one other conversation.
To summarize it from an audiological perspective, yes, audiologists are highly skilled, highly trained people that deal with hearing, but in this sort of situation where it's not just hearing, it's a whole life, there need to be far more empathetic and far more psychologists to the parents than just a pure audiologist.
It's so important because the audiologist is the one person, your contact in a world that you know nothing about. Now they have been in audiology and looking after people with hearing impairment and hearing loss for a very long time, but you as a family are suddenly thrown in the deep end and you have no idea what to do. You don't know where to go. You don't know where to turn to.
You don't know what's right, what's wrong, what you should be doing, and the audiologist is there as a guide. As your advocate in a hearing impaired world and they need to understand you as parents. They need to understand that your psychology as well and what makes you tick, and be there as an encourager not only doing the right thing with the daughter, but so much of the outcome depends on the parental input and that's where the audiologist is absolutely critical. To make sure that the parents are together in the process and that she understands the parents, not just what the actual technical difficulties are with the child's hearing. End of video transcript.
Parents’ Needs
What we can learn about the needs that Kate's parents experienced on their daughter's journey, and how some of these needs were met? As evidenced by this video, Kate's journey has had a positive outcome: she's hearing and communicating very well now at the age of six. However, when we listen to the parents' story, we can hear that there have been difficult times as well.
For example, they repeatedly mentioned that more empathy and understanding from professionals would have made their journey easier. They felt the way the message about Kate's deafness was conveyed was quite abrupt. This prompted them to request a second opinion because they didn't trust the diagnosis they received. The fact that they went home crying and trying to disprove Kate's deafness shows that some professional intervention in managing grief might also have been helpful.
They also mentioned that they needed hearing care professionals to be their mentors and guides on this journey into the unknown world of hearing loss. Kate's father (who interestingly used to be an anesthetist helping surgeons with cochlear implants) urges hearing care professionals to move beyond technical support and be advocates, guides, and even psychologists to the parents. It would have been helpful for them to have had someone who understands the CI journey, and the stress in which parents find themselves at critical times, such as just before or after surgery.
Finally, I think their comment about feedback is an important one was well. We heard from Kate's parents, but also from other parents who we've spoken to, that the hearing care professional (HCP) is their main source of hope and confidence. The HCP is the only one who can give qualified feedback on how the child is doing. The feedback professionals give is taken very seriously by parents, and we need to keep that in mind as we work to guide and support them.
Patients’ Needs
We're going to look at Kate's needs: what they have been on the journey so far and how they have been met. I think we can agree that she's clearly benefited from her early intervention. As we know from research, the earlier the fitting occurs, the greater the chance of success. A cochlear implant cannot do the job alone. Kate was lucky to have parents who are able and willing to put a lot of time and effort into her rehabilitation right from the beginning, despite the associated personal and financial costs.
This has given Kate the ability, the confidence, and the self-advocacy we see her display in the video. It's also the result of having a competent professional team working with her parents to identify the rehabilitation that was right for Kate. Her next most important need would probably be to navigate in the mainstream school environment, and also learning to ask for the support she needs when she needs it.
Professionals’ Needs
Finally, what do the hearing care professionals need to be able to meet the needs of parents and patients? If we think about it in relation to the video, Kate's father made an interesting comment when he said that as an anesthetist who used to work with cochlear implant patients before Kate was born, he had just as much empathy as he thought was necessary. "How much empathy is necessary?" you could ask.
I'm quite convinced he had clearly thought about the fact that he needed to show empathy and I have no doubt that he also wanted to show empathy. However, it seems that he developed what we might call a “professional” kind of empathy that he felt to be suitable, adequate, and perhaps above all, practical, allowing him to fit in all his tasks in a busy work day while also paying attention to patient needs.
It was quite an eye-opening experience for him to be at the receiving end of treatment as Kate’s father. What can this experience teach us about better meeting the needs of patients and parents? Perhaps it's a question of being genuinely curious and taking the time to listen. Every patient, indeed every family, is different, and there are many cues in what parents tell us that can help identify their unique challenges and how we can best help address them. It might also be helpful to rethink our role as professionals and take a more holistic approach to care, where we think of ourselves not only as medical experts, but also as guides and mentors beyond the four walls of the clinic.
