Editor's Note - June 2022: The audiology community mourns the loss of Dr. David Baguley who passed away on June 15, 2022. His legacy lives on in his research, papers, book chapters, and numerous significant professional contributions across his lifetime of work. At AudiologyOnline, we are grateful to have had the opportunity to work with Dr. Baguley for projects such as this excellent 20Q from 2017.
 From the Desk of Gus Mueller
From the Desk of Gus Mueller

Sound is an amazing thing. Different sounds can evoke a very distinct and wide range of emotions, ranging from sad to happy, excited to calming. Even very brief sounds can form an immediate impression. If you are a Baby Boomer, you only have to hear one very unique guitar chord to know that the song that likely will follow is the Beatles’ A Hard Day’s Night.
A few years back, a large survey was conducted regarding what people found to be their favorite sounds. As I recall, the finalists were: a crackling fire in the fire place, the morning chorus of birds, a babbling stream, children laughing, and my favorite—the pop of a wine cork. But what if, in your daily life, you mostly thought of sound as something to avoid rather than enjoy? This often is the life of someone with hyperacusis.
Hyperacusis is an unusual tolerance to ordinary environmental sounds; often inappropriate responses to sounds that are neither threatening nor uncomfortably loud to the average individual. Typically, these are sounds in general, not specific sounds. While this disorder has been known and discussed for some time, it has only been the last couple of decades that researchers have studied it thoroughly. One of those leading researchers is our guest this month at 20Q, David Baguley, PhD.
Dr. Baguley is Professor of Hearing Sciences, University of Nottingham, at the NIHR Nottingham Biomedical Research Centre, Nottingham, UK. He has served as the Chairman of the British Society of Audiology, and is the current President of the British Tinnitus Association. He has been honored as the American Academy of Audiology Distinguished International Audiologist, and has received the Association of and Independent Hearing Practitioners Outstanding Contribution to Audiology Award.
You are probably aware of Dr. Baguley’s hundreds of publications on a variety of audiology topics, with a focus on tinnitus and hyperacusis. Recently, he has summarized much of his work in two books: Tinnitus: Clinical and Research Perspectives, and his soon-to-be-released Hyperacusis: Clinical and Research Perspectives (Plural Publishing). We’re pleased to bring David’s expertise and experience related to the intriguing area of hyperacusis to 20Q.
Gus Mueller, PhD
Contributing Editor
October 2017
Browse the complete collection of 20Q with Gus Mueller CEU articles at www.audiologyonline.com/20Q
20Q: Update - Perspectives on Hyperacusis

David Baguley
Learning Outcomes
After this course, readers will be able to:
- Define hyperacusis, describe its symptoms, and explain how it is different from other sound sensitivity issues.
- Describe commonalities and differences between tinnitus and hyperacusis.
- List considerations for assessing and treating a person with hyperacusis in an audiology practice setting.
- List knowledge gaps and research needs in the area of hyperacusis.
1. Is hyperacusis really something that audiologists need to know about?
Most certainly. Hyperacusis is a poorly understood and under-researched condition that affects many people, both adults and children, and can lead to substantial distress. For many years it has had a low profile, but interest is gathering, and knowledge is being gathered around the world.
2. What exactly do you mean by hyperacusis?
When we talk about hyperacusis we don’t mean the super acute hearing that allows Superman to hear across great distances, or Daredevil to substitute hearing for vision with his blindness. Instead, we mean the experience of the sound environment being overwhelmingly intense. This has been defined as ‘abnormally reduced tolerance to sound’ (Baguley, 2003). It is rather different from the sound sensitivities some people experience during a migraine attack, which is misleadingly called phonophobia, even though discomfort rather than fear of sound is the defining feature in this case. It is also distinct from misophonia, which is a strong aversive reaction to particular and specific sounds, such as eating or breathing sounds. With misophonia, the defining features are disgust and rage.