A Framework Approach to Family Care
We had several experts present to us during the seminar. The insights I would like to share with you now are based on the research done by Christine Yoshinaga-Itano, who is a professor at the University of Colorado Boulder, and works closely with the Marion Downs Center in Denver. She's also a longstanding member of the Ida community and a member of the Ida Institute Advisory Board. At our seminar, she gave an excellent presentation on the family types of decision-making models.
Understanding Family Dynamics and Needs
In this presentation, Dr. Yoshinaga-Itano talked about how we can improve the quality of our support to families by acknowledging that families are different and have different needs, and by understanding their underlying structures and parents’ reactions.
I'll show you a short excerpt of her presentation. You are also welcome to look at the presentation in its entirety on the Ida Institute website.
![]()
Transcript of Video: We have a counselling guide that we use with our professionals. I would talk about the primary processes and the secondary processes of families and the primary processes are all the emotional parts. I can't in 20 minutes talk to you about the whole model, but I've just picked out parts of the training that we do. We actually do quite a bit of training on the first contact and how the professional joins the family.
In other words, how can you tell whether you are connecting with the family? Whether you are communicating with the family. Whether they're comfortable with you, they're accepting of what you have to say. Whether you have a communication that's actually occurring. We look at different aspects like family involvement and how involved the family is capable of being in the intervention and what our role is in figuring out if they're not involved, what is going wrong. What's interfering with their ability to become involved in what we're doing?
We talk about their family system. That's how they communicate with one another. How they make decisions. Every family unit is completely different. Sometimes it's a single parent who's a teenage mom. Sometimes it's a generational family with grandparents, and aunts and uncles, and cousins, and they actually live in a housing area where the responsibility for raising that child is the responsibility of the entire family or it's a community responsibility. It's a communal responsibility like say even in Europe or Denmark where you have daycare centers where they are actually an assistance to the family in raising their children.
We talk about how parents bond with their children and how they react to crisis. Whether or not they are bonding in what we would call a healthy bond or whether they're detaching because of the pain of the fact that they have a child with a hearing disability, or whether they're going the opposite way and they're doing an enmeshment, where they're actually the helicopter parents, where you can no longer separate out the parent from the child. Every family in crisis moves in a different direction and trying to figure out which direction they've gone into and how to help them back into healthy relationships is really the responsibility of the professionals who work with them.
We talk about grief resolution and how you can help parents adapt to the diagnosis of deafness, where they are in the process of grief resolution, and this gets you through this particular model. End of Video.
I think Dr. Yoshinaga-Itano touches on some very central things in regards to how we meet and work with families. When we look at the family as the care system surrounding the child, some patterns begin to emerge. I would like to invite you to reflect on how you work with those patterns in your daily work.
The things that stood out the most for me were first of all, how do we join the family? Are we connecting with them? Are they involved? If not, why is that? Also, how is the family communicating with each other, and with us, and with the child? How are they making decisions about everything? That will likely also impact the way they make decisions about their child's hearing loss. How do they react to crisis? Also, how do they handle grief?
Let’s think about the video of Kate and her family. Perhaps it would have been helpful if we had asked them at the beginning how they were connecting with the diagnosing audiologist. Clearly, they were not connecting very well, because they decided seek a second opinion. Also, how did they react to the crisis and handle the grief? Again, perhaps not so well. Banging pots and pans and crying is quite understandable. This is not a criticism in any way, but an observation that these are questions and signs we need to look out for as we deal with new families.
Elements of an Ideal Patient Journey
Based on the insights we collected through video interviews, with feedback from parents and also through medical presentations such as Christine's, we asked some of our participants to share what the cochlear implant journey looked like in their countries and from their place in the child's journey. Then we asked them to work together across countries and cultures to define key elements of what they would consider the ideal patient journey.
Because the group was so diverse, I did include some suggestions not only for the early phase (diagnosis, surgery, and switch-on), but also coping strategies for later on in the child's rehabilitation. Although these professionals came from very different countries and regions around the world, they quickly agreed on some essential qualities that they believed were crucial to an ideal patient journey.
I would now like to share with you some of the key elements they highlighted. As you listen, please think any other components you believe would be absolutely key to an ideal patient journey.
![]()
Video Transcript: In a dream world, there would be a 24-hour hotline for our patients to contact somebody at any time of the day or night to ask that question that they're thinking about. It's important to communicate even before any amplification is fitted, making sure that the parents are encouraged to continue singing and using motherese that we were talking about earlier.
You spoke about classroom support to the staff, so some of her kids are going to mainstream and depending on the school where they're going, these teachers need to work with the kids, so you really need to make sure that the teachers know what they're getting. So some structured support in terms of that?
We talked about how in our different countries we don't necessarily call it the same thing. In the US, we call it the 1-3-6 Rule where you try to identify the child's hearing loss and diagnose it by the first month you start the child, get them into some kind of intervention program by month three and then start that intervention by month six. We all had variants of that and that's part of the informational side to make sure that all of that's working properly. It can happen in different ways. We have parent-to-parent programs, our web-based, print material, whatever ensuring that the rehab is linked to the mapping and the medical side so it's a back and forth kind of relationship. Ensuring that it's family-centered and child-centered. Ensuring that the school part of this is working properly and everyone at the school is informed about what the child's needs are.
Working with the children at the school as well as with the teachers. Sometimes we forget the peer part of it. Ensuring that we bring the child's peers into the picture. Their friends, the neighborhood, et cetera. Empowering the child little by little to feel like they can talk about their hearing loss and what they need so that when they go out into the world they can take care of themselves. They can tell people what they need and know what it is that they need.
We had a discussion about the importance of developing that parent/child bonding at the front end before implementing the habilitation, so positioning the parent so they are with their child first before the hearing loss; the early support to the parents we had a discussion about how to connect with the parent. How to decide what would be appropriate for a family. We had talked about being able to find out from the family, "What do you need?"
One of our questions to a family could be, "What's your response to change in your life?" because that will often give an indication of how you will approach the change of this child with hearing loss. How do you learn? What's your best way to learn? Is it easier for you to read articles or is it better for you to talk to another parent? Is it better for you to see a diagram? What's the modalities that you learn with, in order that we can adjust our way of communicating to the family.
We determined what a child and a family needs so that we cannot apply one size fits all. So that we can think about, "What's about rural families? What about families from a distance? How do we ensure that we can maintain the same relationship with them as we do for someone that we can see frequently and develop a personal one-on-one relationship with?"
The last point we got to was the team. Knowing that we need to have individuals on the team that can assess all aspects of a child. We can look at the learning needs of a child. To look at the capability of a child in terms of their psychological capability. To look at the aspects of how they relate. What are their sensory motor skills and so on? That whole team approach of how we can make sure that the team is present from the outset.
Supports for children at all of those stages of transition was mentioned here. I know that we're doing work on our transitions, but it's an important piece, and that’s where we see a lot of kids that struggle and we don't want that to be the case. Establishing appropriate expectations for each family dependent on the child's and the family's conditions. We want optimal development for each child, but what that means for a given child depends in part on what they present as, so we need recognition of that.
Finally, quality early interventions that are readily accessible and able to adapt to the needs of the families depending on where they live, what their resources are, the quality of intervention that can be accessed is an important piece. End of video.
Dream Journeys – Some Key Elements
As evidenced by this video, the professionals at our seminar had many things on their wish list. Please think about the topics that resonated with you, and what you think could be important in your daily life.
One of the things that stood out for me was the point about the support for the child and the family is the fact that one size does not fit all. We need to realize, as Dr. Yoshinaga-Itano also mentioned in her presentation, that every family is unique. They have different backgrounds, different dynamics, and different needs. Unless we take these differences into account, we cannot be sure that we're meeting their needs at all times during their journey.
I liked the advice encouraging parents to enjoy their child. Be parents first and let the child be a child first, before they begin to address the hearing loss. I found that to be a very valuable suggestion. Also, empowering the child to talk about their hearing loss and their needs early on will position them to leave school and enter the world being able to advocate for themselves.
The support from key communication partners, especially teachers, I also thought was very relevant because many teachers in mainstream schools do not have knowledge about hearing loss. Having a child with hearing loss enter their class does pose some challenges for the teacher. The better we can help them navigate, the better we can help them support the child, the better the child will function in that classroom setting. Also, helping the children function not only with classroom peers, but also with friends, neighbors, and everywhere else in their social circles is important.