3. Is hyperacusis one specific entity, or are there variations?
As clinicians and researchers have considered hyperacusis, there have been proposals that it can be sub-divided. Tinnitus Retraining Therapy (TRT) has subcategories depending on whether a person has tinnitus alone, hyperacusis alone, or both (Jastreboff & Hazell, 2004). Dr. Richard Tyler and colleagues (Tyler et al., 2014) reviewed the existing literature, and proposed that there are four types of hyperacusis:
- Annoyance hyperacusis
- Fear hyperacusis
- Loudness hyperacusis
- Pain hyperacusis
4. Does this mean that any given patient would have one of these four types of hyperacusis?
It’s not that simple. Further work needs to be done to determine if these are particular subcategories, or attributes of hyperacusis that may or may not be present in a particular patient, or at a particular time. Thinking along those lines, Baguley and Andersson (2007) described a model of hyperacusis where patients may experience fear of sound and injury, irritation/annoyance, and noise sensitivity, and may move around inside that space at different times (Figure 1). This work was undertaken from a biopsychosocial perspective on hyperacusis rather than a traditional medical approach. So, it does seem that there are variations in hyperacusis between patients, and this adds to the complexity.
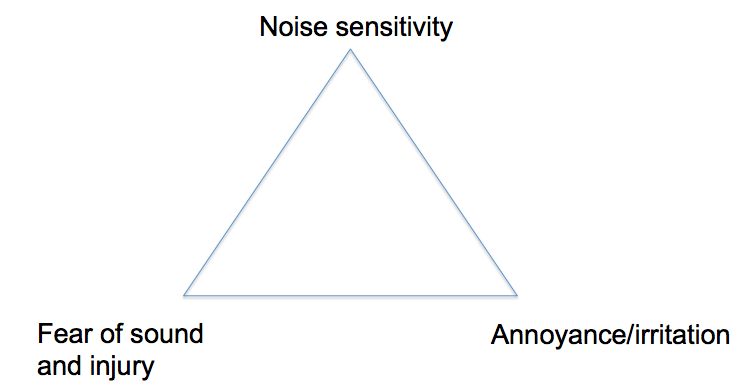
Figure 1. Three component model of hyperacusis (from Baguley & Andersson, 2007, with permission).
5. Isn’t hyperacusis extremely rare?
Unfortunately not, though reliable estimates have only recently become available. A large survey of adults in a general Swedish population found that 9.2% would self identify as having hyperacusis, and 1.9% had been formally diagnosed (Paulin, Andersson, & Nordin, 2016). In children, a UK study (Hall, Humphriss, Baguley, Parker, & Steer, 2016) that surveyed over seven thousand children aged 11 years found that 3.7% described hyperacusis (and 3.1% reported significant tinnitus). Most primary school classes hold about 30 children, so this would equate to one child in every class. As the clinical and scientific communities have only recently become aware of hyperacusis, it is hard to say whether the prevalence is growing.
6. What do people with hyperacusis say about their symptoms?
Dan Malcore is a founder of The Hyperacusis Network (www.hyperacusis.net), which is an excellent self-help resource for people with reduced sound tolerance. He developed hyperacusis some years ago following attendance at a football game where he was close to a blaring loudspeaker. He has written movingly about the experience of developing hyperacusis:
"My symptoms were severe and my life was collapsing around me. In a matter of only few days, I could no longer tolerate the normal sounds of life (conversation, telephone, television). Even my young children whispering to me or the sound of turning my head on my pillow at night was distressing." (Malcore, 2013)
Many people with hyperacusis report pain and distress caused by sound. Some report that not only is sound intense, but also more vivid, like a garish visual picture with hyper-intense contrast. As with Dan, the consequences are withdrawal from the sound environment of everyday life, leading to social isolation. For some, the fear of sound exposure is overwhelming, and potentially leads to a greater reaction when sound is encountered. These encounters can seem like continual relapses, or stepping down into greater trouble.
7. How do most audiologists react to these patients?
Some people with hyperacusis recount interactions with clinicians that are unhelpful, with reports that clinicians were dismissive during patient histories when they related their symptoms and experiences. For other clinicians, the response is compassion, and a desire to help and intervene to bring about recovery.