Finally, ensuring that there is a diverse team of professionals who are skilled in different areas (e.g., psychologists, ENTs, audiologists, etc.) is necessary to help each child cope as well as possible.
Parents’ Needs
Our seminar addressed the needs, challenges and successes of patients, families and professionals throughout the CI rehab journey. One of the most important things we learned about the parents' needs is they felt the professionals involved in the care of their children needed to be more personal. Professionals should move beyond the technicalities in order to strengthen the human connection. As Kate's father stated, a professionals should be a guide or a mentor. Be someone who takes them by the hand as they enter this world of hearing loss that is completely unknown to them.
It's also beneficial to take a flexible approach to care. Again, as we said before, realize that each family is unique. Each family has their own systems with varying backgrounds and different needs. The better we realize that and the more we adjust to that, the better we'll be able to support and serve them.
Mindful communication is something parents appreciate. In all the videos we did for the seminar, parents indicated that not only what is communicated at different times throughout the journey, but also how it's communicated is important. Also, we need to pay attention as to how our communication is received by the parents. Are they sad? Are they frustrated? Are they coping quite well? How can we make sure to pick them up when they're down and bring them forward with us on the journey?
Another concern of parents was that they felt the clinical environment could be cold and sterile. As they sat with their child waiting for examinations and meetings, they felt vulnerable. Some of them indicated that the warmer and more friendly you can make these clinical environments, the less vulnerable and more comfortable they would feel.
Finally, give hope. We heard it from Kate's father as well. Audiologists and other healthcare professionals are the main source of hope because they are the ones who are qualified to have an opinion about how the child is doing. They know what the options and possibilities are for the child. The more they are able to provide that hope, the better parents will be able to cope.
Professionals’ Challenges
We learned that as professionals, sometimes it can be a challenge to work with people from different backgrounds and cultures. There can be cultural issues or sensitivities, resulting in questions about the “dos and don'ts” within a particular culture. There may be language barriers that we need to take into account to ensure the parents are making informed choices. Some of the parents we spoke to said they didn't always understand the task asked of them or the information provided to them, because there might have been a lot of technical jargon, or there was too little explanation. We need to help them make informed choices.
In one of the videos on the Ida website from this seminar series, a set of parents were asked to choose which cochlear implant they wanted for their child on a Friday afternoon. They were sent home with information describing different cochlear implants and asked to come back on Monday to let the hospital know which one they wanted. This information was very difficult for them to understand and in the end, they ended up simply choosing by color (the color that went best with their son's hair). Clearly, we can do a better job of advising parents on what is the right choice for them.
Another point mentioned during the seminar was that healthcare professionals should try and manage the CI journey without taking over the child. During the various stages of obtaining a cochlear implant, there are many examinations that the child must undergo. Parents often felt that the child was taken away from them, and they were left to sit in the waiting room and wait for the child to come back. There were extended periods of time when they felt that the child was not really theirs, but instead a child of the system. As stated by some professionals, they were aware of the fact that there were many examinations and they were trying involve parents as much as possible, but it was not always easy.
Finally, managing parental guilt is a concern. Parents often blame themselves if the child is not progressing as intended. Professionals stated that sometimes it can be difficult to also fit in that part of caretaking. It’s important to remember to support not only the child, but also the parents; give them hope and trust in the fact that the child is doing fine.
Parents enjoyed meeting other families because that was a main source of information and support. They also appreciated tailored guidance from professionals, as well as commitment and empathy. They needed someone who would be that mentor, someone who would take them by the hand on the journey and show that they were there for them. They also valued positive reinforcement, as well as the ability to celebrate successes, however big or small. Simply saying, "Well done. We've managed a little step forward. Let's celebrate that,” was feedback that the parents appreciated, and the professionals as well.
Creating Solutions
As part of the Ida Institute innovation processes, participants were asked to be very creative in their thinking. One idea was to develop simple tools; to develop a simple process when meeting parents to identify questions and concerns they wish to discuss with their child's hearing care professional prior to each appointment, from the time of diagnosis and throughout their rehabilitation. The group presented their ideas, which you can see in the following video.