8. Is hyperacusis simply a side effect of anxiety and/or depression?
There is certainly a link between hyperacusis and mood disorders such as anxiety and depression. A Swedish study (Juris, Andersson, Larsen, & Ekselius, 2013) indicated that of patients being treated for a primary complaint of hyperacusis, 47% could have been diagnosed with an anxiety disorder. The indications are that the mood disorders were a consequence of the hyperacusis, rather than causing the hyperacusis. This notion was supported by another study that looked at the prevalence of reduced sound tolerance in patients with ‘emotional exhaustion’ (meaning chronic stress and depression) and found that very few had hyperacusis (Wallén, Hasson, Theorell, & Canlon, 2012). This fits with the belief of many patients that their anxiety and/or depression were a result of their challenges with sound.
9. I understand how cochlear dysfunction can give rise to hearing loss, but what can lead to reduced sound tolerance?
Good question, and one that researchers are working on! The best proposals presently indicate that with reduced sound tolerance there is some form of increased auditory gain in the central auditory system. Within neural pathways of hearing there are mechanisms that increase the gain of the system; most people are aware of being able to strain to hear, which is an example of this mechanism in play. If this attribute of the hearing system became abnormally increased, or perpetually set on high, then even quite low intensity sound would be perceived as loud. Emotional distress and fear would quickly develop as a result, and such mechanisms may underpin hyperacusis. One challenge is in developing an animal model of hyperacusis; as with tinnitus, this defies researchers in several different ways, which holds back understanding.
10. How does hyperacusis differ from recruitment?
The term recruitment indicates abnormal loudness growth, and is widely believed to be associated with cochlear outer hair cell dysfunction. It is not always possible to completely differentiate this from hyperacusis (and indeed the two may co-exist in some patients) but there are some pointers. In recruitment, low intensity sounds are typically not problematic, but in some patients with hyperacusis, all sound would be intense and distressing. The emotional aspect may also be differentiating: in recruitment, louder sound may be unpleasant, but not aversive, overwhelming, or painful as with hyperacusis. In some patients, hyperacusis varies with their mood (especially driven by anxiety and agitation); in recruitment, one would not expect to observe this. Essentially, recruitment does not imply a problem with the tolerance of sound.
11. Are there medical causes of hyperacusis that I should be looking out for?
Yes indeed! One of the exciting things about audiology is the way that it combines diagnostics with rehabilitation, and working with patients with hyperacusis is no exception. There is an incidence of hyperacusis following resolved conductive hearing loss, in closed head injury, and chronic pain disorders. Also, case reports have linked hyperacusis with multiple sclerosis and with Lyme Disease. A careful clinical history should help identify any clinical red flags for further investigation. You might be wondering how conductive hearing loss would be associated with hyperacusis. The literature on this suggests that persons with conductive hearing loss increase their central auditory gain to compensate for the loss, but that when the loss resolves (following otologic surgery for example), the gain increase persists, so the auditory environment seems overwhelmingly intense.
12. You have mentioned tinnitus several times - are the two related?
This is very interesting. Tinnitus and hyperacusis do occur together in many people. In fact, it was the complaints of reduced sound tolerance in people being treated for troublesome tinnitus that piqued the interest of many people working in the field - including me! In general, we believe that about 40% of people with bothersome tinnitus experience significant problems with sound tolerance, and that 90% of people diagnosed with hyperacusis also experience some tinnitus. These estimates seem valid for children as well as adults. Some information is missing though, particularly regarding how troublesome tinnitus is when the main problem is hyperacusis, and vice versa. This would be of benefit in designing treatment programs, and is not yet available.
13. If tinnitus and hyperacusis are so frequently co-incident, are there common mechanisms?
This would be a possibility, but we need to be careful as symptoms occurring together do not necessarily imply causality or commonality - it may actually be a coincidence! The concept of increased central auditory gain has been of interest to tinnitus researchers. One model of this is to compare the amplitude ratio of the auditory brainstem response waves I and V, arising from the cochlear nerve and lateral lemniscus, respectively. The proposal is that when central auditory gain is increased, the relative amplitude of JV compared to JI is increased, and this has been associated with the concept of ‘hidden hearing loss’ (Schaette & McAlpine, 2011). So, an increase in central auditory gain might be common to both tinnitus and hyperacusis. However, there are several indications that tinnitus and hyperacusis are different phenomena, and may involve separate pathophysiological mechanisms.
14. That’s interesting. Is there research to support that tinnitus and hyperacusis differ pathophysiologically?
These are proposals rather than facts, and need further investigation, but an initial list of the ways that tinnitus and hyperacusis diverge can be seen in Table 1 (modified from Baguley, in press).
| Hyperacusis | Tinnitus |
Influenced by somatic modulation (jaw and head movement) | Rare | Common |
Unilateral or strongly lateralised? | Rare | Common |
Influenced by emotional state and agitation | Somewhat | Very significantly |
Can be transient or intermittent? | Rare: usually consistent | Common |
Table 1. Divergent features of tinnitus and hyperacusis.
As I said, this is an area that needs further research, but there are potentially important implications for treatment programs and protocols if indeed hyperacusis and tinnitus are less directly linked than had previously been assumed.
15. I notice that some of the children I have tested over the years who have autism spectrum disorder (ASD) have sound tolerance issues. Is this similar to hyperacusis?
It is true that some people with autism spectrum disorder (ASD) report problems with sound tolerance, and this can be a major challenge for children with ASD who have little or no control over their sound environment. Professor Temple Grandin, who has ASD, has written about her experiences with sound:
"My hearing is like having a hearing aid with the volume control stuck on 'super loud.' It is like an open microphone that picks up everything. I have two choices: turn the mic on and get deluged with sound, or shut it off. I can't modulate incoming auditory stimulation." (Grandin, 1992)
What isn’t yet clear is the extent to which the sound tolerance challenges associated with ASD are similar to hyperacusis in a more general population, or whether this is a distinct clinical entity.
16. I am convinced that audiologists should engage with patients with hyperacusis. How do we go about assessing hyperacusis in the clinic?
Great, let’s get to the nitty-gritty on this. The first aspect is the clinical history. This is very similar in feel to a tinnitus history, covering both the clinical/diagnostic aspects, but also getting inside the lived experience of the reduced sound tolerance and the impact. This can take a good 45 minutes, so allow plenty of uninterrupted time, and be mindful that an unexpected phone ring or door knock can be distressing for this patient group.
Then comes the challenge of pure-tone audiometry. In some patients the hyperacusis is so marked that coming in at the usual initial presentation level is sufficiently intense to cause distress and pain (Aazh & Moore, 2017). Some modified practice of initially presenting at 20 dB HL and then raising or lowering the intensity can be beneficial. Many patients with a primary complaint of hyperacusis have normal or age appropriate hearing thresholds.
The issues around loudness discomfort testing are complex. The need to perform such a test in the hyperacusis population appears self evident, and treatment efficacy trials will need some such data indicating improvements in dynamic range if the field is going to progress. There are problems though; some loudness discomfort procedures have questionable test-retest and inter-observer variability. And, they can be deeply unpleasant for the patient, who may fear exposure to intense sound in the test and give highly conservative findings. The advice would be proceed with caution, always use an ascending approach, use care to select a low impact and reliable test protocol, and only undertake the test when it is likely to make a contribution to clinical care.
Audiologists experienced with tinnitus coming into the hyperacusis field will be wondering if there is a hyperacusis questionnaire equivalent to the Tinnitus Handicap Inventory or the Tinnitus Functional Index. The short answer is that as of today, there is not - of the three instruments presently available, each has some salient and significant shortcomings (Fackrell & Hoare, in press). Table 2 indicates the features of the questionnaires, and offers a brief note on the areas of weakness. All the questionnaires are intended for adult patients, and while questionnaires for children with hyperacusis are planned, none are yet available. If it is essential to use a questionnaire, then the Hyperacusis Questionnaire (which has been translated into several languages, though with variable validation) is probably the pragmatic choice.