![]()
Transcript of Video: When we started talking about support earlier and what was important in terms of looking at a tool, we picked up from the videos that we've watched about how important it was for families to consider the whole family, not just the child, but to consider the journey. Looking to answer their questions that may not be the questions that we would expect or the information that we wanted to pass. Making sure that we were flexible and could answer the questions that they had at that time rather than simply sticking to a fixed structure.
As well as asking questions, we wanted to talk about information. We'd talk about giving out information to start with. We decided we wanted to come up with a short questionnaire that could be used at any point within the hearing journey. It could be used at diagnosis, it could be used at switch-on, it could still be used 5, 10 years down the line, just to ask the family what are their issues at that particular point.
We had the idea that we'd like something that we could give out in the waiting room. Maybe 10 minutes, 15 minutes before the appointment, to give people time to sit and think about what are their questions? What do they want to ask us? If you ask on the spot I think often it's hard for people to actually take time to think. If we wanted something, we could just hand out, not a long questionnaire, but just a few ideas to prompt some questions that a family might have and give them time to answer.
I think we want to keep it short so that people didn't feel like it would take a large portion of the appointment time.
It puts the family in control. They choose the questions that they want to talk about because we'd come up with a whole suite of questions in a questionnaire, but a lot of them may not be relevant so we're putting the patient in control and the family in control. They can choose which questions they want to talk about.
Options:
“I'm happy about…” -- I just thought it's nice to start off with a positive one.
“I need help with...”
“I'm concerned about...”
“I want to talk about...”
“I hope...”
“I...” -- Very open question and
“I want to find out more about...”
That's just a guide for the parents. The purpose of this tool is to provide a framework and guidance for professionals who are not really trained to do this kind of thing. First of all, it’s open-ended. It gives the parents choices. It can be used actually with a child, or with a family member, with a parent. We did have this idea that it could even be a poster in the waiting room that gives people some thinking time and that once they got used to it that they would actually just get used to coming to the appointments already with these questions in mind. I like the idea of stepping stones. We didn't really come up with a title for it, but actually some of the thoughts came from the Hands and Voices. They have parent bingo questions and they get to choose which one that they want to do. End of video.
My Turn to Talk for Parents