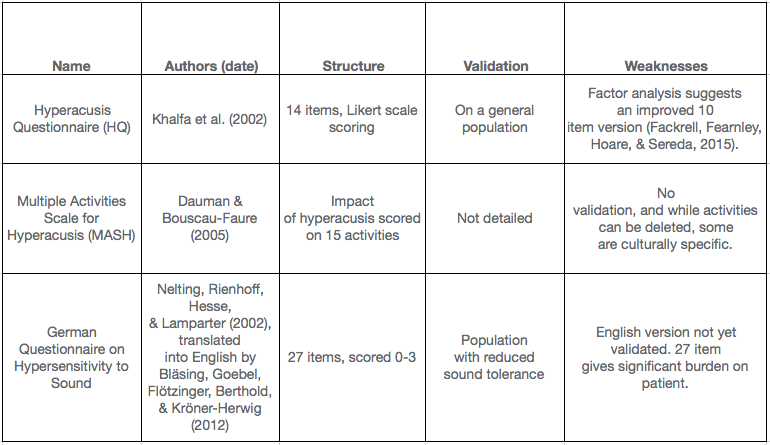
Table 2. Questionnaires for hyperacusis.
17. Great news that I can assess these patients. What about treatments?
There are several techniques that audiologists can use to inform, support, and treat patients with hyperacusis. As with treating tinnitus, the mix can include information, counselling, sound therapy, and relaxation techniques. Different patients may require and benefit from different emphases on each of these elements in their treatment. First though, we should acknowledge that self help may be very beneficial. The Hyperacusis Network has already been mentioned as a powerful resource, and has a very well moderated bulletin board so that hurtful posts rarely persist. There are some patient behaviors that can be unhelpful, though. Overuse of hearing protection can both compound fear and also reduce the input to the central auditory system such that the brain further increases auditory gain (e.g. by straining to hear). This might worsen hyperacusis. Although this is problematic, it is neither kind nor practical to request that a patient immediately desists from using hearing protection. A pragmatic approach might be to gradually wean the patient off the use of hearing protection, but allow it for challenging situations like music events, sporting events, parties, and other socially beneficial situations that involve sound.
18. I would like to hear more about the information and counselling aspects of working with patients who have hyperacusis.
Many patients with hyperacusis have not been given good information and an understanding of their situation, and benefit very significantly when this is provided. Judging when information giving becomes counselling is a fine art, but the listening skills that many audiologists have are invaluable here. Formal counselling and psychological input may also be of benefit. Dr. Linda Juris is a Swedish clinical psychologist who performed a randomized controlled trial of Cognitive Behavioral Therapy (CBT) for patients with a primary complaint of hyperacusis, and some significant benefits were reported (Juris, Andersson, Larsen, & Ekselius, 2014). The problem in many locations though, is that most audiologists are not aware of CBT or trained in it. While there is a CBT-based patient book for tinnitus and hyperacusis (McKenna, Baguley, & McFerran, 2013), for some patients that would not substitute for individual therapy. For tinnitus patients, trials are underway of CBT delivered via the Internet (iCBT – Beukes, Manchaiah, Allen, Baguley, & Andersson, 2015) and this may hold some benefit for hyperacusis in future.
If your hyperacusis patients are anxious and/or depressed, indicate to them that this may be a result of having hyperacusis. Treating these secondary symptoms might improve their quality of life, and advise that they seek specific treatment. Relaxation techniques will likely form an element of such therapy, and can be utilized also by audiologists as an element of treatment.
19. Before we finish, can you tell me a little about sound therapy?
Sure! The use of sound to treat hyperacusis is longstanding, though there is very little in the way of clinical trial evidence. Generally speaking, there have been three approaches. The first approach would be to use some type of in-ear compression device to reduce the intensity of the sound environment. The concern would be the same as that for ear protection - that the brain will seek to normalize the perceived intensity of sound, and hence further increase the auditory gain, leading to greater problems.
The second approach would be to use low intensity, wide band sound, gradually increasing the loudness so that tolerance builds up over time. This stepped or gradated exposure technique has been popular, and forms an element of TRT for hyperacusis. The third approach would be to use low intensity sound at a stable or consistent level, with the hope that the central auditory gain would ‘recalibrate’ and hence normalize. Further research is needed in each of these areas.
The wearable device technology available to audiologists active in tinnitus and hyperacusis has improved dramatically in recent years. Current technology includes sound therapy signals that can be spectrally and amplitude modulated, and has real-world environmental sounds built in or channelled via the devices. This opens a world of opportunity, but also the need to work toward protocols and pathways for the safe and effective use of these devices.
20. You have mentioned several times that more research is needed. How do you see this progressing?
There are several aspects to this. The amount of research is increasing, but there is more to do. Forthcoming work from Nottingham (Fackrell et al., in press) has recently scoped the existing literature on treatments for hyperacusis, indicating what is presently known and where there are gaps in our knowledge. Research questions in hyperacusis have also been identified (Baguley & Hoare, in press) and the following were noted:
- What is the prevalence of hyperacusis in adults and children?
- What are the risk factors associated with hyperacusis?
- What is the natural history of hyperacusis?
- How is ‘pain hyperacusis’ perceived?
- What mechanisms are involved in hyperacusis?
- What is the relationship between hyperacusis and tinnitus?
- Can a questionnaire be developed that accurately measures the impact of hyperacusis, and can be used as a treatment outcome measure?
- What treatments, alone or in combination, are effective for hyperacusis?
A modern approach to the identification of research questions does not rely upon clinicians alone, however, but partners with patients to get insights and guidance directly from their experiences. Such partnering has been undertaken in tinnitus (Hall, Mohamad, Firkins, Fenton, & Stockdale, 2013) and has begun to shape the future of tinnitus research. A similar project is at the planning stage in the UK. Additionally, the organization Hyperacusis Research (www.hyperacusisresearch.org), led by Bryan Pollard, is strongly advocating for focused and cure-directed research in this area. Watch this space!
References
Aazh, H., & Moore, B.C.J. (2017). Incidence of discomfort during pure-tone audiometry and measurement of uncomfortable loudness levels among people seeking help for tinnitus and/or hyperacusis. American Journal of Audiology, 26(3), 226-232.
Baguley, D.M. (2003) Hyperacusis. Journal of the Royal Society of Medicine, 96, 582-585.
Baguley, D.M. (in press). Reflections on the association between hyperacusis and tinnitus. In M. Fagelson & D.M. Baguley (Eds.), Hyperacusis: clinical and research perspectives. San Diego: Plural Publishing.
Baguley, D.M., & Andersson, G. (2007). Hyperacusis: Mechanisms, models, and therapies. San Diego: Plural Publishing.
Baguley, D.M., & Hoare, D.J. (in press). Unanswered questions in hyperacusis. HNO.
Beukes, E.W., Manchaiah, V., Allen, P.M., Baguley, D.M., & Andersson, G. (2015) Internet-based cognitive behavioural therapy for adults with tinnitus in the UK: study protocol for a randomised controlled trial. BMJ Open, 5(9).
Bläsing, L., Goebel, G., Flötzinger, U., Berthold, A., & Kröner-Herwig, B. (2010) Hypersensitivity to sound in tinnitus patients: an analysis of a construct based on questionnaire and audiological data. International Journal of Audiology, 49(7), 518-26. doi: 10.3109/14992021003724996
Dauman, R., & Bouscau-Faure, F. (2005). Assessment and amelioration of hyperacusis in tinnitus patients. Acta Otolaryngologica, 125(5), 503-509.