After the seminar, the Ida Institute turned the tool idea into an online tool called My Turn to Talk for Parents. It's called “for Parents” because we also have a version designed to be used by adult patients. The tool is freely available on the Ida website. It aims to empower parents to make their voices heard at a critical time in decision making in their child's cochlear implant journey.
The way we envision it being used is that families and parents would complete the form before they come to each appointment. That way, the family comes prepared to share and discuss their needs at the given time. It also helps professionals to get to the crux of the matter more quickly so they can be sure to support the family in the way they need it at the time. Having parents prepare before the appointment should also help save time in the appointment.
The online tool is very simple to use and consists of two steps. The first step is a way for the family to map the child's current communication situation (Figure 1).
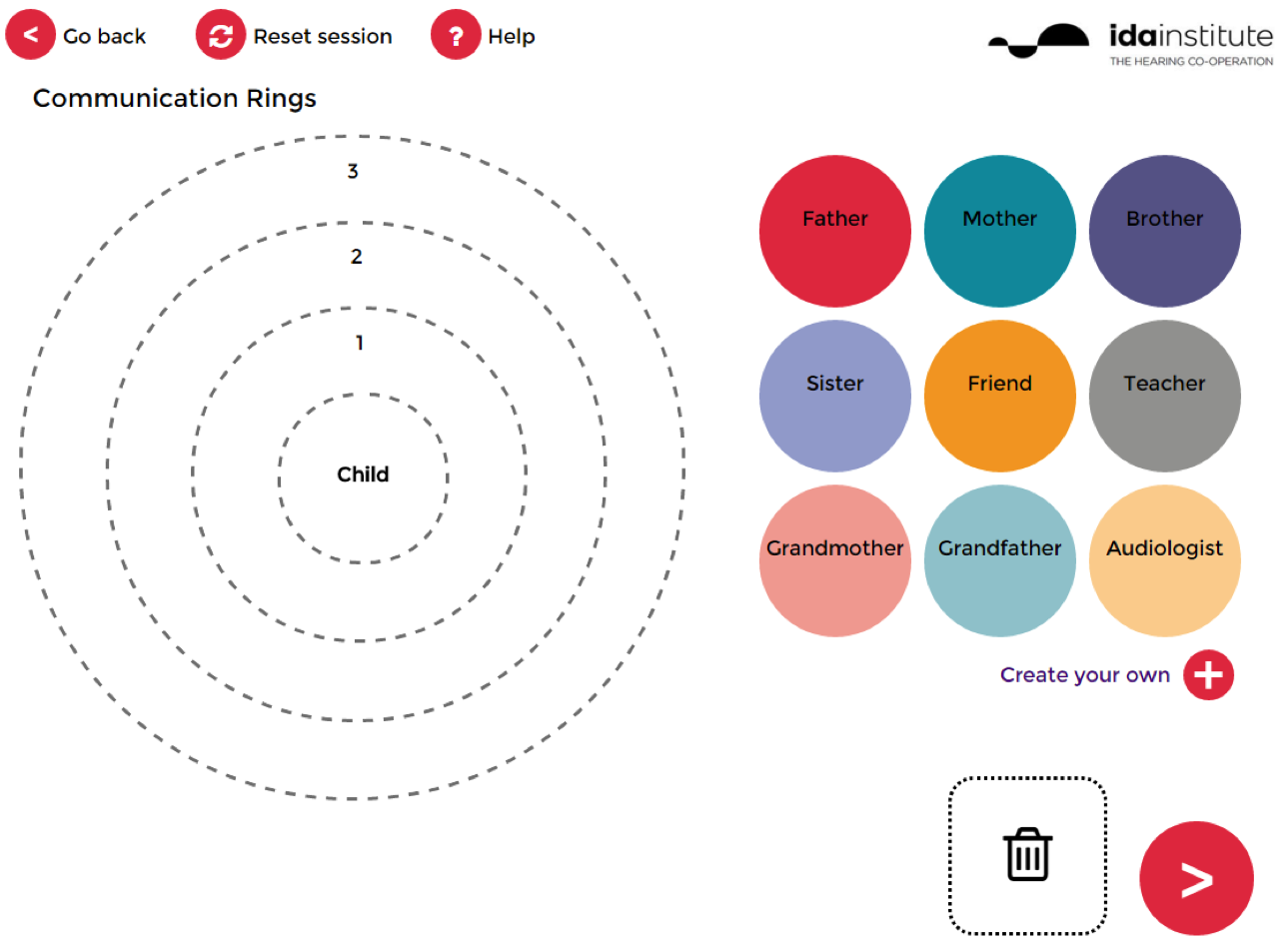
Figure 1. My Turn to Talk for Parents.
You have the child in the middle of the concentric rings. On the side are colorful circles that represent different people involved in the child’s life. You can drag and drop the circles of the people who are the most important communication partners to the child. The ones dropped in the innermost ring #1 represent the most important people to the child. Those placed within the second circle are slightly more removed, and those within the third circle are even more removed. This is an easy way to visually provide an overview of the most important people with whom we need to help this child communicate. This is useful not only for the family, but also for the professional.
Of course, a situation may change. For example, a child may have another disease or condition that requires treatment by a physician. For the duration of that period when that condition is present, the physician might move into being a very close communication partner. Then the physician will move out of the circle again when this problem has been resolved. You can also customize your own labels (e.g., Grandma Mary, Uncle Joe).
For the second step, as shown in the video, we've taken the questions that were proposed and put them into an online format. Before the parents come to the appointment, they can sit in the quiet of their home and, using these talking points, consider:
- I’m happy about…
- I want to talk about…
- I hope…
- I’m concerned about…
- I want to find out more about…
- I need help with…
- I…
They don't have to answer all the questions, but if they do, the answers will then be shown in a PDF document that can be easily printed and brought to the next appointment.
I hope you have enjoyed this very brief insight into our two-day seminar process and the results that have come out of it. Thank you very much for your attention, and we invite you to explore the Ida website to learn more.
Citation
Nielsen, E. (2016, October). Successes, gaps, and challenges in cochlear implant rehabilitation: The cochlear implant journey for children and their families. AudiologyOnline, Article 18285. Retrieved from https://www.audiologyonline.com.