Fackrell, K., Fearnley, C. Hoare, D.J., & Sereda, M. (2015). Hyperacusis Questionnaire as a tool for measuring hypersensitivity to sound in a tinnitus research population. BioMed Research International, 2015, Article ID 290425. https://dx.doi.org/10.1155/2015/290425
Fackrell, K., & Hoare, D. (in press). Scales and questionnaires for decreased sound tolerance. In M. Fagelson & D.M. Baguley (Eds.), Hyperacusis: clinical and research perspectives. San Diego: Plural Publishing.
Fackrell, K., Potgieter, I., Shekawat, G., Baguley, D.M., Sereda, M., & Hoare, D.J. (in press) Clinical interventions for hyperacusis in adults: a scoping review to assess the current position and determine priorities for research. Biomed Research International.
Grandin, T. (1992). An inside view of autism. In E. Scopler & G.B. Meribov (Eds), High functioning individuals with autism. Current issues in autism (pp 105-126). Boston, MA: Springer.
Hall, A.J., Humphriss, R., Baguley, D.M., Parker, M., & Steer, C.D. (2016). Prevalence and risk factors for reduced sound tolerance (hyperacusis) in children. International Journal of Audiology, 55(3), 135-141.
Hall, D., Mohamad, N., Firkins, L, Fenton, M., & Stockdale, D. (2013). Identifying and prioritizing unmet research questions for people with tinnitus: the James Lind Alliance Tinnitus Priority Setting Partnership. Clinical Investigation, 3(1), 21-28.
Jastreboff, P.J., & Hazell, J.W.P. (2004). Tinnitus Retraining Therapy. Implementing the neurophysiological model. Cambridge: Cambridge University Press.
Jüris, L., Andersson, G., Larsen, H.C., & Ekselius, L. (2013). Psychiatric comorbidity and personality traits in patients with hyperacusis. International Journal of Audiology, 52(4), 230-5.
Jüris, L., Andersson, G., Larsen, H.C., & Ekselius, L. (2014). Cognitive behaviour therapy for hyperacusis: a randomized controlled trial. Behavior Reseach and Therapy, 54, 30-7.
Khalfa, S., Dubal, S., Veuillet, E., Perez-Diaz, F., Jouvent, R., & Collet, L. (2002). Psychometric normalization of a hyperacusis questionnaire. ORL, 64, 436-442.
Malcore, D. (2013). The Hyperacusis Network. ENT and Audiology News, 21(6), 72-73. Retrieved from: https://www.entandaudiologynews.com/assets/Uploads/Pdfs/Hyperacusis-JF13.pdf
McKenna, L., Baguley, D.M., & McFerran, D. (2013). Living with tinnitus and hyperacusis. London: Sheldon Press.
Nelting, M., Rienhoff, N.K., Hesse, G., & Lamparter, U. (2002). The assessment of subjective distress related to hyperacusis with a self-rating questionnaire on hypersensitivity to sound. Laryngorhinootologie, 81(5), 327-34.
Paulin, J., Andersson, L., & Nordin, S. (2016). Characteristics of hyperacusis in the general population. Noise & Health, 18(3), 178-184.
Schaette, R., & McAlpine, D. (2011). Tinnitus with a normal audiogram: physiological evidence for hidden hearing loss and computational model. Journal of Neuroscience, 31(38), 13452-7.
Tyler, R.S., Pienkowski, M., Roncancio, E.R., Jun, H.J., Brozoski, T., Dauman, N.,…Moore, B.C.J. (2014). A review of hyperacusis and future directions: Part I. Definitions and manifestations. American Journal of Audiology, 23, 402-419.
Wallén, M.B., Hasson, D., Theorell, T., & Canlon, B. (2012) The correlation between the hyperacusis questionnaire and uncomfortable loudness levels is dependent on emotional exhaustion. International Journal of Audiology, 51(10), 722-9.
Citation
Baguley, D. (2017, October). 20Q: Current perspectives on hyperacusis. AudiologyOnline, Article 21351. Retrieved from www.audiologyonline.com


